Abstract
Objective:
The increasing prevalence of oral diseases in children in developing countries is a major public health concern and creates the need to review various preventive strategies put in place on oral health promotion. In the absence of formal national programs, tertiary health institutions have adopted low-budget school oral education programs targeted at improving oral health awareness and behavioral changes in school children. The aim of this study was to review the school oral health education programs conducted by the Community Dentistry Unit of a tertiary hospital in a major city in Nigeria.
Materials and Methods:
An evaluation of the school oral health education programs conducted in the city over a 5-year period was done. Data collected included: venue of the program, the number of students and teachers educated in each school, screening and referrals, adequacy of teaching aids, desire for revisit, and barriers noted in its conduct.
Results:
A total of 104 oral health education programs were conducted during this period involving 16,248 participants. The majority (80%) of the schools visited were primary schools and 54% were privately owned. Over half of the programs was conducted on assembly grounds, 21% in classrooms, and 13% in school halls. Challenges encountered included: lack of audiovisual aids, transportation problems, inadequacy of screening tools, and insufficient promotional materials. All the schools visited requested for (subsequent) regular visitation.
Conclusion:
The study showed the feasibility of low-budget oral health education and willingness of schools to benefit from such programs. There are barriers to effective communication, which can be mitigated in order to achieve an optimal school oral health education program in a low resource setting.
Keywords: Barriers, education, health promotion, oral health, school
INTRODUCTION
The high level of unmet oral health needs of children in Nigeria is a source of concern and a public health problem.[1,2,3,4] The institution of school-based oral health programs and other promotional activities is, therefore, of public health significance in Nigeria and other developing countries. The school-based oral health programs aim to establish a foundation of good oral health early in life because the lifestyle adopted in childhood and adolescence may have a huge and lasting impact into adulthood. If positive, this may result in adopting preventive oral health behavior throughout adult life.[5,6] Furthermore, the school constitutes a means of networking for parents and guardians through local events and meetings during which messages can be passed to parents, other members of the family, and the community at large.
In many developing countries, notably in Africa, school-based and prevention-oriented oral health programs are nonexistent and poor oral health knowledge exists among the teachers who are supposed to motivate the pupils.[7] One of the many suggested solutions to this problem is regular and frequent organization of training programs for teachers, since one-time training program of school teachers does not result in long-term improvement of oral health of the pupils.[8] However, the limited resources in developing nations like Nigeria coupled with poor allocation to preventive oral health care have hampered effective organization of such programs at a central level. Thus, it is imperative for members of the dental team to regularly play their part in oral health promotion in schools, especially by conducting regular oral health education programs for the pupils and their teachers. Furthermore, studies in other countries have shown that school oral health education can improve the oral cleanliness and gingival health of pupils.[9,10,11,12,13]
Many tertiary oral health institutions in Nigeria have, as part of their curricula, school oral health education programs to salvage the poor state of oral health in the country. They encourage undergraduate dental students to participate in these programs to enrich themselves with the skills needed in passing across the required and appropriate message to the public.[14] In achieving the set target of improving oral health awareness and a positive behavior change in the target population, delivery of quality message in all respects is mandatory. The different challenges and barriers that may be encountered in the process of educating the school pupils and their teachers must be identified and appropriately addressed. If not done, this may ultimately affect the quality of message delivered to them and make it difficult to achieve the right behavioral change.[15,16] The aim of this study, therefore, was to review the oral health education programs conducted in schools by the Community Dentistry Unit of a tertiary health institution in Nigeria and identify the barriers met in conducting the programs.
MATERIALS AND METHODS
Background
The study is descriptive in nature; the data were gathered over a period of 5 years from 2009 to 2013 from the oral health education programs conducted by the Community Dentistry Unit, University College Hospital, Ibadan, Nigeria. Community Dentistry as a unit of the Department of Periodontology and Community Dentistry in the hospital aims at preventing oral diseases, promoting oral health and improving the quality of life of people through the organized efforts of the society. As part of its program to achieve the set aim, the unit conducts low-budget oral health education activities in different subpopulations and areas, including schools, in Ibadan, the capital city of Oyo State.
School oral health education forms one of the major outreach programs conducted by the unit. The oral health education team consists of dentists, public health nurses, and community oral health assistants.
