Abstract
Background
Firefighters have twice as many cardiovascular deaths as police officers and four times as many as emergency medical responders. The etiology for this high prevalence remains unknown. The electrocardiogram (ECG) is a widely used tool to screen populations at risk, but yet there are no available on-duty, high-resolution electrocardiographic (ECG) recordings.
Objective
We sought to evaluate the prevalence of clinical and ECG risk factors among on-duty professional firefighters during 12-lead ECG holter monitoring and exercise stress testing.
Methods
Firefighters were recruited from Surveying and Assessing Firefighters Fitness and ECG (SAFFE) study. This descriptive study recruited firefighters from 7 firehouses across Western New York area, who all completed on-duty, 24-hour Holter ECG monitoring and a standard exercise stress test. All analyses were completed by a reviewer blinded to all clinical data.
Results
112 firefighters (age 44±8 years, mostly white males) completed the study. Even though all firefighters were in normal sinus rhythm, over half of them had at least one high risk ECG risk factor present, including abnormal sympathetic tone (elevated heart rate, 54%), abnormal repolarization (wide QRS-T angle, 25%), myocardial scaring (fragmented QRS, 24%), and myocardial ischemia (ST depression, 24%). In addition, most firefighters tolerated the treadmill exercise stress test well (metabolic equivalent tasks 11.8+2.5), however, almost one third had abnormal stress tests that require further evaluation to rule out subclinical coronary artery disease.
Conclusion
Among on-duty professional firefighters, high risk ECG markers of fatal cardiac events and abnormal stress test results that warrant further evaluation are prevalent. Annual physical checkups with routine 12-lead ECG can identify those who might benefit from preventive cardiovascular services.
Keywords: Electrocardiogram, Firefighters, Risk Stratification
INTRODUCTION
In 2005, the National Fire Protection Association reported that 44% of on-duty firefighter fatalities were due to sudden cardiac death.1 Two years later, Kales and colleagues2 confirmed that 45% of on-duty firefighter deaths were cardiac related so that many are actually dying of cardiac disease rather than of fire-related injuries. On-duty firefighters have twice as many cardiovascular deaths as police officers and four times as many as emergency medical responders.2 The exact etiology why this unique population has relatively higher risk for cardiovascular events is unknown. We previously reported on the prevalence of metabolic syndrome, coronary artery disease, sleep deprivation, binge drinking behaviors, and overall poor mental well-being among professional firefighters,3–5 all of which are known to increase the risk for cardiovascular events. To date, despite the high cardiac risk for firefighters and its societal importance, there are no available high resolution field recordings of the electrocardiogram (ECG) during firefighting activities. Consequently, the aim of this study was to evaluate the prevalence of clinical and ECG risk factors among on-duty professional firefighters.
METHODS
Subjects for this study were recruited from Surveying & Assessing Firefighters Fitness & Electrocardiogram (SAFFE) study between 2008 and 2010. SAFFE Study was a cross-sectional descriptive study that recruited professional firefighters from Western New York (WNY) area. Out of 13 accessible firehouses in WNY area, the research team travelled across seven of these firehouses and professional firefighters were approached while on-duty to participate in the study. Research equipment and supplies were moved from one firehouse to the other to allow all eligible firefighters equal chances for voluntary participation. Since professional firefighters have a physician clearance to be on-duty, no exclusion criteria were applied. Firefighters in WNY area undergo a one-time physical assessment prior to becoming firefighters, and then get enrolled in an optional occupational health monitoring program in a county hospital. Firefighters who consented to participate anonymously completed paper-and-pencil surveys, and then in a private bunk room, research personnel obtained anthropometric measures (i.e., height, weight, abdominal circumference and abdominal height) and vital signs (i.e., baseline blood pressure and heart rate). Two blood pressure readings were taken 5-minute apart after resting in chair for 5-minutes. Each firefighter then completed a symptom-limited standard Bruce exercise treadmill test (ETT), followed by ambulatory 12-lead ECG holter recording for 24 hours. The ECG monitoring was done continuously during all firefighting, exercising, eating, sleeping and leisure activities. A registered nurse was made available in the firehouse during the ETT testing and later 24/7 by phone to respond to all technical difficulties firefighters might encounter with the equipment during the holter monitoring. The nurse also accompanied firefighters during numerous fire and medical responses to keep a log of all response activities. Firefighters received grocery gift cards for completing both the ECG recording and ETT and returning the equipment. The study was approved by the appropriate Institutional Review Board of the State University of New York.
