Abstract
Introduction
Our study primarily aimed at investigating the effect of isoproterenol infusion on tissue oxygen saturation in patients with septic shock. The secondary aim was to assess the relation between cardiac index, central venous oxygen saturation and tissue oxygen saturation.
Methods
This retrospective study was conducted from December 2010 to March 2012. We included 14 consecutive patients with septic shock treated with isoproterenol. All patients were monitored by cardiac index and tissue oxygen saturation. From medical charts, routine hemodynamic data were extracted one hour before and six hours after the onset of isoproterenol infusion.
Results
From baseline to H6, tissue oxygen saturation levels rise from 78 [72-82]% to 85 [78-88]% (p = 0.03). Isoproterenol infusion was associated with an increase of central venous oxygen saturation (from 67 [65-74]% to 84 [77-86]%, p = 0.02) and cardiac index (from 2.9 [2.7-3.1] L/min/m² to 3.9 [3.0-4.4] L/min/m², p = 0.006). Tissue oxygen saturation was correlated neither to cardiac index (p = 0.14, R2 = 0.08) nor to central venous oxygen saturation (p = 0.19, R2 = 0.10).
Conclusions
Use of isoproterenol was associated with an increase of tissue oxygen saturation. This increase was not correlated to cardiac index, suggesting a decoupling between macrocirculation and microcirculation.
Keywords: septic shock, isoproterenol, oxygen saturation, microcirculation
Introduction
Septic shock is characterized by an impairment of microcirculation with reduced capillary density and impaired blood flow [1,2,3].
Near-infrared spectroscopy is one of the technologies available for exploring microcirculation. This technology allows a noninvasive monitoring for vessels with a diameter of less than 1 mm. Near-infrared light (600-800 nm) easily crosses biologic tissues and is absorbed by hemoglobin, myoglobin, and oxidized cytochrome, as described in another study [4].
In septic shock, tissue oxygen saturation below 78% was associated with increased mortality [5]. Norepinephrine administration increases mean arterial pressure higher above 65 mmHg and it was associated with improved microcirculation variables [6]. The use of a positive inotrope resulted in conflicting findings. On the one hand, administration of dobutamine at a low dosage was associated with improved capillary perfusion [7] while, on the other hand, microcirculation was improved only in patients with severe hemodynamic disturbances [8]. Thus, it is unclear whether or not the effect was independent of macrocirculation. Isoproterenol is a synthetic catecholamine with only beta-adrenergic stimulating effects. In septic shock patients with myocardial dysfunction, isoproterenol was associated with improvement of hemodynamics and oxygen variables [9]. As isoproterenol is a more potent vasodilator than dobutamine [10], its use could be associated with changes of microcirculation. The first aim of our study was to investigate the effect of an infusion of isoproterenol on tissue oxygen saturation (StO2) in septic shock patients. The secondary aim was to assess the relation between cardiac index, central venous oxygen saturation (ScvO2) and StO2.
Methods
Patients. From December 2010 to March 2012, we conducted a retrospective study in a 15-bed intensive care unit (ICU) of a 968-bed university hospital (Hôpital Nord, Marseille, France). As it was an observational retrospective study, according to the French Legislation (articles L.1121-1 paragraph 1 and R1121-2, Public Health Code), neither informed consent nor approval of the ethics committee was needed to use routine data.
We retrospectively examined the medical charts of 81 patients with septic shock requiring isoproterenol. All patients admitted for septic shock were treated according to the Surviving Sepsis Guidelines 2008, excepting for the use of positive inotrope agent [11]. The initial fluid therapy was guided by dynamic preload indices. Norepinephrine infusion was targeted to achieve at least mean arterial pressure of 65 mmHg and urine output over 0.5 mL/kg/h. Heart rate, mean arterial pressure, pulse oximetry, and end-tidal carbon dioxide were continuously measured (Patient monitor Intellivue MP 70; Philips, Andover MA). All mechanically ventilated patients were sedated with midazolam and sufentanil to target a Ramsay score between 2 and 3.
In our ICU, isoproterenol was administered instead of dobutamine, to patients in septic shock with myocardial dysfunction [9]. Dobutamine is recommended as the agent of choice to increase cardiac output [11]. However, mechanisms of cardiac depression in septic shock patients are unrelated to myocardial hypoperfusion, or coronary vessels obstruction. Thus, isoproterenol is possibly an alternative to dobutamine for the treatment of sepsis-induced myocardial depression in septic shock patients. In a previous study we showed that infusion of isoproterenol in septic shock patients was safe [9].
