Abstract
Background
Ethnic disparities in metabolic disease risk may be the result of differences in circulating adipokines and inflammatory markers related to ethnic variations in obesity and body fat distribution.
Subjects/Methods
In a cross-sectional design, we compared serum levels of leptin, adiponectin, C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α) in control subjects (321 men and 930 women) from two nested case-control studies conducted within the Multiethnic Cohort Study consisting of whites, Japanese Americans (JA), Latinos, African Americans (AA), and Native Hawaiians (NH). General linear models were applied to evaluate ethnic differences in log-transformed serum biomarker levels before and after adjusting for body mass index (BMI) at cohort entry.
Results
In comparison to whites, significant ethnic differences were observed for all biomarkers except TNF-α. JA men and women had significantly lower leptin and CRP levels than whites and JA women also had lower adiponectin levels. Leptin was significantly higher in AA women (p<0.01), adiponectin was significantly lower in AA men and women (p=0.02 and p<0.001), and CRP and IL-6 were significantly higher in AA men and women. Lower adiponectin (p<0.0001) and CRP (p=0.03) levels were the only biomarkers in NH women that differed from whites; no statistically significant differences were seen for NH men and for Latino men and women. When adjusted for BMI at cohort entry, the differences between the lowest and highest values across ethnic groups decreased for all biomarkers except adiponectin in men indicating that ethnic differences were partially due to weight status.
Conclusions
These findings demonstrate ethnic variations in circulating adipokine and CRP levels before and after adjustment for BMI. Given the limitation of BMI as a general measure of obesity, further investigation with visceral and subcutaneous adiposity measures are warranted to elucidate ethnicity-related differences in adiposity in relation to disparities in obesity-related disease risk.
Keywords: body mass index, ethnicity, leptin, adiponectin, inflammatory markers, C-reactive protein
INTRODUCTION
Obesity is closely linked to the development of diabetes, cardiovascular disease, and cancer1-4 and also related to chronic systemic low-grade inflammation marked by altered circulating levels of adipokine and inflammatory markers.5,6 Thus, adipose tissue, consisting of adipocytes, immune cells, and nerve/connective tissue, is now recognized as an important endocrine and metabolically-active organ. The pro-inflammatory phenotype associated with excess fat mass results in low production of adiponectin and high production of leptin, C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α).5 Interestingly, the pro-inflammatory response appears to differ depending on body fat distribution. Because visceral adipose tissue (VAT) surrounds the internal organs and is more vascular and metabolically active than subcutaneous adipose tissue (SAT), VAT accumulation is thought to be more health hazardous, i.e., increased risks of insulin resistance and related metabolic diseases, than abdominal or peripheral SAT.7 Central adiposity differs by sex and ethnicity,8-10 in particular Asian ethnicity is associated with higher VAT and African American (AA) ethnicity with lower VAT relative to whites.10-12 These variations in adipose tissue composition appear to be linked to ethnic disparities in obesity-related chronic diseases, such as higher rates of diabetes among Japanese Americans (JA) or AA at similar body mass index (BMI) levels.13,14 The hypothesis is that differences in circulating adipokines and inflammatory markers as a result of ethnic differences in the distribution of adipose tissue are partially responsible for these ethnic disparities in obesity-related disease.10,12
In a cross-sectional design, we measured leptin, adiponectin, CRP, IL-6, and TNF-α in fasting serum samples within a multiethnic population of older men and women consisting of whites, JA, Latinos, AA, and Native Hawaiians (NH). We compared circulating levels of these biomarkers across ethnic groups before and after adjustment for body mass index (BMI) to evaluate the plausibility of ethnic differences in biomarker levels due to differences in body fat distribution independent of weight status.
MATERIALS AND METHODS
Study population
This analysis used data collected from control subjects, free of cancer, who participated in nested case-control studies of breast cancer and non-Hodgkin lymphoma (NHL) conducted within the Multiethnic Cohort Study (MEC).15-17 The MEC is a longitudinal study designed to investigate the association of dietary, lifestyle, and genetic factors with the incidence of cancer and other chronic diseases. The cohort was assembled in Hawaii and Los Angeles in 1993-1996, and details on recruitment and baseline information have been reported previously.15 Briefly, subjects from 5 main ethnic groups (whites, JA, Latinos, AA, and NH) were identified primarily through drivers’ license files, supplemented with voter registration lists in Hawaii and Medicare files in California, and were recruited by mailing a self-administered, 26-page questionnaire on diet, anthropometric measures, medical history, family history of cancer, and lifestyle. A total of 215,251 men and women aged 45 to 75 years were included at baseline and formed a representative group of the general population as verified by a comparison of the cohort distributions across educational levels and marital status with corresponding census data for the two geographical areas.15 The study protocol was approved by the Institutional Review Boards of the University of Hawaii and the University of Southern California.
In 1999-2003, a short follow-up questionnaire (Qx2) was sent to all MEC members to update information on body weight and medical conditions; due to deaths and refusal, only 85% of cohort members completed the questionnaire. A prospective MEC biospecimen subcohort was established in 2001-2006 by asking surviving cohort members to provide specimens of blood and urine.18 Of eligible MEC members alive at the time and asked to participate in the biospecimen collection, close to half (67,594 individuals) provided samples. For 95% of the participants, fasting blood samples (≥8 hours) were obtained; the respective proportion for the current analysis was 92%. Blood samples were processed within 4 hours of collection, aliquoted into 0.5-mL cryotubes, and stored in the vapor phase of liquid nitrogen (-186°C) for 5-10 years. When comparing the characteristics at cohort entry of individuals who provided specimens with those who did not, the latter were older by an average of 3 years, had less education, and were more likely to be current smokers. However, there was no substantial difference by several demographic characteristics and cancer risk factors including BMI, dietary fat and vegetable intake, physical activity, and family history of cancer, suggesting that the biospecimen repository participants are broadly representative of the cohort members.
