Abstract
Objectives
To evaluate the accuracy of sonographic classification of chorionicity in a large cohort of twins and investigate which factors may be associated with sonographic accuracy.
Methods
We conducted a secondary analysis of a randomized trial of preterm birth prevention in twins. Sonographic classification of chorionicity was compared with pathologic examination of the placenta. Maternal (age, body mass index, diabetes, and hypertension), obstetric (prior cesarean delivery, gestational age at the first sonographic examination, and antepartum bleeding), and sonographic (oligohydramnios, polyhydramnios, and twin-twin transfusion syndrome) factors were assessed for their possible association with accuracy.
Results
A total of 545 twin sets in which chorionicity was classified by sonography before 20 weeks’ gestation were included; 455 were dichorionic and 90 were monochorionic based on pathologic examination. Sonography misclassified 35 of 545 twin pregnancies (6.4%): 18 of 455 dichorionic twins (4.0%) and 17 of 90 monochorionic twins (19.0%). The sensitivity and specificity of sonographic diagnosis of monochorionicity were 81.1% and 96.0%, respectively. In a multivariable analysis, pregnancies with initial sonographic examinations before 14 weeks’ gestation were less likely to have misclassified chorionicity than those with sonographic examinations at 15 to 20 weeks (odds ratio [OR], 0.47; 95% confidence interval [CI], 0.23–0.96). For each week increase in gestational age, the odds of misclassification rose by 10% (OR, 1.10; 95% CI, 1.01–1.2). In the multivariable analysis, maternal age, body mass index, parity, and prior cesarean delivery were not associated with sonographic accuracy.
Conclusions
Sonography before 20 weeks incorrectly classified chorionicity in 6.4% of twin gestations. Those with first sonographic examinations performed at earlier gestational ages had improved chorionicity diagnosis.
Keywords: accuracy, chorionicity, obstetric ultrasound, sonography, twins
The rate of twin gestations continues to rise, accounting for approximately 33 of 1000 births in 2009.1 Compared with dichorionic twins, monochorionic twins have inherently different complication rates, including fetal loss, fetal anomalies, intrauterine growth restriction, and prematurity.2–7 Monochorionic twins are also at risk for twin-twin transfusion syndrome (TTTS) and twin anemia polycythemia sequence. Therefore, recommendations regarding antepartum surveillance and delivery timing differ by chorionicity, and accurate determination of chorionicity is vital when managing twin gestations.
The sonographic accuracy of chorionicity classification has been previously studied, and reported accuracy rates differ by gestational age at the time of assessment, center experience, and number of sonographic variables used.8–15 However, prior reports have been limited by relatively small numbers. In addition, these studies have not evaluated factors that may potentially limit sonographic accuracy, such as maternal body mass index (BMI), underlying maternal medical disorders, and prior cesarean delivery.
The objective of this study was to evaluate the sonographic accuracy of chorionicity classification in multiple gestations using a large multicenter cohort. In addition, we aimed to study whether maternal, obstetric, and sonographic factors were associated with accuracy.
Materials and Methods
This study was a secondary analysis of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network Trial of Progesterone in Twins and Triplets to Prevent Preterm Birth, which was a placebo-controlled, double-blind, randomized clinical trial conducted between April 2004 and February 2006 at 14 academic medical centers to evaluate whether 17-α-hydroxyprogesterone caproate is effective in the prevention of preterm birth in twin gestations.16 Women carrying twins with a gestational age of at least 16 weeks and no more than 20 weeks 3 days were eligible for the parent trial. Institutional Review Board approval was obtained before initiation of the parent study. For the secondary analysis, an Institutional Review Board exemption was obtained. The parent trial was registered at clinicaltrials.gov (NCT00099164).
A sonographic examination was required between gestational ages of 12 weeks 0 days and 20 weeks 6 days, based on clinical dating, to confirm the duration of gestation and to screen for major fetal anomalies. Pregnancies with major fetal anomalies were excluded. The sonographic classification of chorionicity was recorded at the time of randomization, as was the date of the first sonographic examination. The timing of the initial chorionicity classification was based on local institutional standards. For women who conceived spontaneously, the duration of gestation at the time of randomization was determined according to a previously described algorithm on the basis of the last menstrual period and the results of sonography of the larger fetus.17 For women who conceived by in vitro fertilization, the duration of gestation was calculated on the basis of the date of embryo transfer and the age of the embryos when transferred. Each center’s Institutional Review Board approved the study protocol. Maternal and neonatal outcomes of this population have been reported in a previous publication.16
For this study, patient records were reviewed and data were collected pertaining to sonographic classification of chorionicity before 20 weeks 6 days’ gestation, as well as chorionicity determination by pathologic examination of the placenta postpartum. Determination of chorionicity was performed at each site according to the local protocol and standard criteria, including evaluation of membrane thickness, placenta location, the and twin-peak sign. Evaluation of placentas after delivery was performed at each participating institution, and the diagnosis of chorionicity was based on pathologic criteria. The final pathologic diagnosis was compared with the documented sonographic chorionicity classification, and the sensitivity and specificity of sonography for monochorionicity were determined.
