Abstract
Background
When a hospitalized older patient falls or develops delirium, there are significant consequences for the patient and the health care system. Assessments of inattention and altered consciousness, markers for delirium, were analyzed to determine if they were also associated with falls.
Methods
This retrospective case-control study from a regional tertiary Veterans Affairs referral center identified falls and delirium risk factors from quality databases from 2010 to 2012. Older fallers with complete delirium risk assessments prior to falling were identified. As a control, non-fallers were matched at a 3:1 ratio. Admission risk factors that were compared in fallers and non-fallers included altered consciousness, cognitive performance, attention, sensory deficits, and dehydration. Odds ratio (OR) was reported (95% confidence interval [CI]).
Results
After identifying 67 fallers, the control population (n=201) was matched on age (74.4±9.8 years) and ward (83.6% medical; 16.4% intensive care unit). Inattention as assessed by the Months of the Year Backward test was more common in fallers (67.2% versus 50.8%, OR=2.0; 95% CI: 1.1–3.7). Fallers tended to have altered consciousness prior to falling (28.4% versus 12.4%, OR=2.8; 95% CI: 1.3–5.8).
Conclusion
In this case-control study, alterations in consciousness and inattention, assessed prior to falling, were more common in patients who fell. Brief assessments of consciousness and attention should be considered for inclusion in fall prediction.
Keywords: geriatrics, patient centered outcomes research, patient safety
Background and objective
Inpatient hospital falls negatively impact patient health and are costly to the health care system. Patients who fall while in the hospital have greater rates of mortality,1 longer lengths of stay,2–4 decreased quality of life,3 and increased discharge rates to nursing homes.3 Of these patients who fall, approximately 4.6%–8.0% will incur a moderate to severe injury that further worsens outcomes.2,5–7 Overall, inpatients who fall cost more than those who do not,8 with injured fall patients incurring up to three times the expense.2,5
Considering the costs of falls to patients and hospitals, fall-reduction strategies have become widespread.8–10 While initial success has been documented, maintaining reduced fall rates over time remains a struggle.11 Fall reduction programs require effort targeted at patients who may be at higher risk. A diagnosis of delirium, an acute change in attention and mental status, appears to increase fall risk by up to six times12 and almost half (45%–48%) of all patients who fall are documented as being confused the day of the incident.2,7 Yet, key risk factors for delirium – inattention and altered consciousness – are not adequately or efficiently assessed in many fall-prediction rules.13–15
Delirium and falls share other similar risk factors, including advanced age, cognitive impairment, and polypharmacy.3,16–22 Several prospective studies demonstrate a relationship between delirium and falls;14,15,23 however, there is minimal research on the relationship between clinically applicable brief cognitive screens for delirium (on inattention and altered consciousness) and fall-risk detection. This secondary, case-control analysis of data from a quality improvement project was undertaken to determine if the assessment of inattention and altered consciousness, which are markers for delirium, were also associated with falls. We hypothesized that brief screening for inattention and altered consciousness would be associated with falls.
Design
To determine how inattention and altered consciousness may differ in fallers and a matched control, a retrospective case-control analysis was performed using data from two quality improvement projects. The falls were identified from an ongoing fall-reduction program. The delirium risk assessments were obtained from a delirium risk modification program. Patients who fell and had completed a delirium risk assessment prior to the fall were included. Controls were matched at a 3:1 ratio using age and level of inpatient care (intensive care unit [ICU] versus non-ICU). Age was selected as a matching factor, because it is related but not causative to both delirium and falls. Inpatient care level was selected as a matching factor because nurse-to-patient ratios and illness severity vary between ICU and non-ICU patients. This secondary analysis of quality improvement data was reviewed and approved for dissemination by the VA Boston Institutional Review Board.
Participants
These projects were conducted at the VA Boston Healthcare System (VABHS), West Roxbury campus, Boston, MA, USA, in the 125-bed tertiary referral Veterans Affairs hospital for New England. The VABHS has been actively tracking and improving fall-related processes. All falls are reviewed and classified according to fall type and related injury. Feedback is provided to medical staff and wards. Fall-reduction program outcomes are reported to leadership. In October 2010, the VABHS began a delirium risk modification program.24 Patients aged 60 years or older and admitted to medical wards were briefly interviewed and provided appropriate interventions to modify delirium risk. Patients were not approached if they were admitted for observational purposes or 48 hours had passed since admission.