The indication was based on a cardiac index below 3 L/min/m² or ScvO2 below 70%, despite adequate fluid volume, arterial oxygen saturation (SaO2 >95%), hemoglobin (Hb >10 g/dL), and lack of agitation (Ramsay score between 2 and 3). In routine, a transthoracic echocardiography was performed in all patients in order to confirm the myocardial dysfunction (data not shown). At the discretion of the senior physician, isoproterenol was used in patients with ongoing signs of hypoperfusion despite adequate resuscitation. Isoproterenol was introduced at an initial rate of 0.04 µg/kg/min and increased by 0.01 µg/kg/min according to the cardiac index and ScvO2 responses (with a maximal dose of 0.15 µg/kg/min). All patients had an arterial catheter and a central venous catheter placed through internal jugular vein. ScvO2 was measured by sampling blood from the distal port of the catheter.
Among the 81 patients requiring isoproterenol, we selected the 45 patients equipped with a semi-invasive hemodynamic monitoring (Picco-Plus monitor, Pulsion Medical Systems, Munich, Germany). Next, we included the 14 consecutive patients where the tissue oxygen saturation was monitored by using a tissue spectrometer (InSpectra Model 325; Hutchinson Technology, Hutchinson, MN). The near-infrared spectroscopy probe was placed on clean skin of the thenar eminence. After a 3-min period to stabilize the near-infrared spectroscopy signal, the value of StO2 was recorded. We used probe spacing of 15 mm. A light-scattering calibrator was used to normalize the tissue spectrometer during startup of the system and before each measurement. Sample measurement signals were updated every 3.5 s. In our unit, this monitoring was routinely used in patients with refractory shock, at the discretion of senior physicians.
Data collection. Demographic and clinical data were collected from the medical charts. Hemodynamic data were extracted from medical charts. The following variables were collected: heart rate, mean arterial pressure, ScvO2, StO2, urine output, SaO2, norepinephrine dosages, and positive end-expiratory pressure. In our charts, we extracted data one hour before and six hours after the onset of isoproterenol infusion (collection period).
Statistics. We performed a descriptive analysis of the data and presented quantitative variables as median and interquartile range (IQR), and qualitative data as absolute counts and percentages. Differences were assessed using the appropriate statistical tests (Wilcoxon rank sum test for quantitative variables, and Fisher Test for qualitative variables). All comparisons were two-tailed and a p value < 0.05 was required to exclude the null hypothesis.
Results
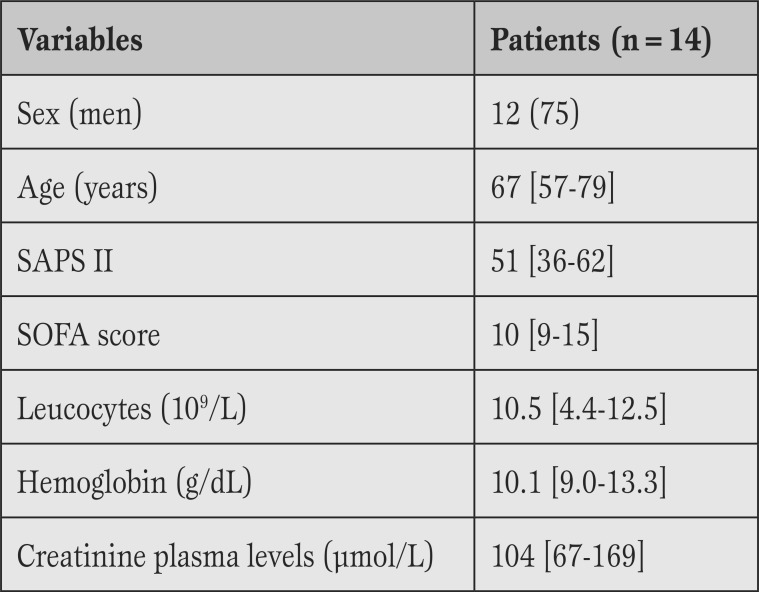
Among the 14 included patients, the ICU mortality rate was 64%. The leading causes of septic shock were pneumonia (n=6) and intra-abdominal infection (n=5). Demographic data and severity scores are shown in Table 1. Three patients (21%) required renal replacement therapy.
On the day of isoproterenol infusion, the median creatinine plasma concentration was 104 [67-169] µmol/L, and the median hemoglobin was 10.1 [9.0-13.3] g/dL (Table 1).
Table 1.
Baseline characteristics of the patients.
