Abstract
Patellofemoral dislocation is a common problem affecting the young and active population. The medial patellofemoral ligament (MPFL) is torn when the patella dislocates as it acts as a checkrein to lateral displacement. This leads to patellar instability, and MPFL reconstruction is required if the dislocation recurs after a trial of rehabilitation. We describe a “V”-shaped patellar tunnel technique to reconstruct the MPFL using an autologous gracilis graft. This modification of the patellar tunnel does not breach the lateral cortex of the patella, and it allows a broader attachment of the tendon graft to the patella, which mimics the normal anatomic attachment of the MPFL to the patella.
The medial patellofemoral ligament (MPFL) functions as a checkrein and acts as a passive soft-tissue restraint to lateral patellar displacement.1-3 It is torn when the patella dislocates.4,5 The indication for MPFL reconstruction is patellar instability.6 Instability ranges from incidental subluxation to traumatic dislocation. A variety of techniques have been described to reconstruct the ligament.7,8 We describe our “V”-shaped patellar tunnel technique.
Technique
The key points of the technique are summarized in Table 1, and the technique is demonstrated in Video 1. The patient is placed supine on the operating table, and a tourniquet is used to aid in hemostasis. Surgery is performed on an overnight-stay basis, and general anesthesia, a femoral nerve block, and intravenous prophylactic antibiotics are administered before the first incision is made.
Table 1.
Key Points
| An arthroscope is used to locate any chondral lesions and assess patellar tracking. |
| The gracilis tendon is harvested and whip-stitched at both ends. |
| The intraosseous patellar tunnel is created using 2 K-wires, angled to meet in the middle of the patella. |
| Graft is passed through the patellar tunnel before being fixed in the femoral tunnel. |
| Arthroscopy is performed through the superolateral portal to assess patellar tracking before fixing the graft in the femoral tunnel. |
| The patient is allowed full weight bearing and range of motion as tolerated. |
Arthroscopy is performed using an anterolateral portal and superolateral portal. The articular surfaces of the patella and trochlea are checked for chondral lesions. The knee is taken through its range of motion while the surgeon assesses patellar tracking from the superolateral portal.
The pes anserine tendon insertion site is palpated, and a 3- to 4-cm oblique incision is made to harvest the gracilis tendon. The gracilis tendon is whip-stitched at both ends with No. 2 Vicryl (Ethicon, Somerville, NJ), leaving long suture tails.
A 2- to 3-cm-long vertical incision is made along the proximal two-thirds of the medial border of the patella (Fig 1A). The medial border of the patella is identified. Two 2-mm K-wires (Ortho Solutions, Essex, England) are inserted in a V-shaped manner into the patella as a guide for the intraosseous patellar tunnel (Fig 1B). The entry point of the first K-wire is identified at around 10 mm distal to the superior pole of the patella on the medial border. The first K-wire is inserted at around a 40° angle (directed distally and laterally) from the medial border toward the middle of the patella. The second K-wire insertion point is identified 15 cm distal to the first K-wire insertion point on the medial border of the patella and is inserted at around a 40° angle (directed proximally and laterally), aiming to meet the first K-wire in the middle of the patella.
Fig 1.
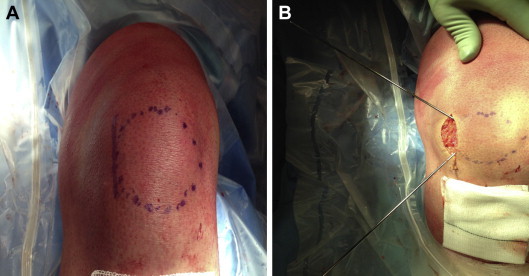
(A) The medial border of the patella is marked, and a 2- to 3-cm incision is made. (B) Two 2-mm K-wires are inserted in a V-shaped manner so that they meet in the middle of the patella.
When the second K-wire meets the first K-wire inside the patella, the first K-wire is seen to vibrate, confirming that the ends of the 2 wires are in contact. A 5-mm cannulated drill (Smith & Nephew, London, England) is sequentially passed over the 2 K-wires to form a V-shaped intraosseous tunnel for graft passage (Fig 2A). This allows at least 10 mm of bone bridge between the 2 tunnel openings on the medial border (Fig 2B).
Fig 2.
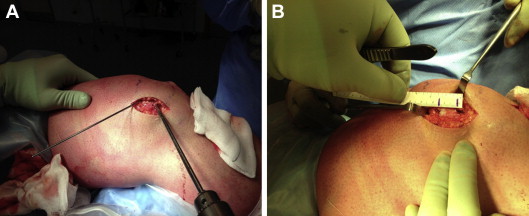
(A) A 5-mm cannulated drill is passed over the K-wires to create a V-shaped patellar tunnel. (B) View of bone bridge between 2 tunnel openings. At least a 10-mm bridge is needed to prevent tunnel blowout.
The meeting of the lateral ends of both tunnels, at the apex of the “V,” is evidenced by extrusion of bone marrow from 1 tunnel while drilling the other tunnel over the K-wire. A final confirmation of the continuity of the 2 tunnels is performed using a saline solution test, in which 5 mL of saline solution is pumped into 1 end of the tunnel and free flow of saline solution is noted through the other end.
The thread end of a curved No. 5 Ethibond needle (Ethicon) is passed from 1 end of the tunnel to the other end, and the suture loop is pulled (Fig 3). The long suture tails attached to 1 end of the gracilis tendon are fed into this loop to retrieve the graft through the other end of the tunnel (Fig 4). Blunt dissection is carried out to develop a plane between the second and third layers of the knee. The graft is passed through this plane before it is fixed in the femoral tunnel.
Fig 3.