For the breast cancer nested case-control study,16 one control for each case diagnosed before December 31, 2009, for whom a pre-diagnostic blood specimen was available, was randomly selected from the eligible pool of postmenopausal women who were alive and free of breast cancer at the age of the case's diagnosis. Similarly, two matching cases were chosen for each case of NHL.17 The controls were matched on year of birth (± one year), location (Hawaii or California), ethnicity, date of blood draw (± 6 months), time of blood draw (±2 hours), hours fasting before blood draw (0-<6, 6-<8, 8-<10, or ≥10), and hormone replacement therapy use at blood draw (current vs. not current). After excluding six women, for whom baseline BMI was outside the plausible range of 15-50 kg/m2, a total of 321 men and 930 women were included in the current analysis. Because subjects were primarily selected from a nested case-control on breast cancer, a greater number of women than men were part of the analysis. The mean time interval between cohort entry and blood collection was 9 years.
Laboratory assays
All assays were performed by the Analytical Biochemistry Shared Resource at the University of Hawaii Cancer Center as reported for the original nested-case control studies following the manufacturer's protocol unless noted otherwise.16,19 Briefly, frozen serum samples were retrieved from the MEC biorepository and analyzed in duplicate to quantify leptin and adiponectin using double-antibody enzyme-linked-immunosorbent-assay (ELISA; R&D Systems, Minneapolis, MN, U.S.A.). CRP was assessed using a Cobas MiraPlus clinical chemistry analyzer (Roche Diagnostics, Indianapolis, IN) and a latex particle enhanced immunoturbidimetry based kit from Pointe Scientific (Lincoln Park, MI). The Luminex panel included IL-6 and TNF-α, which were measured using a slight modification of an Invitrogen (Carlsbad, CA) magnetic high sensitivity 10-plex assay (LHC0001) and Luminex 200 plate reader.16,19 As reported previously16,19 intra-batch coefficients of variation based on 96 blinded duplicate and 9 triplet samples for leptin, adiponectin, CRP, IL-6, and TNF-α were 3.4 -6.4%, 2.5-9.4 %, 3.5-5.0%, 8.9%, and 10.0%, respectively.
Statistical analyses
SAS software version 9.3 (SAS Institute, Inc., Cary, NC) was used to perform all statistical analyses with a two-sided p value of <0.05 considered statistically significant. Participant characteristics, such as age at blood draw, fasting hours prior to blood draw, and BMI, smoking, and diabetes status at cohort entry, were compared across ethnic categories to identify potential confounding factors using generalized linear models (Proc GLM) for continuous variables and chi-square or Fisher's exact tests for categorical variables. Spearman rank order correlation coefficients (r) were calculated between serum biomarker levels and BMI at cohort entry to assess their linear relationships. Generalized linear models were applied to evaluate ethnic differences in serum adipokine and CRP levels, with whites serving as the reference category, and adjusted for BMI at cohort entry (continuous), as well as for month of blood draw (categorical) to account for seasonal variations in biomarker levels and laboratory batch number (categorical) to correct for possible difference across batches. Serum biomarkers and BMI were log-transformed to satisfy model assumptions. Further adjustment for additional characteristics, including age at blood draw, fasting hours prior to blood draw, smoking status, and diabetes status, did not materially impact the results and, therefore, these variables were not included in the final models. Sensitivity analyses were conducted among 93% of men (N=299) and 91% of women (N=849) who had provided weight information approximately 3 years prior to blood draw as part of Qx2. BMI information at the time of the blood draw was only available for 32% of the study participants. Additionally, stratified analyses were performed to compare mean inflammatory biomarker levels across ethnic groups within each weight category defined as normal (<25 kg/m2), overweight (25-<30 kg/m2), or obese (≥30 kg/m2). Due to limited sample size (N=19), stratified analyses excluded NH men.
RESULTS
Of the 321 male participants, 31% were whites, 26% were JA, 19% were Latinos, 19% were AA, and 6% were NH (Table 1). Of the 930 female participants, 22% were whites, 33% were JA, 21% were Latinos, 15% were AA, and 9% were NH. In both men and women, statistically-significant ethnic differences were observed for mean BMI at cohort entry (p<0.05). In men, compared to whites, BMI was lower in JA (24.9 vs. 26.5 kg/m2) and higher in Latinos, AA, and NH (27.5, 27.2, and 29.1 kg/m2, respectively). Similarly, in women, JA had a lower mean BMI than whites (23.8 vs. 25.2 kg/m2) while all other ethnic groups had higher mean BMIs than whites (27.8, 28.9, and 28.0 kg/m2 for Latinos, AA, and NH, respectively). Age at blood draw, fasting hours prior to blood draw, smoking status at cohort entry, or diabetes status at cohort entry did not differ across ethnic groups in either men or women, except that NH women were slightly younger at blood draw. In the entire MEC population, overall proportions of self-reported current smoking at cohort entry (16%) and diabetes status (12 %), as well as mean BMI (26.5 kg/m2), were similar to those of the current study population (data not shown).
Table 1.