Statistical analysis was conducted with SAS software (SAS Institute Inc, Cary, NC). Diagnostic accuracy was assessed by estimating the sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio. In univariable analyses, maternal (BMI, parity, diabetes, and hypertension), obstetric (gestational age at the first sonographic examination, antepartum bleeding, and prior cesarean delivery), and sonographic (oligohydramnios, polyhydramnios, and TTTS) factors were compared between patients with a correct chorionicity classification and those incorrectly classified. Categorical data were compared by the χ2 or Fisher exact test, whereas continuous variables were compared by the Wilcoxon rank sum test. Logistic regression was used to calculate adjusted odds ratios (ORs) for the association between maternal, obstetric, and sonographic factors and sonographic accuracy. P values were obtained from 2-sided tests, with significance set at P < .05.
Results
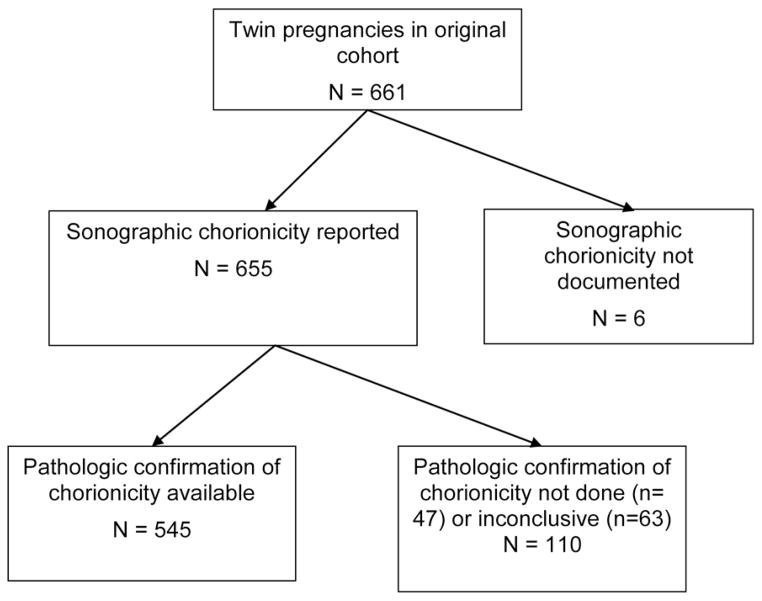
A total of 661 twin gestations were included in the parent trial. Of those, 110 patients lacked either documentation of sonographic chorionicity classification or pathologic confirmation of chorionicity (pathologic assessment not performed or inconclusive), and 6 patients were lost to follow-up (Figure 1). Baseline demographics were not different between the 545 patients included in the final analysis and those excluded, except for cesarean delivery after randomization (Table 1).
Figure 1.
Flowchart of available patients and those included in the analysis.
Table 1.
