Abstract
Objectives
Patients with respiratory distress often seek emergency medical care, and are transported by emergency medical services (EMS). EMS encounters with patients in respiratory distress have not been well described. The study objective was to characterize the epidemiology of prehospital respiratory distress and subsequent patient outcomes.
Methods
This was a population-based cohort study of non-injured adults transported by EMS to any of 16 hospitals between 2002 and 2006. EMS records were linked to hospital administrative data for encounters categorized by EMS personnel as primarily “respiratory distress” in nature. The authors described prehospital patient and encounter characteristics, interventions, hospital discharge diagnoses (using ICD-9-CM codes), and patient outcomes. The association between prehospital variables, defined a priori, and hospital admission were described using multivariable logistic regression.
Results
There were 19,858 EMS encounters, of which 166,908 were for respiratory distress (11.9%, 95% confidence interval [CI] = 11.7% to 12.1%). Half of the patients were admitted to the hospital (n = 9,964), one-third of those required intensive care (n = 3,094), and 10% of hospitalized patients died prior to discharge (n = 948). Fifteen percent of hospitalized patients received invasive mechanical ventilation (n = 1,501), over half of whom were intubated during prehospital care (n = 896). The most common primary discharge diagnoses among prehospital respiratory distress patients admitted to the hospital were congestive heart failure (16%), pneumonia (15%), chronic obstructive pulmonary disease (13%), and acute respiratory failure (13%). Few EMS patients with respiratory distress were coded with a primary diagnosis of acute myocardial infarction (3.5%, n = 350), or underwent percutaneous coronary intervention (0.7%, n = 71). In a multivariable regression model, prehospital factors that were independently associated with hospital admission included initial respiratory rate (odds ratio [OR] 1.29 for an increase in respiratory rate of five breaths per minute, 95% CI = 1.24 to 1.35), and an encounter that originated at a nursing home (OR 2.80, 95% CI = 2.28 to 3.43).
Conclusions
In a ppulation-based cohort, EMS personnel commonly encounter prehospital respiratory distress among medical patients, many of whom require hospital admission to the intensive care unit. These data may help to inform targeted therapy or more efficient triage and transport decisions.
INTRODUCTION
Respiratory distress is a common reason to engage the emergency health care system in the United States, accounting for more than 3.7 million emergency department (ED) visits annually.1 Respiratory distress may result from a variety of problems including chronic obstructive pulmonary disease (COPD), asthma, pneumonia, or congestive heart failure (CHF), and can be generally defined as respiratory demand being greater than capacity.2 Among the elderly, respiratory distress is the second most common reason to visit an ED. When hospitalized, patients with respiratory distress severe enough to result in respiratory failure are almost four times less likely to survive to hospital discharge than patients with cancer or heart disease.3
Emergency medical services (EMS) personnel play a prominent role in triage, transport decisions, and initial management of patients with respiratory distress. Evidence suggests that interventions in the prehospital setting reduce mortality among patients with respiratory distress, particularly when care is provided by advanced rather than basic life support (ALS vs. BLS).4 Yet, paramedics are hampered in their delivery of early, targeted therapy by the challenges in accurately differentiating between the various etiologies of respiratory distress.5,6 Certain therapies, if misapplied, may be harmful to patients with undifferentiated respiratory distress.7–9 A notable example is prehospital unopposed oxygen compared to titrated oxygen in patients with presumed COPD exacerbation.10
Little is known about the frequency with which EMS personnel encounter prehospital respiratory distress, its etiologies, or outcomes. We sought to characterize the epidemiology and outcomes of prehospital respiratory distress, to explore the associations between patient and incident characteristics and hospital admission, and to describe the concordance of EMS clinical impressions with hospital diagnoses. These data provide a framework on which to consider how early diagnosis and therapy may be offered to high-risk patients with prehospital respiratory distress.
METHODS
Study Design
This was a community-based, retrospective cohort study that included all EMS patient encounters between 2002 and 2006 in greater King County, Washington (excluding the city of Seattle). This dataset is part of a larger cohort of King County EMS records used for previous prehospital studies.11–13 The institutional review boards of the Washington State Department of Health and the University of Washington approved the study with waiver of informed consent.
Study Setting and Population
We analyzed patients transported by a countywide EMS system between January 2002 and December 2006. The EMS catchment area includes urban, suburban, and rural areas over approximately 2,000 square miles containing a population of 1.2 million people. This EMS system is structured to respond in a tiered fashion to medical emergencies. The first-tier response is emergency medical technician (EMT)-firefighters who evaluate all patients and provide BLS. BLS providers operate 29 fire departments in the county, receive common initial and ongoing training, and follow standardized patient care protocols. The second tier of the EMS system includes paramedics trained in ALS who work in pairs to evaluate and manage higher-acuity patients. ALS providers are trained in interventions such as intravenous (IV) access, medication administration, and advanced airway management. King County has 25 ALS ambulances on duty at any one time. All paramedics receive common training and provide care under a common set of care guidelines.
