Significance
Although neighborhood outcomes and health may influence each other reciprocally, existing studies overwhelmingly focus on neighborhood effects on health. Health’s influence on neighborhood is largely viewed as a nuisance that may bias neighborhood effects estimates. However, if health shapes whether individuals attain better neighborhoods, understanding selection processes may advance both health and urban policy objectives. We follow a socially vulnerable cohort of Hurricane Katrina survivors from 2003–2010 and find that although health was not associated with neighborhood poverty before the disaster, those with pre-Katrina health problems ended up living in poorer neighborhoods years after the storm. Understanding whether and how poor health impedes poverty deconcentration efforts may help inform programs and policies designed to help low-income families move into—and stay in—higher opportunity neighborhoods.
Keywords: health, neighborhood, selection, disaster, migration
Abstract
In contrast to a large literature investigating neighborhood effects on health, few studies have examined health as a determinant of neighborhood attainment. However, the sorting of individuals into neighborhoods by health status is a substantively important process for multiple policy sectors. We use prospectively collected data on 569 poor, predominantly African American Hurricane Katrina survivors to examine the extent to which health problems predicted subsequent neighborhood poverty. Our outcome of interest was participants’ 2009–2010 census tract poverty rate. Participants were coded as having a health problem at baseline (2003–2004) if they self-reported a diagnosis of asthma, high blood pressure, diabetes, high cholesterol, heart problems, or any other physical health problems not listed, or complained of back pain, migraines, or digestive problems at baseline. Although health problems were not associated with neighborhood poverty at baseline, those with baseline health problems ended up living in higher poverty areas by 2009–2010. Differences persisted after adjustment for personal characteristics, baseline neighborhood poverty, hurricane exposure, and residence in the New Orleans metropolitan area, with baseline health problems predicting a 3.4 percentage point higher neighborhood poverty rate (95% confidence interval: 1.41, 5.47). Results suggest that better health was protective against later neighborhood deprivation in a highly mobile, socially vulnerable population. Researchers should consider reciprocal associations between health and neighborhoods when estimating and interpreting neighborhood effects on health. Understanding whether and how poor health impedes poverty deconcentration efforts may help inform programs and policies designed to help low-income families move to—and stay in—higher opportunity neighborhoods.
Health differences across residential areas have long been recognized, with poorer neighborhoods generally exhibiting worse health outcomes (1–3). Robust associations between economically deprived areas and unhealthy residents have been found using a wide range of neighborhood and health measures (4–7), but causal relationships are not fully understood (8, 9). In particular, researchers struggle to distinguish the extent to which: (i) poor places make people sick (a type of “neighborhood effect”), (ii) being sick causes people to end up in poor neighborhoods (“reverse causation”), and (iii) sick people tend to live in poor places because health and neighborhood outcomes are both governed by a complex set of characteristics, including: multigenerational neighborhood disadvantage (10); socioeconomic status throughout the life course; race/ethnicity, in the context of residential segregation; personality; and other factors (“endogeneity”).
Although neighborhood outcomes and health may influence each other reciprocally throughout the life course and across generations, existing research overwhelmingly investigates mechanisms by which poor areas harm health, including disproportionate exposure to pollution (11), relatively fewer places to be physically active (12), and elevated risk of homicide (13), among many other examples. Designating health as an outcome and neighborhood characteristics as exposures, although key to informing equitable and health-promoting policies (14), is so pervasive that reverse causation and endogeneity are largely relegated to a single nuisance category of “selection.” Selection has been subject to ample theoretical attention (8, 14–16) and empirical scrutiny as a source of bias in neighborhood-effects estimates (17–19), but it is rarely (20, 21) viewed as an outcome of interest in its own right in the context of understanding neighborhood-health interactions.
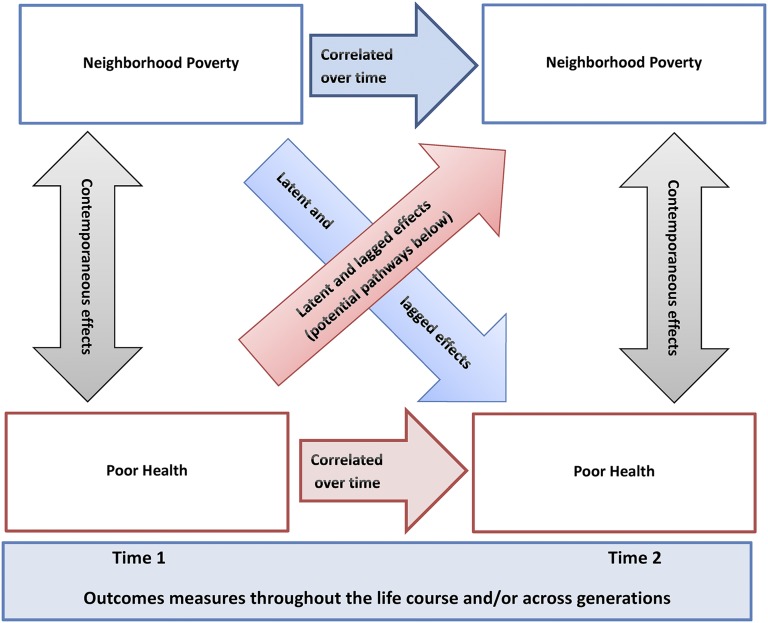
In short, our knowledge of how health affects locational outcomes is limited by disciplinary tendencies to view selection effects merely as a nuisance. However, to the extent that poor health prevents individuals from improving their neighborhood conditions, selection is a substantively important process (22) that may present actionable opportunities for advancing policy objectives, such as improving locational outcomes for low-income families and combating concentrated poverty (23, 24). Furthermore, if health problems increase the chance of living in a poor area, which in turn causes health problems, direct health-related investments could be needed to achieve both health improvements and urban policy objectives. The practical importance of these dynamics motivates the conceptual framework depicted in Fig. 1.