SAPS II=Simplified Acute Physiological Score II (measured at the unit admission); SOFA=Sequential Organ Failure Assessment (measured at the introduction of isoproterenol). Data are presented as absolute counts (percentages) or median [IQR].
The median isoproterenol dose was 0.05 [0.035-0.12] µg/kg/min. All patients survived more than 24 h after the onset of isoproterenol infusion. One patient had an atrial fibrillation in the hour after isoproterenol onset. He was successfully treated with amiodarone.
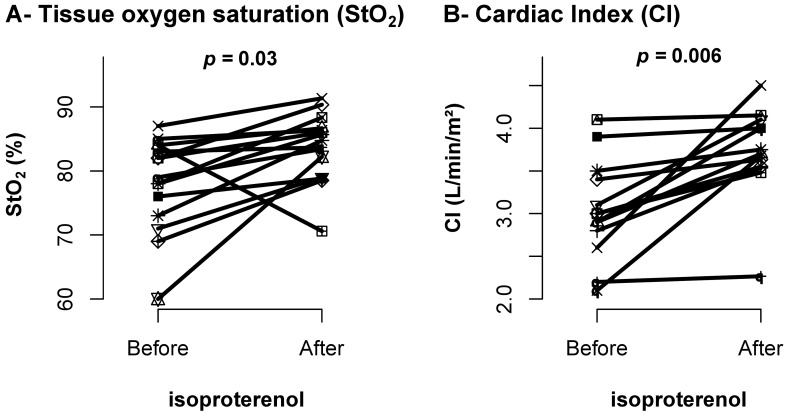
During the collection period, StO2 levels rise from 78 [72-82]% to 85 [78-88]% (p=0.03) (Figure 1A). The baseline StO2 level was below 75% in six (43%) patients. In these patients, the median StO2 levels increased by 9.5%. In contrast, StO2 increased only by 2% in the eight (57%) patients with baseline StO2 levels above 75%.
Isoproterenol administration was associated with cardiac index (2.9 [2.7-3.1] L/min/m² vs. 3.9 [3.0-4.4] L/min/m²; p = 0.006) (Figure 1B) and ScvO2 (67 [65-74]% to 84 [77-86]%; p=0.02) increase.
Figure 1.
Microcirculatory and systemic changes before and after onset of isoproterenol. A: Oxygen tissue saturation (StO2) at baseline (before) and H6 (after). B: Cardiac index (CI) at baseline (before) and H6 (after).
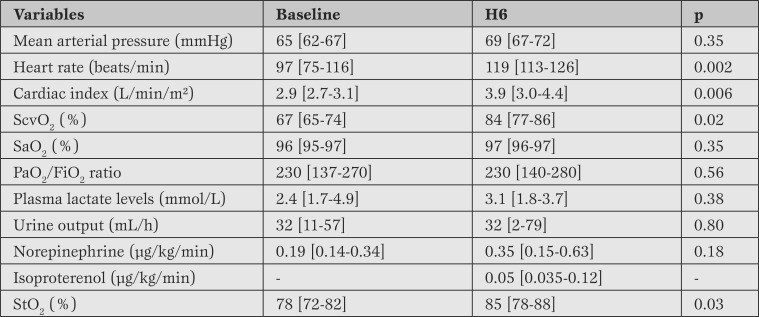
Heart rate increased from 97 [75-116] beats/min to 119 [113-126] beats/min (p=0.002). Mean arterial pressure, norepinephrine infusion rate, SaO2, and positive expiratory pressure remained unchanged before and after isoproterenol infusion (Table 2).
Table 2.
Hemodynamic and respiratory variables before and after (6h) isoproterenol infusion.
Results are expressed as median and interquartile.
StO2 = oxygen tissue saturation; ScvO2 = central venous oxygen saturation; SaO2 = oxygen arterial saturation PaO2/FiO2: = oxygen arterial pressure/inspired fraction of oxygen ratio.
In order to discriminate the systemic effect and the local effect of isoproterenol on microcirculation, a correlation was searched between StO2 and cardiac index as well as StO2 and ScvO2. There was no correlation with cardiac index (p=0.14, R²=0.08) and ScvO2 (p=0.19, R²=0.10). The baseline StO2 level and its variation did not differ between survivors and non-survivors.
Discussion
In the present study, we showed that infusion of isoproterenol in patient with septic shock was associated with an improvement of microcirculation. Due to the lack of correlation between cardiac index, ScvO2 and StO2, our findings suggest that microcirculation and macrocirculation were decoupled in those patients.