Dispatchers for EMS activate the ALS and BLS response concurrently if standardized criteria are fulfilled, based on the patient’s presenting complaint.14 For patients with breathing difficulty, dispatch criteria for an ALS response include at least one of the following: 1) unconscious and unresponsive; 2) is in respiratory distress, defined as either the inability to speak normally (increased work of breathing), or sitting, standing, or leaning forward to breathe (tripod position); 3) breathing difficulty accompanied by chest discomfort if the patient is older than 25 years old; or 4) has audible wheezing or stridor.
Patients are transported to 16 acute care hospitals within the county. BLS transport is the default; ALS providers will transport a patient with isolated breathing difficulty if any of the following criteria are met, or if in their judgment the patient may imminently require ALS (in consultation with direct medical oversight): 1) respiratory rate > 30 breaths per minute, 2) abnormal respiratory pattern, 3) patient in tripod position, 4) failure to respond to inhaled bronchodilators, or 5) acute asthma with history of previous intubation.
Study Protocol
We used probabilistic matching to remove duplicates among EMS records and used hierarchical deterministic matching to link EMS records to 1) the Comprehensive Hospital Abstract Reporting System (CHARS), a statewide database of detailed diagnostic, procedural, and discharge data on all hospitalizations; and 2) the Washington State death record. Additional details on cohort development and the success of data linkage were reported previously.11 We excluded patients with traumatic injury or cardiac arrest, and those younger than 18 years of age. Among the remaining EMS encounters, we included all patients transported to a hospital who had physical exams, including vital signs, documented by EMS personnel.
We defined patients as having respiratory distress based on the initial prehospital provider documenting “respiratory” as the primary reason for prehospital care. EMS personnel also documented a diagnostic impression for each patient with respiratory distress: “shortness of breath/hyperventilation,” “asthma,” “chronic obstructive pulmonary disease (COPD)/emphysema,” “respiratory depression/respiratory arrest,” or “other respiratory.” BLS and ALS providers may separately document diagnostic impressions on the same patient if they are both dispatched (i.e. a two-tier EMS response). We linked these data and used the BLS diagnostic impression as the default, except as noted below.
For EMS patients admitted to hospital, we describe inpatient diagnoses and procedures using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. We defined patient outcomes as intensive care unit admission (identified using critical care revenue codes15), length of stay, hospital mortality, and discharge destination (e.g. new nursing home placement).
We abstracted prehospital clinical data from EMS records, including triage, demographic, procedural, and transport data. Prehospital vital signs were captured from the first provider on scene and included respiratory rate, pulse rate, blood pressure, oxygen saturation, and Glasgow Coma Scale (GCS) score. EMS personnel on scene provided a severity of illness assessment by classifying each encounter as “non-urgent,” “urgent,” or “life-threatening.” We abstracted prehospital interventions including supplemental oxygen, electrocardiographic monitoring, IV access, bag-valve-mask ventilation, and endotracheal intubation. Mechanical, noninvasive positive pressure ventilation was not used prior to hospital arrival.
Data Analysis
We calculated the overall proportion of non-trauma, non-cardiac arrest EMS activations due to respiratory distress with 95% confidence intervals (CI), and the proportion with respiratory distress by age groups. We summarized EMS encounter characteristics for those with respiratory distress, and for the subset of patients admitted to a hospital, we identified inpatient procedures and patient outcomes.
To explore associations between prehospital characteristics and hospital admission, we constructed a multivariable logistic regression model using robust variance estimation. In the model, we included a priori patient variables (e.g. age, sex, systolic blood pressure [sBP], pulse rate, respiratory rate, and pulse oximetry), incident data (e.g. home, public building, street/highway, adult family home, nursing home, or medical facility), and overall assessment by EMS personnel (severity index and diagnostic impression). We used single imputation with normal values substitution for the GCS score and pulse oximetry because multiple imputation in prior analyses of this dataset did not substantially change results.11,13 We included three additional variables as fixed effects in the final logistic model: year in the cohort, the responding EMS agency, and the receiving hospital. We included the latter two variables in order to mitigate the non-independence of observations in these clusters. We decided a priori that provider level of training (i.e. ALS vs. BLS) may be a clinically relevant effect modifier of the association between severity of illness and hospital admission; we included this interaction term in the model and evaluated its significance using a likelihood ratio test. We used STATA 12.0 (StataCorp, College Station, TX) for data analysis, and two-sided p values < 0.05 were considered significant.
To investigate the accuracy with which prehospital personnel are able to identify “phenotypes” of respiratory distress, we compared primary hospital diagnoses at the time of discharge (using ICD-9-CM codes) to the EMS diagnostic impression. We further classified EMS diagnostic impression into symptom-based (e.g. “shortness of breath”) or disease-based (e.g. asthma, COPD, respiratory depression). Diagnostic concordance was analyzed separately for patients transported by ALS and BLS. In cases where both ALS and BLS evaluated the patient and documented diagnostic impressions, we used the diagnostic impression of the transporting provider.