Participant characteristics and serum biomarker levels by sex and ethnicitya
| Male (N=321) | Female (N=930) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| White | Japanese American | Latino | African American | Native Hawaiian | White | Japanese American | Latino | African American | Native Hawaiian | ||
| N | 100 (31%) | 82 (26%) | 60 (19%) | 60 (19%) | 19 (6%) | 207 (22%) | 309 (33%) | 194 (21%) | 140 (15%) | 80 (9%) | |
| Age at blood draw (year) | 69.9±8.5 | 70.1±9.5 | 70.8±6.5 | 69.9±5.7 | 69.3±5.3 | 69.1±7.9 | 68.3±7.9 | 67.9±6.6 | 69.5±7.0 | 66.6±7.1b | |
| Fasting hours prior to blood draw (hours) | 12.5±3.5 | 12.0±3.5 | 11.8±5.2 | 11.7±5.6 | 10.6±5.1 | 12.7±2.2 | 13.2±7.4 | 12.6±3.6 | 12.6±4.5 | 12.7±3.7 | |
| Body mass index at cohort entry (kg/m2) | 26.5±3.6 | 24.9±3.2b | 27.5±3.5 | 27.2±4.0 | 29.1±4.0b | 25.2±4.8 | 23.8±3.7b | 27.8±4.7b | 28.9±5.8b | 28.0±5.1b | |
| Current smoking at cohort entry | 10 (10 %) | 6 (7 %) | 6 (10 %) | 8 (13%) | 0 (0 %) | 21 (10%) | 19 (6%) | 12 (6%) | 22 (16 %) | 11 (14%) | |
| Diabetes at cohort entry | 0 (0%) | 5 (6%) | 1 (2%) | 8 (13%) | 2 (11%) | 4 (2%) | 25 (8%) | 22 (11%) | 14 (10%) | 5 (6%) | |
| Serum biomarker | |||||||||||
| Leptin (ng/mL) |
Unadjusted | 10.2 (8.4-12.0) | 5.5 (4.6-6.5)b | 9.9 (8.0-11.7) | 11.7 (8.6-14.7) | 10.9 (6.9-14.9) | 25.7 (22.8-28.6) | 15.0 (13.9-16.2)b | 32.7 (28.9-36.4) | 45.7 (39.5-52.0)b | 28.9 (24.7-33.2) |
| BMI-adjusted | 7.5 (6.6-8.5) | 5.6 (4.8-6.4)b | 7.1 (6.0-8.3) | 7.7 (6.6-9.1) | 6.1 (4.5-8.2) | 20.4 (18.7-22.2) | 15.3 (14.2-16.5)b | 21.1 (19.2-23.0) | 26.2 (23.5-29.1)b | 19.0 (16.5-21.8) | |
| Adiponectin (μg/mL) |
Unadjusted | 8.7 (7.6-9.9) | 7.2 (6.0-8.3) | 8.2 (7.1-9.3) | 7.1 (5.4-8.8)b | 8.9 (6.7-11.1) | 16.1 (14.7-17.5) | 11.7 (10.6-12.8)b | 12.7 (11.6-13.8) | 11.0 (9.4-12.6)b | 9.3 (7.8-10.8)b |
| BMI-adjusted | 7.2 (6.3-8.2) | 5.7 (4.9-6.6)b | 7.4 (6.3-8.8) | 5.5 (4.6-6.5)b | 8.3 (6.1-11.1) | 12.6 (11.5-13.8) | 8.0 (7.3-8.6)b | 11.9 (10.8-13.1) | 9.6 (8.6-10.8)b | 8.5 (7.3-9.9)b | |
| Leptin:adiponectin ratio (ng/μg) |
Unadjusted | 3.0 (0.9-5.1) | 1.3 (0.9-1.6)b | 1.6 (1.3-2.0) | 2.9 (2.0-3.9)b | 2.0 (0.7-3.3) | 3.3 (2.6-3.9) | 2.7 (2.4-3.1) | 3.9 (3.3-4.5) | 9.8 (4.9-14.6)b | 4.5 (3.7-5.4) |
| BMI-adjusted | 1.4 (1.2-1.7) | 1.2 (1.0-1.6) | 1.2 (0.9-1.5) | 1.0 (0.5-1.6) | 1.9 (1.5-2.3) | 2.2 (1.9-2.5) | 2.5 (2.2-2.8) | 2.2 (1.9-2.5) | 3.6 (3.2-4.2)b | 2.7 (2.2-3.3) | |
| C-reactive protein (mg/L) |
Unadjusted | 3.1 (2.3-4.0) | 1.6 (1.0-2.1)b | 3.5 (2.4-4.6) | 4.0 (3.1-5.0)b | 2.5 (1.1-3.9) | 3.6 (3.0-4.2) | 2.0 (1.6-2.3)b | 4.2 (3.6-4.8) | 5.4 (4.5-6.3) | 3.3 (2.5-4.2)b |
| BMI-adjusted | 2.1 (1.7-2.5) | 1.1 (0.8-1.5)b | 2.3 (1.7-2.9) | 2.9 (2.3-3.7)b | 1.4 (0.8-2.3) | 2.7 (2.3-3.0) | 1.6 (1.4-1.8)b | 2.8 (2.4-3.1) | 3.2 (2.8-3.7) | 2.0 (1.6-2.5)b | |
| Interleukin-6 (pg/mL) |
Unadjusted | 4.1 (2.6-5.7) | 7.8 (1.9-13.8) | 4.0 (1.7-6.2) | 46.3 (1.5-91.1)b | 5.5 (−0.5-11.6) | 12.1 (2.0-22.1) | 7.8 (5.0-10.7) | 9.3 (4.4-14.2) | 17.9 (1.8-34.0) | 9.8 (2.3-17.2) |
| BMI-adjusted | 2.3 (1.7-3.0) | 2.2 (1.5-3.0) | 2.2 (1.4-3.1) | 5.0 (3.6-6.8)b | 2.8 (1.4-5.2) | 3.6 (3.0-4.2) | 3.3 (2.9-3.8) | 3.8 (3.2-4.5) | 4.6 (3.8-5.6) | 4.1 (3.1-5.2) | |
| Tumor necrosis factor-α (pg/mL) |
Unadjusted | 10.1 (1.3-19.0) | 8.0 (4.1-11.8) | 6.1 (2.8-9.5) | 54.0 (−6.0-113.9) | 10.7 (2.9-18.6) | 19.7 (12.3-27.0) | 19.2 (6.5-32.0) | 52.2 (10.4-93.9) | 27.7 (7.4-48.1) | 38.4 (−7.3-84.1) |
| BMI-adjusted | 3.7 (2.8-4.8) | 3.5 (2.6-4.7) | 3.1 (2.1-4.3) | 5.3 (3.8-7.3) | 5.9 (3.2-10.2) | 7.5 (6.3-9.0) | 7.4 (6.4-8.6) | 9.2 (7.7-11.1) | 9.2 (7.3-11.4) | 8.7 (6.5-11.6) | |