Baseline Maternal Characteristics
| Characteristic | Pathologically Confirmed Chorionicity (n = 545) | Pathologic Confirmation Not Done/Inconclusive Chorionicity/LFU (n = 116) | P |
|---|---|---|---|
| Maternal race/ethnicity | .27 | ||
| Non-Hispanic black | 130 (23.9) | 24 (20.7) | |
| Hispanic | 91 (16.7) | 14 (12.1) | |
| Other | 324 (59.5) | 78 (67.2) | |
| Maternal age, ya | .76 | ||
| <20 | 35 (6.8) | 8 (7.5) | |
| 20–29 | 216 (41.7) | 48 (44.9) | |
| ≥30 | 267 (51.5) | 51 (47.7) | |
| Marital status | .07 | ||
| Married/living with partner | 397 (72.8) | 94 (81.0) | |
| Not married | 148 (27.2) | 22 (19.0) | |
| Maternal education | .47 | ||
| Less than high school | 89 (16.3) | 15 (12.9) | |
| High school or equivalent | 109 (20.0) | 28 (24.1) | |
| Greater than high school | 347 (63.7) | 73 (62.9) | |
| Parity | .06 | ||
| 0 | 235 (43.1) | 61 (52.6) | |
| ≥1 | 310 (56.9) | 55 (47.4) | |
| Previous cesarean delivery | 60 (11.0) | 5 (4.3) | .03 |
| Smoking status | .33 | ||
| Smoker | 54 (9.9) | 15 (12.9) | |
| Nonsmoker | 491 (90.1) | 101 (87.1) | |
| Prepregnancy BMI, kg/m2 b | .30 | ||
| <25 | 253 (47.5) | 57 (50.4) | |
| 25–29.9 | 125 (23.5) | 31 (27.4) | |
| ≥30 | 155 (29.1) | 25 (22.1) | |
| Gestational age at 1st sonography, wk | 11.5 ± 4.1 | 12.2 ± 4.4 | .17 |
Data are presented as number (percent) or mean ± SD. LFU indicates lost to follow-up.
Thirty-six missing maternal age.
Fifteen missing BMI.
Of the 545 patients included in the final analysis, 455 were classified as dichorionic and 90 as monochorionic by final pathologic evaluation of the placenta. Sonography misclassified 35 of 545 patients (6.4%); 18 of 455 dichorionic twin sets (4.0%) were misclassified as monochorionic by sonography, whereas 17 of 90 monochorionic twin sets (19.0%) were misclassified as dichorionic by sonography. The sensitivity of sonography for the diagnosis of monochorionicity was 81.1% (95% confidence interval [CI], 73.0%–89.2%), and the specificity was 96.0% (95% CI, 94.3%–97.8%). The positive likelihood ratio for the diagnosis of monochorionicity was 20.5 (95% CI, 12.9–32.6), and the negative likelihood ratio was 0.2 (95% CI, 0.1–0.3).
There were no differences in maternal age, BMI, parity, prior cesarean delivery, or the presence of polyhydramnios or oligohydramnios between those with correct classification of chorionicity and those misclassified (Table 2). Patients with correct classification of chorionicity were more likely to have had a first-trimester sonographic examination (71.0% versus 54.3%; P = .04) and to have had their first sonographic examination performed at an earlier gestational age (11.4 ± 4.1 versus 13.0 ± 4.4 weeks; P = .03; Table 2). Similarly, in multivariable models, only first-trimester sonography was associated with sonographic accuracy, with pregnancies whose examinations were performed at earlier gestational ages (<14 weeks) being less likely to have misclassified chorionicity than those whose initial examinations were performed at 15 to 20 weeks (OR, 0.47; 95% CI, 0.23– 0.96; Table 3). For every week increase in gestational age at the first sonographic examination, the odds of misclassification rose by 10% (OR, 1.10; 95% CI, 1.01–1.2).
Table 2.
Maternal and Sonographic Factors and Accuracy of Sonographic Chorionicity Assessment
| Factor | Chorionicity Correct (n = 510) | Sonographic Chorionicity Misclassified (n = 35) | P |
|---|---|---|---|
| Maternal age, y | 29.8 ± 7.0 | 27.9 ± 5.8 | .41 |
| Maternal BMI, kg/m2 | 27.0 ± 6.8 | 28.3 ± 7.6 | .48 |
| Primiparity | 220 (43.1) | 15 (42.9) | .97 |
| Diabetes | 2 (0.4) | 0 | >.99 |
| Hypertension | 13 (2.6) | 1 (2.9) | .61 |
| Prior cesarean delivery | 56 (11.0) | 4 (11.4) | >.99 |
| TTTS | 7 (1.4) | 1 (2.9) | .41 |
| Polyhydramnios | 7 (1.4) | 0 | >.99 |
| Oligohydramnios | 21 (4.1) | 0 | >.99 |
| Antepartum bleeding | 9 (1.8) | 0 | >.99 |
| Gestational age at 1st sonography, wk | 11.4 ± 4.1 | 13.0 ± 4.4 | .03 |
| 1st-trimester sonography | 362 (71.0) | 19 (54.3) | .04 |
Data are presented as mean ± SD or number (percent).
Table 3.