RESULTS
The Epidemiology of Prehospital Respiratory Distress
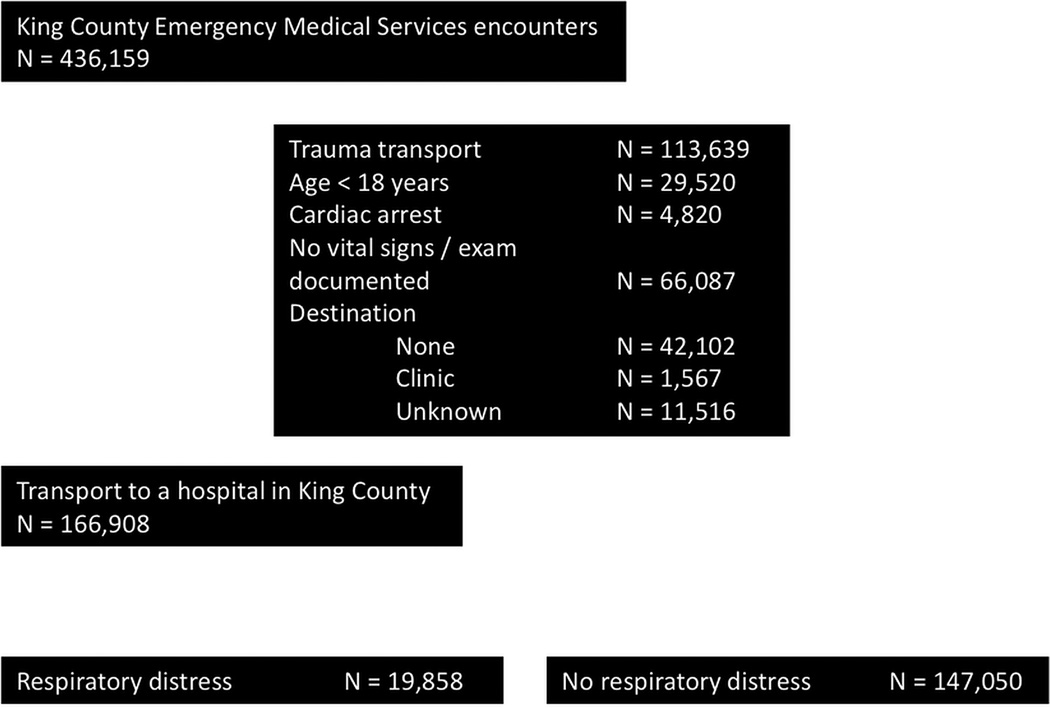
Approximately one in eight EMS non-traumatic, non-arrest encounters was for a patient classified by EMS as respiratory distress (19,858 of 166,908, 11.9%; 95% CI = 11.7% to 12.1%, Figure 1). This estimate ranged between 10.9% and 12.4% annually over the five-year study. Approximately one in six patients evaluated by ALS providers had respiratory distress (17.9%, 95% CI = 17.6% to 18.3%), compared to 1 in 12 for those evaluated by BLS providers only (8.6%, 95% CI = 8.4% to 8.7%). The proportion of EMS encounters for respiratory distress increased across patient age groups (Figure 2).
Figure 1.
Patient accrual.
Figure 2.
The proportion of EMS patients with respiratory distress across age groups among all encounters (black line), ALS encounters (solid grey line), and BLS encounters (dashed grey line).
The Course of Patients with Prehospital Respiratory Distress
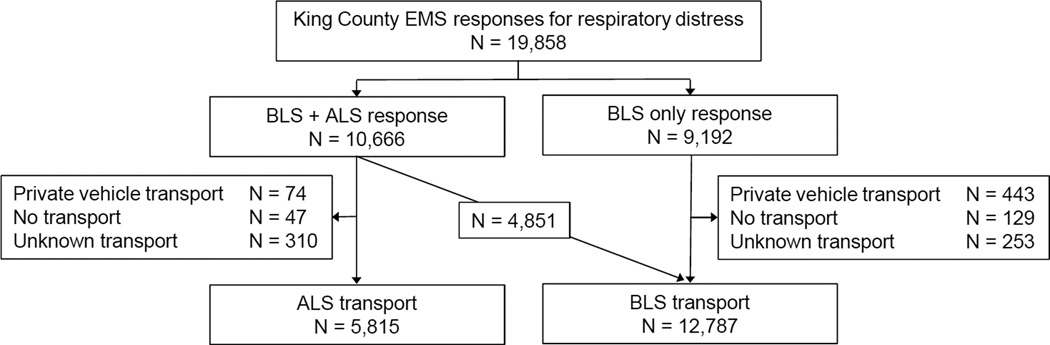
BLS providers responded to all patients with respiratory distress (Figure 3). ALS providers were dispatched to approximately one-half of the patients with respiratory distress (54%, n = 10,666). ALS providers transported more than one-half of these patients (55%, n = 5,815). We observed that most EMS responses for respiratory distress were to the patient’s home (n = 13,807, 70%) (Table 1). A higher proportion of patients seen jointly by ALS and BLS received supplemental oxygen as compared to BLS-only encounters (95% vs. 56%, respectively). ALS providers determined illness severity as “life-threatening” in 13% of the patients they evaluated (n = 1,353) and intubated two-thirds prior to hospital arrival (n = 896).
Figure 3.
The course of patients with prehospital respiratory distress.
Table 1.