In septic shock, the goal of positive inotrope administration is to correct the unbalance between oxygen delivery and oxygen consumption. In our study, we confirmed that isoproterenol is efficient to improve hemodynamic parameters [9]. An atrial fibrillation requiring amiodarone occurred in only one patient. This rate (7.1%) is similar to what was reported in a large cohort of patients with septic shock [12]. Although isoproterenol was not associated with an excess of arrhythmia, the heart rate increase is a side effect that deserves to be considered, with regard to the recent findings about heart rate control in septic shock [13].
Microcirculation is partially dependent of systemic hemodynamics. In a previous study, correction of mean arterial pressure with increasing dose of norepinephrine was associated with improvement of StO2 [6]. Here, despite a mean arterial pressure above 65 mmHg, ScvO2 or peripheral perfusion was still considered as inadequate. This justified the introduction of isoproterenol. This treatment was associated with an increase of StO2. Hence, microvascular vessels were probably recruited with improvement in microcirculation, effect that can be related to a systemic mechanism: the increase in cardiac index. However, as reported elsewhere,cardiac index was not correlated to StO2 [5, 12]. This finding suggests a peripheral misuse of oxygen, as reported elsewhere [3]. Plasma lactate level also tended to increase during the study period, fact that may be partly related to reperfusion.
Previous studies underlined that dobutamine acts on microcirculation independently of its systemic effect [7]. Moreover, the vasodilatory effect of isoproterenol can have a key role in the microcirculation recruitment, as isoproterenol exerts effects on both beta-1- and beta-2-adrenergic stimulating receptors. Compared with dobutamine, its potent effect on beta-2 adrenergic receptors confers a theoretical advantage in terms of microcirculation recruitment [14]. Thus, isoproterenol possibly acts on microcirculation independently of the systemic response.
Regarding microcirculation, there is a need to compare the different positive inotropes. A randomized clinical trial showed that infusion of levosimendan was more efficient than that of dobutamine in order to improve sublingual microcirculatory blood flow [15]. Our findings suggest that future studies should compare isoproterenol to other inotropes.
Our study has several limitations. First, as it is an observational study, a time effect cannot be excluded. However, it would be surprising that the correction of myocardial dysfunction occurred in all patients during the study period. Second, the mortality rate is high. Nevertheless, it is similar to previous studies [9, 13]. Third, the number of patients is small. For this reason, we did not exclude the patients requiring renal replacement therapy. This heterogeneity may have affected the results. Fourth, fluid responsiveness of our patients was assessed using dynamic indices. According to a recent study [16], only 2% of patients admitted to ICU can be evaluated with dynamic indices of fluid responsiveness for hemodynamic status according to the inclusion and exclusion criteria. This is probably a limitation. In routine, we measured dynamic indices in patients fulfilling nearly all required conditions. One can note that only 45 (55%) out of 81 patients treated with isoproterenol were equipped with a monitor measuring dynamic indices. Fifth, we did not perform a vascular occlusion test, as reported in several publications [17,18,19]. The vascular occlusion test serves to assess little changes at the level of microvessel reactivity. However, in the present study, the use of isoproterenol was associated with significant change in the absolute value of StO2.
Conclusion
In our septic shock patients, isoproterenol infusion was associated with an enhancement of both StO2 and cardiac index. The microcirculation recruitment may result from an increase in oxygen delivery, but also from a direct effect of isoproterenol. Future clinical trials are required to confirm these retrospective findings.
Footnotes
Source of Support Nil.
Disclosures None declared.
