Abstract
As da Vinci prostatectomy (dVP) grows in use, urologists continue to work to achieve improved sexual function while maintaining oncologic outcomes. This author set out to evaluate the impact of three different nerve-sparing techniques on not only 12-month and early erectile functional recovery but on negative margin rates as well. The author completed 400 dVP procedures, 300 of which were nerve-sparing. Series 1 utilized selective bipolar cautery for nerve sparing, series 2 used an athermal “clip and peel” posterior dissection technique, and series 3 used an athermal combined anterior and posterior dissection technique with clips and sharp dissection alone. Operative times, blood loss, and margin rates were recorded for all cases, and erectile function was measured by means of pre- and post-operative Sexual Health Inventory for Men (SHIM) score. For series 1, 2, and 3, the average total operative time was 111, 83, and 75 min, average console time was 78, 53, and 58 min, average blood loss was 125, 137, and 150 ml, respectively. Erections capable of intercourse at 3 months were seen in 14% of patients in series 1, 24% of the men in series 2, and 71% of the men in series 3. Negative margin rates were 78% for series 1, 76% for series 2, and 83% for series 3. Recovery of erectile function in the author’s dVP series favors an athermal technique. Short-term data on the combined anterior/posterior approach, including the preservation of the lateral prostatic fascia in the nerve sparing, was the superior of the two athermal techniques evaluated. In addition, this combined anterior and posterior method of nerve sparing using sharp dissection and clips also resulted in the lowest positive margin rates in the author’s series.
Keywords: Erectile function, Prostate cancer, Prostatectomy, Robotic
Introduction
Since the introduction of da Vinci robotics in 2000, its use in radical prostatectomy has gained in popularity. Although the learning curve for this procedure is reported to be less steep than that for laparoscopic prostatectomy, surgeons are still challenged in trying to achieve improved erectile functional outcomes while maintaining oncologic principles. The original description of the neurovascular bundles by Dr. Patrick Walsh [1] has lead to numerous other studies by laparoscopic and robotic surgeons, all in an effort to improve nerve sparing in laparoscopic and robotic prostatectomy. Data from Menon and Tewari [2–4] have demonstrated the presence of additional nerve fibers in the thin tissue layers surrounding the prostate. In their data, when these additional surrounding tissues are preserved along with the traditional neurovascular bundles, sexual function outcomes are improved. Data from Ahlering, Tewari, and others [4–6] show that if a completely athermal technique is used when performing nerve-sparing robotic prostatectomy, there is less thermal injury to the neurovascular bundles, and sexual function outcomes are improved. To the author’s knowledge, however, no group has specifically evaluated the impact of various robotic nerve-sparing techniques by a single surgeon on sexual function and negative margin rates. In this study, the author evaluated the impact of three different nerve-sparing techniques on early erectile functional recovery and negative margin rates.
