Abstract
Background
Since the late 1990s, the British government has launched major strategies to address high teenage pregnancy and abortion rates in England. These have focused in part on improving access to contraception through national campaigns. This study assessed teenage pregnancy and abortion rate trends since 1998 and possible associations with usage of long-acting reversible contraceptives (LARCs).
Methods
Teenage conception rates and age-specific abortion rates were obtained from the Office for National Statistics and the Department of Health. LARC usage data was obtained for Depo-Provera, Implanon/Nexplanon, intrauterine devices, Mirena, and Noristerat from the IMS British Pharmaceutical Index, IMS Hospital Pharmacy Audit, IMS Disease Analyzer, and KT-31 reports. Through linear regression methods, changes in conception and abortion-related outcomes during 1998–2011 and the associations with LARC usage were assessed.
Results
Conception rates for girls younger than 18 years of age decreased significantly between 1998–2011, from 46.6 to 30.7 per 1,000 girls. A statistically significant association was observed between this decrease and increased LARC usage (P=0.0024) in this population. Abortion rates among females aged <18 years or aged 18–19 years decreased between 1998–2011, and their associations with increased LARC usage were statistically significant (P=0.0029 and P=0.0479, respectively). The pattern in older women was complex; abortion rates in women aged 20–24 years or 25–34 years increased slightly from 1998 to 2011, with stabilization during 2007–2011.
Conclusion
Increased LARC usage in England was significantly associated with decreased teenage pregnancy rates and abortion rates in females aged <20 years. Government strategies appears to have a positive impact on these outcomes; however, abortion rates among women over 20 years of age remain an issue.
Keywords: teenage pregnancy, abortion, long-acting reversible contraceptive, LARC
Background
In the late 1990s, Britain had the highest teenage pregnancy rate in Western Europe.1,2 The Department for Education reported a conception rate of 46.6 per 1,000 girls between 15–17 years of age in England in 1998.3 According to the same report, most teenage pregnancies were unplanned, and around half of them ended in an abortion. In addition to having high teenage pregnancy rates, England and Wales also ranked highest among countries in Western Europe in terms of abortion rates. Wellings and Kane reported a rate of 22 legal terminations per 1,000 females aged <20 years in 1997,2 and nearly 174,000 abortions were performed in England and Wales in 1999.4 Abortion rates are often used as a proxy indicator for unintended pregnancy rates,5 thus these data suggest that a high level of unintended pregnancies occur in England and Wales.
Although having a child when young can represent a positive turning point in the lives of some young women, for many more teenagers, unintended pregnancies can have a long-lasting impact on their lives and the lives of their children. According to the Teenage Pregnancy Strategy: Beyond 2010 report, teenage pregnancy is both a cause and result of exclusion, poverty, and inequality, and babies of teenage mothers have a 60% higher risk of dying in their first year.3 Teenage parents also have a significantly increased risk of living in poverty, achieving less at school, and being more likely to be unemployed in later life.3 Therefore, teenage pregnancy has a potentially large impact on the lives of young women and represents a substantial cost to the state in terms of abortion-related care in the National Health Service (NHS) and social care.
In view of these substantial issues, the British government launched two major strategies in 1999 and 2001 that were supported by subcampaigns and the provision of additional funding. The first major strategy was the Teenage Pregnancy Strategy launched in 1999,3,6 which set a target to reduce the rate of conceptions in girls <18 years of age by 50% by 2010. This was followed by the National Strategy of Sexual Health and HIV, which was launched in 20014 and aimed to modernize sexual health and HIV services in England. Several midstrategy campaigns launched between 2005–2007 focused mainly on condom use, while in 2009 the late-strategy campaign “Sex. Worth Talking About” was designed to help young people make more informed choices about contraception and chlamydia testing.7 One of the two main strands of the latter campaign was “Contraception. Worth Talking About”, which focused on contraceptive choices. Additional funding of £26.8 million was also made available between 2008–2010 to increase access to long-acting reversible contraceptives (LARCs) by improving provision and training,8 primarily in the primary care setting. Many primary care trusts utilized incentive payments through Local Enhanced Service schemes to allow them to achieve this increased provision of LARCs. Overall, the strategies, campaigns, and funding focused on a number of areas that included education about sex and relationships in and out of schools, support for parents, and support for teenage parents. One of the major axes of all these initiatives was to provide young people with knowledge and access to contraception, especially LARC methods.
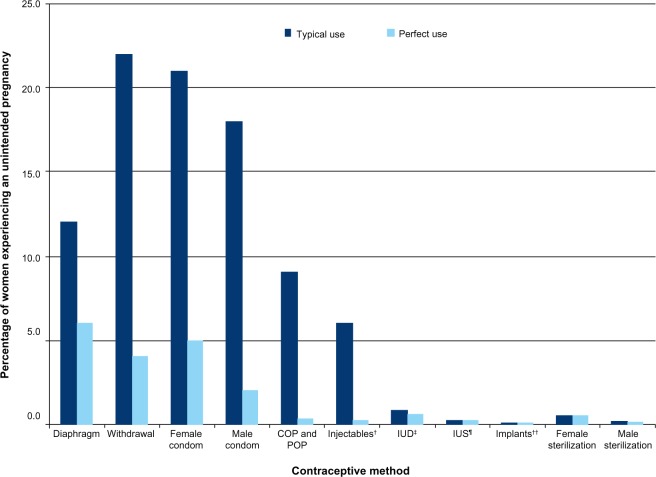
LARCs are defined as contraceptive methods that require administration less than once per menstrual cycle or month.9 LARC methods include injectables, implants, intrauterine devices (IUDs), and intra-uterine systems (IUS). In 2005, the National Institute for Health and Care Excellence (NICE) published a clinical guideline for LARC use (CG30), which demonstrated that all LARC methods were more cost-effective than the combined oral contraceptive pill even after 1 year of use.9 The effectiveness of LARC methods does not depend on daily concordance, unlike the barrier method or oral contraceptive pills for which effectiveness depends on their correct and consistent use (Figure 1).10 Since the implementation of the strategies and campaigns described previously, as well as the availability of additional funding and national guidance, the use of LARC methods has increased in England.
Figure 1.
Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception in the United States.