Patient and response characteristics of EMS encounters with respiratory distress
| Dispatched Level of Service |
|||
|---|---|---|---|
| Variable | All patients | BLS | ALS |
| Complete encounters | 19,858 | 9,192 (46) | 10,666 (54) |
| Mean age, yrs (±SD) | 66 (±19) | 64 (±20) | 68 (±18) |
| Male sex | 7,892 (41) | 3,531 (39) | 4,361 (42) |
| Initial prehospital vital signs | |||
| Respiratory rate, breaths/min, mean (±SD) | 26 (±9) | 23 (±7) | 29 (±9) |
| Oxygen saturation* %, mean (±SD) | 91 (±10) | 94 (±6) | 90 (±11) |
| Systolic blood pressure <100 mm Hg | 1,380 (7) | 509 (6) | 871 (8) |
| Systolic blood pressure >180 mm Hg | 2,218 (11) | 721 (8) | 1,497 (14) |
| Heart rate >100 beats/min | 99 (23) | 94 (20) | 102 (24) |
| Median Glasgow Coma Scale* score (IQR) | 15 (15–15) | 15 (15–15) | 15 (15–15) |
| EMS severity code | |||
| Life-threatening | 1,492 (8) | 139 (2) | 1,353 (13) |
| Urgent | 10,359 (53) | 4,548 (50) | 5,811 (55) |
| Non-urgent | 7,794 (40) | 4,345 (48) | 3,449 (32) |
| EMS provider impression | |||
| Shortness of breath | 12,847 (65) | 6,277 (68) | 6,570 (62) |
| Asthma | 1,517 (8) | 498 (5) | 1,019 (9) |
| COPD / emphysema | 1,393 (7) | 414 (5) | 979 (9) |
| Respiratory depression | 1,055 (5) | 213 (2) | 842 (8) |
| Other | 3,046 (15) | 1,790 (20) | 1,256 (12) |
| Pre-hospital interventions | |||
| Supplemental oxygen | 15,297 (77) | 5,153 (56) | 10,144 (95) |
| Bag valve mask ventilation | 931 (5) | 20 (<1) | 911 (9) |
| Endotracheal intubation | 896 (5) | 0 | 896 (8) |
| ECG monitoring | 8,911 (45) | 650 (7) | 8,261 (77) |
| Intravenous access | 4,737 (24) | 6 (<1) | 4,731 (44) |
| Incident location | |||
| Home | 13,807 (70) | 6,462 (71) | 7,345 (69) |
| Nursing home | 2,666 (13) | 978 (11) | 1,688 (16) |
| Adult family home | 765 (4) | 317 (4) | 448 (4) |
| Medical facility | 711 (4) | 300 (3) | 411 (4) |
| Public building | 595 (3) | 349 (4) | 246 (2) |
| Street / highway | 357 (2) | 212 (2) | 145 (1) |
| Other | 834 (4) | 465 (5) | 369 (4) |
| Mean transport interval* (scene to hospital), min (±SD) | 12.5 (±10) | 13 (±11) | 12 (±9) |
| Admitted to hospital | 9,964 (50) | 3,590 (39) | 6,374 (60) |
Missing data were minimal (<5%) for all variables except the following (with n equal to the number of patients with data): Glasgow Coma Scale score (n=10,574); oxygen saturation (n=4,451); transport interval (n=5,804).
Data are reported as n (%) unless otherwise noted
COPD = chronic obstructive pulmonary disease; ECG = electrocardiogram
Patient Outcomes Following Prehospital Respiratory Distress
One-half of EMS patients with respiratory distress were admitted to the hospital (n = 9,964), and one-third of those received intensive care (n = 3,094) for a median of two days (IQR 1 to 4 days) (Table 2). Mechanical ventilation was delivered in one-half of ICU patients (48%; n = 1,486), more than half of whom were intubated in the prehospital setting. Hospital mortality was 10% for those who were admitted, 13% for those requiring intensive care, and 23% for those requiring mechanical ventilation. Among patients who survived hospitalization, one in eight required new placement in a skilled nursing facility (13%; n = 1,163).
Table 2.
Hospital outcomes and procedures among emergency medical services patients with respiratory distress
| Variable | All Hospitalized Patients (N=9,964) |
|---|---|
| Outcomes | |
| Hospital mortality | 948 (10) |
| Received intensive care | 3,094 (31) |
| Duration of intensive care, days, median (IQR) |
2 (1–4) |
| Length of hospital stay, days, median (IQR) | 4 (2–6) |
| New discharge to skilled nursing facility* | 1,163 (13) |
| Procedures | |
| Invasive mechanical ventilation | 1,486 (15) |
| Tracheostomy | 22 (<1) |
| Bronchoscopy | 145 (1) |
| Percutaneous coronary intervention | 71 (<1) |
New placement in a skilled nursing facility was defined as discharge to a skilled nursing facility for patients’ whose EMS encounter for respiratory distress did not originate at a skilled nursing facility. Denominator for this outcome is patients surviving hospitalization, n=9,016.
Data reported as n (%) unless otherwise noted.