ECG Recording & Analysis
Using H12+ Holter recorders (V3.12; Mortara Instruments, Milwaukee, WI), 12-Lead ECGs were recorded. To optimize signal quality, the firefighters’ skin was shaved, rubbed with alcohol wipes until thoroughly cleaned, and briskly dried with gauze to stimulate capillary flow. Disposable electrodes were applied in the Mason-Likar lead configuration under the firefighters’ uniformed t-shirts and the Holter was secured to their uniformed belt. All leads were simultaneously acquired at a high resolution (1000 samples per second), resulting in high fidelity recordings with a frequency response of 0.05 to 60 Hz. All ECG recordings were then downloaded to a laptop computer equipped with H-Scribe 4 software (Mortara Instrument) for ECG processing and analysis. First, all ECGs were manually annotated to delete noise and artifact by a reviewer blinded to all clinical data. Second, the computer software automatically computed the necessary ECG metrics and exported them to an excel sheet for final analysis. More importantly, high-frequency ECG waveform features like notching in the QRS complex can be missed with the standard upper filter setting of 60 Hz, thus the first 10-second ECG tracing of the 24-hour monitoring period was exported into a portable document format with the standard filter setting at 0.05 to 150 Hz using the ELI LINK program (Mortara Instruments) for subsequent analysis. Table 1 summarizes the high-risk ECG parameters that were computed in the current analysis.
Table 1.
The Definitions of high-risk ECG parameters used in the current analysis
| Variable | Definition | Cutoff for Cardiac Events |
Clinical Significance |
|---|---|---|---|
| Heart Rate | Average R-R interval of all QRS complexes during the whole duration of the recording |
>75 beats / minute 17 | Poor sympathetic tone |
|
QRS duration |
Averaged QRS onset to QRS offset duration of all leads on the standard 10- second ECG |
>120 milliseconds 18 | Abnormal conduction / myocardial damage |
| QTc interval | Averaged QRS onset to T offset interval of all leads on the standard 10- second ECG, corrected for heart rate using Bazett formula |
>470 milliseconds (women); or >450 milliseconds (men) 19 |
Abnormal global repolarization |
| LVH | The presence of this pattern on the standard 10-second ECG using Cornell voltage criteria |
>20 millimeters (women); or >23 millimeters (men) 20 |
Myocardial strain |
| LBBB | The presence of this pattern on the standard 10-second ECG using AHA criteria |
Present 21 | Abnormal conduction / myocardial damage |
| fQRS | RSR morphology; >2 R`; or notching in the nadir of S wave with a narrow QRS (<120 millisecond); or > 2 R` or > 2 notches in the nadir of S wave with a widened QRS |
Present 22 | Myocardial scaring |
| QRS-T angle | The three-dimensional spatial angle between the mean R and T vectors estimated directly from the 12-lead ECG |
>100 °12 | Dispersed repolarization |
| Q waves | Two or more pathologic Q wave (0.04 second wide and ¼ R wave deep) in one territory |
Present 23 | Myocardial scaring |
| HRV | Standard deviation of all normal-to-normal R-R intervals (SDNN) for the recording |
<100 24 | Poor sympathetic tone |
| ST Event | The presence of at least one episode of ST depression of >0.5 mm in leads V2-V3 or >1mm in all other leads in ≥2 contiguous leads for at least five minutes at any time |
Present 25 | Transient myocardial ischemia |
| PVC | The presence of frequent premature ventricular contractions at rate of ≥10 / hour for the duration of holter recording |
Present 18 | Vulnerability to fatal arrhythmia |
| NSVT | At least one episode of ≥3 consecutive ventricular beats at a rate of >120 beats/minute |
Present 18 | Vulnerability to fatal arrhythmia |
Abbreviations. LVH: left ventricular hypertrophy; LBBB: Left Bundle Branch Block; fQRS: fragmented QRS complex; HRV: heart rate variability; PVC: premature ventricular contraction; NSVT: non-sustained ventricular tachycardia
Exercise Treadmill Testing
Eligible firefighters completed a standard Bruce protocol ETT using X-Scribe™ stress testing system (Mortara Instruments). The system wirelessly acquires diagnostic-quality ECGs during treadmill testing and displays these ECGs on a high-definition computer screen monitor. The system displays real-time 12-lead ECG signal during the exercise test. The system also computes a signal-averaged ST-T complex for each ECG lead for real-time, automated baseline comparison during the ETT. This highly sensitive feature allows clinicians to easily recognize even minor stress-induced ST segment and slope changes for real-time or offline analyses. The X-Scribe system also automatically measured blood pressure readings at 5-minute intervals and continuously measures oxygen saturation during test and recovery. Of note, firefighters were kept on the treadmill as long as they could tolerate, even if they exceeded their maximum heart rate (symptom-limited exercise). All analyses were completed by a reviewer blinded to research data. According to the current clinical guidelines,6 the presence of exercise-induced, horizontal ST depression ≥ 2 mm in ≥ 2 contagious leads for ≥ 30 seconds at peak or recovery of ETT was considered indicative of underlying coronary artery disease and positive ETT test. ST depression ≥ 1 mm but < 2 mm was considered non-conclusive ETT test and indicative of further evaluation.