Notes: †Depo-Provera (Pfizer, Inc., New York, NY, USA); ‡ParaGard® T-380A (Teva Women’s Health, Inc., Sellersville, PA, USA); ¶Mirena; ††Implanon (Merck Sharp & Dohme [Hertfordshire, UK]). Reprinted from Contraception, 83(5), Trussell J, Contraceptive failure in the United States, 397–404, Copyright © 2011, with permission from Elsevier.10
Abbreviations: COP, combined oral pill; IUD, intrauterine device; IUS, intrauterine system; POP, progestogen-only pill.
The objectives of this study were first to determine whether a significant decrease in teenage pregnancy and abortion rates has occurred in England since 1998, and second to determine whether an association exists over time between LARC usage and teenage pregnancy and abortion rates. Similar analyses were also conducted on data from the Strategic Health Authorities (SHA), which were responsible for the management of the local NHS, in order to assess whether similar results were observed at the local level.
Methods
Teenage pregnancy and abortion data
Teenage pregnancy data were sourced from the Conception Statistics reports for England and Wales from 1998 to 2011, published by the Office for National Statistics.11 These reports provide annual teenage conception rates per 1,000 girls aged <18 years (defined as 15–17 years), which are considered to be an accurate indicator of teenage pregnancy. Three types of abortion data were available and included in the study: age-standardized abortion rates per 1,000 females aged 15–44 years, crude abortion rates per 1,000 females within various age groups (<18, 18–19, 20–24, 25–34, 35–44 years) and the percentages of women aged <25 years and of all ages with repeat abortions. Abortion rates were obtained from the reports published by the Department of Health (DH): Abortion Statistics reports for England and Wales, from 1998 to 2011.12 In this study, abortion rates were used as a proxy to estimate changes in unintended pregnancies over time.
LARC usage data
The LARC methods recommended by the NICE guidelines13 were considered in this analysis, which included injectables (Depo-Provera [Pfizer, Inc., New York, NY, USA]; Noristerat [Bayer AG, Leverkusen, Germany]), implants (Implanon (Merck Sharp & Dohme [Hertfordshire, UK]), Nexplanon (Merck Sharp & Dohme)), IUDs and the IUS (Mirena [Bayer AG]). Although Noristerat only represents a very low market share, it was deemed important to include it in the analyses because it is generally used during shortages of Depo-Provera. LARC unit sales from both primary care and secondary care were included. For the purposes of this analysis the terms primary and secondary care relate to the setting in which the product was purchased. Primary care sales were predominately from general practice, and secondary care sales were mostly from Contraception and Sexual Health (CaSH) clinics (where product was obtained via hospital pharmacies). Some CaSH clinics obtain contraceptive products through primary care routes; therefore a small amount of CaSH usage would have been included in the primary care sales data.
Usage data were obtained from three main sources. First, the IMS British Pharmaceutical Index (BPI) and Hospital Pharmacy Audit (HPA)14 provided unit sales for the 1998–2011 period for most of the LARC methods considered (Depo-Provera, Implanon, Nexplanon, Mirena, and Noristerat), in primary and secondary care. This database does not include data for IUDs; therefore, the projected annual number of IUD prescriptions in primary care was obtained for the UK between 1998–2011 from IMS® Disease Analyzer (IMS Health, Danbury, Connecticut, USA).15 It was assumed that number of prescriptions was a reasonable proxy for actual sales. Secondary care IUD sales data in England from 1998–2011 were estimated from the number of first contacts (first face-to-face consultation in the financial year) with women at Community Contraceptive Services (ie, CaSH clinics and voluntary advice agencies such as Brook which offers free and confidential sexual health information for people aged under 25 years). As reported in the KT-31 reports published by the NHS contraceptive services.16 IUDs are fitted for a duration of 5–10 years depending on the device, and only a single routine follow-up visit is recommended after the first menses, or 3–6 weeks after insertion.9 Therefore, it was assumed that within any year, the first contact visit at the clinic occurs only to fit a new IUD and not to replace an IUD that has failed before the end of its indicated duration, with no additional follow-on (subsequent) visits required for repeated monitoring with the IUD in place.9
In addition, SHA-specific data were captured from the same sources in order to determine whether results obtained at the national level were similar across different SHAs. Data for Noristerat were not provided by SHA, but it was assumed that Noristerat sales were low enough not to impact the results because they only represent a small proportion of total LARC sales.
Data preparation and assumptions
Data were obtained from various sources, and data restructuring and further assumptions were required to provide analytical datasets for the purpose of this study.
England-specific data were required for this analysis but some data were only reported for the UK (eg, secondary care LARC sales between 1998–2006 from the IMS HPA). Wherever necessary, a year-specific proportion was applied to UK data in order to derive England-specific sales data. The year-specific proportion was defined as each year population estimates of England divided by the UK population estimates of that year, which were obtained from the Office for National Statistics website.17
Primary care sales data for Depo-Provera in IMS BPI were found to be incomplete until 2009, which led to a significant increase of unit sales between 2008–2009. In order to prevent any misinterpretation of the trend of LARC usage over time and its impact on outcomes, the average between the trend observed over the 1998–2008 period (13% increase) and the trend observed over the entire 1998–2011 period (18% increase) was added to the 1998–2008 values. Sales data during that period were then inflated by 16%.
A breakdown of the data by age category was required to conduct age-specific analyses, but age groups differed between the data sources. LARC usage data from IMS Disease Analyzer® and KT-31 were redistributed to match the age groups of the outcomes variables (Table S1). In addition, LARC unit sales reported by IMS BPI and HPA were not broken down by age category. Therefore, it was assumed that the age distribution of these unit sales was the same as those reported in IMS Disease Analyzer® for primary care and in KT-31 reports for secondary care. The total number of LARC unit sales was split on the basis of the assumed age distributions. The final study age groups were 15–17, 18–19, 20–24, 15–24, 25–34, 35–44, and 15–44 years.
Annual secondary care IUD data from KT-31 reports cover a period from April 1 to March 31 instead of calendar years. Therefore, secondary care IUD data were redistributed into calendar years.