Planning and delivery
The process of conducting oral health education begins with securing an appointment with the proposed school authority prior to the conduct of any oral health program by a member of the team. This starts with the fixing of appointment with the school authorities; this process usually involves gathering information from the school authorities about the audience to whom oral health education will be given, the time for the program, as well as how much time is allotted for it. Furthermore, the venue of the program is arranged by the school authorities. The choice of message will be done accordingly, all based on prior information gathered from the school. This will determine and tailor the oral health education message to the audience according to age and class as well as socioeconomic background. The time allotted will be known to plan effectively how long the message delivery will take and if or when the tooth brushing exercise will be performed, as well as if screening will be possible. The aim and objectives of the visit will be outlined ensuring that they conform to the theme of the message to be delivered. Assessment of available resources will also be done in terms of personnel, logistics as well as teaching aids, and availability of reinforcements usually in the form of toothbrushes and tooth pastes. The strategy to be used will also be discussed among the members of the team. Assigning of roles and rehearsal if necessary will be done prior to the visit. The message is delivered as planned by the team and adequately monitored to ensure the process is according to the plan. The key oral health education messages are based on oral hygiene, fluoride use, diet, and dental attendance. In some cases, specific diseases of interest to the school pupils and their teachers are discussed.
The school education is done in stages; the first stage entails introduction of the team, followed by delivery of the message with demonstration of tooth brushing using the Nasher mouth model and toothbrush, and finally asking questions by the teachers and the students. It is made as interactive as possible to engage the audience and generate greater interest. In circumstances where the time allotted permits, the pupils and teachers are screened for common oral diseases.
The evaluation of the program is usually done by asking the pupils and teachers, as the case may be, questions related to the delivered message. Correct answers are reinforced by giving incentives such as toothbrushes and tooth pastes.
Data collection
The data for this study were collected prospectively over a period of 5 years – between January 2009 and December 2013. School oral health education programs conducted for purposes other than educating the teachers and their pupils were excluded from this audit. Data collection was based on modification of Donabedian model of quality evaluation, which assessed the structure, process, and outcome.[17,18]
For this study, structure was evaluated based on the venue of the program; this took into consideration the availability of chairs for the audience, electric power supply to the projector, availability of trained personnel to conduct oral health education programs, and the availability of education aids such as audiovisuals used in conducting the programs. The process component was evaluated by the number of students and teachers screened and referred for further dental management, adequacy of teaching aids such as handbills and leaflets, pictures projected for the audience, method of imparting skills on self-oral hygiene, and methods of conducting the oral health education. The outcome component was assessed by the willingness of the schools to welcome a revisit. Other information obtained included: Name of the school, type of school (whether privately owned or government operated), whether the team was invited or not, and the number of students and teachers educated in each school. The data collected were entered into SPSS version 21 software and analyzed.
RESULTS
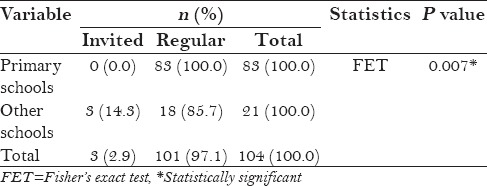
A total of 104 school oral health education programs were conducted during the study period. The schools that participated in the programs were either privately owned schools (56) or government operated (48). The majority (83, 79.8%) of the schools visited were primary schools; 19 (18.3%) were secondary schools and 2 (1.9%) were tertiary institutions. A total of 16,248 pupils/students and teachers were educated (mean of 113 participants in each primary school and 325 in each secondary/tertiary school; P < 0.001) [Table 1]. Only three of the schools invited the team for the oral health program, of which two were public schools and one was privately owned. Two out of the three schools were tertiary institutions and the third one a secondary school [Table 2]. Invitation by these schools was for the team to attend a health week in the private school and post graduate week celebration in the public school. The other oral health education programs were initiated by the dental team.
Table 1.
Characteristics of the schools and the study participants
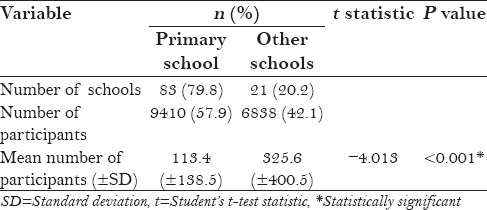
Table 2.
Mode of fixing appointments in the different schools
Structure
The venues for the oral health education included school halls, assembly grounds, classrooms, school clinics, and libraries, with assembly grounds being the most often used location [Figure 1]. The audience for the oral health education stood up when the program was conducted on the assembly ground, while chairs were provided for the audience to sit on at sessions conducted in the halls, classrooms, and libraries.