Data are presented as mean±SD or N (%) except for serum biomarkers, which are shown in mean (lower-upper confidence limits) or geometric mean (lower-upper confidence limits) after adjustment for body mass index; percentages may not add to 100 due to rounding. Men had missing data for fasting hours prior to blood draw (N=3); leptin (N=1); leptin:adiponectin ratio (N=1); and C-reactive protein (N=2), and women had missing data for fasting hours prior to blood draw (N=3). Comparisons of ethnic groups were performed using generalized linear model (continuous variables) with or without adjustment for body mass index (BMI) or chi-square/Fisher's exact test (categorical variables); BMI and biomarker measures were log-transformed to satisfy model assumptions.
P value < 0.05 for difference in mean values from white (reference group).
Serum biomarker levels were generally higher in women than in men (Table 1); most notably, leptin and TNF-α levels were 2-4 fold higher. Serum leptin levels (Table 2) were highly positively correlated with baseline BMI in both sexes and all ethnic groups, with correlations ranging from r=0.52 for Latinos to r=0.71 for JA in men and from r=0.50 for NH to r =0.69 for whites in women (p<0.05 for all). On the other hand, serum adiponectin levels were inversely related with BMI and only statistically significant in women (p<0.01). The leptin:adiponectin ratio was positively associated with BMI in men and women (p<0.01 for both). Serum CRP levels also showed modest correlations with BMI in men and women (p<0.01 for both), whereas serum IL-6 levels were only associated in women (p<0.01) and serum TNF-α levels only inversely correlated in men (p<0.05).
Table 2.
Correlations (Spearman coefficients) between serum adipocytokine levels and body mass index at cohort entry by ethnicity
| Malea | Female | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | White | Japanese American | Latino | African American | Native Hawaiian | All | White | Japanese American | Latino | African American | Native Hawaiian | |
| N | 321 | 100 | 82 | 60 | 60 | 19 | 930 | 207 | 309 | 194 | 140 | 80 |
| Leptin | 0.63b | 0.57b | 0.71b | 0.52b | 0.64b | 0.59b | 0.67b | 0.69b | 0.62b | 0.57b | 0.58b | 0.50b |
| Adiponectin | −0.10 | −0.16 | −0.19 | −0.12 | −0.01 | −0.11 | −0.32b | −0.41b | −0.38b | −0.40b | −0.28b | −0.09 |
| Leptin:adiponectin ratio | 0.51b | 0.50b | 0.62b | 0.40b | 0.38b | 0.33 | 0.61b | 0.64b | 0.57b | 0.61b | 0.53b | 0.36b |
| C-reactive protein | 0.24b | 0.22b | 0.29b | −0.03 | 0.17 | 0.11 | 0.39b | 0.30b | 0.21b | 0.32b | 0.40b | 0.32b |
| Interleukin-6 | 0.04 | 0.15 | 0.02 | −0.15 | −0.18 | 0.34 | 0.12b | 0.04 | 0.11 | 0.07 | 0.14 | −0.05 |
| Tumor necrosis factor-α | −0.15b | −0.05 | −0.23b | −0.28b | −0.11 | 0.05 | −0.01 | −0.16b | 0.02 | 0.01 | −0.02 | −0.10 |
Data were missing for leptin (N=1), leptin:adiponectin ratio (N=1), and C-reactive protein (N=2) for men.
P value < 0.05
In univariate comparisons, significant ethnic differences were observed for all biomarkers except TNF-α (Table 1). As compared to whites, JA men and women had significantly lower leptin and CRP levels, and JA women also had lower adiponectin levels. Leptin was significantly higher in AA women (p<0.01), adiponectin was significantly lower in AA men and women (p=0.02 and p<0.001), and CRP and IL-6 were significantly higher in AA men and women. Lower adiponectin (p<0.0001) and CRP (p=0.03) were the only biomarkers in NH women that differed from whites; no statistically significant differences were seen for NH men and Latino men and women. When adjusted for BMI at cohort entry, the differences between the lowest and highest values across ethnic groups decreased for all biomarkers except adiponectin in men. For example, the difference of 30.7 ng/mL in leptin between AA and JA women was reduced to 11.1 ng/mL after adjustment for BMI indicating that the higher levels in AA were partially due to their higher BMI. In addition, the lower serum adiponectin levels were significant for both JA men and women (p=0.03 and p<0.0001) in models that included BMI.