LARCs have significant differences in their recommended duration of use. As such, the unit sales data reflect the frequency at which each method is readministered, and this analysis needed to account for both volumes of sales and frequency of administration in order to reflect the true usage of LARC. This was achieved by calculating the estimated average duration of use for each LARC method, expressed in number of menstrual cycles covered. Depo-Provera, Implanon/Nexplanon, Mirena, and Noristerat have an expected length of use, according to product license, of 3 cycles, 36 cycles, 60 cycles, and 2 cycles, respectively. IUDs were assumed to have a duration of use of 96 cycles, based on the recommended duration for T-Safe CU380A (Eurim Pharm, Saaldorf-Surheim, Germany) at the time the NICE guidance on LARC was published in 2005. T-Safe CU380A currently has the highest market share (55% in 2011 according to IMS Disease Analyzer®) and NICE used it as the reference IUD in the economic evaluation of LARC methods they conducted as part of CG30.13 In addition, women who had their LARC method removed early for any reason were accounted for by adjusting the recommended duration for each method with the corresponding removal rates, as reported in the NICE economic evaluation of LARC methods. Applying a removal rate is not relevant for Depo-Provera and Noristerat, as these are injections and cannot be removed; therefore, this method was only applied to IUS, IUDs, and implants (Table S2). Throughout the analyses, cycles were assumed to be of 1 month duration.
Preparation of the data by SHA required assumptions and calculations that were identical to those applied at the national level.
Statistical analyses
Simple linear regression models were built on each outcome of interest separately, using 14 annual data points over the 1998–2011 period, using time as a covariate to assess change in rates over time. Results are shown graphically and P-values of the effect of time on outcomes of interest derived from the fitted regression models are reported on the figures to assess the statistical significance of the association between the outcome variable and time.
Similarly, multiple linear regression models were built on each outcome of interest over the 1998–2011 period, using time and LARC usage as covariates to determine whether an association exists between LARC usage and change in rates, adjusted for the effect of time. P-values of the LARC usage coefficient estimates derived from the fitted regression models were used to assess the statistical significance of the association between LARC usage and the outcomes of interest. These P-values are reported on the figures.
Statistical significance was assessed at the 5% level and all statistical analyses were conducted in SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Long-acting reversible contraceptive usage over time
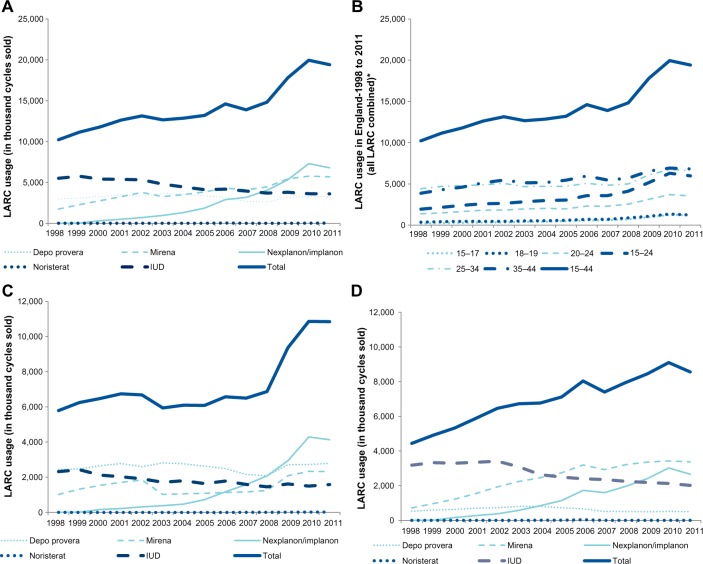
Total LARC usage, as defined by number of cycles sold, increased by 89.7% in females aged 15–44 years, from 10.2 million cycles sold in 1998 to 19.4 million cycles in 2011 (Figure 2). The greatest increase was observed in younger age groups, with a six-fold and three-fold increase in use amongst the <18 years of age and 18–19 years of age groups, respectively.
Figure 2.
Number of LARC cycles sold from 1998–2011.
Notes: (A) By method, primary and secondary care combined; (B) by age group; (C) primary care only; (D) secondary care only.
Abbreviations: IUD, intrauterine device; LARC, long-acting reversible contraceptive.
When considering each product individually, the greatest usage increase was observed for Implanon/Nexplanon (zero reported sales in 1998, followed by a 228-fold increase between 1999–2011). Usage of Mirena also increased by 2.3-fold, whereas the number of cycles of Depo-Provera sold remained fairly constant (10.5% increase) and IUD usage decreased by 34.5%. A drop in Implanon/Nexplanon cycles sold was observed between 2010–2011, which drove a similar drop in total LARC usage during that period.
It can be noted that a sharper increase in LARC usage has occurred since 2007, overall and in all age groups studied. This increase since 2007 was greater in primary care compared to secondary care (CaSH clinics), with increases of 67.0% and 15.7% between 2007–2011, respectively (Figure 2B and C).
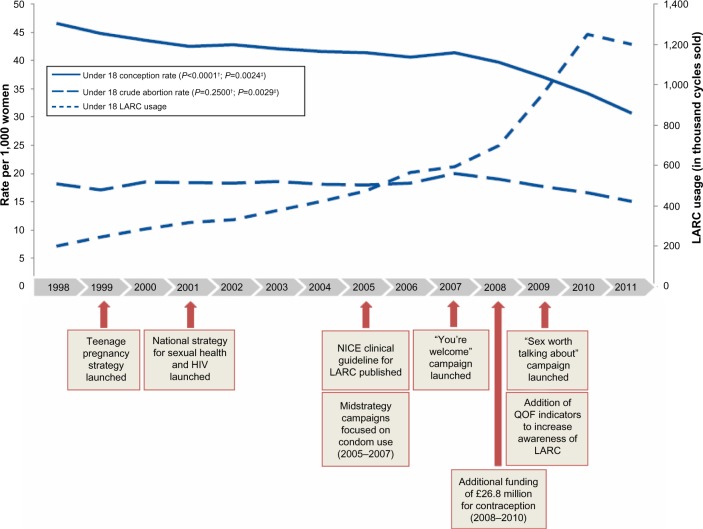
Teenage pregnancy and abortion rates over time
A steady and statistically significant decrease in teenage pregnancy was observed in England, with a steeper decline since 2007 (Figure 3). Conception rates per 1,000 girls aged <18 years decreased by 34.1%, from 46.6 in 1998 to 30.7 in 2011, and this change was shown to be statistically significant (P<0.0001). A substantial proportion of this decrease was observed between 2007–2011, where the conception rate in this age group dropped by 25.8%.
Figure 3.
