Abstract
Ebola hemorrhagic fever is a deadly disease caused by several species of ebolavirus. The current outbreak of 2014 is unique in that it has affected a greater number of people than ever before. It also has an unusual geographic distribution. Nonspecific findings such as fever and generalized weakness have traditionally been very common early in the acute phase. Ophthalmic manifestations have also been reported in significant numbers. Conjunctival injection has been identified in both the acute and late phases. Subconjunctival hemorrhage and excessive lacrimation have also been reported. Various forms of uveitis have been associated with the convalescent phase of the disease. When identified in conjunction with other signs such as fever, acute findings such as conjunctivitis may contribute to the diagnosis of Ebola hemorrhagic fever. Ideally, serologic testing should be performed prior to isolation and treatment of these individuals. Considering the prevalence of the current outbreak and the threat of transcontinental spread, ophthalmic health professionals need to be aware of the ocular manifestations of Ebola hemorrhagic fever as well as the associated signs and symptoms in order to prevent further spread.
Keywords: conjunctivitis, ebolavirus, subconjunctival hemorrhage, uveitis, Ebola hemorrhagic fever
Ocular manifestations of Ebola
The recent tragic events unfolding in western Africa have sparked a renewed interest in a deadly yet mysterious disease. The genus Ebolavirus, known to cause Ebola hemorrhagic fever, is a group of RNA viruses that derives its name from the river next to which it was discovered. It is a member of the filovirus family and encompasses 5 species: Zaire ebolavirus, Sudan ebolavirus, Bundibugyo ebolavirus, Taï Forest ebolavirus, and Reston ebolavirus.1,2 While human-to-human transmission is known to occur through exposure to body fluids, the natural reservoir is most likely one or multiple species of fruit bats. Exposure to and consumption of these bats as well as to nonhuman primates may be the method of animal-to-human transmission.1,3 As of August 2014, the reported number of cases has reached 3,069.4
Ebola hemorrhagic fever is known for its varied constellation of severe signs and symptoms. After an initial incubation period of 2–21 days, fever, extreme asthenia, diarrhea, nausea, vomiting, anorexia, abdominal pain, headaches, arthralgias, myalgia, and/or back pain may begin.5 Fever is by far the most prevalent sign of active disease, occurring early and in as many as 94.1% of patients.6 However, ocular manifestations are also important to identify because they may aid in the diagnosis. Ocular signs have been observed in both the acute and late settings.5,7 Conjunctival injection has been reported in as many as 58% of infected patients and often presents bilaterally.8 Subconjunctival hemorrhage as well as excessive lacrimation have been reported as well.7,9 The pathophysiology behind these manifestations is unclear. Species of ebolavirus have traditionally presented themselves in rural locations. Poor access to ophthalmic equipment and experienced practitioners as well as the danger posed by close-quarter examinations has limited the level of investigation.7 However, conjunctival injection and subconjunctival hemorrhage are easily recognizable, which makes the ophthalmic examination a rapid and simple method of identifying patients who are in need of further screening measures such as quantification of body temperature. Ultimately, serologic testing (viral RNA or viral antibodies) is necessary to confirm the diagnosis of Ebola hemorrhagic fever.10 Without this, patients with more common febrile illnesses such as malaria may be isolated and may contract ebolavirus if in close quarters with infected individuals.11
Subacute/chronic ophthalmic manifestations are also of importance. Patients who have been infected with ebolavirus follow one of two pathways: they may rapidly progress to a more intense hemorrhagic state where death is nearly inevitable or they may enter a convalescent phase. Interestingly, patients who enter this phase are at risk for uveitic episodes. In a study documenting findings of the 1995 outbreak in what is now the Democratic Republic of the Congo, 15% (three patients) of patients who entered the convalescent phase developed uveitis. Episodes were by no means uniform in nature. Each patient developed a unique variation of uveitis including anterior uveitis, posterior uveitis, and panuveitis. Despite the complexity of findings, treatment required only topical steroids and cycloplegia. Inflammation was quelled, but long-term sequelae were not investigated.7 Further inquiry is necessary to identify whether this is in fact a causal relationship or simply an association.