Multivariable Analysis of the Effect of Maternal and Sonographic Factors on Correct Classification of Chorionicity
| Factor | Adjusted OR (95% CI) | P |
|---|---|---|
| 1st-trimester sonography | 0.47 (0.23–0.96) | .04 |
| Maternal age | 0.97 (0.92–1.03) | .35 |
| Maternal BMI | 1.02 (0.97–1.07) | .40 |
| Nulliparity | 1.11 (0.51–2.42) | .78 |
| Prior cesarean delivery | 1.10 (0.35–3.48) | .87 |
Each factor was adjusted for all other factors in the table.
Discussion
In our cohort, sonography performed before 20 weeks’ gestation incorrectly classified chorionicity in 6.4% of twin gestations. Importantly, 19% of monochorionic twin sets were incorrectly classified as dichorionic. It is possible that sonographers were more inclined to classify twins as dichorionic given their increased incidence compared with monochorionic twins. Several sonographic parameters may assist clinicians in differentiating monochorionic from dichorionic twins. The number and location of placentas, a thick membrane composed of two chorionic and two amniotic membranes, a “lambda” or “twin-peak” sign, the presence of TTTS, and discordant fetal sex have been previously described both as isolated parameters and in various combinations. Unfortunately, prior studies were often limited in size, and some sonographic parameters may not be present until later in gestation (TTTS), whereas others are easier to determine in the first trimester (twin-peak sign).
Misclassification of chorionicity is particularly worrisome given recent data highlighting the increased morbidity and mortality associated with monochorionic twins. In a study of 2161 twin pregnancies, McPherson and colleagues5 found that monochorionic pregnancies had an increased risk of a single demise (adjusted OR, 1.69; 95% CI, 1.04–2.75) and a double demise (adjusted OR, 2.11; 95% CI, 1.02–4.37). Increased mortality rates in monochorionic twins may be related to increased rates of TTTS, although some data suggest an increased risk of stillbirth even in apparently normal monochorionic twins.2,7 The fact that 17 of 90 monochorionic twin sets (19%) were misclassified as dichorionic in our cohort suggests that some patients may not have been treated appropriately.
In our cohort, pregnancies that had their first sonographic examinations performed before 14 weeks’ gestation were less likely to have misclassified chorionicity compared with those that had their first scans performed at 15 to 20 weeks (OR, 0.47; 95% CI, 0.23–0.96). Moreover, for every week increase in gestational age, the odds of misclassification rose by 10%. The benefit of chorionicity classification in the first trimester (and even as early as 41 days’ gestation) has been described in prior studies.14 In their study of 131 twin sets, Stenhouse and colleagues9 described an overall 95% accurate classification rate, but when chorionicity was determined before 14 weeks’ gestation, the correct diagnosis was made in 95 of 96 twin sets. In addition to greater accuracy, early classification of chorionicity may also enable the selection of appropriate prenatal diagnostic methods, as both aneuploidy screening interpretation and genetic diagnostic testing methods may be influenced by chorionicity.
The fact that other maternal and sonographic factors such as maternal BMI and prior cesarean delivery were not associated with sonographic classification of chorionicity is interesting given prior reports detailing the effect of these variables on other sonographic examinations, including second-trimester detection of fetal anomalies.18,19 It is possible that earlier sonographic examinations in women with limited transabdominal image quality prompted transvaginal imaging, or that our study was not adequately powered to assess the true effect of these variables.
Our study was not without limitations. First, the timing of each patient’s first sonographic examination was recorded as a part of this study, but the timing of chorionicity classification was not. Therefore, for women who underwent both first- and second-trimester sonography before randomization, it is unclear when the initial chorionicity classification occurred. Our finding that pregnancies whose sonographic examinations were performed at earlier gestations were associated with improved chorionicity classification suggests that chorionicity was likely determined at the time of earlier examinations. In addition, we were unable to analyze sonographer expertise and which sonographic factor or factors were used to classify chorionicity, as these elements were not standardized as part of the original study protocol. It is possible that different or even fewer sonographic parameters were used in the misclassified cases compared with those with correct classification. That being said, each site determined chorionicity independently; therefore, our data may be more representative of the true sonographic misclassification rate than previously reported limited single-center case series.
These data highlight the importance of evaluating chorionicity early in gestation and the limitation of sonographic classification of monochorionic twins. A diagnosis of “twins” should therefore be replaced by either “monochorionic twins” or “dichorionic twins.”20 Moreover, reconsidering the classification of dichorionicity in certain circumstances (eg, with features suggestive of TTTS) may be warranted to achieve optimal antepartum surveillance, although additional studies are warranted to confirm such conclusions.