Figure 1.
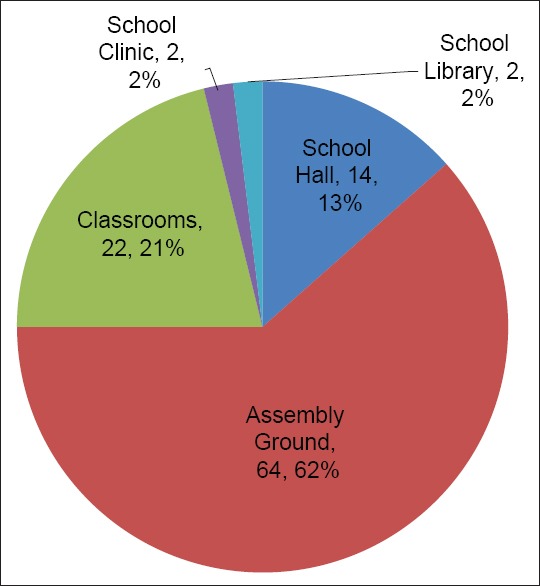
Venue for the oral health education programs
Qualified and trained dentists led the team in all the oral health education programs and educated the pupils as well as conducted the screening exercises. The trained public health nurse assisted in disseminating the information to the audience. Only two of the schools had audiovisual aids that the team could use, and these were tertiary institutions [Table 3]. The team, therefore, took along hired audiovisual aids, but erratic power supply often made it impossible to use them. Three of the schools visited, all being primary schools, were located in areas with no access roads.
Table 3.
Assessment criteria
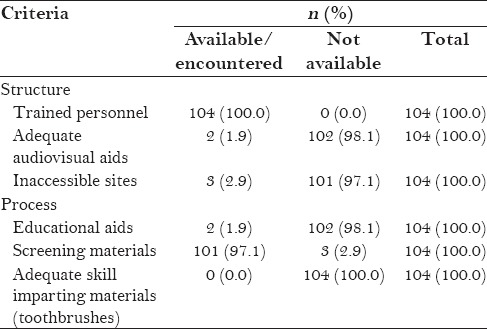
Process
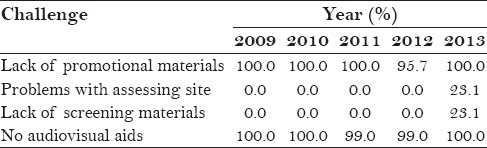
Oral examination materials to screen the pupils and their teachers were not available in 3 (2.9%) schools. Another challenge noted was non-availability of oral health education aids, with the most reported problem being inadequate oral health promotional materials such as posters, handbills, and leaflets to assist in information dissemination to the pupils and their teachers. The process of imparting skills was inadequate as the only available aid was the Nasher mouth model that was used to demonstrate tooth cleaning procedure by the team. It was also used by the pupils and their teachers to demonstrate the cleaning procedure that was taught. Toothbrushes were not available at any of the programs conducted for the pupils to demonstrate the taught tooth cleaning by the dentists on themselves [Table 3]. The challenges encountered in terms of promotional materials, access, screening materials, and audiovisual aids persisted over the 5 years of the study, and appeared to be worsening as regards access and lack of screening materials [Table 4].
Table 4.
Challenges and year of conduct of program
Outcome
All the schools were enthusiastic about the visit. According to the audit, none of the schools turned down the request by the dental team to conduct oral health education in their school. In fact, 28 (26.9%) schools made specific request at the time of the exploratory visit to include dental caries – causes, treatment, and prevention – in the health talk. The number of participants referred for further dental consultation after each session ranged from 0 to 15 (median of 5). They were referred to the Primary Oral Health Care Center established in the inner, low-income, area of the city and their subsequent attendance was confirmed. All the schools received the team well and were willing to entertain a revisit. They requested for regular visitation to form part of their curriculum and had since received the team once or twice.