Material and methods
A single surgeon performed 400 consecutive da Vinci radical prostatectomies. Those surgeries performed on patients with an age at surgery of less than 66, a pre-operative Sexual Health Inventory for Men (SHIM) score of greater than 14, and in whom a bilateral nerve-sparing surgery was performed were included in this data set. Bilateral nerve sparing was performed on patients with no palpable nodule on rectal exam, a PSA of less than ten, a Gleason score of less than eight, and with 50% or less of the sampled cores on each side positive for prostate cancer. da Vinci prostatectomy was performed in all cases using the standard transperitoneal approach described by Guillonneau et al. [7]. Data on all cases were collected and included patient demographics, total operative time, console time, estimated blood loss, pathologic stage, and margin status. Erectile functional outcomes were measured by pre- and post-operative SHIM scores. In addition, all patients followed a regimen of full-strength dosing of a PDE-5 inhibitor two times per week taken before bedtime. Erections capable of intercourse were defined as the ability to achieve vaginal penetration. The data sets involved the use of three different nerve-sparing techniques. Series 1 utilized selective bipolar cautery with the dissection of the neurovascular bundles beginning at the posterior aspect of the prostate and continuing with selective bipolar and sharp dissection caudally for nerve sparing. Series 2 used an athermal “clip and peel” posterior dissection technique whereby the initial plane was again developed along the posterior aspect of the prostate. In this series Weck hemoclips and sharp dissection alone were used for the initial dissection of the neurovascular bundles off the prostate without any use of cautery. The plane was then continued caudally, using mostly blunt dissection, peeling the neurovascular bundle away from the prostate. Series 3 used an athermal technique that included the dissection of the lateral prostatic fascia with the neurovascular bundles. For this series, a combined anterior and posterior dissection technique was used in which Weck clips and sharp dissection were applied without the use of cautery and with minimal blunt dissection. In this combined anterior/posterior approach, the initial plane was developed anteriorly with an incision being made high on the anterior aspect of the prostate around the 10 and 2 o’clock locations (Fig. 1). Sharp dissection was then utilized to continue the plane towards the posterior prostate about one third to halfway down the gland. A second plane was then created posteriorly using Weck hemoclips and sharp dissection. This posterior plane was continued up towards the anterior plane about one-third of the way along the posterior portion of the prostate (Fig. 2). The remaining attachments at the junction of the anterior and posterior planes were then connected using sharp dissection (Fig. 3), and the nerve preservation was completed (Fig. 4).
Fig. 1.
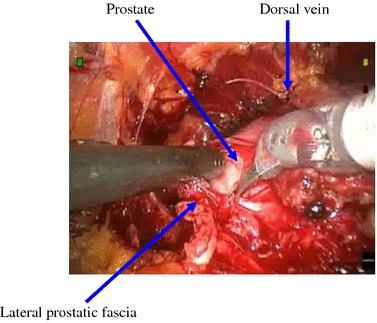
Creating the anterior plane for left-sided nerve-sparing
Fig. 2.
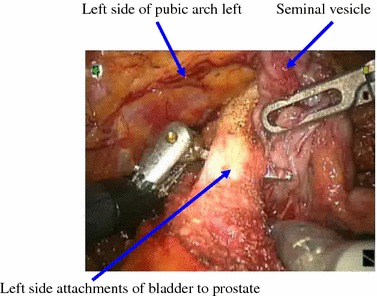
Creating the posterior plane for left-sided nerve sparing
Fig. 3.
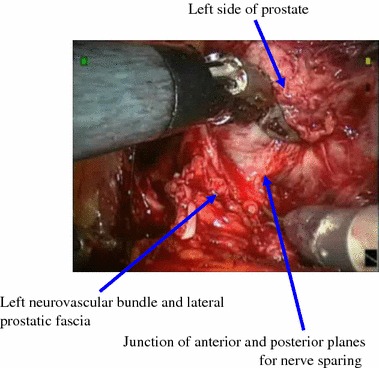
Connecting the anterior and posterior planes for left-side nerve sparing
Fig. 4.
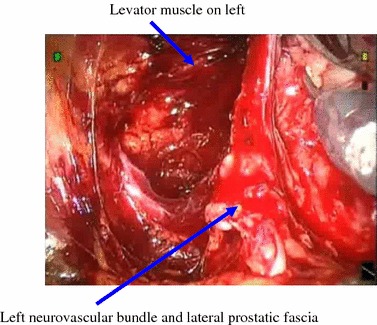
Completed left-sided nerve sparing
Results
Statistical analysis using ANOVA and Kruskal-Wallis tests were performed by a statistician on the data sets. For all three series there was not a statistically significant difference in age or pre-operative SHIM score with a P value of greater than 0.05 (Table 2). For series 1, 2, and 3, the average total operative time was 111, 83, and 75 min, the average console time was 78, 53, and 58 min, and the average blood loss 125, 137, and 150 ml, respectively (Table 1).
Table 2.