Acknowledgments
We thank the following subcommittee members who participated in protocol development and coordination between clinical research centers (Margaret Cotroneo, RN, and Allison T. Northen, MSN, RN), protocol/data management and statistical analysis (Elizabeth Thom, PhD), and protocol development and oversight (Catherine Y. Spong, MD). This project was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; HD27869, HD21410, HD40512, HD34136, HD34208, HD40485, HD27915, HD40544, HD40560, HD27917, HD40500, HD34116, HD40545, HD27860, and HD36801) and the National Center for Research Resources (M01 RR00080 and UL1 RR024989); its contents do not necessarily represent the official view of the NICHD, National Heart, Lung, and Blood Institute, National Center for Research Resources, or National Institutes of Health. Source of the study: NICHD Maternal-Fetal Medicine Units Network Trial of Progesterone in Twins and Triplets to Prevent Preterm Birth study (clinicaltrials.gov number NCT00099164).
Abbreviations
- BMI
body mass index
- CI
confidence interval
- OR
odds ratio
- TTTS
twin-twin transfusion syndrome
Other Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network Members
In addition to the authors, other members of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network are as follows: George Washington University Biostatistics Center—E. Thom, A. Braga, E. Cardenas, L. Leuchtenburg; University of Alabama at Birmingham—W. Andrews, J. Sheppard, A. Northen; University of Pittsburgh—E. Daugherty, M. Cotroneo, H. Simhan; Drexel University—M. Hoffman, S. Wilson, C. Tocci, M. Lake, M. Talucci; Northwestern University—M. Dinsmoor (NorthShore University Health System), G. Mallett, P. Simon, M. Huntley, M. Ramos; Eunice Kennedy Shriver National Institute of Child Health and Human Development—C. Spong, S. Tolivaisa; University of Utah—K. Anderson, F. Porter (LDS Hospital), A. Guzman (McKay-Dee Hospital Center), K. Jolley (Utah Valley Regional Medical Center), S. Quinn (LDS Hospital); Columbia University—R. Berkowitz, S. South, L. Paley, S. Bousleiman, V. Carmona; The Ohio State University—F. Johnson, C. Latimer; Case Western Reserve University—C. Milluzzi, C. Heggie, H. Ehrenberg, B. Stetzer, A. Merlino; University of North Carolina at Chapel Hill—K. Boggess, K. Dorman, S. Timlin; Wayne State University—G. Norman, C. Sudz, S. Blackwell; Brown University—D. Allard; University of Texas Southwestern Medical Center—K. Leveno, L. Moseley; University of Texas Health Science Center—D. Soebbing-Cross, J. Martinez, B. Glenn-Cole, L. Gilstrap; and Wake Forest University Health Sciences—P. Meis, M. Swain, K. Johnson, K. Lanier, C. Leftwich. Maternal-Fetal Medicine Units Network Steering Committee Chair: G. Anderson, MD (University of Texas Medical Center, Galveston, TX).
Footnotes
The study was presented at the 2013 American Institute of Ultrasound in Medicine Annual Convention; April 6–10, 2013; New York, New York.
References
- 1.National Center for Health Statistics. Births: 2009. Centers for Disease Control and Prevention website; 2010. National vital statistics reports. http://www.cdc.gov/nchs/births. [Google Scholar]
- 2.Lee YM, Wylie BJ, Simpson LL, D’Alton ME. Twin chorionicity and the risk of stillbirth. Obstet Gynecol. 2008;111:301–308. doi: 10.1097/AOG.0b013e318160d65d. [DOI] [PubMed] [Google Scholar]
- 3.Harper LM, Weis MA, Odibo AO, Roehl KA, Macones GA, Cahill AG. Significance of growth discordance in appropriately grown twins. Am J Obstet Gynecol. 2013;208:393e1–393.e5. doi: 10.1016/j.ajog.2013.01.044. [DOI] [PubMed] [Google Scholar]
- 4.D’Antonio F, Khalil A, Dias T, Thilaganathan B Southwest Thames Obstetric Research Collaborative (STORK) Early fetal loss in monochorionic and dichorionic twin pregnancies: the STORK multiple pregnancy cohort. Ultrasound Obstet Gynecol. 2013;41:632–636. doi: 10.1002/uog.12363. [DOI] [PubMed] [Google Scholar]