Main measures
Falls were reported as they occurred by nursing staff on incident reports. The nursing staff was responsible for categorizing the fall into one of three groups: accidental, unanticipated, or anticipated. An accidental fall is an unexpected slip caused by something in the environment (eg, cords, clutter, spills on the floor).25 An unanticipated fall is caused by undocumented patient conditions such as neurological issues or physical weakness (eg, stroke or heart attack), and therefore cannot be predicted or prevented.25 In contrast, an anticipated fall can be predicted through an examination of patient characteristics (eg, impaired vision or cognition), making it preventable.25 Nursing staff recorded the type of injuries incurred during a fall (eg, abrasions, lacerations, contusions).
Delirium risk assessment
Delirium risk factors were collected during inpatient assessments as part of the delirium risk modification program. Documented risk factors included: inattention, sensory impairment, and an elevated blood urea nitrogen/creatinine ratio. Inattention was assessed using Months of the Year Backward (MOYB), Days of the Week Backward (DOWB), and the Clock-in-the-Box (CIB) tests. The MOYB and DOWB were scored separately as either correct or incorrect. On the CIB, patients could receive 0–8 points (0= worst). An incorrect response on the MOYB, the DOWB, or a score of <4 on the CIB was indicative of cognitive difficulty.26 Those unable to read the instructions of the CIB, or who reported difficulty with vision (and did not have access to corrective eyewear) were considered to be visually impaired. Blood urea nitrogen and creatinine levels were extracted from the medical record as a measure of dehydration (blood urea nitrogen/creatinine >18.0).
Altered consciousness was also measured during inpatient assessments using the modified Richmond Agitation and Sedation Scale (mRASS), a text modification for less acutely ill patients. The mRASS asks an open-ended question followed by observation for 10 seconds and completion of a −5 to +4 rating scale. Alert and calm (mRASS =0) is considered normal, and positive numbers refer to hypervigilant states, while negative numbers denote levels of sedation. Previous research identified that abnormal mRASS was associated with delirium, particularly when administered longitudinally.26
Data analysis
After matching, within-group comparisons were performed between patients who did not fall and those who fell. After examining descriptive statistics, an OR (95% CI) was calculated. Further comparisons were conducted between anticipated fallers and their matches. Injury was treated as an ordinal variable, and an analysis of variance was performed. STATA SE version 11.0 (StataCorp LP, College Station, TX, USA) was used for all analyses.
Key results
From October 2010 to September 2012, over 4,500 patients participated in the delirium risk modification program. During this time, 198 first-time falls occurred on medical wards participating in the program (Figure 1). Delirium risk assessments were completed in 116 of the patients who fell. Of these, 43 delirium risk assessments collected from patients after the fall and six patients with accidental falls were excluded. This resulted in a total of 67 fall cases that were matched with 201 control cases by age and level of care. Fifty-six of the falls were anticipated, so further comparisons were possible between these fallers and their 168 matches.
Figure 1.
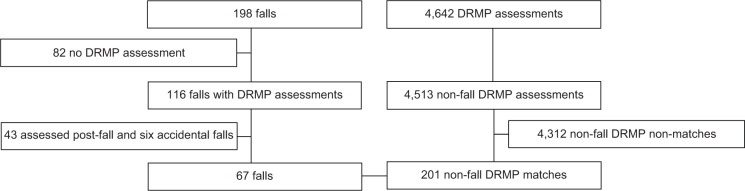
Selection of fallers and matched non-fallers.
Notes: The fall and DRMP databases were merged. DRMP patients screened post-fall and accidental fallers were excluded because the population characteristics differ. The left side of the figure shows the fallers who participated in the DRMP. The right side shows non-fallers who participated in the DRMP. Horizontal lines indicate groups that were excluded from analysis. Vertical lines indicate groups that were kept in the pool at each stage. The horizontal line between the bottom two squares represents the fallers in the DRMP and the non-fallers in the DRMP who were matched at a rate of 3:1.
Abbreviation: DRMP, delirium risk modification program.