Statistical Analysis
All analyses were conducted using Statistical Package for Social Sciences (SPSS v 21.0 for Windows) and p< 0.05 was considered statistically significant. Dynamic variables are reported as mean ± standard deviation (SD) and categorical variables as n (%). Comparison between groups was completed using Independent Samples t-test for dynamic variables and chi-square for categorical variables.
RESULTS
One hundred and twelve (n=112) firefighters were enrolled in the SAFFE study (age = 43.6±7.7 years, 96% men, 81% white), Table 2. Almost half (49%) of the firefighters were overweight and more than 40% were obese (BMI≥30 kg/m2) with more than half (55%) have a waist circumference > 100 centimeters, a predictor of insulin resistance. Systolic and diastolic blood pressure readings were slightly elevated, but within pre-hypertensive stage. One third of firefighters were in the diagnostic range of hypertension, but only <20% were being treated. In addition, 13% were active smokers, 3% had a history of coronary artery disease or a coronary intervention, and 9% had a respiratory disease (i.e., asthma, chronic obstructive pulmonary disease (COPD), or sleep apnea).
Table 2.
Baseline Demographic and Anthropometric Characteristics (n=112)
| Characteristic | |
|---|---|
| Age (years) | 43.6±7.7 |
| Male Sex (n, %) | 107 (95.5%) |
| Race (n, %) | |
| White | 91 (81%) |
| Black | 15 (13.4%) |
| Years as a firefighter | 15.5±7.0 |
| Body Mass Index (BMI, kg/m2) | 29.5±4.1 |
| Normal (BMI<25) | 11 (9.8%) |
| Overweight (25<BMI<30) | 55 (49.1%) |
| Obese (30<BMI<35) | 38 (33.9%) |
| Very Obese (BMI>35) | 8 (7.1%) |
| Waist Circumference (cm) | 101.3±11.8 |
| Central Obesity (>100 cm) | 63 (56.3%) |
| Abdominal Height (cm) | 22.7±4.4 |
| Blood Pressure (mmHg) | |
| Systolic | 129.3±14.9 |
| Diastolic | 81.8±10.6 |
| BP >140/90 | 35 (31.3%) |
| Past Medical History (n, %) | |
| Hypertension | 20 (17.9%) |
| Hyperlipidemia | 9 (8.0%) |
| Coronary artery disease | 3 (2.7%) |
| Asthma or COPD | 5 (4.4%) |
| Sleep Apnea | 5 (4.4%) |
| Smoking History (n, %) | |
| Active smoker | 14 (12.5%) |
| Previous smoker | 13 (11.6%) |
ECG Characteristics
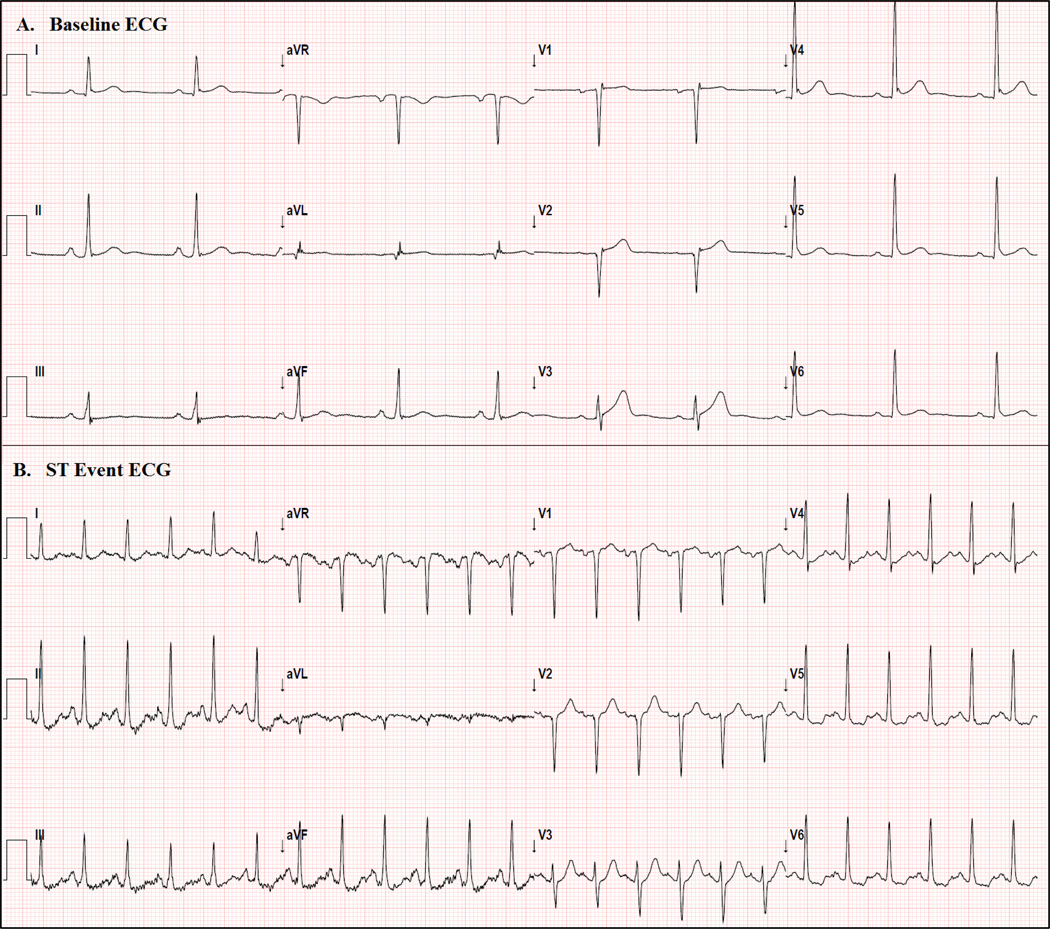
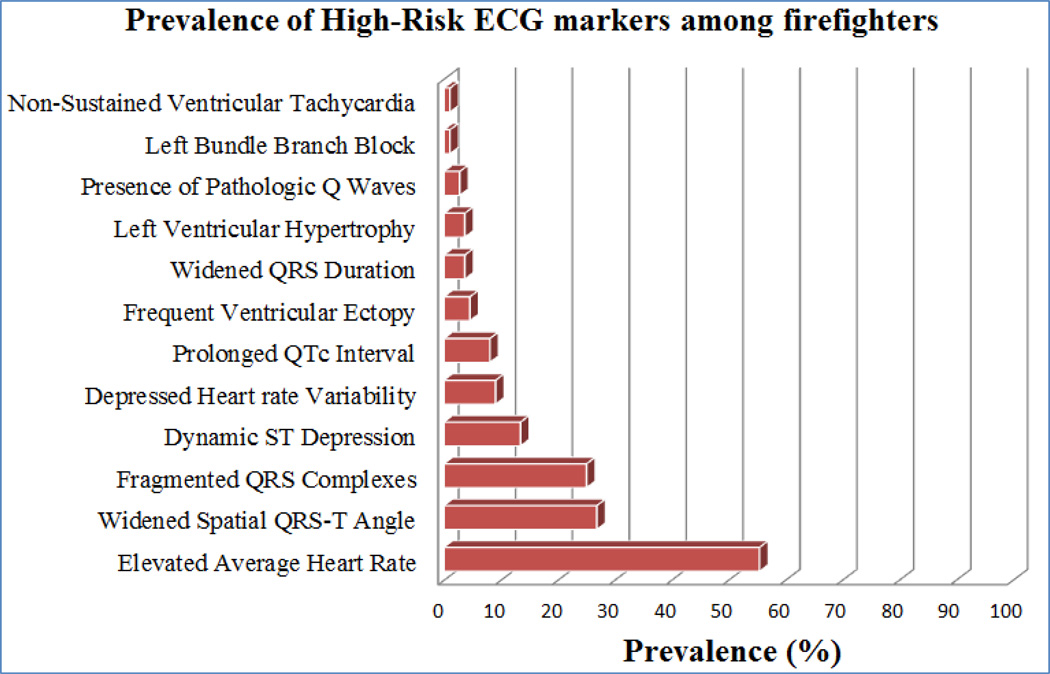
Confirming our pilot study, 7 the quality of the ECG data was ample for arrhythmia and myocardial ischemia interpretation (Figure 1). All firefighters were in normal sinus rhythm and on-duty heart rates (HR) ranged from minimum of 47±7 beats per minute (bmp) to maximum of 143±21 bpm. Although no lethal arrhythmias occurred, non-sustained ventricular tachycardia (NSVT) did occur once. Many firefighters exceeded