Fig. 1.
Reciprocal relationship between neighborhoods and health.
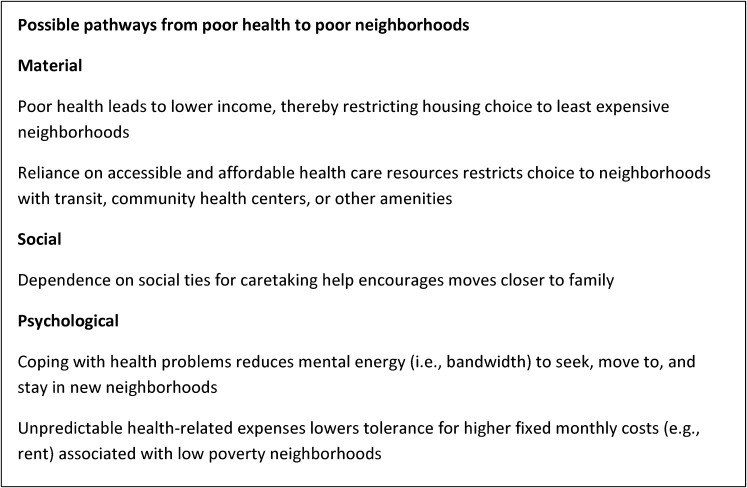
Much like the relationship between socioeconomic status and health throughout the life course (25), the interplay between health and place operates reciprocally over short- and long-term time frames, and through different mechanisms at different life stages. As shown in Fig. 1, neighborhoods may have nearly immediate effects on health, for example through exposure to violence, and health may also have contemporaneous effects on neighborhood outcomes, for example by constraining opportunities to move. We also note that latent and lagged effects are possible in both directions. For example, neighborhood-based lead exposure in childhood carries not only immediate risks, but also lagged effects, including lower adult IQ. In the opposite direction, childhood developmental delays could lead to lower adult earnings, in turn restricting neighborhood choice, even across multiple lags. More examples of how health may shape neighborhood attainment are described in Fig. 2. The relative importance of health effects on neighborhoods versus neighborhood effects on health are expected to vary according to the nature of exposures and their timing vis-à-vis sensitive developmental periods. Finally, Fig. 1 emphasizes that both health and locational outcomes are correlated over time and across generations. In the United States, we note that race/ethnicity is a uniquely important moderator of geographic mobility, and will therefore influence the degree to which neighborhood environments are similar over time and intergenerationally (10).
Fig. 2.
Possible pathways from poor health to poor neighborhoods.
Given geographic, racial/ethnic, and socioeconomic disparities in health, this framework may clarify the role health plays in reinforcing the intersection of racial/ethnic segregation and concentrated poverty (26, 27). Understanding if poor health helps direct individuals into poorer neighborhoods, and distinguishing whether this sorting reflects endogeneity or casual effects of health on neighborhood outcomes, may help inform a wide range of housing, education, and health policies that seek to decouple individual socioeconomic status, race/ethnicity, health, and neighborhood.
We use prospectively collected data on a sample of Hurricane Katrina survivors to examine if health problems predict subsequent neighborhood poverty. These data exploit high and unplanned mobility after a disaster, providing a unique opportunity to examine health as a determinant of neighborhood poverty. It is generally difficult to distinguish neighborhood effects from selection in observational data (28, 29), and to differentiate the mechanisms by which health may affect neighborhood outcomes, for example by influencing propensity to move, quality of move, or locational stability (18, 30). Our study design features three key strengths that help overcome some of these methodological hurdles. First, study inclusion criteria produced homogeneity in our sample that reduces the potential for structural confounding (29). Second, participants experienced considerable variation in neighborhood environments unlikely to be observed in a nondisaster context because Hurricane Katrina spurred high mobility among survivors as well as changes in New Orleans’ demographic composition. Finally, because participants moved in response to an exogenous shock, we are able to explore health-selection processes net of unmeasured differences in propensity to move.
Results
Table 1 provides a demographic and socioeconomic profile of our predominantly poor, African American, female sample. Participants reported good health at baseline (<5% reported fair or poor health) and somatic health complaints were more common than were diagnosed medical conditions. The mean Census tract (“neighborhood”) poverty rate was 26% at baseline and 21% at follow-up in 2009–2010, reflecting both moves out of high-poverty New Orleans areas and changes in the composition of New Orleans itself. By 2009–2010, participants had lived in an average of 2.4 (SD: 1.25) different homes since Hurricane Katrina struck in 2005.
Table 1.
Sample characteristics (n = 569)
| Neighborhood poverty and hurricane exposure | Mean (SD) or percent |
| Neighborhood poverty | |
| Baseline neighborhood poverty rate (2003–2004) | 26 (14) |
| Follow-up neighborhood poverty rate (2009–2010) | 21 (13) |
| Baseline (2003–2004) demographic and socioeconomic characteristics | |
| Welfare/cash assistance (%) | 11.6 |
| Food stamp assistance (%) | 63.1 |
| Female (%) | 93.8 |
| Age | 25.2 (4.5) |
| Number of children | 1.8 (1.1) |
| Non-Hispanic White (%) | 10.2 |
| Non-Hispanic Black (%) | 84.9 |
| Hispanic (%) | 2.8 |
| Other race/ethnicity (%) | 2.1 |
| Married, living with spouse (%) | 8.8 |
| Married, living apart from spouse (%) | 11.4 |
| Unmarried, living with partner (%) | 5.8 |
| Unmarried, not living with partner (%) | 74 |
| Hurricane exposure | |
| Flood depth (feet) | 1.5 (2.2) |
| Bereaved (%) | 33.0 |
| Baseline (2003–2004) health characteristics | |
| Reports any health problem (%) | 44.5 |
| Diagnosed with a physical medical condition (%) | 24.4 |
| Reports at least one health complaint (%) | 30.1 |
| K6 scale of psychological distress (range: 0–24) | 4.9 (4.1) |
| Body mass index* | 28.9 (7.5) |
| Diagnosed with asthma (%) | 12.7 |
| Diagnosed with diabetes (%) | 0.5 |
| Diagnosed with a heart condition (%) | 2.5 |
| Diagnosed with high blood pressure or hypertension (%) | 8.1 |
| Diagnosed with high cholesterol (%) | 1.1 |
| Diagnosed with anther physical medical condition (%) | 10.4 |
| No health insurance (%) | 38.7 |
| Smoker (%) | 11.2 |
| Experiences frequent headaches or migraines (%) | 15.6 |
| Has back problems (%) | 19.3 |
| Has digestive problems (%) | 3.7 |
| Self-reported health is excellent (%) | 35.3 |
| Self-reported health is very good (%) | 37.6 |
| Self-reported health is good (%) | 23.7 |
| Self-reported health is fair (%) | 3.2 |
| Self-reported health is poor (%) | 0.2 |
n = 552.