Prehospital characteristics associated with hospital admission
We observed many characteristics independently associated with hospital admission, including increasing age, male sex, and abnormal prehospital physiology (e.g. greater respiratory and heart rates, lower sBP and oxygen saturation) (Table 3). EMS encounters that originated at the patient’s home or a nursing home were associated with more than two-fold higher odds of hospital admission than encounters elsewhere. We observed an interaction between prehospital severity of illness and the level of prehospital care (BLS only vs. ALS; p < 0.01), whereby a “life-threatening” severity of illness assigned by ALS was associated with the greatest adjusted odds of hospital admission as compared to a “non-urgent” patient cared for by BLS only (Table 3).
Table 3.
Multivariable logistic regression model of prehospital characteristics associated with hospital admission among all EMS encounters with respiratory distress*
| Variable | Adjusted Odds Ratio |
95% CI | P value |
|---|---|---|---|
| Age, by 5 years | 1.14 | 1.13–1.15 | <0.0001 |
| Male sex | 1.17 | 1.09–1.25 | <0.0001 |
| Vital signs | |||
| Respiratory rate, by 5 breaths per min | 1.29 | 1.24–1.35 | <0.0001 |
| Pulse oximetry, by 10% | 0.81 | 0.75–0.88 | <0.0001 |
| Systolic blood pressure, by 10 mmHg | 0.98 | 0.97–0.99 | <0.0001 |
| Heart rate, by 10 beats per min | 1.09 | 1.07–1.11 | <0.0001 |
| Glasgow Coma Scale score | 0.97 | 0.94–0.99 | 0.02 |
| EMS provider impression | |||
| Shortness of breath | 1.21 | 1.10–1.33 | <0.0001 |
| Asthma | 0.75 | 0.64–0.88 | <0.0001 |
| COPD / emphysema | 1.26 | 1.08–1.47 | 0.003 |
| Respiratory depression | 1.50 | 1.24–1.82 | <0.0001 |
| Other | Ref | . | . |
| EMS severity code^ | |||
| ALS patients | |||
| Life-threatening | 3.24 | 2.71–3.86 | <0.0001 |
| Urgent | 2.13 | 1.92–2.36 | <0.0001 |
| Non-urgent | 1.29 | 1.16–1.43 | <0.0001 |
| BLS patients | |||
| Life-threatening | 1.54 | 0.998–2.38 | 0.05 |
| Urgent | 1.31 | 1.18–1.45 | <0.0001 |
| Non-urgent | Ref | . | . |
| Incident location | |||
| Routine / home | 2.19 | 1.83–2.61 | <0.0001 |
| Nursing home | 2.80 | 2.28–3.43 | <0.0001 |
| Public building | 1.04 | 0.79–1.37 | 0.76 |
| Street / highway | 0.74 | 0.52–1.04 | 0.09 |
| Adult family home | 2.12 | 1.65–2.73 | <0.0001 |
| Medical facility | 2.75 | 2.16–3.51 | <0.0001 |
Model uses robust variance estimates, and includes the year in cohort, the responding EMS agency, and receiving hospital as fixed effects (not shown). Total observations with complete data were 17,156.
Likelihood ratio test for multiplicative interaction term (ALS x EMS severity code) p<0.01. Referent category for all EMS severity code terms is BLS x non-urgent.
COPD = chronic obstructive pulmonary disease
Concordance of EMS impressions and hospital diagnoses
Of the 9,443 prehospital respiratory distress patients admitted after EMS transport, 6,564 (70%) received primary discharge diagnoses related to respiratory disease (i.e. pulmonary edema, COPD, asthma, pneumonia, pulmonary embolism, lung cancer, or acute respiratory failure). A higher proportion of respiratory distress identified during ALS transport (74%) as compared to BLS transport (66%) included primary diagnoses related to respiratory disease (Tables 4A and 4B).
Table 4.