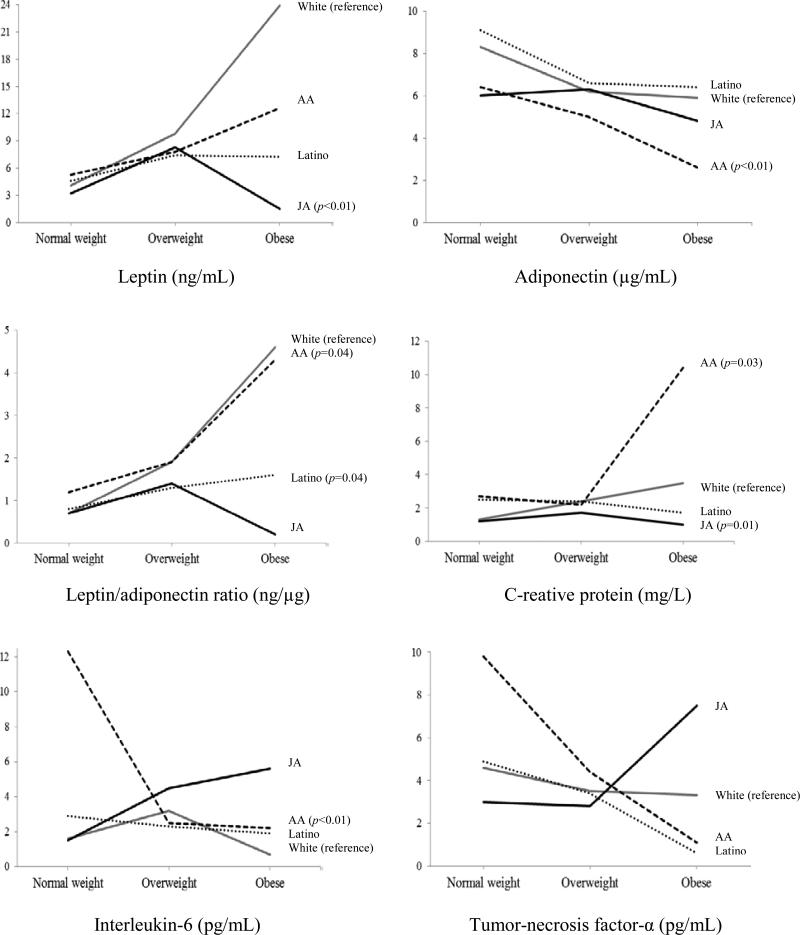
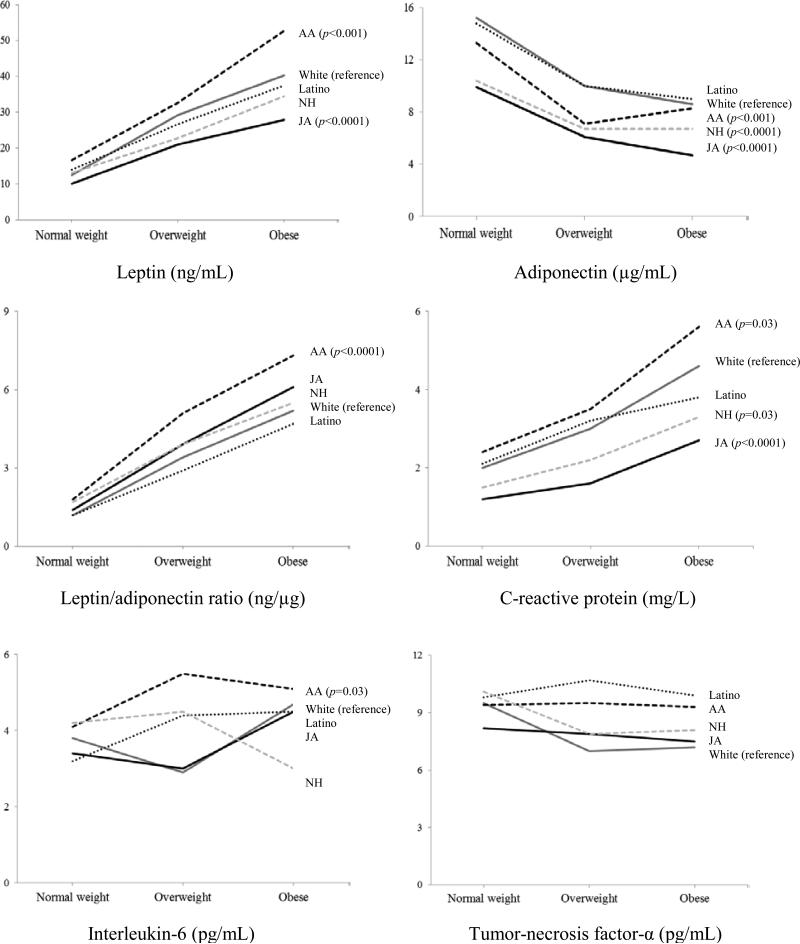
In the fully adjusted models stratified by weight status (Figures 1 and 2 and Supplemental Tables 1 and 2), JA women had significantly lower levels of leptin, adiponectin, and CRP than whites, whereas AA women had higher levels of leptin, CRP, and IL-6 as well as lower levels of adiponectin. The mean values for NH were generally between those for JA and white women but only significantly different from whites for adiponectin and CRP and those for Latinas were close to whites. The patterns in men were less distinct due to their smaller numbers but similar differences in biomarker levels were generally observed for JA and AA men as for women. Sensitivity analyses using the more recent BMI values generally observed similar ethnic differences as the analyses using BMI at cohort entry (data not shown).
Figure 1.