Fallers were matched with non-fallers on age (74.4±9.8 years) and ward type (16.4% ICU and 83.6% non-ICU). Consistent with the Veterans Affairs (VA) population, 100% of the fall group and 99.0% of the matched sample was male. As detailed in Table 1, patients who fell were more likely to perform poorly on cognitive assessments of attention (73.1% versus 61.2% [OR=1.7; 95% CI: 0.9–3.4]) and tended to have abnormal mRASS assessments (28.4% versus 12.4% [OR=2.8; 95% CI: 1.3–5.8]) relative to non-fallers. Of the cognitive assessments measuring attention, fallers were more likely to get the MOYB incorrect (67.2% versus 50.8% [OR=2.0; 95% CI: 1.1–3.7]), the DOWB incorrect (28.1% versus 13.2% [OR=2.6; 95% CI: 1.2–5.4]), or to score in the impaired range on the CIB (49.1% versus 39.4% [OR=1.5; 95% CI: 0.8–2.7]). The CIs for the delirium risk factors of vision (CI: 0.5–1.6) and dehydration (CI: 0.6–2.0) demonstrated no significant difference.
Table 1.
Delirium risk factors in falls versus non-falls
| No-fall control % (n) (N=201) | Fall % (n) (N=67) | Odds ratio* 95% confidence interval | |
|---|---|---|---|
| Characteristics | |||
| Age | 74.4 (9.8) | 74.4 (9.8) | N/A |
| Male | 99.0 (199) | 100.0 (67) | N/A |
| Ward (non-ICU) | 83.6 (168) | 83.6 (56) | N/A |
| Altered consciousness | |||
| Abnormal mRASS | 12.4 (25) | 28.4 (19) | 2.8 (1.3–5.8) |
| Delirium risk factors | |||
| Impaired cognitive performance | 61.2 (123) | 73.1 (49) | 1.7 (0.9–3.4) |
| CIB abnormal‡ | 39.4 (61/155) | 49.1 (28/57) | 1.5 (0.8–2.7) |
| MOYB incorrect | 50.8 (102) | 67.2 (45) | 2.0 (1.1–3.7) |
| DOWB incorrect‖ | 13.2 (25/189) | 28.1 (18) | 2.6 (1.2–5.4) |
| Sensory impairment | |||
| Vision deficit | 35.8 (72) | 32.8 (22) | 0.9 (0.5–1.6) |
| Dehydration | |||
| BUN/CR >18 | 62.2 (125) | 64.2 (43) | 1.1 (0.6–2.0) |
Notes:
Odds ratio between no-fall control group and fall group.
Missing 46 from the no-fall control and ten from the fall group.
Missing nine from the no-fall control group and three from the fall group. Due to the qualitative nature of the study, the CIB and DOWB were not collected on all patients.
Abbreviations: BUN/CR, blood urea nitrogen/creatinine; CIB, Clock-in-the-Box; DOWB, Days of the Week Backward; ICU, intensive care unit; MOYB, Months of the Year Backward; mRASS, modified Richmond Agitation and Sedation Scale; N/A, not applicable.
Table 2 describes the comparison of anticipated fallers versus non-fallers. Anticipated fallers, relative to non-fallers, were more likely to demonstrate poor cognitive performance on measures of attention (75.0% versus 60.1% [OR=2.0; 95% CI: 1.0–4.3]) and to have an abnormal mRASS (32.1% versus 10.1% [OR=4.2; 95% CI: 1.8–9.5]). In comparison to non-fallers, they were more likely to score in the impaired range on the CIB (50.0% versus 38.9% [OR=1.6; 95% CI: 0.8–3.3]). Vision deficits and dehydration did not significantly differ between anticipated fallers and those without falls. Table 3 shows a significant association between mRASS, CIB, MOYB, and fall injury.
Table 2.
Delirium risk factors in anticipated fall predictability
| Anticipated no-fall matches % (n) (N=168) | Anticipated falls % (n) (N=56) | Anticipated OR* 95% confidence interval | |
|---|---|---|---|
| Altered consciousness | |||
| Abnormal mRASS | 10.1 (17) | 32.1 (18) | 4.2 (1.8–9.5) |
| Delirium risk factors | |||
| Impaired cognitive performance | 60.1 (101) | 75.0 (42) | 2.0 (1.0–4.3) |
| CIB abnormal§ | 38.9 (49/126) | 50.0 (23/46) | 1.6 (0.8–3.3) |
| MOYB incorrect | 50.6 (85) | 69.6 (39) | 2.2 (1.1–4.6) |
| DOWB incorrect¶ | 13.4 (21/157) | 29.6 (16/54) | 2.7 (1.2–6.1) |
| Sensory impairment | |||
| Vision deficit | 36.3 (61) | 37.5 (21) | 1.1 (0.5–2.1) |
| Dehydration | |||
| BUN/CR >18 | 63.1 (106) | 62.5 (35) | 1.0 (0.5–1.9) |
Notes:
Odds ratio between no-fall matches and anticipated fallers.