LARC usage and outcomes rates in women aged <18 years.
Notes: P-values represent †the statistical significance of rate change over time and ‡the association between the rate change and LARC usage.
Abbreviations: HIV, human immunodeficiency virus; LARC, long-acting reversible contraceptive; NICE, National Institute for Health and Care Excellence; QOF, Quality and Outcomes Framework.
Between 1998–2011, crude abortion rates, a proxy for unintended pregnancies, in girls aged <18 years (Figure 3) and in women aged 18–19 years (Figure 4A) decreased by 17.2% and 14.0%, respectively. These changes were not statistically significant over the full study period, but since 2007 a statistically significant accentuation of the decrease in these younger age groups was observed: crude abortion rates dropped by 24.6% in girls aged <18 years (P=0.0047) and by 15.8% in women aged 18–19 years (P=0.0005).
Figure 4.
LARC usage and crude abortion rates and age-standardized abortion rates.
Notes: Crude abortion rates per 1,000 women aged (A) 18–19 years; (B) 20–24 years; (C) 25–34 years; and age-standardized abortion rates per 1,000 women aged (D) 15–44 years. P-values represent †the statistical significance of rate change over time and ‡the association between the rate change and LARC usage.
Abbreviation: LARC, long-acting reversible contraceptive.
Crude abortion rates increased slightly in women aged 20–24 years (2.6%, P=0.6347; Figure 4B) and significantly in women aged 25–34 years (13.0%, P<0.0001; Figure 4C) between 1998–2011. No change was observed in women aged ≥35 years (<1%, P=0.7949; data not shown). Stabilization of crude abortion rates in women aged ≥20 years was observed between 2007–2011.
Age-standardized abortion rates per 1,000 females aged 15–44 years showed a constant increase between 1998–2007 (9.3%), followed by a decrease of 6.4% between 2007–2009 and no change during the last 2 years (Figure 4D). As a result of the trend observed until 2007, age-standardized abortion rates were shown to increase over the full study period, and that increase was statistically significant (P=0.0395).
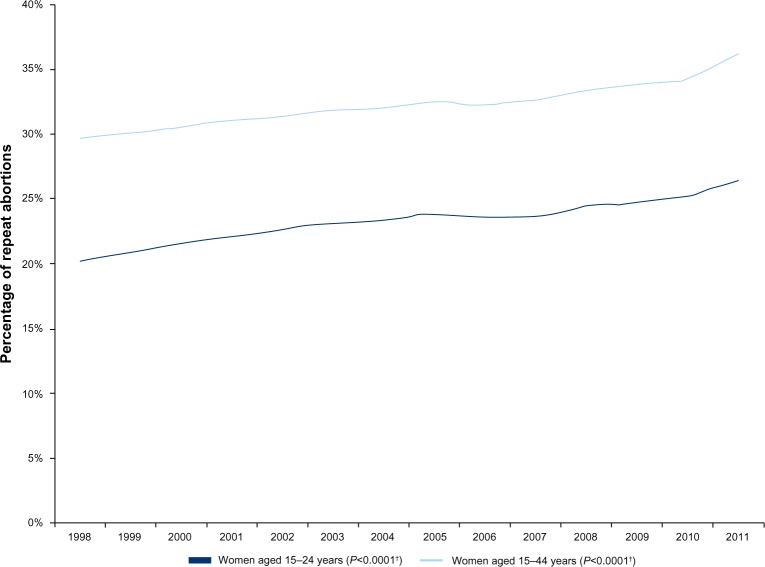
The percentage of women with repeat abortions increased steadily from 1998–2011 by 30.7% and 22.0% in females aged 15–24 years and 15–44 years, respectively (Figure 5). This increase was statistically significant in both age categories (P<0.0001).
Figure 5.
Percentage of repeat abortions.
Note: †P-values represent the statistical significance of rate change over time.
Association between LARC usage and teenage pregnancy and abortion rates
Conception rates in girls aged <18 years decreased by 34.1% over the study period, while LARC cycle sales in the same age group were six times higher in 2011 than in 1998. A noticeably steeper increase in LARC usage and decrease in conception rates was also observed from 2007 (Figure 3). The decrease in conception rates was found to have a statistically significant association with the increase of LARC sales in the group aged <18 years (P=0.0024). The crude abortion rate in girls aged <18 years decreased over the full study period, and a statistically significant association was found with increased LARC usage in the same age group (P=0.0029; Figure 3).
Similarly, LARC usage in the group aged 18–19 years increased significantly over the entire period, with a steeper increase observed since 2007. The crude abortion rate in this age group showed little change between 1998–2007 and a statistically significant decrease during the 2007–2011 period only (Figure 4A). Likely driven by the changes in the later years, the association between the crude abortion rate and LARC usage was shown to be statistically significant over the entire period (P=0.0479). To a lesser extent, similar results were found for the association between crude abortion rates and LARC usage in women aged 20–24 years (Figure 4B) and 25–34 years (Figure 4C). LARC usage was shown to increase overall in these age groups, especially during the 2007–2011 period when a slight decrease of crude abortion rate was also observed. As a result, the analyses reported a statistically significant association between increasing LARC usage and decreasing crude abortion rates in the groups aged 20–24 years and 25–34 years (P=0.0016 and P=0.0258, respectively), despite a rise in abortion rates in these groups over the entire study period.
No statistically significant change was observed in crude abortion rates in women aged 35–44 years during the study period, and the percentage of women with repeat abortions steadily increased. As a result, no association could be found between these outcomes and LARC usage in the corresponding age categories.
Analyses at the SHA level
Teenage pregnancy and abortion data were available only since 2007 at the SHA level. This analysis showed a great disparity between SHAs in terms of teenage pregnancy and abortion rates, and no correlations between these rates and LARC usage could be identified. These results are not shown but are available on request.
Discussion
This analysis showed that a number of positive changes have occurred since the implementation of campaigns and funding aimed at addressing teenage pregnancy and abortions in England. The most significant change observed is the 34.1% decrease in conception rates in girls aged <18 years since 1998. It is less than the national 10-year target of 50% set by the Teenage Pregnancy Strategy launched in 1999,18 but it is nevertheless a positive change and it will be important to see if this trend continues during the next few years. Crude abortion rates in that age group and in women aged 18–19 years have also followed a substantial decrease of 17.2% and 14.0%, respectively, although this change was not found to be statistically significant.
