Abstract
Lateral ankle sprains are common; if conservative treatment fails and chronic instability develops, stabilization surgery is indicated. Numerous surgical procedures have been described, but those that most closely reproduce normal ankle lateral ligament anatomy and kinematics have been shown to have the best outcomes. Arthroscopy is a common adjunct to open ligament surgery, but it is traditionally only used to improve the diagnosis and the management of any associated intra-articular lesions. The stabilization itself is performed open because standard anterior ankle arthroscopy provides only partial visualization of the anterior talofibular ligament from above and the calcaneofibular ligament attachments cannot be seen at all. However, lateral ankle endoscopy can provide a view of this area that is superior to open surgery. We have developed a technique of ankle endoscopy that enables anatomic positioning of the repair or fixation of the graft. In this article we describe a safe and reproducible arthroscopic anatomic reconstruction of the lateral ligaments of the ankle using a gracilis autograft. The aim of this procedure is to obtain a more physiological reconstruction while maintaining all the advantages of an arthroscopic approach.
Ankle sprains involving the lateral ligament complex, particularly the anterior talofibular ligament (ATFL) and the calcaneofibular ligament (CFL), are common. Most patients recover after this injury with conservative treatment, with 10% to 40% progressing to chronic ankle instability requiring surgical stabilization.1 Historically, the Broström-Gould procedure, consisting of a midsubstance re-tensioning of the damaged ATFL and CFL with additional reinforcement, has been considered the gold standard procedure.2 However, anatomic reconstruction using a tendon graft is increasing in popularity.3
Although good results have been reported with both of the aforementioned surgical strategies, there is increasing interest in the use of arthroscopy to assist or to perform the stabilization.4 This technique may replace the open approaches that are currently performed.5 The goal of the arthroscopy is not only to improve the diagnosis and the management of associated intra-articular lesions but also to control the anatomic positioning of the repair/graft. Nonanatomic positioning of the graft over-constrains the ankle or subtalar joints and may alter the biomechanics of the articulation, resulting in joint degeneration over time.6 In addition, there has been controversy as to which patients need only ATFL reconstruction and which patients need both ATFL and CFL reconstruction. This article is the first to describe a safe and reproducible fully arthroscopic anatomic reconstruction of the lateral ligaments of the ankle using a gracilis autograft.
Surgical Technique
Four arthroscopic portals are needed: a classic anteromedial portal (portal 1) and anterolateral portal (portal 2), a sinus tarsi portal (portal 3), and a retromalleolar tendoscopic portal (portal 4) (Fig 1). Before the procedure is begun, it is recommended to mark portal 3. This portal is positioned at the level of the superior side of the peroneus brevis and at the posterior side of the extensor retinaculum.
Fig 1.

Landmarks and portals: anteromedial portal (portal 1), anterolateral portal (portal 2), sinus tarsi portal (portal 3), and retromalleolar tendoscopic portal (portal 4). It should be noted that portal 2 is made by transillumination.
A 4-mm 30° arthroscope is introduced through portal 1. The ankle is positioned in maximum dorsiflexion to obtain the optimal view of the lateral gutter (Fig 2). In this position, portal 2 is made by transillumination.
Fig 2.
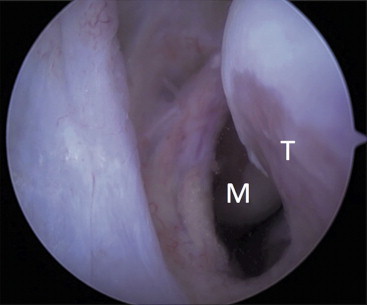
Arthroscopic view of lateral gutter before dissection. (M, malleolus; T, lateral side of talus.)
Anterior Ankle Arthroscopy and Anterolateral Ankle Dissection
Dissection with a shaver starts with debridement and visualization of the inferior part of the anterior tibiofibular ligament. The dissection continues distally by releasing the superior part of the ATFL from the malleolus to the talus. After this stage, the dissection continues outside the joint on the lateral side of the ATFL.