SHIM and urinary control outcomes
| Nerve-sparing technique | Median SHIM scorea pre-operative | Median SHIM score at 3 months | Median pads per day (no.) | Median age (years) |
|---|---|---|---|---|
| Bipolar | 25 | 5 | 0 | 56 |
| Athermal clip and peel | 25 | 5 | 0 | 56 |
| Athermal anterior/posterior | 25 | 20 | 0 | 59 |
aSHIM score, Sexual Health Inventory for Men score
Table 1.
Intraoperative data
| Nerve-sparing technique | Average total operative time (min) | Average console time (min) | Average blood loss (ml) |
|---|---|---|---|
| Bipolar | 111 | 78 | 125 |
| Athermal clip and peel | 83 | 53 | 137 |
| Athermal anterior/posterior | 75 | 58 | 150 |
For series 1, 2, and 3, the median age of the patients was 56, 56, and 59, respectively; for all three series of patients, the median pads per day were zero, and the median pre-operative SHIM score was 25. There was no statistically significant difference in age, pre-operative SHIM score, or post-operative urinary control between the three groups, as demonstrated by a P value of greater than 0.05 (Table 2). Final pathology revealed pT2 and pT3 tumors in 91.7 and 8.3% of the patients in series 1, 88.9 and 11.1% of the patients in series 2, and 88.3 and 11.7% of the patients in series 3, respectively. At 3 months post-operative, erections capable of intercourse were achieved by 14% of the men in series 1, 24% of the men in series 2, and 71% of the men in series 3. The difference in erectile functional outcomes, as measured by SHIM score, for the athermal technique versus selective bipolar was significant at a P value of less than 0.05. The difference in SHIM scores measured at 3 months in the two athermal nerve-sparing methods was also statistically significant at a P value of less than 0.05. The negative margin rate for series 1 was 78%, for series 2, 76%, and for series 3, 82% (Table 3).
Table 3.
Erectile functional outcomes
| Nerve-sparing technique | Erections capable of intercourse at 3 months (%) | Negative margin rate (%) |
|---|---|---|
| Bipolar | 14 | 78 |
| Athermal clip and peel | 24 | 76 |
| Athermal anterior/posterior | 70 | 83 |
Discussion
As we seek to do a better job of preserving our patient’s potency with robotic radical prostatectomy, we must remain cognizant of the fact that maximizing negative margin rates must remain the priority. We do not want to compromise our oncologic outcome in an effort to do a better job preserving potency. The concept of preservation of the investing tissue surrounding the prostate has been popularized by Menon and Tewari [2–4, 8]; in their data, when these additional surrounding tissues are preserved along with the traditional neurovascular bundles, sexual function outcomes are improved. Furthermore, in the hands of these highly experienced robotic surgeons, the preservation of these tissues did not result in increased positive margin rates. As other urologists with lesser robotic experience alter their nerve-sparing technique to preserve more of this investing tissue for the purpose of improving potency outcomes, it is critical that oncologic principles are not compromised in the process. In the author’s case series, there was a propensity for positive margins at the attachments of the prostate to the bladder and the lateral investing tissue when a blunt “peeling” method alone was used to develop the plane for separating the neurovascular tissue off the prostate. Commonly, the author found the area of greatest adherence of the prostate to the bladder and the neurovascular tissue at the 4 and 8 o’clock positions. By separating the antero-lateral and posterior investing tissue off the prostate using a combined anterior and posterior technique, the author approached this area of greatest adherence from two directions. When the area of adherence was then reached, the tissue above and below it was free. This gave the author better visualization of the plane between this limited area of adherent tissue and the prostate. When sharp dissection alone was then used to divide the remaining attachments at this location, pathologic examination revealed fewer capsular perforations, and negative margin rates were improved. In addition, by sparing more of the laterally investing tissue around the prostate with this method, sexual function outcomes were also improved.