the cutoff point for cardiovascular risk for many ECG risk factors (Figure 2). Among the 12 high-risk ECG markers analyzed in this study, NSVT occurred the least frequently while more than half of the firefighters had accelerate average heart rates over 24-hour monitoring period. There was no interactions between firefighters’ demographic (i.e., age and sex) and clinical (i.e., BMI, waist circumference, blood pressure, past and medical history) characteristics and the incidence of any high-risk ECG parameters.
Figure 1. Resting 12-Lead ECG in a Professional Firefighter while on duty.
(A) Shows the baseline ECG of 44 year-old white male at the beginning of holter monitoring;
(B) Shows the ST segment changes during a response to a fire call.
Figure 2. Prevalence of High-Risk ECG markers among firefighters.
This figure shows the prevalence of high-risk ECG markers of cardiac death among professional firefighters.
Exercise Treadmill Testing Characteristics
Almost all firefighters (n=110, 98%) successfully completed a symptom-limited ETT using a standard Bruce protocol. On average, it took each firefighter 12 min (4th stage Bruce protocol, speed 4.2 mph with 16% grade) to achieve 93% of the maximum HR. Findings were diagnostic of myocardial ischemia in nearly 13 (11.6%) firefighters and inconclusive findings that warrant further investigation were seen in approximately 21 (19%) more firefighters (Table 3). There were no age, sex, or clinical differences between those who passed or failed the ETT. On average, trends of blood pressure peak and recovery were normal, with most increase seen in the systolic blood pressure (+40 mmHg) at peak. Oxygen saturation, measured with continuous pulse oximetry probe on the index finger, was normal (≥94%) during start and recovery, with eight firefighters (7%) showing desaturation (<90%) at peak of ETT.
Table 3.
Characteristics of the Exercise Treadmill Test
| ETT Test Findings |
||||
|---|---|---|---|---|
| Test Characteristic | All (n = 110) | Normal Test (n = 76, 70%) |
Inconclusive or Abnormal Test (n = 34, 30%) |
p |
| Summary Measures | ||||
| Total Test Time (minutes) | 11.5±3.0 | 11.1+3.3 | 12.4+2.2 | 0.02 |
| Target HR (beats/minute) | 176.5±7.6 | 177.4+8.2 | 174.5+5.6 | NS |
| % Achieved of Target HR (%) | 92.7±7.5 | 91.2+7.2 | 96.0+7.0 | 0.01 |
| Max Treadmill Speed (miles/hour) | 4.5±0.7 | 4.4+0.8 | 4.6+0.6 | NS |
| Max Treadmill Incline (%) | 17.0±3.6 | 16.6+2.2 | 17.8+5.5 | NS |
| Max Metabolic Equivalent Task (MET) | 11.8±2.5 | 11.5+2.7 | 12.6+1.8 | 0.01 |
| Heart Rate Measures | ||||
| Initial | 79.1+12.6 | 80.8+11.4 | 76.1+14.3 | NS |
| Test-Peak | 166.1±18.2 | 163.5+18.2 | 171.2+17.2 | 0.03 |