The dissection of this zone will end with the peel off of the talar footprint of the ATFL. This is wide and is located at the midpoint of the junction of the body and neck of the talus (demarcated by the edge of the cartilage). A guidewire is then introduced through portal 3 and positioned under a direct arthroscopic view on the prepared malleolar area. The direction of the guide pin is superior and posterior to reach the posterior cortex of the fibula 3 to 5 cm proximal and posterior to the distal tip. We then use a cannulated 4.5-mm drill from the anterior to the posterior cortex of the fibula. On the same guide pin, a 6-mm drill is used to enlarge the tunnel distally to a 1-cm depth. This part of the tunnel is the part dedicated to the transplant.
Lateral Ankle Endoscopy and Lateral Ankle Dissection
The next step requires dissection from the CFL to the ATFL to reach the preliminary dissection. The ankle is placed in the lateral position. A retromalleolar tendoscopic portal7 is made 1 cm from the tip of the lateral malleolus (portal 4) (Fig 3). The shaver is introduced through portal 3 under the control of the arthroscope in portal 4. Dissection starts at the superior side of the peroneus brevis just in front of its proper tunnel, clearing the tissue anterior to the CFL toward the sinus tarsi and along the lateral side of the subtalar joint (Fig 4).
Fig 3.

Retromalleolar tendoscopic visualization of peroneus brevis.
Fig 4.
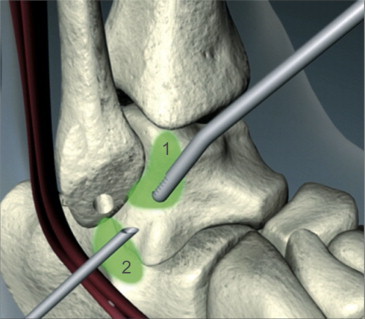
Arthroscopic and endoscopic dissection of lateral hindfoot: dissection from anterolateral arthroscopy (1) and dissection by tendoscopy and lateral endoscopy (2).
At this stage, it is possible to finish the dissection safely by positioning the arthroscope in portal 3 and the instruments in portal 2. A visual field from the fibular tunnel to the talar insertion of the ATFL is obtained. A 3-cm-deep 6-mm talar tunnel is prepared after localization of the footprint.
Preparation of CFL Calcaneal Insertion
The preparation continues with the arthroscope in portal 2 and the instruments in portal 3 to follow the CFL to its calcaneal insertion. A 3-cm-deep 6-mm tunnel is made at the calcaneal footprint.
Graft Insertion and Fixation
A gracilis autograft is prepared by use of a ZipLoop device (Biomet, Warsaw, IN) (Fig 5) to reconstruct the CFL and the ATFL. The arthroscope is then repositioned in portal 2, and the ZipLoop device is introduced into the fibular tunnel through portal 3. This pulls the graft into the expanded anterior part of the tunnel. The CFL graft is introduced into its tunnel and secured with an Organic-Core interference screw (Biomet) measuring 6 × 25 mm. A 1.4-mm JuggerKnot bone anchor (Biomet) is positioned at the base of the talar tunnel under arthroscopic control. One strand is sutured to the graft, and the other strand is used to pull the graft into the tunnel by using it as a pulley. An ALLthread LactoSorb anchor (Biomet) is used as an interference screw (Fig 6). These posts are sutured with the traction strand of the JuggerKnot device to reinforce fixation. It should be noted that manual tension is applied on the 2 grafts before final fixation with the ankle in the neutral position (Video 1, Table 1).
Fig 5.

Preparation of gracilis graft.
Fig 6.
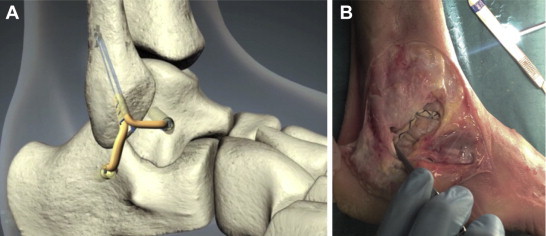
(A) Anatomic arthroscopic reconstruction with gracilis. (B) Cadaveric dissection after arthroscopic reconstruction.