As expected in a geographically concentrated and homogenous sample, tests revealed no difference in mean baseline neighborhood poverty rates for those with versus without baseline health problems (Table 2). However, those with health problems at the start of the study were living in higher poverty areas by 2009–2010 compared with their healthier counterparts.
Table 2.
t-Test for difference in mean neighborhood poverty rate between healthy and unhealthy residents in 2003–2004 and in 2009–2010
| Baseline health status measure | Reports problem | Does not report problem | t-Test for difference in means with unequal variances, P value |
| Baseline (2003–2004) neighborhood poverty rate, mean (SE) | |||
| Any health problem | 26.9 (1.0) | 25.1 (0.7) | 0.15 |
| Medical diagnosis of physical health problem | 24.9 (1.1) | 26.2 (0.7) | 0.31 |
| Somatic health complaint | 27.3 (1.3) | 25.3 (0.6) | 0.16 |
| Follow-up (2009–2010) neighborhood poverty rate, mean (SE) | |||
| Any health problem | 22.8 (0.9) | 19.4 (0.7) | 0.002 |
| Medical diagnosis of physical health problem | 23.2 (1.1) | 20.2 (0.6) | 0.02 |
| Somatic health complaint | 22.9 (1.1) | 20.1 (0.6) | 0.03 |
These differences persisted after adjustment for personal characteristics, baseline neighborhood poverty, hurricane exposure, and residence in the New Orleans metropolitan area, with baseline health problems predicting a 3.4 percentage point higher neighborhood poverty rate [95% confidence interval (CI): 1.41, 5.47]. Estimated in separate models, three measures of baseline health status, including: (i) somatic complaints, (ii) reported diagnosed physical health problems, and (iii) any somatic complaint or diagnosed condition, predicted higher subsequent neighborhood poverty (Table 3). When modeled together, both diagnosed conditions and somatic health complaints independently predicted neighborhood poverty rates, although having a diagnosed condition exhibited a larger effect size and stronger association with poverty than did reporting a somatic complaints. We found no evidence that diagnosed conditions and somatic complaints interacted (95% CI: −5.34, 4.45), nor did we find that lack of health insurance moderated the effects of having either a diagnosed conditions (95% CI: −4.80, 4.73) or a somatic complaints (95% CI: −5.38, 3.63).
Table 3.
Adjusted associations between health conditions and follow-up neighborhood poverty rate in 2009–2010
| Variable | Model 1: Any health problem | Model 2: Diagnosed physical health problem only | Model 3: Somatic health complaints only | Model 4: Diagnosed physical health problem and somatic health complaints | ||||
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | |
| Intercept | 7.24 | −0.29, 14.76 | 7.41 | −0.12, 14.95 | 7.57* | 0.00, 15.13 | 6.78 | −0.75, 14.32 |
| Any baseline health problem | 3.44*** | 1.41, 5.47 | ||||||
| Medical diagnosis of physical health problem | 3.65** | 1.34, 5.97 | 3.36** | 1.03, 5.69 | ||||
| Somatic health complaint | 2.63* | 0.41, 4.85 | 2.23* | 0.01, 4.46 | ||||
| Baseline poverty rate | 0.26*** | 0.18, 0.33 | 0.27*** | 0.20, 0.35 | 0.26*** | 0.18, 0.34 | 0.26*** | 0.19, 0.34 |
| Black (White = ref) | 4.47* | 0.84, 8.11 | 3.89* | 0.29, 7.49 | 4.36* | 0.68, 8.05 | 4.62* | 0.96, 8.29 |
| Hispanic (White = ref) | 0.81 | −5.89, 7.51 | 0.83 | −5.88, 7.54 | 0.96 | −5.78, 7.71 | 1.2 | −5.50, 7.91 |
| Other race (White = ref) | 1.8 | −5.73, 9.32 | 1.24 | −6.29, 8.77 | 1.61 | −5.95, 9.18 | 1.58 | −5.94, 9.10 |
| Baseline age | −0.19 | −0.44, 0.07 | −0.18 | −0.44, 0.07 | −0.17 | −0.43, 0.08 | −0.18 | −0.44, 0.07 |
| Male sex | 0.15 | −4.15, 4.46 | −0.24 | −4.56, 4.07 | 0.08 | −4.24, 4.41 | −0.18 | −4.48, 4.12 |
| Number of children at baseline | 0.39 | −0.62, 1.39 | 0.46 | −0.55, 1.46 | 0.38 | −0.63, 1.39 | 0.43 | −0.58, 1.43 |
| Married, not cohabitating at baseline (married, cohabitating = ref) | −0.67 | −5.31, 3.97 | −0.32 | −4.96, 4.32 | −0.38 | −5.04, 4.28 | −0.55 | −5.18, 4.08 |
| Unmarried, cohabitating at baseline (married, cohabitating = ref) | 2.8 | −2.62, 8.21 | 3.51 | −1.90, 8.92 | 3.09 | −2.35, 8.53 | 3.15 | −2.26, 8.56 |
| Unmarried, not cohabitating at baseline (married, cohabitating = ref) | 2.94 | −0.89, 6.77 | 3.28 | −0.55, 7.11 | 3.1 | −0.75, 6.95 | 3.11 | −0.72, 6.93 |
| Lives in New Orleans metro area at follow-up | 4.63*** | 2.57, 6.69 | 4.63*** | 2.56, 6.69 | 4.65*** | 2.57, 6.72 | 4.56*** | 2.50, 6.62 |
| Received cash assistance/Welfare at baseline | 4.15* | 0.95, 7.35 | 3.89* | 0.68, 7.10 | 4.16* | 0.94, 7.37 | 3.94* | 0.74, 7.14 |