- 5.McPherson JA, Odibo AO, Shanks AL, Roehl KA, Macones GA, Cahill AG. Impact of chorionicity on risk and timing of intrauterine fetal demise in twin pregnancies. Am J Obstet Gynecol. 2012;207:190.e1–190.e6. doi: 10.1016/j.ajog.2012.07.031. [DOI] [PubMed] [Google Scholar]
- 6.Oldenburg A, Rode L, Bodker B, et al. Influence of chorionicity on perinatal outcome in a large cohort of Danish twin pregnancies. Ultrasound Obstet Gynecol. 2012;39:69–74. doi: 10.1002/uog.10057. [DOI] [PubMed] [Google Scholar]
- 7.Morikawa M, Yamada T, Yamada T, Sato S, Cho K, Minakami H. Prospective risk of stillbirth: monochorionic diamniotic twins vs dichorionic twins. J Perinat Med. 2012;40:245–249. doi: 10.1515/jpm-2011-0205. [DOI] [PubMed] [Google Scholar]
- 8.Monteagudo A, Timor-Tritsch IE, Sharma S. Early and simple determination of chorionic and amniotic type in multifetal gestations in the first fourteen weeks by high-frequency transvaginal ultrasonography. Am J Obstet Gynecol. 1994;170:824–829. doi: 10.1016/s0002-9378(94)70291-8. [DOI] [PubMed] [Google Scholar]
- 9.Stenhouse E, Hardwick C, Maharaj S, Webb J, Kelly T, Mackenzie FM. Chorionicity determination in twin pregnancies: how accurate are we? Ultrasound Obstet Gynecol. 2002;19:350–352. doi: 10.1046/j.1469-0705.2002.00679.x. [DOI] [PubMed] [Google Scholar]
- 10.Lee YM, Cleary-Goldman J, Thaker HM, Simpson LL. Antenatal sonographic prediction of twin chorionicity. Am J Obstet Gynecol. 2006;195:863–867. doi: 10.1016/j.ajog.2006.06.039. [DOI] [PubMed] [Google Scholar]
- 11.Wan JJ, Schrimmer D, Tache V, et al. Current practices in determining amnionicity and chorionicity in multiple gestations. Prenat Diagn. 2011;31:125–130. doi: 10.1002/pd.2663. [DOI] [PubMed] [Google Scholar]
- 12.Shetty A, Smith AP. The sonographic diagnosis of chorionicity. Prenat Diagn. 2005;25:735–739. doi: 10.1002/pd.1266. [DOI] [PubMed] [Google Scholar]
- 13.Senat MV, Quarello E, Levaillant JM, Buonumano A, Boulvain M, Frydman R. Determining chorionicity in twin gestations: three-dimensional (3D) multiplanar sonographic measurement of intra-amniotic membrane thickness. Ultrasound Obstet Gynecol. 2006;28:665–669. doi: 10.1002/uog.2835. [DOI] [PubMed] [Google Scholar]
- 14.Copperman AB, Kaltenbacher L, Walker B, Sandler B, Bustillo M, Grunfeld L. Early first-trimester ultrasound provides a window through which the chorionicity of twins can be diagnosed in an in vitro fertilization (IVF) population. J Assist Reprod Genet. 1995;12:693–697. doi: 10.1007/BF02212895. [DOI] [PubMed] [Google Scholar]
- 15.Mahony BS, Filly RA, Callen PW. Amnionicity and chorionicity in twin pregnancies: prediction using ultrasound. Radiology. 1985;155:205–209. doi: 10.1148/radiology.155.1.3883418. [DOI] [PubMed] [Google Scholar]
- 16.Rouse DJ, Caritis SN, Peaceman AM, et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357:454–461. doi: 10.1056/NEJMoa070641. [DOI] [PubMed] [Google Scholar]
- 17.Carey JC, Klebanoff MA, Hauth JC, et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. N Engl J Med. 2000;342:534–540. doi: 10.1056/NEJM200002243420802. [DOI] [PubMed] [Google Scholar]
- 18.Best KE, Tennant PW, Bell R, Rankin J. Impact of maternal body mass index on the antenatal detection of congenital anomalies. BJOG. 2012;119:1503–1511. doi: 10.1111/j.1471-0528.2012.03462.x. [DOI] [PubMed] [Google Scholar]
- 19.Paladini D. Sonography in obese and overweight pregnant women: clinical, medicolegal and technical issues. Ultrasound Obstet Gynecol. 2009;33:720–729. doi: 10.1002/uog.6393. [DOI] [PubMed] [Google Scholar]
- 20.Moise KJ, Johnson A. There is no diagnosis of twins. Am J Obstet Gynecol. 2010;203:1–2. doi: 10.1016/j.ajog.2009.12.002. [DOI] [PubMed] [Google Scholar]