Table 1.
Surgical Steps, Pearls, and Pitfalls
| Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Anterior ankle arthroscopy | The anteromedial portal is made in a position of dorsiflexion, and the arthroscope is placed to see the lateral gutter. | A lack of dorsiflexion will result in poor visualization of the lateral gutter. |
| Lateral gutter preparation | Everything between the AITFL and the ATFL has to be removed. | Inadequate clearance will make correct placement of the tunnel difficult. |
| Malleolar tunnel | The arthroscope is used in portal 2 and the instruments in portal 3. | Poor placement of portal 3 can result in misdirection of the malleolar tunnel. |
| Tendoscopy | The arthroscope is introduced in portal 4 and the instruments in portal 3. After good preparation, the arthroscope is switched to portal 3 and the instruments to portal 2. | It is important to identify the posterior tibiofibular ligament because this can be mistaken for the CFL. |
| Talar tunnel | The talar tunnel is placed at a point halfway up the anterior border of the lateral facet of the talus. | Care has to be taken to avoid the tunnel running into the subtalar joint. |
| Malleolar tunnel | The arthroscope is placed in portal 2 and the instruments in portal 3. | It is important not to miss the remnant fibers of the CFL. |
| Placement of calcaneal tunnel | The arthroscope is placed in portal 3 and the instruments in portal 2. | It is necessary to protect the peroneal structures from damage. |
| Position of transplant in malleolar tunnel | The arthroscope is in portal 2 and the transplant in portal 3. The surgeon pulls on the toggle-lock suture. | If the transplant is too large, it will not go sufficiently far into the 6-mm tunnel. |
| Placement of transplant in malleolar tunnel | Tension is made with the foot at 90°. | It is important to put the screw guide deep inside to yield good placement of the screw. |
| Placement of calcaneal end of transplant | Tension is made with the foot at 90°. | The surgeon uses a suture to maintain tension on the graft; otherwise, the CFL reconstruction will be too loose. |
| Placement of talar end of transplant | Tension is made with the foot at 90° by pulling on 1 post of the JuggerKnot anchor. The transplant is fixed in the tunnel by the screw. | It is important to maintain the tension on the JuggerKnot. If it is too weak, the surgeon instead can pass the guidewire through onto the medial side of the talus with a pulling suture linked to the transplant to draw it through to the correct tension. |
Discussion
Many surgical procedures have been developed for treating lateral ankle instability. These are typically classified as either anatomic or nonanatomic reconstruction techniques. Nonanatomic reconstruction techniques for the lateral ankle ligaments have been widely studied and have shown good efficacy in restoring stability of the hindfoot with good functional results.8 However, the long-term results show postoperative loss of range of motion, recurrence of instability, and an increased incidence of degenerative changes of the hindfoot.9 Maintenance of the full range of motion of the hindfoot has been shown to reduce the long-term risk of osteoarthritis and/or chronic pain.10 Therefore, according to these previous reports, anatomic reconstructive surgery should be preferred to restore the normal kinematics of the hindfoot and to maintain satisfactory long-term results.3,11
Ankle joint instability usually coexists with intra-articular symptoms. Mechanical joint instability results from deficient ATFL and/or CFL ligaments, and functional instability is caused by weakened proprioception. The intra-articular symptoms may be due to primary or secondary intra-articular lesions. With a high prevalence of intra-articular pathology, it is therefore recommended to perform an arthroscopy at the time of surgery. This allows surgeons to address the intra-articular lesions and the lateral instability concomitantly.