| Received food stamps at baseline | 0.31 | −1.97, 2.58 | 0.37 | −1.91, 2.64 | 0.22 | −2.07, 2.51 | 0.24 | −2.03, 2.52 |
| Flood depth | 0.05 | −0.42, 0.52 | 0.07 | −0.40, 0.54 | 0.06 | −0.41, 0.54 | 0.06 | −0.41, 0.54 |
| Death of friend/family member as a result of hurricanes | −1.08 | −3.24, 1.08 | −1.01 | −3.18, 1.15 | −0.91 | −3.09, 1.26 | −1.07 | −3.23, 1.09 |
| Model R2 | 0.20 | 0.20 | 0.20 | 0.21 | ||||
*P < 0.05, **P < 0.01, ***P < 0.001.
When we adjusted for factors that might help explain how health influences selection into poor neighborhoods, associations between baseline health, and subsequent poverty were attenuated. Modeled alone, neither variable nor thematic group of variables representing family structure, economic resources, psychological distress, and social support, reduced the magnitude of the association between health status and poverty rate substantially. When modeled jointly, these candidate causal mechanisms reduced the estimated effect of baseline health problems from 3.4 (95% CI: 1.41, 5.47) to 3.0 percentage points (95% CI: 0.83, 5.24), although confidence intervals were wide around both estimates. In models that estimated the effect of each health measure on neighborhood poverty separately, health persisted as a significant predictor of poverty after full adjustment. However, when diagnosed physical conditions and somatic complaints were entered simultaneously in fully adjusted models, somatic complaints no longer predicted neighborhood poverty (Table 4).
Table 4.
Fully adjusted associations between health conditions and follow-up neighborhood poverty rate in 2009–2010
| Variable | Model 1: Any health problem | Model 2: Diagnosed physical health problem only | Model 3: Somatic health complaints only | Model 4: Diagnosed physical health problem and somatic health complaints | ||||
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | |
| Intercept | 10.22 | −0.29, 20.73 | 10.19 | −0.36, 20.73 | 10.24 | −0.32, 20.80 | 9.49 | −1.06, 20.03 |
| Any baseline health problem | 3.03** | 0.83, 5.24 | ||||||
| Medical diagnosis of physical health problem | 2.90* | 0.39, 5.41 | 2.67* | 0.15, 5.19 | ||||
| Somatic health complaint | 2.47* | 0.07, 4.86 | 2.21 | −0.19, 4.61 | ||||
| Baseline poverty rate | 0.24*** | 0.16, 0.32 | 0.25*** | 0.17, 0.33 | 0.24*** | 0.16, 0.32 | 0.24*** | 0.16, 0.32 |
| Black (White = ref) | 4.14* | 0.02, 8.26 | 3.76 | −0.35, 7.87 | 4.24* | 0.07, 8.41 | 4.36* | 0.21, 8.51 |
| Hispanic (White = ref) | 0.63 | −6.30, 7.56 | 0.77 | −6.18, 7.72 | 0.75 | −6.21, 7.71 | 0.97 | −5.97, 7.91 |
| Other race (White = ref) | −6.75 | −17.77, 4.27 | −7.1 | −18.16, 3.96 | −6.46 | −17.51, 4.59 | −7.09 | −18.12, 3.94 |
| Baseline age | −0.2 | −0.48, 0.07 | −0.21 | −0.49, 0.06 | −0.19 | −0.47, 0.08 | −0.2 | −0.47, 0.07 |
| Male sex | −0.25 | −4.94, 4.44 | −0.44 | −5.14, 4.27 | −0.22 | −4.93, 4.49 | −0.38 | −5.07, 4.32 |
| Number of children at baseline | 1.50* | 0.19, 2.81 | 1.61* | 0.30, 2.92 | 1.52* | 0.20, 2.84 | 1.55* | 0.24, 2.86 |
| Married, not cohabitating at baseline (married, cohabitating = ref) | −3.63 | −8.77, 1.51 | −3.24 | −8.39, 1.91 | −3.59 | −8.75, 1.57 | −3.46 | −8.61, 1.68 |
| Unmarried, cohabitating at baseline (married, cohabitating = ref) | −0.14 | −6.10, 5.81 | 0.52 | −5.43, 6.47 | 0.22 | −5.75, 6.18 | 0.22 | −5.72, 6.17 |
| Unmarried, not cohabitating at baseline (married, cohabitating = ref) | −0.28 | −4.60, 4.04 | 0.04 | −4.29, 4.36 | −0.11 | −4.44, 4.22 | −0.06 | −4.37, 4.26 |
| Lives in New Orleans metro area at follow-up | 3.79*** | 1.58, 6.00 | 3.78*** | 1.57, 6.00 | 3.89*** | 1.68, 6.10 | 3.73*** | 1.52, 5.94 |
| Received cash assistance/Welfare at baseline | 4.50** | 1.09, 7.91 | 4.34* | 0.92, 7.76 | 4.50* | 1.07, 7.92 | 4.39* | 0.98, 7.80 |
| Received food stamps at baseline | 0.9 | −1.56, 3.37 | 0.92 | −1.54, 3.39 | 0.78 | −1.69, 3.25 | 0.82 | −1.65, 3.28 |
| Flood depth | 0.17 | −0.33, 0.68 | 0.18 | −0.32, 0.69 | 0.19 | −0.32, 0.69 | 0.18 | −0.32, 0.68 |
| Death of friend/family member as a result of hurricanes | −1.4 | −3.71, 0.91 | −1.4 | −3.71, 0.92 | −1.31 | −3.63, 1.00 | −1.4 | −3.71, 0.91 |
| Social Support (0–27, low to high support) at follow-up | −0.01 | −0.32, 0.29 | 0.01 | −0.30, 0.31 | −0.01 | −0.32, 0.29 | 0.01 | −0.30, 0.31 |
| Monthly household income at follow-up | 0 | −0.00, 0.00 | 0 | −0.00, 0.00 | 0 | −0.00, 0.00 | 0 | −0.00, 0.00 |
| Unmarried, cohabitating at follow-up (married = ref) | 4.53* | 1.04, 8.02 | 4.47* | 0.97, 7.97 | 4.59* | 1.09, 8.09 | 4.39* | 0.89, 7.88 |