Geometric mean biomarker levels by ethnicity across weight categories in men after adjustment for log-transformed continuous BMI, month of blood draw (categorical), and laboratory analysis batch number (categorical). White = gray solid line; Japanese American (JA) = black solid line; Latino = black dotted line; and African American (AA) = black short-dash line. Native Hawaiians are not included due to the limited sample size (N=19). P values in parentheses present significant differences from whites (reference group) after adjustment for log-transformed body mass index (continuous), month of blood draw (categorical), and laboratory analysis batch number (categorical).
Figure 2.
Geometric mean biomarker levels by ethnicity across weight categories in women after adjustment for log-transformed continuous BMI, month of blood draw (categorical), and laboratory analysis batch number (categorical). White = gray solid line; Japanese American (JA) = black solid line; Latino = black dotted line; African American (AA) = black short-dash line; and Native Hawaiian (NH) = gray short-dash line. P values in parentheses present significant differences from whites (reference group) after adjustment for log-transformed body mass index (continuous), month of blood draw (categorical), and laboratory analysis batch number (categorical).
DISCUSSION
In this cross-sectional study among a multiethnic population of older men and women with a wide range of BMI levels, ethnic differences in serum adipokine and CRP levels were detected in men and women. As compared to whites, leptin levels were lower in JA men and women and higher in AA women, adiponectin levels were lower in AA men and women and in JA and NH women, CRP was lower in JA men and women as well as in NH women and higher in AA men and women after taking into account BMI. The fact that the ethnic differences in biomarkers were only reduced and not eliminated after including BMI suggests that part of the ethnic differences are due to other causes, e.g., the relative proportions of VAT vs. SAT, genetics, or lifestyle factors, although BMI explains a large proportion of the ethnic differences in biomarker levels. Despite a mean time interval of 9 years between BMI at cohort entry and blood collection, leptin was strongly associated with baseline BMI and a sensitivity analysis with BMI values collected 3 years before the blood draw detected similar associations. The current findings add to the limited data supporting the presence of ethnic variations in circulating adipokine levels, which may be the result of differences in body composition and body fat distribution that lead to disparities in obesity-related diseases.13,14 Higher levels of biomarkers in women than men reflect their higher proportion of adipose tissue and may also contribute to variations in obesity-related disease risks.
The current findings in postmenopausal women are in agreement with our previous report among a small sample of premenopausal women,10 which described lower serum levels of leptin, adiponectin, and CRP in JA than white women after adjustment for BMI. Therefore, the lower circulating levels of these biomarkers in JA women seem consistent across menopausal status and sex. Support for the hypothesis that lower adiponectin levels may reflect higher proportions of VAT in JA as compared to whites across weight categories comes from a small study of MEC women who underwent dual energy X-ray absorptiometry (DXA) and abdominal magnetic resonance imaging (MRI) scans. JA women were noted to have higher percentages of abdominal VAT than white women with similar BMIs.11 A study measuring total body fat by bioelectrical impedance analysis, also reported lower adiponectin levels in JA and Chinese American than white women after adjustment for waist circumference.20 Our results in AA women agree with a previous study that detected higher unadjusted IL-6 and CRP levels in AA than white women12 and a report of higher leptin and lower adiponectin levels in AA than white women, but not in AA men who only showed lower adiponectin levels.20 This raises the possibility that AA are more prone to a state of inflammation given similar BMI levels and more likely to develop chronic conditions associated with inflammation. The higher IL-6 levels previously observed in Hispanic women12 disagree with the lack of differences in our Latino women.
Since adiponectin is thought to play a favorable pathophysiological role in obesity-related diseases,21 the current evidence supports the idea that adiponectin is partially responsible for ethnic-specific disparities in obesity-related diseases.13,14 The possible relation with body fat distribution was strengthened by a study showing that variations in VAT and SAT measured by computed tomography (CT) partially explained the differences in biomarker levels across ethnic groups.12 However, the presence of additional confounding factors was indicated by statistically significant associations for Hispanics and AA after adjustment for VAT and SAT. Therefore, ethnic differences in levels of adipokine and inflammatory marker, if they truly exist, are unlikely to be fully explained by differences in common measures of general adiposity and body fat distribution, such as BMI and waist circumference. To further elucidate the underlying mechanisms for ethnic-specific differences in biomarker levels, future studies need to examine specific fat depots or adipocyte morphology that are not traditionally measured in epidemiologic studies, specifically, liver fat, superficial vs. deep SAT, adipocyte size or adipocyte hypertrophy22-24 and understand the important influence of genetic and lifestyle factors on adiposity.25-28
There are several strengths to the present study. The multiethnic population allowed comparisons across ethnic groups with a broad range of BMI levels. The population-based, large-scale cohort design strengthened the generalizability of study results. There were also important limitations to note. Since no measures of adiposity other than self-reported BMI were available, we were not able to explore whether the ethnic differences were related to variations in adiposity, especially the relative proportion and distribution of VAT vs. SAT. Moreover, anthropometric measurements at the time of blood draw were unavailable for a majority of participants, but the sensitivity analysis with BMI information from Qx2 collected 3 years before the blood draw did not indicate major changes in weight status over time. In comparison to previous reports,29-32 serum leptin levels in our study population were relatively high. Nevertheless, we observed similar ethnic differences, such as higher concentrations in African Americans than Whites,31 and low levels in Japanese.33 Younger age and lower BMIs may partially explain the observed differences in leptin levels.10,31,32 In addition, differences in analytic methods (ELISA vs. RIA), standards provided by the company, and volume used for the assays may have contributed to the absolute concentrations of leptin reported in different studies. Caution needs to be exercised when interpreting the results of the stratified analyses by weight category; the number of participants was small in several ethnic-specific BMI categories, especially in men. Finally, the fact that the current study population consisted of the controls in nested-case control studies of NHL and breast cancer, although taken from a large population-based cohort, may limit the representativeness of our findings to the general population.