The benefits of an arthroscopic approach over an open approach have already been shown in other ankle conditions such as ankle fusion,12 cheilectomy, and debridement.13 Studies have shown that converting to an arthroscopic technique can be demanding, with a long learning curve and an increase in surgical time; however, the advantages of preserving the soft-tissue envelope and the improved visualization outweigh these issues.14 One can see an improved recovery, less pain, a lower rate of soft-tissue complications, and improved healing through better preservation of the blood supply.
Thus it seems logical to move toward an arthroscopic anatomic reconstruction of the ankle ligaments. The arthroscopy improves the management of associated intra-articular lesions and allows anatomic positioning of the graft. Recently, several arthroscopically assisted techniques have been described for lateral ankle ligament reconstruction.6,15-18 These techniques, which are technically demanding, have shown early promise in Level IV studies with short-term follow-up. They effectively replicate the Broström-Gould procedure and fail to achieve true anatomic reconstruction.7
In a recent cadaveric study, Drakos et al.18 showed that several anatomic structures lie in close proximity to the ATFL and CFL sutures during arthroscopic ankle stabilization. The proximity of the peroneus tertius and the extensor tendons to the ATFL makes them at highest risk of entrapment, in theory, and the proximity of the intermediate branch of the superficial peroneal nerve yields a high risk of significant morbidity. Therefore we believe that the combined arthroscopic and percutaneous techniques are at high risk of producing complications. Our technique, which starts with an arthroscopic intra-articular exploration followed by a progressive extra-articular cleaning of the lateral gutter, allows identification and preservation of all lateral structures including the superficial layer. By using a well-established arthroscopic portal that is located away from the anatomic structures at risk of damage, we did not observe any neurologic complications in our first 40 cases.
Soft-tissue complications (infection, wound dehiscence, and skin ulcer/blister) were reported significantly more in the foot and ankle when compared with other orthopaedic procedures.19 In addition, we believe that the use of only the arthroscopy might reduce these higher rates of complications.
The described procedure is technically demanding, but the most difficult step in the procedure is the lateral ankle endoscopic dissection, and cadaveric training is recommended. There are few structures at risk; in fact, it is only the peroneal tendons that are present in the operative field. However, these can be seen throughout the procedure and are easily avoided. The superficial peroneal nerve is also at risk, as it is during insertion of the anterolateral ankle portal during standard ankle arthroscopy. However, in this technique this portal needs to be made as far lateral as possible and slightly inferior so that it sits a little way down the lateral gutter and thus is likely to reduce the risk to the nerve.
We believe that further investigation and reporting of results are required before the described technique can be adopted as a standard procedure; however, in this series we have shown that the technique shows promise and that it is possible to reduce the period of immobilization and increase the rate of rehabilitation.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.G. receives support from Biomet. T.B. receives support from Arthrex. B.S.-C. receives support from Arthrex.
Supplementary Data
Anatomic arthroscopic reconstruction of lateral ligaments of ankle with gracilis autograft.
References
- 1.de Vries J.S., Krips R., Sierevelt I.N., Blankevoort L., van Dijk C.N. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011;8:CD004124. doi: 10.1002/14651858.CD004124.pub3. [DOI] [PubMed] [Google Scholar]
- 2.Messer T.M., Cummins C.A., Ahn J., Kelikian A.S. Outcome of the modified Broström procedure for chronic lateral ankle instability using suture anchors. Foot Ankle Int. 2000;21:996–1003. doi: 10.1177/107110070002101203. [DOI] [PubMed] [Google Scholar]