DISCUSSION
Oral health education is an essential aspect of oral health promotion that equips individuals with the required knowledge needed to improve their oral health and be able to recognize healthy choices for a healthier lifestyle. Although a weak link exists between knowledge and behavior, nonetheless, ignorance will not likely translate into the desired behavior change. It is, therefore, apparent that the template on which any behavior change is based is knowledge. This study described an audit of the school oral health education programs conducted by a tertiary oral health institution in a developing country. Developing countries present with peculiarities such as low income, inadequate health facilities, and inequality in oral and general health among others. School oral health education program is one of the cost-effective oral health programs aimed at prevention of oral diseases and promotion of good oral health. These programs are usually conducted by oral health personnel aiming, as much as possible, to reach the different strata of the society.
In this audit, both the government-sponsored and privately owned schools were covered by the dental team. Although a higher proportion of the schools visited belonged to the former, efforts were made to cover the two types of schools in order to reduce health inequalities as much as possible as had been noted to exist.[7] A higher proportion of pupils attending public schools in the country belong to the lower socioeconomic classes as the schools are almost free for the pupils. Conversely, pupils attending privately operated schools pay tuition fees that could be exorbitant; thus, only pupils whose parents could afford the tuition fees attend such schools and are more likely to be from higher socioeconomic classes. Furthermore, pupils attending public schools have been reported to engage in less frequent tooth brushing and are noted to visit the dentists less frequently compared to those attending private schools.[1] On the other hand, private school pupils are more likely to have higher dental caries experience because of their dietary habits including snacking and in-between meals.[1,19] Thus, inclusion of the different school types in the oral health education program is necessary and pupils in both schools may benefit from the program.
The majority of the schools visited by the dental team, as revealed by this audit, were primary schools; this was to initiate young minds early in life and impart as much as possible oral health knowledge at an early stage. It could, however, also be attributable to the more flexible time table of the primary schools in this part of the world. Some tertiary educational institutions were also visited, but it is worthy of note that the two tertiary institutions were universities in the town and both institutions invited the team for oral health education programs as part of their annual school activities and health week. This was encouraging to the team as students of those institutions appeared to have placed oral health on a favorable priority scale, which is not usual in developing countries.[20] That some students of tertiary educational institutions engage in this positive oral health behavior gives us hope that there could be gross improvement in oral health awareness in developing countries, if it continues.
Over one-half of the oral health education programs were conducted on the assembly grounds, which may be due to the absence of an appropriate school hall that could conveniently take all the school pupils. It may equally be because the school in question wanted the program to take place in the morning during their usual assemblage in order to not leave out any pupil. Having a supportive environment is one of the elements of oral health promotion, which also becomes important for the receivers of the message (audience) during oral health education program. In the conduct of oral health education of which the final aim is good behavior change, a supportive and conducive environment is important to make the audience attentive as well as to be interested in the message to be passed across to them.[5] To circumvent the uncomfortable environment in some schools visited, the pupils and teachers chose alternatives such as the assembly ground where ventilation is good for the oral health education. But when this is done at mid-day, the weather condition may be hot and finally uncomfortable for the audience. Moreover, in such instances, the use of the projector or blackboards for illustration may be impossible.
Generally, there were inadequate oral health promotional materials, as only a model to demonstrate the brushing technique was available for use. Oral health education materials are essential aids to oral health education which may be in the form of information sheets, posters, leaflets, handbills, flip charts, or display boards among others. They help the audience to understand the topic being discussed better and are more encouraging to the younger age group when pictures are shown giving a better representation of the message.[5,9,10,12,13] Inadequacy of these materials, however, is worrisome, as it may affect the quality of the message being delivered. Use of any of the different methods of oral health education should, ideally, be adequately aided with different teaching materials based on the principle that there should be active involvement and reinforcement.[21,22] Furthermore, the process of delivering the oral health messages in schools should be made interactive, age specific, child centered, and skill based.[5,21]
Oral health education conducted in schools in developing countries use the lecture methods assisted by teaching aids such as models, chalk, blackboards, posters, and charts, with tooth brushing demonstration exercise serving as the skill imparting section.[9] On the other hand, in developed countries such as Denmark, different oral health education methods and aids are utilized.[23] Some of the methods used include lecture methods, role play, and experimental methods. These techniques are also adequately aided with materials like picture books, models, puppets, coloring books, leaflets, video, overhead projection, slides, worksheets, games, jigsaws, puzzles, and computer programs, depending on the age.[23] The use of different health education methods in addition to sufficient teaching aids has been found effective in improving the oral health knowledge, attitude, and practices, as well as the oral health status of children.[10,11,13,24,25]
The Community Dentistry Unit's conduct of oral health education comprised mainly the lecture method, which is child centered and interactive in order to actively engage the children in the process of message delivery. Furthermore, the program is age matched with the lectures complemented with songs in the younger age groups for easy comprehension as well as to draw the attention of these age groups. The lecture method used by the team is similar to the way teaching is conducted in primary and secondary schools in the environment. However, complementing the process adequately with pictures, leaflets and posters, and other educational aids was grossly deficient in almost all the schools visited. Moreover, supervised tooth brushing method has been advocated for the correct behavior change.[26] This was not possible in our setting due to financial constraints to supply the pupils with toothbrushes.