In conclusion, the current findings suggest that ethnic differences in circulating adipokine and CRP levels are present to a similar extent in men and women even after accounting for differences in weight status. Ethnic-specific modifiers of metabolic activity in adipose tissue or genetic variations may contribute to our findings of ethnic differences in biomarkers. Given the limitation of BMI as a measure of adiposity that does not account for differences in the distribution of adipose tissue, additional VAT and SAT measures, ideally from CT or MRI, will be needed and are planned by our group to understand the relation between ethnicity and adiposity on circulating adipokines and other obesity-related biomarkers.
Supplementary Material
ACKNOWLEDGEMENTS
The Multiethnic Cohort Study has been supported by grants R37 CA 54281, R01 CA 63464, P01 CA033619, and UM1 CA164973 from the National Cancer Institute. Partial support was also provided by NCI grant P01 CA138338. SMC and NJO had been supported by Postdoctoral Training grant R25 CA 90956 from NCI. The Analytical Biochemistry Shared Resource of the University of Hawaii Cancer Center is supported, in part, by grant P30 CA71789 from NCI. The authors thank William Cooney and Jennifer Lai for their technical performance of serum biomarker assays.
Footnotes
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
SUPPLEMENTARY INFORMATION
Supplementary tables are available at the journal's website.
REFERENCES
- 1.Fujimoto WY. The importance of insulin resistance in the pathogenesis of type 2 diabetes mellitus. Am J Med. 2000;108(Suppl 6a):9S–14S. doi: 10.1016/s0002-9343(00)00337-5. [DOI] [PubMed] [Google Scholar]
- 2.Yehuda-Shnaidman E, Schwartz B. Mechanisms linking obesity, inflammation and altered metabolism to colon carcinogenesis. Obes Rev. 2012;13:1083–1095. doi: 10.1111/j.1467-789X.2012.01024.x. [DOI] [PubMed] [Google Scholar]
- 3.Rose DP, Haffner SM, Baillargeon J. Adiposity, the metabolic syndrome, and breast cancer in African-American and white American women. Endocr Rev. 2007;28:763–777. doi: 10.1210/er.2006-0019. [DOI] [PubMed] [Google Scholar]
- 4.Fantuzzi G. Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 2005;115:911–919. doi: 10.1016/j.jaci.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 5.Harford KA, Reynolds CM, McGillicuddy FC, Roche HM. Fats, inflammation and insulin resistance: insights to the role of macrophage and T-cell accumulation in adipose tissue. Proc Nutr Soc. 2011;70:408–417. doi: 10.1017/S0029665111000565. [DOI] [PubMed] [Google Scholar]
- 6.Bulcao C, Ferreira SR, Giuffrida FM, Ribeiro-Filho FF. The new adipose tissue and adipocytokines. Curr Diabetes Rev. 2006;2:19–28. doi: 10.2174/157339906775473617. [DOI] [PubMed] [Google Scholar]
- 7.Hocking S, Samocha-Bonet D, Milner KL, Greenfield JR, Chisholm DJ. Adiposity and Insulin Resistance in Humans: The Role of the Different Tissue and Cellular Lipid Depots. Endocr Rev. 2013 doi: 10.1210/er.2012-1041. [DOI] [PubMed] [Google Scholar]
- 8.Patel PS, Buras ED, Balasubramanyam A. The role of the immune system in obesity and insulin resistance. J Obes. 2013;2013:616193. doi: 10.1155/2013/616193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6(Suppl 1):60–75. doi: 10.1016/j.genm.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conroy SM, Chai W, Lim U, Franke AA, Cooney RV, Maskarinec G. Leptin, Adiponectin, and Obesity among Caucasian and Asian Women. Mediators Inflamm. 2011;2011:253580. doi: 10.1155/2011/253580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim U, Ernst T, Buchthal SD, Latch M, Albright CL, Wilkens LR, et al. Asian women have greater abdominal and visceral adiposity than Caucasian women with similar body mass index. Nutr Diabetes. 2011;1:e6. doi: 10.1038/nutd.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carroll JF, Fulda KG, Chiapa AL, Rodriquez M, Phelps DR, Cardarelli KM, et al. Impact of race/ethnicity on the relationship between visceral fat and inflammatory biomarkers. Obesity (Silver Spring) 2009;17:1420–1427. doi: 10.1038/oby.2008.657. [DOI] [PubMed] [Google Scholar]
- 13.Maskarinec G, Erber E, Grandinetti A, Verheus M, Oum R, Hopping BN, et al. Diabetes incidence based on linkages with health plans: the multiethnic cohort. Diabetes. 2009;58:1732–1738. doi: 10.2337/db08-1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Resnick HE, Valsania P, Halter JB, Lin X. Differential effects of BMI on diabetes risk among black and white Americans. Diabetes Care. 1998;21:1828–1835. doi: 10.2337/diacare.21.11.1828. [DOI] [PubMed] [Google Scholar]