| a. Concordance of ALS diagnostic impression with primary discharge diagnosis among patients hospitalized after ALS transport for respiratory distress | ||||||
|---|---|---|---|---|---|---|
| ALS diagnostic impression |
||||||
| Primary Discharge Diagnosis* |
All Hospitalized Patients† (n=3,997) |
Shortness of Breath (n=2,433) |
COPD (n=454) |
Asthma (n=300) |
Respiratory Depression (n=477) |
Other (n=333) |
| Congestive heart failure |
615 (15) | 477 (20) | 39 (9) | 14 (5) | 54 (11) | 31 (9) |
| Pneumonia | 397 (10) | 247 (10) | 56 (12) | 13 (4) | 34 (7) | 47 (14) |
| Acute respiratory failure |
927 (23) | 471 (19) | 126 (28) | 76 (25) | 181 (38) | 73 (22) |
| COPD | 527 (13) | 294 (12) | 143 (32) | 40 (13) | 40 (8) | 10 (3) |
| Asthma | 240 (6) | 90 (4) | 11 (2) | 123 (41) | 9 (2) | 7 (2) |
| Acute myocardial infarction |
162 (4) | 109 (4) | 13 (3) | 6 (2) | 20 (4) | 14 (4) |
| Pulmonary embolism | 70 (2) | 54 (2) | 2 (<1) | 0 (0) | 1 (<1) | 13 (4) |
| Lung cancer | 32 (1) | 24 (1) | 1 (<1) | 0 (0) | 3 (1) | 4 (1) |
| Any of the above | 2,970 (74) | 1,766 (73) | 391 (86) | 272 (91) | 342 (72) | 199 (60) |
| None of the above | 1,027 (26) | 667 (27) | 63 (14) | 28 (9) | 135 (28) | 134 (40) |
| B. Concordance of BLS diagnostic impression with primary discharge diagnosis among patients hospitalized after BLS transport for respiratory distress | ||||||
|---|---|---|---|---|---|---|
| BLS diagnostic impression |
||||||
| Primary Discharge Diagnosis* |
All Hospitalized Patients (n=5,446) |
Shortness of Breath (n=3,822) |
COPD (n=344) |
Asthma (n=180) |
Respiratory Depression (n=203) |
Other (n=897) |
| Congestive heart failure |
896 (16) | 751 (20) | 29 (8) | 17 (9) | 17 (8) | 82 (9) |
| Pneumonia | 1,000 (18) | 663 (17) | 66 (19) | 20 (11) | 32 (16) | 219 (24) |
| Acute respiratory failure |
354 (7) | 230 (6) | 36 (10) | 9 (5) | 37 (18) | 42 (5) |
| COPD | 718 (13) | 503 (13) | 135 (39) | 18 (10) | 16 (8) | 46 (5) |
| Asthma | 255 (5) | 135 (4) | 14 (4) | 85 (47) | 6 (3) | 15 (2) |
| Acute myocardial infarction | 169 (3) | 118 (3) | 8 (2) | 6 (3) | 5 (2) | 32 (4) |
| Pulmonary embolism | 128 (2) | 93 (2) | 2 (1) | 2 (1) | 6 (3) | 25 (3) |
| Lung cancer | 74 (2) | 61 (2) | 1 (<1) | 1 (1) | 0 (0) | 11 (1) |
| Any of the above | 3,594 (66) | 2,554 (67) | 291 (85) | 158 (88) | 119 (59) | 472 (53) |
| None of the above | 1,852 (34) | 1,268 (33) | 53 (15) | 22 (12) | 84 (41) | 425 (47) |
All frequencies are given as n (%).
This table presents data on the 3,997 of 5,815 patients (69%) who were admitted to the hospital following ALS transport for respiratory distress.
Categories are mutually exclusive and are defined by the following ICD-9-CM codes: congestive heart failure (428–428.9); pneumonia (480–487.0); acute respiratory failure (518.81, 518.82, 518.84); COPD (491–492.8, 493.2, 496); asthma (493.0, 493.1, 493.8, 493.9); acute myocardial infarction (410–410.91, excluding all 410.x2); pulmonary embolism (415.11–415.19); lung cancer (162.2–162.9).
COPD = chronic obstructive pulmonary disease; ICD-9-CM = International Classification of Diseases, 9th revision, clinical modification
All frequencies are given as n (%).
This table presents data on the 5,446 of 12,787 patients (43%) who were admitted to the hospital following BLS transport for respiratory distress.
Categories are mutually exclusive and are defined by the following ICD-9-CM codes: congestive heart failure (428–428.9); pneumonia (480–487.0); acute respiratory failure (518.81, 518.82, 518.84); COPD (491–492.8, 493.2, 496); asthma (493.0, 493.1, 493.8, 493.9); acute myocardial infarction (410–410.91, excluding all 410.x2); pulmonary embolism (415.11–415.19); lung cancer (162.2–162.9).
EMS personnel documented a symptom-based impression in two-thirds of respiratory distress encounters. Fewer patients received disease-based impressions, including 22% with asthma and 20% with COPD. We observed fair concordance between EMS impressions and hospital diagnoses of asthma and COPD (Tables 4A and 4B). Few patients in whom ALS providers suspected asthma or COPD were diagnosed with CHF (5%), or acute myocardial infarction (2%).
DISCUSSION
In a large, community-based cohort over 5 years, we found that respiratory distress was responsible for one in eight non-trauma, non-arrest EMS encounters. We observed that EMS patients with respiratory distress are commonly admitted, and have a hospital mortality outcome (10%) comparable to those hospitalized after blunt trauma, chest pain, or suspected stroke.16
The morbidity and mortality of prehospital respiratory distress syndromes in the current study support consensus statements identifying it as a top research priority.17,18 Notable prior work found a similar mortality rate in prehospital respiratory distress in Ontario, Canada (14%), which was improved by the addition of ALS to BLS providers.4 In our study of a two-tier EMS system, almost half of prehospital respiratory distress encounters received BLS care alone, and 64% were not transported by ALS. This suggests a robust opportunity to explore how triage within the EMS system, including those with different designs (e.g. single-tier, paramedic only) could modify the outcomes of patients with prehospital respiratory distress.