| 2-minute Recovery | 135.4+20.3 | 133.5+20.4 | 139.6+19.6 | NS |
| Blood Pressure Measures | ||||
| Initial (Systolic) | 129.9±15.5 | 129.6+16.8 | 130.8+12.4 | NS |
| Initial (Diastolic) | 79.0±11.4 | 78.8+11.3 | 79.5+12.0 | NS |
| Test-Peak (Systolic) | 167.9±27.5 | 166.5+27.9 | 171.6+26.5 | NS |
| Test-Peak (Diastolic) | 77.0±13.9 | 77.9+13.4 | 75.2+15.0 | NS |
| 2-minute Recovery (Systolic) | 152.2±23.9 | 150.9+22.6 | 155.0+26.6 | NS |
| 2-minute Recovery (Diastolic) | 75.2±15.4 | 76.1+15.6 | 73.4+15.2 | NS |
| Oxygen Saturation Measures | ||||
| Initial (%) | 97.3±1.3 | 97.3+1.3 | 97.4+1.2 | NS |
| Test-Peak (%) | 92.3±4.4 | 92.9+4.2 | 91.3+4.7 | NS |
| 2-minute Recovery (%) | 96.1±1.6 | 95.8+1.8 | 96.5+1.1 | NS |
ETT=exercise treadmill testing, NS=not statistically significant, bold values=statistically significant
DISCUSSION
Our findings demonstrate that high-risk ECG markers of fatal cardiac events and abnormal stress test results that warrant further evaluation are prevalent. We were successful in obtaining diagnostic-quality ECGs for arrhythmia and ischemia detection in this middle-age, high-risk population. To our knowledge, this is the first study to record high-resolution 12-lead ECGs of professional firefighters while on duty. Over half of the firefighters had at least one high-risk ECG risk factor and almost one third had abnormal stress tests. Of note, more than 75% of on-duty fatalities in the US are older than 45 years 8 and nearly one half (47%) of our sample was in that age group.
ECG Markers of Mortality
An elevated average 24 hour HR, an indicator of poor sympathetic tone,9 was seen in over 50% of the sample. This finding is consistent with on-duty firefighter’s activities that are strenuous and often require firefighters to work at their maximal HR for prolonged periods or even beyond, as seen in this study. However, the depressed heart rate variability (HRV) seen in nearly 10% of these firefighters provides more specific insights about how such abnormalities in heart rate fluctuation can increase the risk of cardiac death. Depressed HRV indicates autonomic dysfunction and increased risk of fatal arrhythmic events.10 A more ominous finding is the presence of a widened QRS-T angle in nearly 25% of the sample. The spatial angle between mean R and T vectors denote abnormal repolarization and underlying cardiac pathology. 