Although rationale of how the use of this approach resulted in lower capsular perforation rates and hence better negative margins and how the preservation of more of the lateral investing tissue and it’s additional nerve fibers would result in better sexual function outcomes, the author acknowledges that the improved negative margins as well as the improved sexual function outcomes may be partially accounted for by the growing experience of the surgeon. Since the three series in this data set were performed in succession and not simultaneously, enhanced surgeon experience as the series progressed may account for some of the enhanced outcomes seen later in the data series. This critical point is further supported by looking at the author’s most recent 40 patients: these patients met the selection criteria outlined in this paper, had the combined anterior-posterior technique performed, but their sexual function data were not mature enough to be included at the time of submission. In these more recent 40 patients pathology revealed 90% of cancers were pT2, 10% were pT3, and the total negative margin rate for all patients was 92.5%.
As more urologists make the transition to performing robotic radical prostatectomy, we must remind ourselves that although robotics offers advantages to the surgeon and patient, it also brings with it unique challenges for the surgeon. Importantly, regardless of the advantages this technology affords, it is not a replacement for surgeon experience.
The reader is referred to references [9–23] for background material that is directly relevant to this article and which will provide more detailed information on the topics discussed herein.
Acknowledgments
Statistical analysis was performed by Charlie Johnson, PhD., Senior Manager of Bioinformatics, Asuragen.
References
- 1.Lepor H, Gregerman M, Crosby R, Mostofi FK, Walsh PC. Precise localization of the autonomic nerves from the pelvic plexus to the corpora cavernosa: a detailed anatomical study of the adult male pelvis. J Urol. 1985;133:207. doi: 10.1016/s0022-5347(17)48885-9. [DOI] [PubMed] [Google Scholar]
- 2.Tewari A, et al. Nerve sparing during robotic radical prostatectomy: use of computer modeling and anatomic data to establish critical steps and maneuvers. Curreny Urol Rep. 2005;6(2):126–128. doi: 10.1007/s11934-005-0080-8. [DOI] [PubMed] [Google Scholar]
- 3.Menon M, et al. Robotic radical prostatectomy with the “veil of aphrodite” technique: histologic evidence of enhanced nerve preservation. Eur Urol. 2006;49(6):1065–1073. doi: 10.1016/j.eururo.2006.02.050. [DOI] [PubMed] [Google Scholar]
- 4.Tewari A, et al. The proximal neurovascular plate and the tri-zonal neural architecture around the prostate gland: importance in the athermal robotic technique of nerve-sparing prostatectomy. Br J Urol. 2006;98(2):314–323. doi: 10.1111/j.1464-410X.2006.06266.x. [DOI] [PubMed] [Google Scholar]
- 5.Ahlering T, et al. Early potency outcomes with cautery free neurovascular bundle preservation with robotic laparoscopic radical prostatectomy. J Endourol. 2005;19(6):715–718. doi: 10.1089/end.2005.19.715. [DOI] [PubMed] [Google Scholar]
- 6.Ong AM. Nerve sparing radical prostatectomy: effects of hemostatic energy sources on the recovery of cavernous nerve function in a canine model. J Urol. 2004;172(4 Pt 1):1318–1322. doi: 10.1097/01.ju.0000139883.08934.86. [DOI] [PubMed] [Google Scholar]
- 7.Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris experience. J Urol. 2000;163:418. doi: 10.1016/S0022-5347(05)67890-1. [DOI] [PubMed] [Google Scholar]