| Divorced at follow-up (married= ref) | 4.37* | 0.08, 8.67 | 4.66* | 0.35, 8.96 | 4.54* | 0.23, 8.85 | 4.58* | 0.28, 8.87 |
| Widowed at follow-up (married= ref) | −1.46 | −24.90, 21.98 | −2.31 | −25.79, 21.17 | −2.31 | −25.81, 21.20 | −1.71 | −25.14, 21.72 |
| Never married, not cohabitating at follow-up (married = ref) | 4.28** | 1.35, 7.21 | 4.19** | 1.25, 7.12 | 4.19** | 1.25, 7.13 | 4.19** | 1.27, 7.12 |
| Number of children ages 4–17 in household at follow-up | −1.66* | −2.98,-0.34 | −1.69* | −3.01, −0.37 | −1.68* | −3.00, −0.36 | −1.68* | −3.00, −0.37 |
| Used at follow-up | −1.75 | −4.30, 0.80 | −1.65 | −4.21, 0.91 | −1.85 | −4.40, 0.70 | −1.63 | −4.18, 0.92 |
| Monthly household income | 0 | −0.00, 0.00 | 0 | −0.00, 0.00 | 0 | −0.00, 0.00 | 0 | −0.00, 0.00 |
| Nonspecific psychological distress (0–24, low to high distress) | 0.12 | −0.11, 0.36 | 0.14 | −0.09, 0.38 | 0.14 | −0.09, 0.38 | 0.11 | −0.12, 0.35 |
| Model R-squared | 0.25 | 0.25 | 0.25 | 0.25 | ||||
*P < 0.05, **P < 0.01, ***P < 0.001.
We found that health status was not associated with Census tract poverty in the 7–19 mo following Hurricane Katrina, meaning that health did not appear to sort respondents into neighborhood immediately after the disaster. Mean neighborhood poverty rates for healthy (22.5% poverty) versus unhealthy residents (22.1% poverty) were indistinguishable (t test for a difference in means: P = 0.70), and associations between health problems and 2006–2007 poverty were null in fully adjusted models (Table 5). Because measurement error in neighborhood poverty estimates drawn from 2006 to 2010 data could have biased results toward the null, we refit models using Census 2000 estimates of 2006–2007 neighborhood poverty and saw consistent results.
Table 5.
Fully Adjusted associations between health conditions and neighborhood poverty rate immediately following Hurricane Katrina (2006-2007)
| Predictor | β | 95% CI |
| Any health problem | 0.08 | −2.24, 2.39 |
| Medical diagnosis of physical health problem | 2.17 | −0.47, 4.81 |
| Somatic health complaint | 0.26 | −2.25, 2.77 |
Models adjusted for baseline neighborhood poverty rate, race/ethnicity, sex, age, marital status, number of children, welfare assistance, and food stamp assistance; bereavement and flood depth as a result of Hurricane Katrina; and residence in the New Orleans metropolitan area in 2006–2007.
Discussion
We present three salient findings. First, we show that baseline health problems were predictive of living in poorer neighborhoods 4 to 5 y after Katrina. Given that health status was not associated with neighborhood poverty at baseline, results demonstrate the potential for a shock to spur health selection into neighborhoods. When we controlled for characteristics that could have influenced both baseline health and subsequent neighborhood outcomes, we did not find evidence of confounding by demographic, socioeconomic, family structure, or other factors. Additionally, although New Orleans overall exhibits dramatic geographic health disparities by neighborhood wealth, with a life expectancy gap of 25.5 y between the most and least impoverished zip codes (31), our sampling design allowed us to focus on health variability within a relatively homogenous, socially vulnerable population. A lack of attenuation after introducing statistical controls, plus planned homogeneity in our sample, suggest that health may have been an important causal driver of neighborhood outcomes. However, because we could not precisely measure and control for all potentially relevant personal characteristics, the selective migration we observe could instead reflect complex underlying differences in individuals’ chances of being sick and of ending up in economically deprived areas. Identifying mechanisms that translated health into subsequent neighborhood outcomes would have strengthened a causal interpretation of the findings, but we could not pinpoint specific intermediary outcomes that explained how worse health led to residence in poorer neighborhoods.
Second, although somatic health complaints and diagnosed medical conditions both predicted higher neighborhood poverty, diagnosed conditions exhibited larger and stronger effects even after adjusting for insurance status. Finally, we provide insight into the temporal dimension of health selection into neighborhoods, showing that sorting processes not detectable by 7–19 mo postdisaster were evident 4–5 y following Hurricane Katrina.