Unfortunately, not all of the outcomes of interest have showed such a positive trend. Age-standardized abortion rates, a proxy for unintended pregnancies, followed a statistically significant increase between 1998 and 2011 in women aged 15–44 years. In addition, crude abortion rates in women aged 20–24 years and women aged 25–34 years increased during the study period, and no change was observed in women aged ≥35 years. Finally, the percentage of women with repeat abortions has increased steadily since 1998.
It can be noted that the 2007–2011 period has seen a faster decline in most of the outcomes studied. In that period alone, conception rates and crude abortion rates in women aged <18 years have dropped by 25.8% and 24.6%, respectively. To a lesser extent, age-standardized abortion rates and crude abortion rates in women aged 18–19 years also showed a statistically significant decrease during that period. The 2007–2011 period also shows a stabilization of crude abortion rates in women aged 20 years and older, with a slight decrease in women aged 20–24 years.
All age groups reported an increase in LARC usage over the study period and the number of LARC cycles sold in women aged 15–44 years has increased by almost 90%. In particular, younger age groups (<18 years and 18–19 years) have seen a substantial increase in their LARC usage that is reflected by an increase of up to six-fold in these age groups. It is important to notice the faster increase of LARC usage observed in all age groups since 2007, because more positive changes in outcomes were also observed in that period.
The observed increase in LARC usage over time, which was driven in part by government policies, additional funding, and national guidance, has been shown to have had a positive effect on teenage pregnancy and abortion rates, particularly in the younger age groups. An association between decreasing conception and abortion rates and increasing LARC usage was found in the younger age groups, in particular those aged <18 years and 18–19 years. We believe that government actions have had a beneficial effect on teenage pregnancy and abortions in young women, which is likely due to the strategies and campaigns specifically targeted on teenage pregnancy. In addition, special efforts by way of additional funding were made to increase access to LARC in 2008 with an additional £26.8 million in funding to improve access to contraception in England,19 the period during which the greatest increase in LARC usage was observed. This additional funding was largely targeted towards primary care services, which is reflected by a 58.0% increase in primary care LARC usage between 2008–2010. It is known that more than half of teenage pregnancies result in abortion;3 therefore, a reduction in abortion rates in younger women along with positive change in teenage pregnancy rates is consistent with the expected impact of these strategies.
The smaller changes in abortion rates observed in the older age groups (>19 years) and the lack of evidence of an association between LARC usage and abortion rates in the group aged 35–44 years group suggest that more actions are needed to address unintended pregnancies in women aged ≥20 years. This is consistent with the recently published Framework for Sexual Health Improvement in England,20 which aims to reduce unwanted pregnancies and improve access to contraception among women of all ages. The high percentage of repeat abortions and its constant increase since 1998 despite all campaigns and funding put in place suggest that further actions are required to address this continuing issue.
The UK still has one of the highest teenage pregnancy rates in Western Europe,21 and England and Wales rank second highest after Scotland in terms of abortion rates in women aged <20 years.22 The results of this analysis demonstrate that clear progress has been made; however, further support to women in terms of information and access to contraception is needed. It is critical that the positive changes observed are maintained, to prevent a reversal of the positive effects seen to date. This will be particularly important in light of the changes to the NHS in England that have been put in place since April 2013. Commissioning of sexual health services, including contraception services, will become fragmented and it will be critical to ensure that in this time of upheaval and efficiency savings, ongoing sexual health service provision is prioritized.
Several limitations need to be taken into account when interpreting the study results. Firstly, LARC usage is only one indicator of the government measures taken towards teenage pregnancy and abortion, and it cannot be interpreted as a measure of the effectiveness of government policies. Furthermore, many other government and societal factors that impact the rates of teenage pregnancy and abortion were not taken into account in this study. Examples of potential factors include: oral contraceptive usage and sex education, induced abortions, concurrent social issues and society expectations, religion, spontaneous abortions, economics, and maternal deaths before or at term. A future study that adjusts for these additional factors may provide a more accurate estimation of the impact of LARC usage on the rates of teenage pregnancy and abortion.
In addition, the data that were available for this study had significant limitations. Due to a lack of individual patient level data, substantial data manipulation had to be conducted in order to align LARC usage data with outcomes data, and assumptions had to be made. The use of aggregated data also contributed to the difficulty in investigating other confounding factors in addition to LARC usage and the specific effect on teenage pregnancy and abortion. The derivation of England data from UK data, the re-distribution of age groups across the various data sources, the method used to address missing Depo-Provera data, and assuming first contacts with women using IUD at contraceptive services to be a reasonable proxy for IUD unit sales in secondary care may all have introduced some bias in LARC usage. Although the approach taken – to use number of cycles sold instead of unit sales – enabled us to take into account actual LARC usage, the assumptions and calculations used to derive number of cycles sold may have introduced some additional bias. Also, no data from abortion clinics were available and LARC methods used for other indications were not accounted for (eg, IUS for heavy menstrual bleeding). Therefore, more robust data sources for LARC usage, such as patient registries, may enable further investigation of the relationship between LARC usage and pregnancy outcomes.
Finally, studying the entire 1998–2011 period may have limited the findings, as trends varied during that period. A more stable trend has been observed since 2007, which may be related to further actions taken by the government, and more research focusing on 2007 and beyond may provide more robust results. More robust analyses of local data may provide further information as to whether trends observed at the national level are also reported regionally. Additional studies and analyses on removable LARC methods (IUDs, IUSs, implants) compared with nonremovable LARC methods (injectables) could highlight any differences in effectiveness in decreasing teenage pregnancy rates and abortion rates.
Despite its limitations, this study is the first to look at trends in teenage pregnancy and abortions and to investigate how LARC usage was associated with these trends as a possible indicator of the results of actions taken by the government since 1998 to tackle these issues. It seems highly likely that the government actions have resulted in a positive impact on teenage pregnancy and that improving LARC uptake and availability has contributed to this, even if further work is needed to ensure not only young women benefit from access to information and contraceptive methods. Repeating this study again in 5 years with better data will provide more robust results, especially now that the Sexual and Reproductive Health Activity Data set is available.
Conclusion
This study has shown that the increase in LARC usage observed in England between 1998–2011 was statistically significantly associated with decreased teenage pregnancy rates and decreased abortion rates in women 19 years of age and younger.