Our results may also inform ways in which EMS management of prehospital respiratory distress could be incorporated into regionalized systems of critical care. Such systems in parts of the United States currently coordinate the triage and management of patients with certain time-sensitive, critical conditions, including trauma,19 acute myocardial infarction,20 and stroke21 from the time of prehospital retrieval through hospital discharge. For patients with respiratory distress, our data could serve as the foundation for interventional trial design. For critically ill patients with prehospital respiratory failure, future research using this framework could identify early predictors of prolonged mechanical ventilation, for example, which would facilitate the decision to transport to a facility designated to provide more sophisticated ICU care.
The accuracy of EMS personnel in recognition of distinct “phenotypes” of respiratory distress has important implications. If we are to consider future treatments for prehospital respiratory distress, paramedics must rapidly identify a respiratory distress “phenotype” and select targeted therapy. We observed that EMS personnel identified airflow obstruction (i.e. COPD and asthma) with fair accuracy, but used symptom-based impressions (e.g. “shortness of breath”) more often. This reliance on symptom-based impression could, in part, reflect the limited nature of the respiratory diagnostic categories available in the electronic prehospital clinical record. Future research on EMS diagnostic accuracy could consider providing ample and specific diagnoses to EMS personnel that were not available in the present study (e.g. pneumonia, cardiogenic pulmonary edema). Without the time or advanced diagnostics of hospital-based clinicians, any assessment is challenging – and similarly difficult in other conditions.22 More precise prehospital phenotypes may derive from point-of-care measurements and multi-marker panels currently under study in the emergency department and for prehospital sepsis.23–25
LIMITATIONS
We classified patients as having respiratory distress based on the initial EMS provider’s assessment, and excluded those patients without physical exams. Our estimates are therefore conservatively biased, as other patients may have been dyspneic but were classified with alternative primary complaints. We do not have data on prehospital medication administration by EMS personnel, and are unable evaluate the association of specific interventions and patient outcomes. The concordance of EMS diagnostic impression with final hospital diagnoses may be biased if EMS personnel were influenced by the clinician assessments conveyed by hospital staff. We also studied a community sample in one U.S. county served by a single EMS system. The generalizability of our findings may be variable in predominantly rural regions, outside of the United States, and where different prehospital procedures are used (e.g. non-invasive positive pressure mask ventilation). Finally, there may have been changes in the practice of prehospital medicine or in the prevalence of certain diseases in the U.S. population since the study period (2002 through 2006), which may further limit generalizability.
CONCLUSIONS
Prehospital respiratory distress is often encountered by EMS personnel and is associated with substantial morbidity and mortality. Commonly measured patient and prehospital characteristics may identify patients with respiratory distress at a greater likelihood of requiring hospital admission. Further research into the “phenotypes” of prehospital respiratory distress may inform targeted therapy or more efficient triage and transport decisions.
Acknowledgments
Funding sources/disclosures: Dr. Prekker is receiving salary support from a National Institutes of Health (NIH) T32 Institutional Training Grant as a senior research fellow in pulmonary and critical care at the University of Washington. Drs. Feemster and Au are supported by the Department of Veterans Affairs, Health Services Research & Development. Dr. Feemster is supported in part by a grant from the NIH (K23HL111116). Dr. Seymour is supported in part by a grant from the NIH (K23GM104022). Role of sponsors: the views represented in this manuscript represent those of the authors and do not necessarily reflect those of the Department of Veterans Affairs.
Footnotes
Prior presentations: Presented at the American Thoracic Society International Conference, May 2013, Philadelphia, PA.
The authors have no conflicts of interest to report.
References
- 1.Centers for Disease Control and Prevention. [Accessed Jan 25, 2014];National Hospital Ambulatory Medical Care Survey (NHAMCS) - 2009 emergency department summary tables. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2009_ed_web_tables.pdf. [Google Scholar]
- 2.Braithwaite S, Perina D. Chapter 17. Dyspnea. In: JA Marx, RS Hockberger, RM Walls, et al., editors. Rosen's Emergency Medicine: Concepts and Clinical Practice. 7th. Philadelphia, PA: Elsevier; 1983. pp. 124–131. [Google Scholar]
- 3.Hall MJ, Levant S, DeFrances CJ. Trends in inpatient hospital deaths: National Hospital Discharge Survey, 2000–2010. NCHS Data Brief. 2013;118:1–8. [PubMed] [Google Scholar]