11 An abnormal angle has a larger hazard ratio for fatal cardiac events than other established risk factors.12 Another prevalent marker was fragmented QRS complexes seen in nearly 20% of our sample. This high-risk ECG pattern indicates myocardial scaring and is also strongly correlated with subsequent cardiac events in clinical populations.13 Of note, nearly one fifth of our sample is known to have a past cardiac history. Another known marker of death is dynamic ST depression that was prevalent in more than 10% of our sample. ST depression indicates subclinical myocardial ischemia in asymptomatic adults and can be a key for identifying those at greater risk who might benefit from early treatment.14 Similarly, nearly 12%–30% of firefighters had abnormal stress test results that might indicate subclinical coronary artery disease. Finally, nearly 8% of firefighters had a prolonged QTc interval, a historically known risk factor of fatal arrhythmic events.15 Other high-risk ECG marker were not prevalent but remain a strong prognostic marker of subsequent cardiac events, including left bundle branch block (1%) and non-sustained ventricular tachycardia (1%).
Firefighters and the Risk of Cardiovascular Mortality
Compared to other first responders, firefighters are at increased risk for cardiovascular events.1 Previous retrospective studies showed that firefighters with a past medical history of coronary artery disease, active smokers, and those who have hypertension are at excess risk for on duty cardiac events.16 In this study, only 3% of firefighters had a prior history of coronary artery disease, but nearly 10% had undiagnosed high blood pressure and 13% were active smokers. Even though we did not find any correlations between these clinical characteristics and other high risk holter or stress ECG findings, but our results indicate that nearly 12%–30% of firefighters might have subclinical coronary artery disease that might explain the increased risk for on-duty cardiac events in this high risk population. Of note, literature indicates that fire suppression activities are associated with the highest risk of mortality among firefighters, these fire suppression activities increase the risk approximately 10 to 100 times as high as that for nonemergency firefighting duties.2 This indicates that future efforts need to focus more on studying the relationship between thermal stress and the pathogenesis of coronary artery disease, which might provide interesting and important insights about this phenomenon. Finally, given that firefighters often undergo a one-time physical assessment prior to becoming firefighters, primary prevention programs need to focus on mandatory annual physical checkups to screen for cardiovascular risk factors (i.e., subclinical coronary artery disease and untreated hypertension) and other incentive programs that can encourage firefighters to quit smoking and stay in shape.