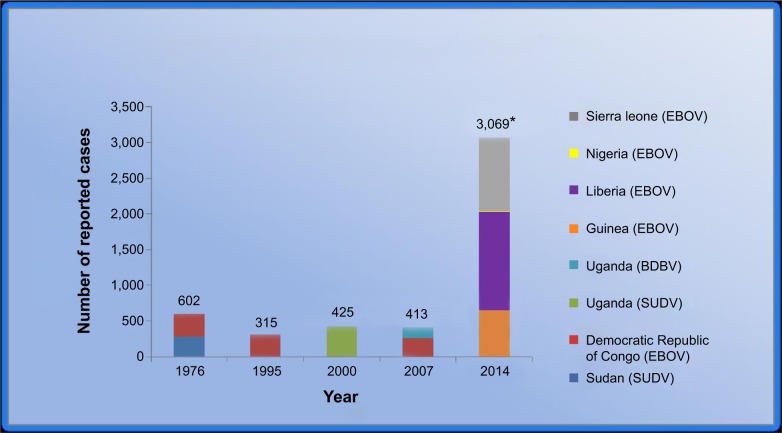
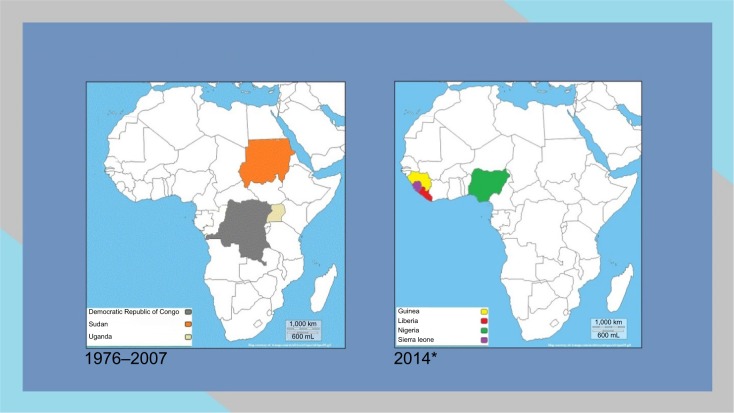
The current Ebola hemorrhagic fever outbreak involves only the Zaire ebolavirus species, and it has infected more people than any previously recorded outbreak (Figure 1). In addition, it demonstrates a unique and perplexing geographic distribution (Figure 2). These factors, in combination with the threat of transcontinental spread of the disease, make it increasingly important for medical professionals in every arena to become familiar with its signs and symptoms. Those in the ophthalmic community may come in contact with patients who complain of fever as well as ocular signs such as injection and subconjunctival hemorrhage. If patients have a recent history of international travel or other risk factors, they should be transferred to a tertiary care center for serologic testing. Patients entering the convalescent phase should be followed for evidence of uveitis. Topical steroids and cycloplegia have been proven to be effective, but further investigation of the natural history and long-term effects of this manifestation are warranted.
Figure 1.
A graphical representation of the number of reported cases from major Ebola virus outbreaks (>150 cases) from the years 1976–2014.
Note: *Cases from January to August 2014.
Abbreviations: BDBV, Bundibugyo ebolavirus; EBOV, Zaire ebolavirus; SUDV, Sudan ebolavirus.
Figure 2.
Past (1976–2007) and present (2014) maps of Africa demonstrating the Ebola virus outbreak distribution.
Note: *Cases from January to August 2014.
Footnotes
Disclosure
The authors report no conflict of interest in this work.
References
- 1.Bausch DG, Schwarz L. Outbreak of ebola virus disease in Guinea: where ecology meets economy. PLoS Negl Trop Dis. 2014;8(7):e3056. doi: 10.1371/journal.pntd.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bossi P, Tegnell A, Baka A, et al. Bichat guidelines for the clinical management of haemorrhagic fever viruses and bioterrorism-related haemorrhagic fever viruses. Euro Surveill. 2004;9(12):E11–E12. [PubMed] [Google Scholar]
- 3.World Health Organization Outbreak of Ebola haemorrhagic fever in Gabon officially declared over. Wkly Epidemiol Rec. 1996;71:125–126. [Google Scholar]
- 4.2014 Ebola Outbreak in West Africa – Case Counts [webpage on the Internet] Atlanta: Centers for Disease Control and Prevention; 2014. [Accessed August 30th, 2014]. [updated October 18, 2014]. Available from: http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html. [Google Scholar]
- 5.Bwaka MA, Bonnet MJ, Calain P, et al. Ebola hemorrhagic fever in Kikwit, Democratic Republic of the Congo: clinical observations in 103 patients. J Infect Dis. 1999;179(Suppl 1):S1–S7. doi: 10.1086/514308. [DOI] [PubMed] [Google Scholar]
- 6.Lamunu M, Lutwama JJ, Kamugisha J, et al. Containing a haemorrhagic fever epidemic: the Ebola experience in Uganda (October 2000–January 2001) Int J Infect Dis. 2004;8(1):27–37. doi: 10.1016/j.ijid.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Kibadi K, Mupapa K, Kuvula K, et al. Late ophthalmologic manifestations in survivors of the 1995 Ebola virus epidemic in Kikwit, Democratic Republic of the Congo. J Infect Dis. 1999;179(Suppl 1):S13–S14. doi: 10.1086/514288. [DOI] [PubMed] [Google Scholar]
- 8.Piot P, Bureau P, Breman G, et al. Clinical aspects of Ebola virus infection in Yambuku area, Zaire, 1976. In: Pattyn SR, editor. Ebola virus haemorrhagic fever. Amsterdam: Elsevier/North-Holland Biomedical Press; 1978. pp. 17–21. [Google Scholar]
- 9.Smith DH, Francis F, Simpson DIH. African haemorrhagic fever in the southern Sudan, 1976: the clinical manifestations. In: Pattyn SR, editor. Ebola virus haemorrhagic fever. Amsterdam: Elsevier/North-Holland Biomedical Press; 1978. pp. 27–30. [Google Scholar]
- 10.Formenty P. Ebola-Marburg viral diseases. In: Heymann DL, editor. Control of communicable diseases manual. Washington, DC: American Public Health Association; 2008. pp. 204–207. [Google Scholar]
- 11.Ebola (Ebola Virus Disease) [webpage on the Internet] Atlanta: Centers for Disease Control and Prevention; 2014. [Accessed August 27th, 2014]. [updated September 19, 2014]. Available from: http://www.cdc.gov/vhf/ebola/diagnosis/ [Google Scholar]