Difficulty in accessing the school was documented in a few cases, which was probably due to the location of the schools. This made transportation to the site unpleasant and resulted in walking long distances in the hot and humid tropical weather. This is one of the peculiarities of developing countries, as some areas lack good roads for vehicular transportation of the team to their destination. Inadequacy of oral examination materials for screening of the participants was another reported challenge. This particular problem is resource related and shows the poor fiscal allocation to preventive oral health activities. There is a need to address these challenges if more favorable outcomes are to be obtained from oral health education in similar settings.
A major limitation of this study is that the behavior change, which is the ultimate outcome, could not be assessed in this study as it is only possible to evaluate over a long term and, therefore, was not an objective of the study. Also, the outcome could not be objectively assessed. This could have been done using tools such as questionnaires to assess the knowledge, attitude, and practices of the school pupils pre- and post-oral health education and by oral examination to assess if there are changes in their oral health status. However, the present audit did not have baseline data with which to compare, and hence, another prospective audit has been commenced to achieve this additional objective.
CONCLUSION
In conclusion, the present study showed that low-budget oral health education programs are feasible in developing countries and the schools visited demonstrated willingness to benefit from such initiatives. There are barriers to effective communication noted in the process and structure components of the quality evaluation model, which can be mitigated in order to achieve an optimal school oral health education program that will meet the set targets.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Adekoya-Sofowora CA, Nasir WO, Oginni AO, Taiwo M. Dental caries in 12-year-old suburban Nigerian school children. Afr Health Sci. 2006;6:145–50. doi: 10.5555/afhs.2006.6.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Denloye OO, Bankole OO, Onyeaso CO. Dental health service utilization by children seen at the University College Hospital-an update. Odontostomatol Trop. 2004;27:29–32. [PubMed] [Google Scholar]
- 3.Folayan MO, Khami MR, Folaranmi N, Orenuga O, Popoola BO, O Olatosi O, et al. Determinants of preventive dental practice for children among final-year dental students in Nigeria. Int J Paediatr Dent. 2014;24:43–50. doi: 10.1111/ipd.12024. [DOI] [PubMed] [Google Scholar]
- 4.Sofola OO, Folayan MO, Oginni AB. Changes in the prevalence of dental caries in primary school children in Lagos State, Nigeria. Niger J Clin Pract. 2014;17:127–33. doi: 10.4103/1119-3077.127419. [DOI] [PubMed] [Google Scholar]
- 5.Oral Health Promotion; An Essential Element of Health Promoting School. Geneva: World Health Organization (WHO); 2003. WHO Information Series on School Health: Document Eleven; pp. 1–69. [Google Scholar]
- 6.Pomarico L, de Souza IP, Tura LF. Oral health profile of education and health professionals attending handicapped children. Pesqui Odontol Bras. 2003;17:11–6. doi: 10.1590/s1517-74912003000100003. [DOI] [PubMed] [Google Scholar]
- 7.Sofola OO, Agbelusi GA, Jeboda SO. Oral health knowledge, attitude and practices of primary school teachers in Lagos State. Niger J Med. 2002;11:73–6. [PubMed] [Google Scholar]
- 8.Frencken JE, Borsum-Andersson K, Makoni F, Moyana F, Mwashaenyi S, Mulder J. Effectiveness of an oral health education programme in primary schools in Zimbabwe after 3.5 years. Community Dent Oral Epidemiol. 2001;29:253–9. doi: 10.1034/j.1600-0528.2001.290403.x. [DOI] [PubMed] [Google Scholar]