The overall age-standardized abortion rate and crude abortion rates in women aged 20 years and older increased over the entire study time period, although stabilization of these rates has been observed since 2007. Despite this, an association was found between LARC usage and abortion rates in women aged 20–24 years and 25–34 years, but not in those aged 35 years and older.
These results highlight that increased LARC usage as a result of government policies and additional funding, in addition to the improvements in education and awareness driven by the same policies, has had a beneficial effect on outcomes in younger women. However, a lesser effect was seen in women aged 20 years and older, and England still has one of the highest rates of teenage pregnancy and unintended pregnancy in western Europe. Further work is needed to ensure that the positive changes achieved so far in younger age groups are maintained and are extended to reach older women.
Supplementary materials
Table S1.
Data collection and aligning methods for conception, abortion, and LARC usage methods
| Conception
|
Abortion
|
LARC usage method
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Conception rates | Age-standardized abortion rates | Crude abortion rates | Repeat abortion | DEPO | IMP/NEXP | MIR | NOR | IUD | |
| Source/data collection method | Conception Statistics reports for England and Wales from 1998–2011, published by the Office for National Statistics | Department of Health | Department of Health | Department of Health | IMS British Pharmaceutical Index and IMS Hospital Pharmacy Audit for primary and secondary sales data | IMS Disease Analyzer for primary care sales; number of first contacts with women at Community Contraceptive Services as reported in KT-31 | |||
| Transformation 1 | For aligning secondary care IUD (KT-31) data prior to 2006–2007 with conception rates, it is assumed that data for ages 13–15 years is for age 15 years, and data for ages 16–19 years is split evenly into ages 16–17 years and ages 18–19 years | For aligning secondary care IUD (KT-31) data prior to 2006–2007 with age-standardized abortion rates for ages 15–44 years, it is assumed that data for ages 13–15 years is for age 15 years only, while all remaining age categories are combined | Crude abortion rates for ages 25–34 years are obtained by combining data for ages 25–29 years and ages 29–34 years | For repeat abortions, data for all ages <25 years are assumed to be for ages 15–24 years, and data for all ages are assumed to be for ages 15–44 years | Breakdown by age (15–17, 18–19, 2 0–24, 15–24, 25–34, 35–44, and 15–44 years) was performed by assuming the same distribution of patients as in the IMS Disease Analyzer ® data for primary care and in KT-31 for secondary care | Assumed that women who attend the clinic in a given year have their IUD fitted that year and not in previously, and that women who obtain a fitted IUD do not return to the clinic | |||
| Transformation 2 | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with conception rates for ages 15–17 years, data for age 15 years and ages 16–17 years are combined | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with age standardized- abortion rates for ages 15–44 years, the data for ages <15 years are excluded and all remaining age categories are combined | For aligning secondary care IUD (KT-31) data prior to 2006–2007 with crude abortion rates: for ages 15–44 years, it is assumed that data for ages 13–15 years is for age 15 years only while all remaining age categories were combined; for ages 15–17 years, it is assumed data for ages 13–15 years is for age 15 years only, while data for ages 16–19 years is split into ages 16–17 years and ages 18–19 years; for ages 16–19 years, it is assumed data for ages 16–19 years is split into 16–17 years and 18–19 years | For aligning secondary care IUD (KT-31) prior to 2006–2007 with repeat abortion rates: for ages <25 years, it is assumed that data for ages 13–15 years are for age 15 years only, and data for ages <16 years, 16–19 years, and 20–24 years are combined; it is assumed that data for ages 13–15 years are for age 15 years only, while all remaining age categories are combined | UK data were applied a year-specific population ratio in order to derive England-specific sales data for secondary-care LARC sales between 1998–2006 from IMS Hospital Pharmacy Audit | Annual secondary care IUD data from KT-31 reports covered a period from April 1 to March 31; secondary-care IUD data were therefore redistributed into calendar years | |||
| Transformation 3 | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with repeat abortion rates: for ages 15–44 years, exclude data for ages <15 and combine remaining age categories; for ages 15–17 years, combine data for age 15 years and ages 16–17 years | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with repeat abortion rates: for ages <25, data for ages 15, 16–17, 18–19, and 20–24 years are combined; for all ages, ages <15 is excluded and all remaining categories are combined | Incomplete DEPO primary-care sales data for 1998–2008 required these sales to be adjusted, and the average difference observed between the trends over the 1998–2008 period and over the entire period was added to the original sales values | ||||||
Abbreviations: DEPO, Depo-Provera; IMP, Implanon; IUD, Intrauterine device; LARC, long-acting reversible contraceptives; MIR, Mirena; NEXP, Nexplanon; NOR, Noristerat.
Table S2.
Estimated average duration of LARC use
| LARC | Expected length of use in years (cycles) | Annual removal rate (% of women)
|
Average duration (number of years) | Average duration (number of cycles) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Year 6 | Year 7 | Year 8 | ||||
| MIR | 5 (60) | 25.3% | 13.3% | 8.4% | 6.0% | 3.9% | n/a | n/a | n/a | 3 | 37 |
| IMP/NEXP | 3 (36) | 22.5% | 14.5% | 9.0% | n/a | n/a | n/a | n/a | n/a | 2 | 29 |
| IUD† | 8 (96) | 21.6% | 13.4% | 11.8% | 9.1% | 5.7% | 1.0% | 1.0% | 1.0% | 4 | 51 |
| DEPO | 0.3 (3) | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 0.3 | 3 |
| NOR | 0.2 (2) | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 0.2 | 2 |
Notes:
Based on T-Safe CU380A. Reproduced from: National Collaborating Centre for Women’s and Children’s Health. Long-Acting Reversible Contraception. NICE Clinical Guideline No.30. London: RCOG Press; 2013, with the permission of the Royal College of Obstetricians and Gynaecologists.1
Abbreviations: DEPO, Depo-Provera; IMP, Implanon; IUD, Intrauterine device; LARC, long-acting reversible contraceptive; MIR, Mirena; NEXP, Nexplanon; NOR, Noristerat.