Taken together, our results demonstrate that selective migration occurred slowly over time following Hurricane Katrina, and suggest that better health may have protected respondents against neighborhood deprivation in this highly mobile, socially vulnerable sample. Health differences mattered despite the overall good health and youth of the participants, and despite the fact that respondents were moving out of—and into—poorer than average neighborhoods. The fact that health did not differentiate participants based on the quality of their initial post-Katrina neighborhoods [which has also been described in previous work (32)], nor was health the driver of initial post-Katrina mobility, narrows the pool of candidate processes by which health could have influenced neighborhood outcomes. For example, better health may have helped people seek out higher opportunity areas in subsequent postdisaster moves, or it may have protected against returns to high-poverty areas after initial displacement. In the Moving to Opportunity housing mobility experiment, which helped families move from high to lower poverty areas, researchers observed returns to poor neighborhoods over time (33), underscoring the challenges associated with sustaining gains in neighborhood economic resources. The role of health status in mitigating or exacerbating these challenges would be a fruitful area for future research.
A key limitation of the analysis is our inability to distinguish endogeneity from causal effects of health on neighborhood outcomes. More generally, this methodological hurdle extends to most observational studies of neighborhood effects on health. Modeling the reciprocal relationships represented in our conceptual framework (Fig. 1) is almost certain to surface the same challenge: although observational data are needed to model real-world, dynamic relationships between health and neighborhood, analyses of such data are plagued by the threat of uncontrolled confounding. At the same time, interpreting causal effects from randomized housing mobility experiments carries its own set of well-documented challenges (19). We are limited in our ability to test for a health gradient in neighborhood attainment because of a lack of detailed data on severity of health conditions or on any objectively measured health outcomes. Furthermore, homogeneity in our sample, although advantageous in allowing us to compare neighborhood outcomes for healthy versus less healthy respondents, limits the generalizability of our findings.
Finally, it is possible that observed neighborhood differences by health would never have emerged in this sample absent Hurricane Katrina. That is, health selection processes may function differently, or not at all, in different populations or in nondisaster contexts. Because neighborhood poverty decreased for both healthy and —to a lesser extent—unhealthy respondents after the storm, survivors’ selective migration may reflect their differing capacities to leverage the tragedy of Hurricane Katrina into an opportunity. We cannot know if such a uniquely disruptive event was required for these differences to materialize, or if it simply hastened and amplified processes that occur in response to more common crises, such as the death of a loved one, job loss, or divorce, for example. It is easy to imagine how better health might confer an advantage to those in transition after major life events occur or when unexpected opportunities present themselves, but research on nondisaster populations is needed to empirically test for health effects on neighborhood outcomes in the general population.
Notwithstanding these limitations, demonstrating evidence of health selection into residential areas following a shock helps to inform research and policy. Although we conceptualize a dynamic interplay between neighborhood and health over time, a unidirectional interest in neighborhood effects on health currently dominates the literature. Studies in this realm should at least consider reciprocal associations between health and neighborhoods when estimating and interpreting effect estimates of neighborhood characteristics on health outcomes. From a policy perspective, new strategies to tackle concentrated poverty are sorely needed, and direct investments in health may help to interrupt longstanding relationships among poor places, poor people, and poor health.
More evidence on mechanisms linking health to subsequent neighborhood attainment would be critical to planning such investments, although testable pathways include reluctance to move away from social ties who help with childcare and other caretaking, minimizing housing payments in response to the threat of unplanned health-related costs or lost wages, and reduced “bandwidth” available to seek out new neighborhoods while coping with health problems (34). A different perspective on casual pathways asks what factors at the neighborhood level actively draw sicker versus healthier residents. In other words, it is not just that residents seek neighborhoods, but that neighborhoods also seek residents (35). Further investigation is needed into which structural aspects of urban inequality cast sicker residents into lower resources environments.
Understanding how health impacts mobility decisions, and how neighborhoods sort residents according to health, could not only improve initiatives designed to help low income families move to—and stay in—higher opportunity neighborhoods, but could also clarify population-level implications of extant health disparities for poverty deconcentration and racial/ethnic desegregation efforts.
Materials and Methods
Data.
Data come from the Resilience in Survivors of Katrina (RISK) project, a longitudinal study of 1,019 Hurricane Katrina survivors. Prehurricane data were prospectively collected on young, poor, predominantly African American parents from New Orleans as part of the Opening Doors Evaluation, a randomized-design program aimed to increase academic persistence in community colleges (36). Subjects were recruited from two community colleges in New Orleans in 2003–2005, with eligibility requirements that participants be between the ages of 18 and 34, be the parent of at least one dependent child under 19, have a household income under 200% of the federal poverty level, and have a high school diploma or equivalent. When Hurricane Katrina struck on August 29, 2005 in the midst of follow-up data collection, the Opening Doors Evaluation was redesigned to become the RISK Project. The RISK project followed participants to collect post-Katrina data on health, social factors, and economic well-being at two postdisaster follow-up waves (37, 38); we located and surveyed 711 of the original respondents by phone in 2006–2007 and 752 respondents in 2009–2010. The study was approved by the Harvard and Princeton Institutional Review Boards.
We were able to match 648 participants to census tract poverty rates for their baseline and 2009–2010 follow-up addresses, which were the primary study waves of interest for this analysis. Of these geocoded respondents, we excluded 15 people who did not provide information on race, 11 missing data on family structure, 24 missing mental health measures, 9 missing baseline individual socioeconomic status measures, and 20 missing one or more health measure. Our final analytic sample of 569 lived in 215 census tracts in 2003–2004 before Hurricane Katrina and in 367 tracts across 23 states by 2009–2010.