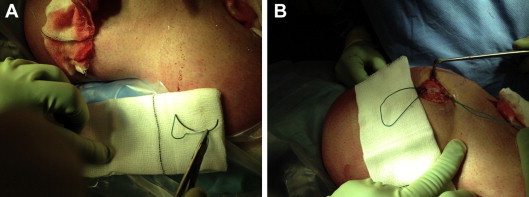
(A) The No. 5 Ethibond needle is held in the reverse direction so that the thread end of the needle is fed into the patellar tunnel first. (B) View of suture loop after No. 5 Ethibond needle has been passed through patellar tunnel.
Fig 4.
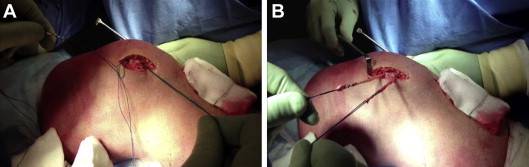
(A) Suture tails attached to the gracilis tendon are fed into the Ethibond suture loop to guide the graft through the patellar tunnel. (B) View of gracilis tendon with whip-stitched ends after having passed it through V-shaped patellar tunnel. These 2 ends are fixed in the femoral tunnel.
The medial epicondyle and adductor tubercle are palpated and exposed using a 2- to 3-cm incision. A Beath pin is passed from the medial to lateral side starting superior to the medial epicondyle. A cannulated drill of the size equal to the thickness of the gracilis graft is passed over the Beath pin to form a medial femoral tunnel. A No. 3 nylon suture (Ethicon) is passed through the femoral tunnel using the eye of the Beath pin, and then the long suture tails at the end of the gracilis tendon are fed into this nylon suture loop and pulled from the lateral side so that the graft is pulled into the medial femoral tunnel.
Arthroscopy through the superolateral portal is repeated at this stage to assess patellar tracking before securing the graft in the tunnel with an interference screw. This step prevents over-tensioning of the graft. The graft passes through a V-shaped tunnel in the patella, and both of its ends are secured in the medial femoral tunnel. Wound closure is performed, and an extension knee splint is applied. The patient is allowed full weight bearing and range of motion as tolerated.
Discussion
The MPFL is a soft-tissue restraint preventing lateral displacement of the patella.1 It is non-isometric and has a mean tensile strength of 208 N.9,10 It arises in the depression formed between the medial epicondyle and adductor tubercle. It inserts on the proximal two-thirds of the medial patellar border. The MPFL lies in the second layer on the medial side of the knee.10 It tightens in full extension and loosens in flexion.10 The MPFL is most taut in full extension, whereas the patella subluxates mostly at 20° of flexion.11 MPFL disruption occurs in patellar dislocation, which in turn affects the patellar tracking due to a lateral force in the absence of the MPFL.
The reconstruction techniques are of 2 types: a “tunnel technique,” in which a patellar tunnel is created, and a “suture technique,” in which sutures or anchors are used for patellar fixation of the graft.10 A systematic review showed that a trend of more overall complications was noted with the tunnel technique (29%) compared with the suture technique (21%).10 However, the risk of recurrent dislocation/subluxation and apprehension/hypermobility was more common with the suture technique than with the tunnel technique.10 The suture technique had a redislocation/subluxation rate of 4.8% compared with 3.3% for the tunnel technique. The risk of apprehension/hypermobility was 24.0% with the suture technique compared with 8.6% with the tunnel technique.10
The most severe complication of fracture has been reported in single or double trans-patellar tunnels, in which the graft is passed through the patella for lateral fixation.10 Our technique avoids traversing the full width of the patella and thus lateral fixation.
The advantages of the described V-shaped tunnel technique for MPFL reconstruction are that it does not breach the lateral cortex of the patella and it allows broader attachment of the tendon graft to the patella, which mimics the normal anatomic attachment of the MPFL to the patella. It also avoids the risk of a prominent EndoButton (Smith & Nephew) on the lateral patellar border. The potential risk of this technique is tunnel blowout if there is a small bone bridge between the 2 tunnel openings on the medial border. We have always maintained at least a 10-mm bone bridge between the 2 tunnel openings and have had no problems.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Different stages of MPFL reconstruction using V-shaped patellar tunnel.
References
- 1.Conlan T., Garth W.P., Jr., Lemons J.E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Desio S.M., Burks R.T., Bachus K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 3.Camp C.L., Krych A.J., Dahm D.L., Levy B.A., Stuart M.J. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38:2248–2254. doi: 10.1177/0363546510376230. [DOI] [PubMed] [Google Scholar]
- 4.Garth W.P., Jr., DiChristina D.G., Holt G. Delayed proximal repair and distal realignment after patellar dislocation. Clin Orthop Relat Res. 2000;377:132–144. doi: 10.1097/00003086-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Sallay P.I., Poggi J., Speer K.P., Garrett W.E. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24:52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 6.Bitar A.C., Demange M.K., D’Elia C.O., Camanho G.L. Traumatic patellar dislocation: Nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med. 2012;40:114–122. doi: 10.1177/0363546511423742. [DOI] [PubMed] [Google Scholar]
- 7.Drez D., Jr., Edwards T.B., Williams C.S. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 8.Muneta T., Sekiya I., Tsuchiya M., Shinomiya K. A technique for reconstruction of the medial patellofemoral ligament. Clin Orthop Relat Res. 1999;359:151–155. doi: 10.1097/00003086-199902000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Mountney J., Senavongse W., Amis A.A., Thomas N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87:36–40. [PubMed] [Google Scholar]
- 10.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amis A.A., Firer P., Mountney J., Senavongse W., Thomas N.P. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–220. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Different stages of MPFL reconstruction using V-shaped patellar tunnel.