- 15.Kolonel LN, Henderson BE, Hankin JH, Nomura AM, Wilkens LR, Pike MC, et al. A multiethnic cohort in Hawaii and Los Angeles: baseline characteristics. Am J Epidemiol. 2000;151:346–357. doi: 10.1093/oxfordjournals.aje.a010213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ollberding NJ, Kim Y, Shvetsov YB, Wilkens LR, Franke AA, Cooney RV, et al. Prediagnostic leptin, adiponectin, C-reactive protein, and the risk of postmenopausal breast cancer. Cancer Prev Res (Phila) 2013;6:188–195. doi: 10.1158/1940-6207.CAPR-12-0374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morimoto Y, Conroy SM, Ollberding NJ, Henning SM, Franke AA, Wilkens LR, et al. Erythrocyte membrane fatty acid composition, serum lipids, and non-Hodgkin's lymphoma risk in a nested case-control study: the multiethnic cohort. Cancer Causes Control. 2012;23:1693–1703. doi: 10.1007/s10552-012-0048-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park SY, Wilkens LR, Henning SM, Le ML, Gao K, Goodman MT, et al. Circulating fatty acids and prostate cancer risk in a nested case-control study: the Multiethnic Cohort. Cancer Causes Control. 2009;20:211–223. doi: 10.1007/s10552-008-9236-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Conroy SM, Maskarinec G, Morimoto Y, Franke AA, Cooney RV, Wilkens LR, et al. Non-hodgkin lymphoma and circulating markers of inflammation and adiposity in a nested case-control study: the multiethnic cohort. Cancer Epidemiol Biomarkers Prev. 2013;22:337–347. doi: 10.1158/1055-9965.EPI-12-0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khan UI, Wang D, Sowers MR, Mancuso P, Everson-Rose SA, Scherer PE, et al. Race-ethnic differences in adipokine levels: the Study of Women's Health Across the Nation (SWAN). Metabolism. 2012;61:1261–1269. doi: 10.1016/j.metabol.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsuzawa Y. Adiponectin: a key player in obesity related disorders. Curr Pharm Des. 2010;16:1896–1901. doi: 10.2174/138161210791208893. [DOI] [PubMed] [Google Scholar]
- 22.Kohli S, Sniderman AD, Tchernof A, Lear SA. Ethnic-specific differences in abdominal subcutaneous adipose tissue compartments. Obesity (Silver Spring) 2010;18:2177–2183. doi: 10.1038/oby.2010.94. [DOI] [PubMed] [Google Scholar]
- 23.Anand SS, Tarnopolsky MA, Rashid S, Schulze KM, Desai D, Mente A, et al. Adipocyte hypertrophy, fatty liver and metabolic risk factors in South Asians: the Molecular Study of Health and Risk in Ethnic Groups (mol-SHARE). PLoS One. 2011;6:e22112. doi: 10.1371/journal.pone.0022112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azuma K, Curb JD, Kadowaki T, Edmundowicz D, Kadowaki S, Masaki KH, et al. Ethnic difference in liver fat content: a cross-sectional observation among Japanese American in Hawaii, Japanese in Japan, and non-Hispanic whites in United States. Obes Res Clin Pract. 2013;7:e198–e205. doi: 10.1016/j.orcp.2011.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lara-Castro C, Hunter GR, Lovejoy JC, Gower BA, Fernandez JR. Apolipoprotein A-II polymorphism and visceral adiposity in African-American and white women. Obes Res. 2005;13:507–512. doi: 10.1038/oby.2005.53. [DOI] [PubMed] [Google Scholar]
- 26.Mente A, Meyre D, Lanktree MB, Heydarpour M, Davis AD, Miller R, et al. Causal Relationship between Adiponectin and Metabolic Traits: A Mendelian Randomization Study in a Multiethnic Population. PLoS One. 2013;8:e66808. doi: 10.1371/journal.pone.0066808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mente A, Razak F, Blankenberg S, Vuksan V, Davis AD, Miller R, et al. Ethnic variation in adiponectin and leptin levels and their association with adiposity and insulin resistance. Diabetes Care. 2010;33:1629–1634. doi: 10.2337/dc09-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lara-Castro C, Hunter GR, Lovejoy JC, Gower BA, Fernandez JR. Association of the intestinal fatty acid-binding protein Ala54Thr polymorphism and abdominal adipose tissue in African-American and Caucasian women. J Clin Endocrinol Metab. 2005;90:1196–1201. doi: 10.1210/jc.2004-0676. [DOI] [PubMed] [Google Scholar]
- 29.Rossi IA, Bochud M, Bovet P, Paccaud F, Waeber G, Vollenweider P, et al. Sex difference and the role of leptin in the association between high-sensitivity C-reactive protein and adiposity in two different populations. Eur J Epidemiol. 2012;27:379–384. doi: 10.1007/s10654-012-9671-0. [DOI] [PubMed] [Google Scholar]
- 30.Ruhl CE, Everhart JE, Ding J, Goodpaster BH, Kanaya AM, Simonsick EM, et al. Serum leptin concentrations and body adipose measures in older black and white adults. Am J Clin Nutr. 2004;80:576–583. doi: 10.1093/ajcn/80.3.576. [DOI] [PubMed] [Google Scholar]
- 31.Lilja M, Rolandsson O, Shaw JE, Pauvaday V, Cameron AJ, Tuomilehto J, et al. Higher leptin levels in Asian Indians than Creoles and Europids: a potential explanation for increased metabolic risk. Int J Obes (Lond) 2010;34:878–885. doi: 10.1038/ijo.2010.19. [DOI] [PubMed] [Google Scholar]
- 32.Ruhl CE, Everhart JE. Leptin concentrations in the United States: relations with demographic and anthropometric measures. Am J Clin Nutr. 2001;74:295–301. doi: 10.1093/ajcn/74.3.295. [DOI] [PubMed] [Google Scholar]
- 33.Nakamura Y, Ueshima H, Okuda N, Miura K, Kita Y, Okamura T, et al. Relation of dietary and lifestyle traits to difference in serum leptin of Japanese in Japan and Hawaii: the INTERLIPID study. Nutr Metab Cardiovasc Dis. 2012;22:14–22. doi: 10.1016/j.numecd.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.