- 8.Menon M, et al. Potency following robotic radical prostatectomy: a questionnaire based analysis of outcomes after conventional nerve sparing and prostatic fascia sparing techniques. J Urol. 2005;174(6):2291–2296. doi: 10.1097/01.ju.0000181825.54480.eb. [DOI] [PubMed] [Google Scholar]
- 9.Ahlering T, et al. Robotic radical prostatectomy: a technique to reduce pT2 positive margins. Urology. 2004;64(6):1224–1228. doi: 10.1016/j.urology.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Ahlering T, et al. Feasability study for robotic radical prostatectomy cautery-free neurovascular bundle preservation. Urology. 2005;65(5):994–997. doi: 10.1016/j.urology.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 11.Schuessler WW, Kavoussi LR, Clayman RV, Vancaille TH (1992) Laparoscopic radical prostatectomy: initial case report (abstract 130). J Urol 147:246A
- 12.Guillonneau B, Cathelineau X, Barret E, Rozet F, Vallancien G. Laparoscopic radical prostatectomy: technical and early oncological assessment of 40 operations. Eur Urol. 1999;36(1):14–20. doi: 10.1159/000019921. [DOI] [PubMed] [Google Scholar]
- 13.Singh A, Fagin RF, Shah G, Shekarriz B (2003) Anatomic bladder neck dissection technique in laparoscopic radical prostatectomy. Video presented at 21st world congress on endourology and SWL, vol 10.3. A303
- 14.Katz R, Salomon L, Hoznek A, de la Taille A, Antiphon P, Abbou CC. Positive surgical margins in laparoscopic radical prostatectomy: the impact of apical dissection, bladder neck remodeling and nerve preservation. J Urol. 2003;169:2049–2052. doi: 10.1097/01.ju.0000065822.15012.b7. [DOI] [PubMed] [Google Scholar]
- 15.Menon M, Tewari A, Baize B, Guillonneau B, Vallancien G. Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: the Vattikuti urology institute experience. Urology. 2002;60:864–868. doi: 10.1016/S0090-4295(02)01881-2. [DOI] [PubMed] [Google Scholar]
- 16.Menon M, Shrivastava A, Tewari A, Sarle R, Hemal A, Peabody JO, et al. Laparoscopic and robot assisted radical prostatectomy: establishment of a structured program and preliminary analysis of outcomes. J Urol. 2002;168:945–949. doi: 10.1016/S0022-5347(05)64548-X. [DOI] [PubMed] [Google Scholar]
- 17.Tewari A, Peabody J, Sarle R, Balakrishnan G, Hemal A, Shrivastava A, et al. Technique of da Vinci robot-assisted anatomic radical prostatectomy. Urology. 2002;60:569. doi: 10.1016/S0090-4295(02)01852-6. [DOI] [PubMed] [Google Scholar]
- 18.Abbou C-C, Hoznek A, Salomon L, Olsson LE, Lobontiu A, Saint F, et al. Laparoscopic radical prostatectomy with a remote controlled robot. J Urol. 2001;165:1964. doi: 10.1016/S0022-5347(05)66251-9. [DOI] [PubMed] [Google Scholar]
- 19.Binder J, Kramer W. Robotically assisted laparoscopic radical prostatectomy. BJU Int. 2001;87:408. doi: 10.1046/j.1464-410x.2001.00115.x. [DOI] [PubMed] [Google Scholar]
- 20.Rabbani F, Stapleton AMF, Kattan MW, Wheeler TM, Scardino PT. Factors predicting recovery of erections after radical prostatectomy. J Urol. 2000;164:1929. doi: 10.1016/S0022-5347(05)66921-2. [DOI] [PubMed] [Google Scholar]
- 21.Catalona WJ, Basler JW. Return of erections and urinary continence following nerve sparing radical retropubic prostatectomy. J Urol. 1993;150:905. doi: 10.1016/s0022-5347(17)35645-8. [DOI] [PubMed] [Google Scholar]
- 22.Smith JA., Jr Robotically assisted laparoscopic prostatectomy: an assessment of its contemporary role in the surgical management of localized prostate cancer. Am J Surg. 2004;188(Suppl 4A):63S–67S. doi: 10.1016/j.amjsurg.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Menon M. Vattikuti Institute prostatectomy, a technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: experience of over 1,100 cases. Urol Clin North Am. 2004;31(4):701–717. doi: 10.1016/j.ucl.2004.06.011. [DOI] [PubMed] [Google Scholar]