Measures.
Our outcome of interest was neighborhood poverty rate at the second follow-up (2009–2010). Participants were geocoded to 2010 Census tract boundaries and assigned 2006–2010 American Community Survey poverty rate estimates. At baseline, participants reported if they had ever been diagnosed with a range of medical conditions, including asthma, high blood pressure, diabetes, high cholesterol, heart problems, or any other physical health problems not listed. They also described if they suffered from a range of somatic health complaints, including back pain, migraine, and digestive problems. From these data, we constructed three dichotomous health measures that served as our primary predictor variables: (i) any health problem, (ii) any diagnosed physical condition, and (iii) any somatic complaint. We also collected baseline data on demographic factors, including race/ethnicity, sex, and age; family structure, including marital status and number of children; individual socioeconomic status as measured by receipt of welfare and food stamps; and address, which was used to link respondents to a pre-Katrina neighborhood poverty rate derived from Census 2000 data.
Analysis.
To look for evidence of health selection into neighborhoods following Hurricane Katrina, we tested for differences in mean neighborhood poverty rates between healthy versus unhealthy participants at baseline and again at postdisaster follow-up. Whereas differences in neighborhood deprivation at both baseline and follow-up would indicate that sicker people in our sample tended to live in poorer places, no difference at baseline followed by an emergent difference in 2009–2010 would be suggestive of selective migration over the study period.
Next, we sought to examine endogeneity versus reverse causation as an explanation for any observed differences in neighborhood poverty by health status. To do this, we used ordinary least-squares estimation to regress follow-up neighborhood poverty on baseline health controlling for potential confounding factors, such as baseline neighborhood poverty and personal characteristics, including demographic, family structure, and socioeconomic status measures. Adjusted models also controlled for New Orleans-specific effects because the metropolitan area is poorer than the national average. We included an indicator of whether follow-up neighborhoods were located in the New Orleans metropolitan area to account for disaster-related concerns (e.g., disrupted health care systems) that might disproportionally take sicker individuals away from New Orleans, and as a result, into lower poverty areas. Finally, we controlled for severity of hurricane exposure, as measured by flood depth and whether a friend or family member died as a result of Hurricane Katrina or Hurricane Rita, because severe hurricane exposure could both worsen health and influence chances of displacement outside the New Orleans metropolitan area.
Attenuated conditional associations between baseline health and subsequent neighborhood attainment would support endogeneity as an explanation for selective migration following Hurricane Katrina, with personal characteristics predicting both where people lived and how healthy they were. Alternatively, persistent associations between health and subsequent neighborhood poverty would underscore health as a potentially meaningful driver of neighborhood attainment in this sample.
Third, we added potential mediators to fully adjusted models. Factors that we hypothesized were both sensitive to baseline health and consequential for subsequent neighborhood attainment included: (i) family structure, which was measured by marital status and the number of school aged children (ages 4–17) in the household, because it could affect the perceived importance of living in a low poverty neighborhood; (ii) economic resources, including employment status and household income, which often restrict housing choices; (iii) nonspecific psychological distress measured by the K6 (39), which could reduce motivation to seek out low poverty areas; and (iv) perceived social support, which could provide information and instrumental resources needed to find better neighborhoods, among other mechanisms. Of 569 respondents, 91 were missing data on one or more of these 2009–2010 follow-up measures and were therefore excluded from fully adjusted models. However, those with complete versus missing data did not differ with regards to mean baseline or follow-up poverty rate, prevalence of health problems, or demographic characteristics.
Finally, we conducted a sensitivity analysis to explore the timing of any observed selective migration effects, specifically exploiting data collected during the first postdisaster follow-up wave in 2006–2007, 7–19 mo following Hurricane Katrina. We hypothesized that displacement was essentially random with respect to health immediately following Hurricane Katrina (32, 40), and that although 7–19 mo would not allow enough time for sorting to occur, selective migration might be evident years later in 2009–2010.
Acknowledgments
We thank Debra Umberson and Jackelyn Hwang and the two reviewers for comments on previous versions, and Christina Paxson for her leadership on the earlier phases of the Resilience in Survivors of Katrina project. This paper was funded by National Institutes of Health Grants R01HD046162 and RO1HD057599, the National Science Foundation, and the MacArthur Foundation. M.C.A. is supported by the Harvard School of Public Health's Yerby Postdoctoral Fellowship Program. S.V.S., J.E.R., and M.C.W. are supported by Robert Wood Johnson Investigator Awards in Health Policy.
Footnotes
The authors declare no conflict of interest.
See QnAs on page 16230.