Reference
- 1.National Institute for Health and Care Excellence . CG30: Long-acting reversible contraception [webpage on the Internet] London, UK: NICE; 2014. [Accessed June 22, 2014]. Available from: http://publications.nice.org.uk/long-acting-reversible-contraception-cg30. [Google Scholar]
Acknowledgments
We thank Venkata Putcha, freelance statistician contracted by HERON – A PAREXEL® Company, for his contribution to the statistical analyses. We also thank Samuel Stoddard and Catherine Kielar, scientific writers at HERON – A PAREXEL® Company, for the feedback they provided by reviewing this manuscript.
Author contributions
All authors made substantial contributions to data generation and analysis, drafting or critical revision of the manuscript, and approval for the final version to be published.
Disclosure
This study was sponsored by Merck Sharp & Dohme Ltd. Samantha Humphreys is a current employee of Merck Sharp & Dohme Ltd. Guilhem Pietri (HERON – A PAREXEL® Company) was contracted by Merck Sharp & Dohme Ltd to conduct the study analysis and develop the manuscript. Jingbo Yu is a current employee of Merck and Co, Inc. Anne Connolly presently consults, and in the past has consulted, with manufacturers of products discussed in this article. The authors report no other conflicts of interest in this work.
References
- 1.National Institute of Health and Care Excellence . Reducing the rate of teenage conceptions. An international review of the evidence (data from Europe) – Part 1 [webpage on the Internet] London, UK: NICE; 1999. [Accessed March 21, 2013]. [updated December 11, 2009]. Available from: http://admin.nice.org.uk/nicemedia/documents/pregnancyinternationalpt1.pdf. [Google Scholar]
- 2.Wellings K, Kane R. Trends in teenage pregnancy in England and Wales: how can we explain them? J R Soc Med. 1999;92(6):277–282. doi: 10.1177/014107689909200603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department for Education . Teenage Pregnancy Strategy: Beyond 2010 [webpage on the Internet] London, UK: The National Archives; 2010. [Accessed March 21, 2013]. Available from: https://www.education.gov.uk/publications/standard/Teenagepregnancysexualhealth/Page1/DCSF-00224-2010. [Google Scholar]
- 4.Department of Health . Better prevention, better services, better sexual health – The national strategy for sexual health and HIV [webpage on the Internet] London, UK: The National Archives; 2001. [Accessed March 21, 2013]. Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4003133. [Google Scholar]
- 5.Lucas S. Unprotected Nation: The Financial and Economic Impacts of Restricted Contraceptive and Sexual Health Services. London, UK: Reckitt Benckiser Healthcare (UK) Ltd.; 2013. [Accessed March 21, 2013]. http://www.wecantgobackwards.org.uk/uploads/media/17/15738.pdf. [Google Scholar]
- 6.Department of Health, Department for Children, Schools and Families . Teenage Pregnancy and Sexual Health Marketing Strategy. London, UK: Crown Copyright; 2009. [Accessed March 21, 2013]. Available from: http://www.nhs.uk/sexualhealthprofessional/Documents/Sexual_Health_Strategy_2009.pdf. [Google Scholar]
- 7.Sexual Health Professional . Sex. Worth talking about [homepage on the Internet] London, UK: National Health Service; 2009. [Accessed March 21, 2013]. Available from: http://www.nhs.uk/sexualhealthprofessional/Pages/index.aspx. [Google Scholar]
- 8.Medical Foundation for AIDS and Sexual Health (MedFASH) Progress and Priorities – Working Together for High Quality Sexual Health. Review of the National Strategy for Sexual Health and HIV. London, UK: Medical Foundation for AIDS and Sexual Health (Med-FASH); 2008. [Accessed March 21, 2013]. Available from: http://www.medfash.org.uk/uploads/files/p17abl1iai1e961d438j2pjl1rp7p.pdf. [Google Scholar]
- 9.National Institute for Health and Care Excellence . CG30: Long-acting reversible contraception [webpage on the Internet] London, UK: NICE; 2014. [Accessed June 22, 2014]. Available from: http://publications.nice.org.uk/long-acting-reversible-contraception-cg30. [Google Scholar]
- 10.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Office for National Statistics . Conception Statistics, England and Wales, 2012 [webpage on the Internet] Newport, South Wales, UK: Office for National Statistics; 2014. [Accessed October 22, 2012]. Available from: http://www.ons.gov.uk/ons/rel/vsob1/conception-statistics--england-and-wales/2012/index.html. [Google Scholar]
- 12.Department of Health . Abortion statistics, England and Wales [webpage on the Internet] London, UK: Crown Copyright; 2013. [Accessed October 22, 2012]. Available from: https://www.gov.uk/government/collections/abortion-statistics-for-england-and-wales. [Google Scholar]
- 13.National Institute for Health and Clinical Excellence . Long-Acting Reversible Contraception: The Effective and Appropriate Use of Long-Acting Reversible Contraception. London, UK: RCOG Press; 2013. [Accessed June 22, 2014]. Available from: http://www.nice.org.uk/nicemedia/live/10974/29912/29912.pdf. [PubMed] [Google Scholar]
- 14.IMS Health . IMS Health, British Pharmaceutical Index (BPI) and Hospital Pharmacy Audit (HPA) 2012. [Google Scholar]
- 15.IMS . IMS UK Disease Analyzer (August and November 2012) as interpreted by MSD Ltd. 2012. [Google Scholar]
- 16.Health and Social Care Information Centre . NHS Contraceptive Services – England, 2011–2012, Community contraceptive clinics [webpage on the Internet] Leeds, UK: HSCIC; 2014. [Accessed October 22, 2012]. Available from: http://www.hscic.gov.uk/article/2021/Website-Search?productid=9063&q=NHS+contraceptive+services+1997&sort=Relevance&size=10&page=1&area=both#top. [Google Scholar]
- 17.Office for National Statistics . Vital Statistics: Population and Health Reference Tables [webpage on the Internet] Newport, South Wales, UK: Office for National Statistics; 2014. [Accessed June 22, 2014]. Available from: http://www.ons.gov.uk/ons/rel/vsob1/vital-statistics--population-and-health-reference-tables/index.html. [Google Scholar]
- 18.National Health Service . The Rotherham Teenage Pregnancy Strategy: Annual Report 2010 – 2011. Rotherham, UK: NHS; 2011. [Accessed March 21, 2013]. Available from: http://moderngov.rotherham.gov.uk/documents/s44868/PART%202%20Teenage%20pregnancy%20strategy.pdf. [Google Scholar]
- 19.Family Planning Association . Contraception. London, UK: FPA; 2011. [Accessed June 22, 2014]. Available from: http://www.fpa.org.uk/sites/default/files/contraception-policy-statement.pdf. [Google Scholar]