- 4.Stiell IG, Spaite DW, Field B, et al. Advanced life support for out-of-hospital respiratory distress. N Engl J Med. 2007;356(21):2156–2164. doi: 10.1056/NEJMoa060334. [DOI] [PubMed] [Google Scholar]
- 5.Pozner CN, Levine M, Shapiro N, Hanrahan JP. Concordance of field and emergency department assessment in the prehospital management of patients with dyspnea. Prehosp Emerg Care. 2003;7(4):440–444. doi: 10.1080/312703002144. [DOI] [PubMed] [Google Scholar]
- 6.Williams TA, Finn J, Celenza A, Teng T-H, Jacobs IG. Paramedic identification of acute pulmonary edema in a metropolitan ambulance service. Prehosp Emerg Care. 2013;17(3):339–347. doi: 10.3109/10903127.2013.773114. [DOI] [PubMed] [Google Scholar]
- 7.Singer AJ, Emerman C, Char DM, et al. Bronchodilator therapy in acute decompensated heart failure patients without a history of chronic obstructive pulmonary disease. Ann Emerg Med. 2008;51(1):25–34. doi: 10.1016/j.annemergmed.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Wuerz RC, Meador SA. Effects of prehospital medications on mortality and length of stay in congestive heart failure. Ann Emerg Med. 1992;21(6):669–674. doi: 10.1016/s0196-0644(05)82777-5. [DOI] [PubMed] [Google Scholar]
- 9.Peacock WF, Hollander JE, Diercks DB, Lopatin M, Fonarow G, Emerman CL. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008;25(4):205–209. doi: 10.1136/emj.2007.050419. [DOI] [PubMed] [Google Scholar]
- 10.Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ. 2010;341:c5462. doi: 10.1136/bmj.c5462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seymour CW, Kahn JM, Cooke CR, Watkins TR, Heckbert SR, Rea TD. Prediction of critical illness during out-of-hospital emergency care. JAMA. 2010;304(7):747–754. doi: 10.1001/jama.2010.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seymour CW, Cooke CR, Hebert PL, Rea TD. Intravenous access during out-of-hospital emergency care of noninjured patients: A population-based outcome study. Ann Emerg Med. 2012;59(4):296–303. doi: 10.1016/j.annemergmed.2011.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seymour CW, Cooke CR, Heckbert SR, et al. Prehospital systolic blood pressure thresholds: A community-based outcomes study. Acad Emerg Med. 2013;20:597–604. doi: 10.1111/acem.12142. [DOI] [PubMed] [Google Scholar]
- 14.Culley LL, Henwood DK, Clark JJ, Eisenberg MS, Horton C. Increasing the efficiency of emergency medical services by using criteria based dispatch. Ann Emerg Med. 1994;24(5):867–872. doi: 10.1016/s0196-0644(54)00223-5. [DOI] [PubMed] [Google Scholar]
- 15.Seymour CW, Iwashyna TJ, Ehlenbach WJ, Wunsch H, Cooke CR. Hospital-level variation in the use of intensive care. Health Serv Res. 2012;47(5):2060–2080. doi: 10.1111/j.1475-6773.2012.01402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dean JM, Vernon DD, Cook L, Nechodom P, Reading J, Suruda A. Probabilistic linkage of computerized ambulance and inpatient hospital discharge records: a potential tool for evaluation of emergency medical services. Ann Emerg Med. 2001;37(6):616–626. doi: 10.1067/mem.2001.115214. [DOI] [PubMed] [Google Scholar]
- 17.Maio RF, Garrison HG, Spaite DW, et al. Emergency Medical Services Outcomes Project I (EMSOP I): prioritizing conditions for outcomes research. Ann Emerg Med. 1999;33:423–432. doi: 10.1016/s0196-0644(99)70307-0. [DOI] [PubMed] [Google Scholar]
- 18.Sayre MR, White LJ, Brown LH, McHenry SD. The National EMS Research Strategic Plan. Prehosp Emerg Care. 2005;9(3):255–266. doi: 10.1080/10903120590962238. [DOI] [PubMed] [Google Scholar]
- 19.MacKenzie EJ, Hoyt DB, Sacra JC, et al. National inventory of hospital trauma centers. JAMA. 2003;289(12):1515–1522. doi: 10.1001/jama.289.12.1515. [DOI] [PubMed] [Google Scholar]
- 20.Jollis JG, Al-Khalidi HR, Monk L, et al. Expansion of a regional ST-segment-elevation myocardial infarction system to an entire state. Circulation. 2012;126(2):189–195. doi: 10.1161/CIRCULATIONAHA.111.068049. [DOI] [PubMed] [Google Scholar]
- 21.Alberts MJ, Latchaw RE, Jagoda A, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42(9):2651–2665. doi: 10.1161/STROKEAHA.111.615336. [DOI] [PubMed] [Google Scholar]
- 22.Jaronik J, Mikkelson P, Fales W, Overton DT. Evaluation of prehospital use of furosemide in patients with respiratory distress. Prehosp Emerg Care. 2006;10(2):194–197. doi: 10.1080/10903120500541282. [DOI] [PubMed] [Google Scholar]
- 23.Kajimoto K, Madeen K, Nakayama T, Tsudo H, Kuroda T, Abe T. Rapid evaluation by lung-cardiac-inferior vena cava (LCI) integrated ultrasound for differentiating heart failure from pulmonary disease as the cause of acute dyspnea in the emergency setting. Cardiovasc Ultrasound. 2012;10:49–56. doi: 10.1186/1476-7120-10-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prosen G, Klemen P, Stmad M, Grmec S. Combination of lung ultrasound (a comet-tail sign) and N-terminal pro-brain natriuretic peptide in differentiating acute heart failure from chronic obstructive pulmonary disease and asthma as cause of acute dyspnea in prehospital emergency setting. Crit Care. 2011;15(2):R114. doi: 10.1186/cc10140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seymour CW. Improving the diagnosis of infection during out-of-hospital emergency care: are biomarkers the next step? Prehosp Emerg Care. 2011;15(3):439–441. doi: 10.3109/10903127.2011.561415. [DOI] [PubMed] [Google Scholar]