Missing 46 from the no-fall control, ten from the anticipated fall group, and zero from the unanticipated fall group.
Missing nine from the no-fall control, two from the anticipated fall group, and one from the unanticipated fall group. Due to the qualitative nature of the study, the CIB and DOWB were not collected on all patients.
Abbreviations: BUN/CR, blood urea nitrogen/creatinine; CIB, Clock-in-the-Box; DOWB, Days of the Week Backward; MOYB, Months of the Year Backward; mRASS, modified Richmond Agitation and Sedation Scale; OR, odds ratio.
Table 3.
Delirium risk factors in fall result
| No-fall matches % (n) (N=201) | No injury % (n) (N=48) | Injury % (n) (N=19) | P-value* | |
|---|---|---|---|---|
| Altered consciousness | ||||
| Abnormal mRASS | 12.4 (25) | 22.9 (11) | 42.1 (8) | <0.01 |
| Delirium risk factors | ||||
| Impaired cognitive performance | 61.2 (123) | 75.0 (36) | 68.4 (13) | 0.19 |
| CIB abnormal‡ | 39.4 (61/155) | 52.6 (20) | 42.1 (8) | 0.33 |
| MOYB incorrect | 50.8 (102) | 66.7 (32) | 68.4 (13) | 0.06 |
| DOWB incorrect‖ | 13.2 (25/189) | 26.1 (12) | 33.3 (6) | 0.02 |
| Sensory impairment | ||||
| Vision deficit | 35.8 (72) | 31.3 (15) | 36.8 (7) | 0.83 |
| Dehydration | ||||
| BUN/CR >18 | 62.2 (125) | 56.3 (27) | 84.2 (16) | 0.10 |
Notes:
P-value between no-fall matches no-injury falls and injury-falls.
Missing 46 from the no-fall control, ten from the no injury group, and zero from the injury group.
Missing nine from the no-fall control, two from the no injury group, and one from the injury group. Due to the qualitative nature of the study, the CIB and DOWB were not collected on all patients.
Abbreviations: BUN/CR, blood urea nitrogen/creatinine; CIB, Clock-in-the-Box; DOWB, Days of the Week Backward; MOYB, Months of the Year Backward; mRASS, modified Richmond Agitation and Sedation Scale.
Discussion
This case-control study found that inattention (as measured by the MOYB and DOWB) and altered consciousness (assessed by the mRASS) prior to falling were associated with falls. Clinically, brief assessments of inattention and consciousness performed upon admission may contribute to identification of patients who are at risk of falls and delirium. Since both delirium and falls result in negative health outcomes for patients and increased costs for health care systems, there is a strong incentive to utilize brief assessments of attention and mental status. This is consistent with previous research which shows that incident delirium increases risk of falling.12
Recent systematic reviews demonstrated that multicomponent fall-27 and delirium-prevention28 programs were effective. There is substantial overlap between fall and delirium prevention with improving cognitive stimulation, sensory input, and ambulation. Identification of risk is a critical first step for both fall and delirium prevention programs. Thus, our finding of the association between poor cognitive performance on brief assessments of attention and falls has face validity, as well as clinical applicability.
Current fall risk assessments, such as the Morse Scale,29 the Hendrich II Fall Risk Model,15 and STRATIFY,14 do not include assessments of attention. A fall-prediction scale which includes clinically applicable brief assessments of attention as well as consciousness could potentially benefit performance.
Time is a critical commodity on an inpatient ward. The value of additional assessments must be weighed. The assessments of consciousness (mRASS) and attention (DOWB or MOYB) utilized in this analysis are brief. The mRASS, a measure of consciousness, is completed in <15 seconds. DOWB/MOYB, measures of attention, each require about a minute. CIB requires 2–3 minutes.30 However, the knowledge gained with these brief assessments represents an opportunity to inform delirium and fall risk. The Richmond Agitation and Sedation Scale and the MOYB are already core components of a delirium assessment tool entitled the Brief Confusion Assessment Method,31 so further validation could result in availability of the mRASS and MOYB for widespread clinical adaptation.