Conclusion
Firefighters are a unique population with many occupational health problems. In this study, we found that nearly 10% of firefighters had undiagnosed and untreated hypertension and approximately 30% had possible coronary artery disease, which is higher than what is typically expected among middle-age adults. Over half of these firefighters had at least one high risk ECG risk factor present, including abnormal sympathetic tone, abnormal repolarization, myocardial scaring, and myocardial ischemia. Annual physical check-ups with routine 12-lead ECG can identify those who might benefit from preventive cardiovascular services. This preliminary work may help develop a non-invasive risk stratification approach to better identify professional firefighters at risk for cardiovascular events. Over the longer horizon, algorithmic guidelines are needed to route at-risk firefighters for optimal and timely cardiac care.
Acknowledgments
Sponsored by a grant for the National Institute of Health (R21 NR-011077, MGC)
Footnotes
No Conflict of Interests
References
- 1.Fahy R. US firefights fatalities due to sudden cardiac death 1995–2004. National Fire Protection Association National Institute for Occupational Safety and Health (NIOSH); 2005. [Google Scholar]
- 2.Kales SN, Soteriades ES, Christophi CA, Christiani DC. Emergency duties and deaths from heart disease among firefighters in the United States. New England Journal of Medicine. 2007;356:1207–1215. doi: 10.1056/NEJMoa060357. [DOI] [PubMed] [Google Scholar]
- 3.Carey MG, Al-Zaiti SS, Liao LM, Martin HN, Butler RA. A Low-Glycemic Nutritional Fitness Program to Reverse Metabolic Syndrome in Professional Firefighters: Results of a Pilot Study. Journal of Cardiovascular Nursing. 2011;26:298–304. doi: 10.1097/JCN.0b013e31820344d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carey MG, Al-Zaiti SS, Dean GE, Sessanna L, Finnell DS. Sleep Problems, Depression, Substance Use, Social Bonding, and Quality of Life in Professional Firefighters. Journal of Occupational and Environmental Medicine. 2011;53:928–933. doi: 10.1097/JOM.0b013e318225898f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Zaiti S, Runco K, Carey M. Increased T-Wave Complexity Can Indicate Subclinical Myocardial Ischemia in Asymptomatic Adults. Journal of Electrocardiology. 2011;44:684–688. doi: 10.1016/j.jelectrocard.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibbons RJ, Balady GJ, Timothy Bricker J, et al. ACC/AHA 2002 guideline update for exercise testing: summary articleA report of the American college of cardiology/American heart association task force on practice guidelines (committee to update the 1997 exercise testing guidelines) 12345. Journal of the American College of Cardiology. 2002;40:1531–1540. doi: 10.1016/s0735-1097(02)02164-2. [DOI] [PubMed] [Google Scholar]
- 7.Carey MG, Thevenin BJ-M. High-Resolution 12-Lead Electrocardiograms of On-Duty Professional Firefighters: A Pilot Feasibility Study. J Cardiovasc Nurs. 2009;24:261–267. doi: 10.1097/JCN.0b013e3181a4b250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mbanu I, Wellenius GA, Mittleman MA, Peeples L, Stallings LA, Kales SN. Seasonality and coronary heart disease deaths in United States firefighters. Chronobiol Int. 2007;24:715–726. doi: 10.1080/07420520701535787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.ROBINSON BF, EPSTEIN SE, BEISER GD, BRAUNWALD E. Control of Heart Rate by the Autonomic Nervous System: Studies in Man on the Interrelation Between Baroreceptor Mechanisms and Exercise. Circulation Research. 1966;19:400–411. doi: 10.1161/01.res.19.2.400. [DOI] [PubMed] [Google Scholar]
- 10.Carney RM, Blumenthal JA, Stein PK, et al. Depression, Heart Rate Variability, and Acute Myocardial Infarction. Circulation. 2001;104:2024–2028. doi: 10.1161/hc4201.097834. [DOI] [PubMed] [Google Scholar]