Cite as: Wiramus S, Textoris J, Bardin R, Vigne C, Kelway C, Martin C, Leone M. Isoproterenol infusion and microcirculation in septic shock. Heart, Lung and Vessels. 2014; 6(4): 274-279
References
- De Backer D, Creteur J, Preiser J C, Dubois M J, Vincent J L. Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med. 2002;166:98–104. doi: 10.1164/rccm.200109-016oc. [DOI] [PubMed] [Google Scholar]
- Ellis C G, Jagger J, Sharpe M. The microcirculation as a functional system. Crit Care. 2005;9:3–8. doi: 10.1186/cc3751. [(Suppl 4)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis C, Bateman R M, Sharpe M D, Sibbald W J, Gill R. Effect of a maldistribution of microvascular blood flow on capillary O2 extraction in sepsis. Am J Physiol Heart Circ Physiol. 2002;282:156–164. doi: 10.1152/ajpheart.2002.282.1.H156. [DOI] [PubMed] [Google Scholar]
- Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent J L. The prognostic value of muscle StO2 in septic patients. Intensive Care Med. 2007;33:1549–1556. doi: 10.1007/s00134-007-0739-3. [DOI] [PubMed] [Google Scholar]
- Leone M, Blidi S, Antonini F, Meyssignac B, Bordon S, Garcin F. et al. Oxygen tissue saturation is lower in nonsurvivors than in survivors after early resuscitation of septic shock. Anesthesiology. 2009;111:366–371. doi: 10.1097/ALN.0b013e3181aae72d. [DOI] [PubMed] [Google Scholar]
- Georger J F, Hamzaoui O, Chaari A, Maizel J, Richard C, Teboul J L. Restoring arterial pressure with norepinephrine improves muscle tissue oxygenation assessed by near-infrared spectroscopy in severely hypotensive septic patients. Intensive Care Med. 2010;36:1882–1889. doi: 10.1007/s00134-010-2013-3. [DOI] [PubMed] [Google Scholar]
- De Backer D, Creteur J, Dubois M J, Sakr Y, Koch M, Verdant C. et al. The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med. 2006;34:403–408. doi: 10.1097/01.ccm.0000198107.61493.5a. [DOI] [PubMed] [Google Scholar]
- Enrico C, Kanoore Edul V S, Vazquez A R, Pein M C, Pérez de la Hoz R A, Ince C. et al. Systemic and microcirculatory effects of dobutamine in patients with septic shock. J Crit Care. 2012;27:630–638. doi: 10.1016/j.jcrc.2012.08.002. [DOI] [PubMed] [Google Scholar]
- Leone M, Boyadjiev I, Boulos E, Antonini F, Visintini P, Albanèse J. et al. A reappraisal of isoproterenol in goal-directed therapy of septic shock. Shock. 2006;26:353–357. doi: 10.1097/01.shk.0000226345.55657.66. [DOI] [PubMed] [Google Scholar]
- Dellinger R P, Levy M M, Carlet J M, Bion J, Parker M M, Jaeschke R. et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- Meierhenrich R, Steinhilber E, Eggermann C, Weiss M, Voglic S, Bögelein D. et al. Incidence and prognostic impact of new-onset atrial fibrillation in patients with septic shock: a prospective observational study. Crit Care. 2010;14:108–108. doi: 10.1186/cc9057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozina H, Podbregar M. Near-infrared spectroscopy during stagnant ischemia estimates central venous oxygen saturation and mixed venous oxygen saturation discrepancy in patients with severe left heart failure and additional sepsis/septic shock. Crit Care. 2010;14:42–42. doi: 10.1186/cc8929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morelli A, Ertmer C, Westphal M, Rehberg S, Kampmeier T, Ligges S. et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA. 2013;310:1683–1691. doi: 10.1001/jama.2013.278477. [DOI] [PubMed] [Google Scholar]
- Leone M, Albanèse J, Martin C. Positive inotropic stimulation. Curr Opin Crit Care. 2002;8:395–403. doi: 10.1097/00075198-200210000-00005. [DOI] [PubMed] [Google Scholar]
- Morelli A, Donati A, Ertmer C, Rehberg S, Lange M, Orecchioni A. et al. Levosimendan for resuscitating the microcirculation in patients with septic shock: a randomized controlled study. Crit Care. 2010;14:232–232. doi: 10.1186/cc9387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahjoub Y, Lejeune V, Muller L, Perbet S, Zieleskiewicz L, Bart F. et al. Evaluation of pulse pressure variation validity criteria in critically ill patients: a prospective observational multicentre point-prevalence study. Br J Anaesth. 2014;112:681–685. doi: 10.1093/bja/aet442. [DOI] [PubMed] [Google Scholar]
- Payen D, Luengo C, Heyer L, Resche-Rigon M, Kerever S, Damoisel C. et al. Is thenar tissue hemoglobin oxygen saturation in septic shock related to macrohemodynamic variables and outcome? Crit Care. 2009;13:6–6. doi: 10.1186/cc8004. [(Suppl 5)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezemer R, Lima A, Myers D, Klijn E, Heger M, Goedhart P T. et al. Assessment of tissue oxygen saturation during a vascular occlusion test using near-infrared spectroscopy: the role of probe spacing and measurement site studied in healthy volunteers. Crit Care. 2009;13:4–4. doi: 10.1186/cc8002. [(Suppl 5)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez H, Mesquida J, Simon P, Kim H K, Puyana J C, Ince C. et al. Characterization of tissue oxygen saturation and the vascular occlusion test: influence of measurement sites, probe sizes and deflation thresholds. Crit Care. 2009;13:3–3. doi: 10.1186/cc8001. [(Suppl 5)] [DOI] [PMC free article] [PubMed] [Google Scholar]