Strengths
This study combined two quality improvement databases to examine the relationship between clinically applicable brief cognitive screens of attention and altered mental status and falls. Due to the large size of the delirium risk modification program, it was possible to match patients on age and ward at a ratio of 3:1, providing a good control group.
Limitations
This research is limited by generalizability. All subjects were from a VA hospital which resulted in an overrepresentation of males due to the nature of the VA population. In the future, it may be beneficial to replicate this study with more female participants. While women are less likely to die from a fall,22 these falls are more costly, as women are more likely to have an osteoporotic fracture.22 Additionally, due to the quality improvement project data source, this study would have benefitted from more systematic and comprehensive data collection including measures of disease comorbidity and severity of illness. Lastly, formal delirium assessments would allow health care providers to consistently monitor the delirium status of patients.
Conclusion
This study found that poor performance on measures of attention and mental status, which are markers for delirium, are associated with falls. Thus, introduction of brief screening for consciousness and attention may have benefit for both fall- and delirium-prevention programs with the potential to decrease the associated morbidity, mortality, and health care system costs.
Acknowledgments
We are indebted to the Veterans who participated in our fall- and delirium-prevention programs. We are thankful to the VABHS Boston Delirium Task Force and Patient Safety Officers for continued collaboration to improve outcomes for the Veterans we serve. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government. This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development. This study is supported by the VA Delirium Patient Safety Center of Inquiry and T21 Alternative to Non-institutional Long Term Care award. Doherty, Archambault, Kelly and Rudolph are employees of the US Government. Dr Rudolph also received support from a VA Career Development Award. The abstract for this paper was presented at the 4th annual meeting of the American Delirium Society in June 2014.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Brand CA, Sundararajan V. A 10-year cohort study of the burden and risk of in-hospital falls and fractures using routinely collected hospital data. Qual Saf Health Care. 2010;19(6):e51. doi: 10.1136/qshc.2009.038273. [DOI] [PubMed] [Google Scholar]
- 2.Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med. 1995;99(2):137–143. doi: 10.1016/s0002-9343(99)80133-8. [DOI] [PubMed] [Google Scholar]
- 3.Corsinovi L, Bo M, Ricauda Aimonino N, et al. Predictors of falls and hospitalization outcomes in elderly patients admitted to an acute geriatric unit. Arch Gerontol Geriatr. 2009;49(1):142–145. doi: 10.1016/j.archger.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Hill KD, Vu M, Walsh W. Falls in the acute hospital setting – impact on resource utilisation. Aust Health Rev. 2007;31(3):471–477. doi: 10.1071/ah070471. [DOI] [PubMed] [Google Scholar]
- 5.Nadkarni JB, Iyengar KP, Dussa C, Watwe S, Vishwanath K. Orthopaedic injuries following falls by hospital in-patients. Gerontology. 2005;51(5):329–333. doi: 10.1159/000086370. [DOI] [PubMed] [Google Scholar]
- 6.Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732–739. doi: 10.1111/j.1525-1497.2004.30387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stenvall M, Olofsson B, Lundström M, Svensson O, Nyberg L, Gustafson Y. Inpatient falls and injuries in older patients treated for femoral neck fracture. Arch Gerontol Geriatr. 2006;43(3):389–399. doi: 10.1016/j.archger.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Haines TP, Bennell KL, Osborne RH, Hill KD. Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial. BMJ. 2004;328(7441):676. doi: 10.1136/bmj.328.7441.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing. 2004;33(4):390–395. doi: 10.1093/ageing/afh130. [DOI] [PubMed] [Google Scholar]