- 20.Department of Health . A Framework for Sexual Health Improvement in England. London, UK: Crown Copyright; 2013. [Accessed June 22, 2014]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/142592/9287-2900714-TSO-SexualHealthPolicyNW_ACCESSIBLE.pdf. [Google Scholar]
- 21.Avery L, Lazdane G. What do we know about sexual and reproductive health of adolescents in Europe? Eur J Contracept Reprod Health Care. 2010;15(Suppl 2):S54–S66. doi: 10.3109/13625187.2010.533007. [DOI] [PubMed] [Google Scholar]
- 22.Sedgh G, Bankole A, Singh S, Eilers M. Legal abortion levels and trends by woman’s age at termination. Perspect Sex Reprod Health. 2013;45(1):13–22. doi: 10.1363/4501313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Data collection and aligning methods for conception, abortion, and LARC usage methods
| Conception
|
Abortion
|
LARC usage method
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Conception rates | Age-standardized abortion rates | Crude abortion rates | Repeat abortion | DEPO | IMP/NEXP | MIR | NOR | IUD | |
| Source/data collection method | Conception Statistics reports for England and Wales from 1998–2011, published by the Office for National Statistics | Department of Health | Department of Health | Department of Health | IMS British Pharmaceutical Index and IMS Hospital Pharmacy Audit for primary and secondary sales data | IMS Disease Analyzer for primary care sales; number of first contacts with women at Community Contraceptive Services as reported in KT-31 | |||
| Transformation 1 | For aligning secondary care IUD (KT-31) data prior to 2006–2007 with conception rates, it is assumed that data for ages 13–15 years is for age 15 years, and data for ages 16–19 years is split evenly into ages 16–17 years and ages 18–19 years | For aligning secondary care IUD (KT-31) data prior to 2006–2007 with age-standardized abortion rates for ages 15–44 years, it is assumed that data for ages 13–15 years is for age 15 years only, while all remaining age categories are combined | Crude abortion rates for ages 25–34 years are obtained by combining data for ages 25–29 years and ages 29–34 years | For repeat abortions, data for all ages <25 years are assumed to be for ages 15–24 years, and data for all ages are assumed to be for ages 15–44 years | Breakdown by age (15–17, 18–19, 2 0–24, 15–24, 25–34, 35–44, and 15–44 years) was performed by assuming the same distribution of patients as in the IMS Disease Analyzer ® data for primary care and in KT-31 for secondary care | Assumed that women who attend the clinic in a given year have their IUD fitted that year and not in previously, and that women who obtain a fitted IUD do not return to the clinic | |||
| Transformation 2 | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with conception rates for ages 15–17 years, data for age 15 years and ages 16–17 years are combined | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with age standardized- abortion rates for ages 15–44 years, the data for ages <15 years are excluded and all remaining age categories are combined | For aligning secondary care IUD (KT-31) data prior to 2006–2007 with crude abortion rates: for ages 15–44 years, it is assumed that data for ages 13–15 years is for age 15 years only while all remaining age categories were combined; for ages 15–17 years, it is assumed data for ages 13–15 years is for age 15 years only, while data for ages 16–19 years is split into ages 16–17 years and ages 18–19 years; for ages 16–19 years, it is assumed data for ages 16–19 years is split into 16–17 years and 18–19 years | For aligning secondary care IUD (KT-31) prior to 2006–2007 with repeat abortion rates: for ages <25 years, it is assumed that data for ages 13–15 years are for age 15 years only, and data for ages <16 years, 16–19 years, and 20–24 years are combined; it is assumed that data for ages 13–15 years are for age 15 years only, while all remaining age categories are combined | UK data were applied a year-specific population ratio in order to derive England-specific sales data for secondary-care LARC sales between 1998–2006 from IMS Hospital Pharmacy Audit | Annual secondary care IUD data from KT-31 reports covered a period from April 1 to March 31; secondary-care IUD data were therefore redistributed into calendar years | |||
| Transformation 3 | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with repeat abortion rates: for ages 15–44 years, exclude data for ages <15 and combine remaining age categories; for ages 15–17 years, combine data for age 15 years and ages 16–17 years | For aligning secondary care IUD (KT-31) data for 2006–2007 and after with repeat abortion rates: for ages <25, data for ages 15, 16–17, 18–19, and 20–24 years are combined; for all ages, ages <15 is excluded and all remaining categories are combined | Incomplete DEPO primary-care sales data for 1998–2008 required these sales to be adjusted, and the average difference observed between the trends over the 1998–2008 period and over the entire period was added to the original sales values | ||||||
Abbreviations: DEPO, Depo-Provera; IMP, Implanon; IUD, Intrauterine device; LARC, long-acting reversible contraceptives; MIR, Mirena; NEXP, Nexplanon; NOR, Noristerat.
Table S2.
Estimated average duration of LARC use
| LARC | Expected length of use in years (cycles) | Annual removal rate (% of women)
|
Average duration (number of years) | Average duration (number of cycles) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Year 6 | Year 7 | Year 8 | ||||
| MIR | 5 (60) | 25.3% | 13.3% | 8.4% | 6.0% | 3.9% | n/a | n/a | n/a | 3 | 37 |
| IMP/NEXP | 3 (36) | 22.5% | 14.5% | 9.0% | n/a | n/a | n/a | n/a | n/a | 2 | 29 |
| IUD† | 8 (96) | 21.6% | 13.4% | 11.8% | 9.1% | 5.7% | 1.0% | 1.0% | 1.0% | 4 | 51 |
| DEPO | 0.3 (3) | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 0.3 | 3 |
| NOR | 0.2 (2) | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 0.2 | 2 |
Notes:
Based on T-Safe CU380A. Reproduced from: National Collaborating Centre for Women’s and Children’s Health. Long-Acting Reversible Contraception. NICE Clinical Guideline No.30. London: RCOG Press; 2013, with the permission of the Royal College of Obstetricians and Gynaecologists.1
Abbreviations: DEPO, Depo-Provera; IMP, Implanon; IUD, Intrauterine device; LARC, long-acting reversible contraceptive; MIR, Mirena; NEXP, Nexplanon; NOR, Noristerat.