References
- 1.Macintyre S, Ellaway A. In: Social Epidemiology. Berkman LF, Kawachi I, editors. Oxford Univ Press; New York: 2000. [Google Scholar]
- 2.Kawachi I, Berkman LF. Neighborhoods and Health. Oxford Univ Press; New York: 2003. [Google Scholar]
- 3.Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 4.Diez Roux AV, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 5.Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Racial disparities in context: A multilevel analysis of neighborhood variations in poverty and excess mortality among black populations in Massachusetts. Am J Public Health. 2005;95(2):260–265. doi: 10.2105/AJPH.2003.034132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: A multilevel analysis of Massachusetts births, 1989-1991. Am J Epidemiol. 2006;164(9):823–834. doi: 10.1093/aje/kwj313. [DOI] [PubMed] [Google Scholar]
- 7.Inagami S, Cohen DA, Finch BK. Non-residential neighborhood exposures suppress neighborhood effects on self-rated health. Soc Sci Med. 2007;65(8):1779–1791. doi: 10.1016/j.socscimed.2007.05.051. [DOI] [PubMed] [Google Scholar]
- 8.Subramanian SV, Glymour MM, Kawachi I. Macrosocial Determinants of Population Health. Springer; New York: 2007. Identifying causal ecologic effects on health: A methodological assessment; pp. 301–331. [Google Scholar]
- 9.Duncan GJ, Connell JP, Klebanov PK. Conceptual and methodological issues in estimating causal effects of neighborhoods and family conditions on individual development. Neighborhood Poverty. 1997;1:219–250. [Google Scholar]
- 10.Sharkey P. Stuck in Place: Urban Neighborhoods and the End of Progress Toward Racial Equality. Univ of Chicago Press; Chicago: 2013. [Google Scholar]
- 11.Ponce NA, Hoggatt KJ, Wilhelm M, Ritz B. Preterm birth: The interaction of traffic-related air pollution with economic hardship in Los Angeles neighborhoods. Am J Epidemiol. 2005;162(2):140–148. doi: 10.1093/aje/kwi173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 13.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: Individual and neighbourhood determinants. J Epidemiol Community Health. 2000;54(7):517–524. doi: 10.1136/jech.54.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oakes JM. The (mis)estimation of neighborhood effects: Causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58(10):1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: Social processes and new directions in research. Annu Rev Sociol. 2002;28:443–478. [Google Scholar]
- 17.Zick CD, et al. Re-visiting the relationship between neighbourhood environment and BMI: An instrumental variables approach to correcting for residential selection bias. Int J Behav Nutr Phys Act. 2013;10:27. doi: 10.1186/1479-5868-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grafova IB, Freedman VA, Lurie N, Kumar R, Rogowski J. The difference-in-difference method: Assessing the selection bias in the effects of neighborhood environment on health. Econ Hum Biol. 2014;13:20–33. doi: 10.1016/j.ehb.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clampet‐Lundquist S, Massey DS. Neighborhood effects on economic self-sufficiency: A reconsideration of the moving to opportunity experiment. Am J Sociol. 2008;114(1):107–143. [Google Scholar]
- 20.van Lenthe FJ, Martikainen P, Mackenbach JP. Neighbourhood inequalities in health and health-related behaviour: Results of selective migration? Health Place. 2007;13(1):123–137. doi: 10.1016/j.healthplace.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Dunn E, Winning A, Subramanian SV. 2014. Does poor health predict moving, move quality, and desire to move?: A study examining health effects on neighborhood selection in US adolescents and adults. Health Place 30:154–164.
- 22.Sampson RJ, Sharkey P. Neighborhood selection and the social reproduction of concentrated racial inequality. Demography. 2008;45(1):1–29. doi: 10.1353/dem.2008.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Briggs X de S, Comey J, Weismann G. Struggling to stay out of high-poverty neighborhoods: Housing choice and locations in moving to opportunity’s first decade. Hous Policy Debate. 2010;20(3):383–427. [Google Scholar]
- 24.Brooks-Gunn J, Duncan G, Aber JL. Neighborhood Poverty, Volume 2: Policy Implications in Studying Neighborhoods. Russell Sage Foundation; New York: 1997. [Google Scholar]
- 25.Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- 26.Massey D, Denton N. American Apartheid: Segregation and the Making of the Underclass. Harvard Univ Press; Cambridge, MA: 1998. [Google Scholar]
- 27.Quillian L. Segregation and poverty concentration: The role of three segregations. Am Sociol Rev. 2012;77(3):354–379. doi: 10.1177/0003122412447793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharkey P. An alternative approach to addressing selection into and out of social settings neighborhood change and African American children’s economic outcomes. Sociol Methods Res. 2012;41(2):251–293. [Google Scholar]
- 29.Oakes JM. Commentary: Advancing neighbourhood-effects research—Selection, inferential support, and structural confounding. Int J Epidemiol. 2006;35(3):643–647. doi: 10.1093/ije/dyl054. [DOI] [PubMed] [Google Scholar]
- 30.Hanson S. Perspectives on the geographic stability and mobility of people in cities. Proc Natl Acad Sci USA. 2005;102(43):15301–15306. doi: 10.1073/pnas.0507309102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orleans Parish Place Matters Team . Place Matters for Health in Orleans Parish: Ensuring Opportunities for Good Health for All. Joint Center for Political and Economic Studies; Washington, DC: 2012. [Google Scholar]
- 32.Arcaya M, James P, Rhodes JE, Waters MC, Subramanian SV. Urban sprawl and body mass index among displaced Hurricane Katrina survivors. Prev Med. 2014;65:40–46. doi: 10.1016/j.ypmed.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clark WAV. Intervening in the residential mobility process: neighborhood outcomes for low-income populations. Proc Natl Acad Sci USA. 2005;102(43):15307–15312. doi: 10.1073/pnas.0507308102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mullainathan S, Shafir E. Scarcity: Why Having Too Little Means So Much. Macmillan; New York: 2013. [Google Scholar]
- 35.Sampson RJ. Great American City: Chicago and the Enduring Neighborhood Effect. Univ of Chicago Press; Chicago: 2012. [Google Scholar]
- 36.Brock T, Richburg-Hayes L. Paying for Persistence: Early Results of a Louisiana Scholarship Program for Low-Income Parents Attending Community College. MRDC; New York: 2006. [Google Scholar]
- 37.Rhodes J, et al. The impact of hurricane Katrina on the mental and physical health of low-income parents in New Orleans. Am J Orthopsychiatry. 2010;80(2):237–247. doi: 10.1111/j.1939-0025.2010.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paxson C, Fussell E, Rhodes J, Waters M. Five years later: Recovery from post traumatic stress and psychological distress among low-income mothers affected by Hurricane Katrina. Soc Sci Med. 2012;74(2):150–157. doi: 10.1016/j.socscimed.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kessler RC, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 40.Fussell E. In: Displaced: Life in the Katrina Diaspora. 1st Ed. Weber L, Peek LA, editors. Univ of Texas Press; Austin, TX: 2012. pp. 150–166. [Google Scholar]