- 3.Takao M., Oae K., Uchio Y., Ochi M., Yamamoto H. Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: A new technique using an interference fit anchoring system. Am J Sports Med. 2005;33:814–823. doi: 10.1177/0363546504272688. [DOI] [PubMed] [Google Scholar]
- 4.Lui T.H. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23:554.e1–554.e5. doi: 10.1016/j.arthro.2006.07.038. www.arthroscopyjournal.org Available at. [DOI] [PubMed] [Google Scholar]
- 5.Espinosa N., Smerek J., Kadakia A.R., Myerson M.S. Operative management of ankle instability: Reconstruction with open and percutaneous methods. Foot Ankle Clin. 2006;11:547–565. doi: 10.1016/j.fcl.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Nery C., Raduan F., Del Buono A., Asaumi I.D., Cohen M., Maffulli N. Arthroscopic-assisted Broström-Gould for chronic ankle instability: A long-term follow-up. Am J Sports Med. 2011;39:2381–2388. doi: 10.1177/0363546511416069. [DOI] [PubMed] [Google Scholar]
- 7.Guillo S., Calder J.D. Treatment of recurring peroneal tendon subluxation in athletes: Endoscopic repair of the retinaculum. Foot Ankle Clin. 2013;18:293–300. doi: 10.1016/j.fcl.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Guillo S., Bauer T., Lee J.W. Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99:S411–S419. doi: 10.1016/j.otsr.2013.10.009. (suppl) [DOI] [PubMed] [Google Scholar]
- 9.Snook G.A., Chrisman O.D., Wilson T.C. Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am. 1985;67:1–7. [PubMed] [Google Scholar]
- 10.Schmidt R., Cordier E., Bertsch C. Reconstruction of the lateral ligaments: Do the anatomical procedures restore physiologic ankle kinematics? Foot Ankle Int. 2004;25:31–36. doi: 10.1177/107110070402500107. [DOI] [PubMed] [Google Scholar]
- 11.Neuschwander T.B., Indresano A.A., Hughes T.H., Smith B.W. Footprint of the lateral ligament complex of the ankle. Foot Ankle Int. 2013;34:582–586. doi: 10.1177/1071100712466851. [DOI] [PubMed] [Google Scholar]
- 12.Pakzad H., Thevendran G., Penner M.J., Qian H., Younger A. Factors associated with longer length of hospital stay after primary elective ankle surgery for end-stage ankle arthritis. J Bone Joint Surg Am. 2014;96:32–39. doi: 10.2106/JBJS.K.00834. [DOI] [PubMed] [Google Scholar]
- 13.Scranton P.E., McDermott J.E. Anterior tibiotalar spurs—A comparison of open versus arthroscopic debridement. Foot Ankle. 1992;13:125–129. doi: 10.1177/107110079201300303. [DOI] [PubMed] [Google Scholar]
- 14.Zwiers R., Wiegerinck J.L., Murawski C.D., Smyth N.A., Kennedy J.G., van Dijk C.N. Surgical treatment for posterior ankle impingement. Arthroscopy. 2013;29:1263–1270. doi: 10.1016/j.arthro.2013.01.029. [DOI] [PubMed] [Google Scholar]
- 15.Vega J., Golanó P., Pellegrino A., Rabat E., Peña F. All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot Ankle Int. 2013;34:1701–1709. doi: 10.1177/1071100713502322. [DOI] [PubMed] [Google Scholar]
- 16.Cottom J.M., Rigby R.B. The “all-inside” arthroscopic Broström procedure: A prospective study of 40 consecutive patients. J Foot Ankle Surg. 2013;52:568–574. doi: 10.1053/j.jfas.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 17.Giza E., Shin E.C., Wong S.E. Arthroscopic suture anchor repair of the lateral ligament ankle complex: A cadaveric study. Am J Sports Med. 2013;41:2567–2572. doi: 10.1177/0363546513500639. [DOI] [PubMed] [Google Scholar]
- 18.Drakos M., Behrens S.B., Mulcahey M.K., Paller D., Hoffman E., DiGiovanni C.W. Proximity of arthroscopic ankle stabilization procedures to surrounding structures: An anatomic study. Arthroscopy. 2013;29:1089–1094. doi: 10.1016/j.arthro.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 19.Hunter J, Olsen J, Digiovanni CW, Anglen J, Baumhauer JF. The most common patient safety problems in elective foot and ankle orthopaedic surgery. Presented at the American Academy of Orthopaedic Surgeons Annual Meeting, Chicago, IL, March 19-23, 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anatomic arthroscopic reconstruction of lateral ligaments of ankle with gracilis autograft.