- 9.Bhardwaj VK, Sharma KR, Luthra RP, Jhingta P, Sharma D, Justa A. Impact of school-based oral health education program on oral health of 12 and 15 years old school children. J Educ Health Promot. 2013;2:33. doi: 10.4103/2277-9531.115820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saied-Moallemi Z, Virtanen JI, Vehkalahti MM, Tehranchi A, Murtomaa H. School-based intervention to promote preadolescents’ gingival health: A community trial. Community Dent Oral Epidemiol. 2009;37:518–26. doi: 10.1111/j.1600-0528.2009.00491.x. [DOI] [PubMed] [Google Scholar]
- 11.Shenoy RP, Sequeira PS. Effectiveness of a school dental education program in improving oral health knowledge and oral hygiene practices and status of 12- to 13-year-old school children. Indian J Dent Res. 2010;21:253–9. doi: 10.4103/0970-9290.66652. [DOI] [PubMed] [Google Scholar]
- 12.Tai B, Du M, Peng B, Fan M, Bian Z. Experiences from a school-based oral health promotion programme in Wuhan City, PR China. Int J Paediatr Dent. 2001;11:286–91. doi: 10.1046/j.1365-263x.2001.00281.x. [DOI] [PubMed] [Google Scholar]
- 13.Yazdani R, Vehkalahti MM, Nouri M, Murtomaa H. School-based education to improve oral cleanliness and gingival health in adolescents in Tehran, Iran. Int J Paediatr Dent. 2009;19:274–81. doi: 10.1111/j.1365-263X.2009.00972.x. [DOI] [PubMed] [Google Scholar]
- 14.Ibiyemi O, Taiwo JO, Oke GA. Dental education in the rural community: A Nigerian experience. Rural Remote Health. 2013;13:2241. [PubMed] [Google Scholar]
- 15.Kay EJ, Locker D. Is dental health education effective? A systematic review of current evidence. Community Dent Oral Epidemiol. 1996;24:231–5. doi: 10.1111/j.1600-0528.1996.tb00850.x. [DOI] [PubMed] [Google Scholar]
- 16.van Palenstein Helderman WH, Munck L, Mushendwa S, van’t Hof MA, Mrema FG. Effect evaluation of an oral health education programme in primary schools in Tanzania. Community Dent Oral Epidemiol. 1997;25:296–300. doi: 10.1111/j.1600-0528.1997.tb00943.x. [DOI] [PubMed] [Google Scholar]
- 17.Donabedian A. Quality assurance. Structure, process and outcome. Nurs Stand. 1992;7(Suppl QA):4–5. [PubMed] [Google Scholar]
- 18.Donabedian A. The role of outcomes in quality assessment and assurance. QRB Qual Rev Bull. 1992;18:356–60. doi: 10.1016/s0097-5990(16)30560-7. [DOI] [PubMed] [Google Scholar]
- 19.Jürgensen N, Petersen PE. Oral health and the impact of socio-behavioural factors in a cross sectional survey of 12-year old school children in Laos. BMC Oral Health. 2009;9:29. doi: 10.1186/1472-6831-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okunseri C, Chattopadhyay A, Lugo RI, McGrath C. Pilot survey of oral health-related quality of life: A cross-sectional study of adults in Benin City, Edo State, Nigeria. BMC Oral Health. 2005;5:7. doi: 10.1186/1472-6831-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jürgensen N, Petersen PE. Promoting oral health of children through schools--results from a WHO Global Survey 2012. Community Dent Health. 2013;30:204–18. [PubMed] [Google Scholar]
- 22.Haleem A, Siddiqui MI, Khan AA. School-based strategies for oral health education of adolescents-a cluster randomized controlled trial. BMC Oral Health. 2012;12:54. doi: 10.1186/1472-6831-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: An opportunity for oral health promotion. Bull World Health Organ. 2005;83:677–85. [PMC free article] [PubMed] [Google Scholar]
- 24.Chandrashekar BR, Suma S, Kiran K, Manjunath BC. The use of school teachers to promote oral hygiene in some secondary school students at Hyderabad, Andhra Pradesh, India: A short term prospective pilot study. J Family Community Med. 2012;19:184–9. doi: 10.4103/2230-8229.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gauba A, Bal IS, Jain A, Mittal HC. School based oral health promotional intervention: Effect on knowledge, practices and clinical oral health related parameters. Contemp Clin Dent. 2013;4:493–9. doi: 10.4103/0976-237X.123056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chapman A, Copestake SJ, Duncan K. An oral health education programme based on the National Curriculum. Int J Paediatr Dent. 2006;16:40–4. doi: 10.1111/j.1365-263X.2006.00677.x. [DOI] [PubMed] [Google Scholar]