- 10.Tzeng HM, Yin CY, Anderson A, Prakash A. Nursing staff’s awareness of keeping beds in the lowest position to prevent falls and fall injuries in an adult acute surgical inpatient care setting. Medsurg Nurs. 2012;21(5):271–274. [PMC free article] [PubMed] [Google Scholar]
- 11.Coussement J, De Paepe L, Schwendimann R, Denhaerynck K, Dejaeger E, Milisen K. Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(1):29–36. doi: 10.1111/j.1532-5415.2007.01508.x. [DOI] [PubMed] [Google Scholar]
- 12.Mahoney JE, Palta M, Johnson J, et al. Temporal association between hospitalization and rate of falls after discharge. Arch Intern Med. 2000;160(18):2788–2795. doi: 10.1001/archinte.160.18.2788. [DOI] [PubMed] [Google Scholar]
- 13.Morse JM, Black C, Oberle K, Donahue P. A prospective study to identify the fall-prone patient. Soc Sci Med. 1989;28(1):81–86. doi: 10.1016/0277-9536(89)90309-2. [DOI] [PubMed] [Google Scholar]
- 14.Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049–1053. doi: 10.1136/bmj.315.7115.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hendrich AL, Bender PS, Nyhuis A. Validation of the Hendrich II Fall Risk Model: a large concurrent case/control study of hospitalized patients. Appl Nurs Res. 2003;16(1):9–21. doi: 10.1053/apnr.2003.YAPNR2. [DOI] [PubMed] [Google Scholar]
- 16.Williams MA, Campbell EB, Raynor WJ, Jr, Musholt MA, Mlynarczyk SM, Crane LF. Predictors of acute confusional states in hospitalized elderly patients. Res Nurs Health. 1985;8(1):31–40. doi: 10.1002/nur.4770080107. [DOI] [PubMed] [Google Scholar]
- 17.Foreman MD. Confusion in the hospitalized elderly: incidence, onset, and associated factors. Res Nurs Health. 1989;12(1):21–29. doi: 10.1002/nur.4770120105. [DOI] [PubMed] [Google Scholar]
- 18.Rockwood K. Acute confusion in elderly medical patients. J Am Geriatr Soc. 1989;37(2):150–154. doi: 10.1111/j.1532-5415.1989.tb05874.x. [DOI] [PubMed] [Google Scholar]
- 19.Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097–1101. [PubMed] [Google Scholar]
- 20.Schor JD, Levkoff SE, Lipsitz LA, et al. Risk factors for delirium in hospitalized elderly. JAMA. 1992;267(6):827–831. [PubMed] [Google Scholar]
- 21.Lakatos BE, Capasso V, Mitchell MT, et al. Falls in the general hospital: association with delirium, advanced age, and specific surgical procedures. Psychosomatics. 2009;50(3):218–226. doi: 10.1176/appi.psy.50.3.218. [DOI] [PubMed] [Google Scholar]
- 22.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12(5):290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morse JM, Tylko SJ, Dixon HA. Characteristics of the fall-prone patient. Gerontologist. 1987;27(4):516–522. doi: 10.1093/geront/27.4.516. [DOI] [PubMed] [Google Scholar]
- 24.Kelly B, Archambault E, Lawrence K, Rudolph J. Delirium: A practical prevention program. Fed Pract. 2013;30(1):33–35. [Google Scholar]
- 25.Morse J. Preventing patient falls. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- 26.Chester JG, Beth Harrington M, Rudolph JL, VA Delirium Working Group Serial administration of a modified Richmond Agitation and Sedation Scale for delirium screening. J Hosp Med. 2012;7(5):450–453. doi: 10.1002/jhm.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miake-Lye IM, Hempel S, Ganz DA, Shekelle PG. Inpatient fall prevention programs as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):390–396. doi: 10.7326/0003-4819-158-5-201303051-00005. [DOI] [PubMed] [Google Scholar]
- 28.Reston JT, Schoelles KM. In-facility delirium prevention programs as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):375–380. doi: 10.7326/0003-4819-158-5-201303051-00003. [DOI] [PubMed] [Google Scholar]
- 29.Morse JM, Morse RM, Tylko SJ. Development of a Scale to Identify the Fall-Prone Patient. Can J Aging. 1989;8(4):366–377. [Google Scholar]
- 30.Grande LJ, Rudolph JL, Milberg WP, Barber CE, McGlinchey RE. Detecting cognitive impairment in individuals at risk for cardiovascular disease: the “Clock-in-the-Box” screening test. Int J Geriatr Psychiatry. 2011;26(9):969–975. doi: 10.1002/gps.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med. 2013;62(5):457–465. doi: 10.1016/j.annemergmed.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