- 11.Rautaharju PM, Prineas RJ, Zhang Z-M. A simple procedure for estimation of the spatial QRS/T angle from the standard 12-lead electrocardiogram. Journal of Electrocardiology. 2007;40:300–304. doi: 10.1016/j.jelectrocard.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Kors JA, Kardys I, van der Meer IM, et al. Spatial QRS-T angle as a risk indicator of cardiac death in an elderly population. Journal of Electrocardiology. 2003;36:113–114. doi: 10.1016/j.jelectrocard.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 13.Pietrasik G, Goldenberg I, Zdzienicka J, Moss AJ, Zareba W. Prognostic Significance of Fragmented QRS Complex for Predicting the Risk of Recurrent Cardiac Events in Patients With Q-Wave Myocardial Infarction. American Journal of Cardiology. 2007;100:583–586. doi: 10.1016/j.amjcard.2007.03.063. [DOI] [PubMed] [Google Scholar]
- 14.Deanfield JE, Shea M, Ribiero P, et al. Transient ST-segment depression as a marker of myocardial ischemia during daily life. The American Journal of Cardiology. 1984;54:1195–1200. doi: 10.1016/s0002-9149(84)80066-1. [DOI] [PubMed] [Google Scholar]
- 15.Webber DM, Montague TH, Bird NP. Meta-analysis of QTc interval - pooling data from heterogeneous trials. Pharmaceutical Statistics. 2002;1:17–23. [Google Scholar]
- 16.Geibe JR, Holder J, Peeples L, Kinney AM, Burress JW, Kales SN. Predictors of On-Duty Coronary Events in Male Firefighters in the United States. The American Journal of Cardiology. 2008;101:585–589. doi: 10.1016/j.amjcard.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Jouven X, Empana J-P, Schwartz PJ, Desnos M, Courbon D, Ducimetiere P. Heart-Rate Profile during Exercise as a Predictor of Sudden Death. New England Journal of Medicine. 2005;352:1951–1958. doi: 10.1056/NEJMoa043012. [DOI] [PubMed] [Google Scholar]
- 18.Goldberger JJ, Cain ME, Hohnloser SH, et al. AHA/ACC/HRS Scientific Statement on Noninvasive Risk Stratification Techniques for Identifying Patients at Risk for Sudden Cardiac Death: A Scientific Statement From the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. Circulation. 2008;118:1497–1518. [PubMed] [Google Scholar]
- 19.Straus S, Kors J, De Bruin ML, et al. Prolonged QTc Interval and Risk of Sudden Cardiac Death in a Population of Older Adults. Journal of the American College of Cardiology. 2006;47:362–367. doi: 10.1016/j.jacc.2005.08.067. [DOI] [PubMed] [Google Scholar]
- 20.Priori S, Aliot E, Blomstrom-Lundqvis C. Task Force on Sudden Cardiac Death of the European Society of Cardiology. European Heart Journal. 2001;22:1374–1450. doi: 10.1053/euhj.2001.2824. [DOI] [PubMed] [Google Scholar]
- 21.Surawicz B, Childers R, Deal BJ, Gettes LS. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part III: Intraventricular Conduction Disturbances A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. Journal of the American College of Cardiology. 2009;53:976–981. doi: 10.1016/j.jacc.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 22.Das MK, Zipes DP. Fragmented QRS: A predictor of mortality and sudden cardiac death. Heart Rhythm. 2009;6:S8–S14. doi: 10.1016/j.hrthm.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 23.Richardson K, Engel G, Yamazaki T, Chun S, Froelicher V. Electrocardiographic damage scores and cardiovascular mortality. Am Heart J. 2005;149:458–463. doi: 10.1016/j.ahj.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 24.Umetani K, Singer D, McCraty R, Atkinson M. Twenty-Four Hour Time Domain Heart Rate Variability and Heart Rate: Relations to Age and Gender Over Nine Decades Journal of the American College of Cardiology. 1998;31:593–601. doi: 10.1016/s0735-1097(97)00554-8. [DOI] [PubMed] [Google Scholar]
- 25.Holmvang L, Luscher M, Clemmensen P, Thygesen K, Grande P. Very Early Risk Stratification Using Combined ECG and Biochemical Assessment in Patients With Unstable Coronary Artery Disease (A Thrombin Inhibition in Myocardial Ischemia [TRIM] Substudy) Circulation. 1998;98:2004–2009. doi: 10.1161/01.cir.98.19.2004. [DOI] [PubMed] [Google Scholar]