Abstract
This study is set to match and compare results of the analysis of impacts of cost sharing on households with those on health-care providers in two selected districts in Tanzania. The setting is intended to establish and compare concurrently the impact of cost sharing on health-care utilization as viewed from both the providers and beneficiary households.
The findings of the study indicate that quality of primary health care has improved as a result of the introduction of cost sharing. Attendance and hence utilization in health facilities has also increased. Mortality rate, at least for one district has not worsened. By implication then, cost sharing appears to have a positive impact on the provision of primary health care, except for a few cases that fail to consult because of the fees. An appropriately managed exemption facility is likely to eliminate the negative impact.
Introduction
Policy reform for user fees in public health care in poor countries was derived from the general argument that provision of health care in those countries is so dismal that people would want to pay for some improvement1. Such arguments are augmented by prevalence of acute resource gaps and inability of the fiscal system to raise adequate funding for the health sector. The early literature on the impact of user fees on quality of, and access to public health care show mixed results with general indication that attendance in public health facilities decreased2. However, there are studies, which show that user fees plus improved services result in improved access3. In addition, a number of studies look on the impact of fees on access by various social groups with varied conclusions as well4 warns that uniform user charges in lower level public health facilities in Tanzania may be regressive, adversely affecting utilization among the poor especially women and the elderly. They therefore call for an effective exemption and waiver system in public health facilities. The government of Tanzania introduced user fees at the hospital level in the mid-1990s in line with the popular arguments for fees in public health care. To date, the government is preparing to move forward and introduce fees in sub-district level health facilities. In Tanzania, case studies on the impact of user fees have generally focused on access5. There are a few studies however that look on both quality change and access to public health care6. Though there have been many studies on the impact of user fees, a number of issues with regard to gains and losses from user fees are still unresolved. It is not yet clear whether cost sharing is generating the anticipated impacts in terms of quality improvement and universal access to basic quality health care at the primary level, particularly by those deemed vulnerable to such fees. This study examines the impacts of user fees at primary level, by bringing out evidence from the on-going Community Health Fund in two districts of Iringa (R) and Kilosa. By matching analysis of household data with that of the corresponding primary health facilities, the impacts of user fees on quality, access and utilization are systematically tracked.
Basic concepts and definitions
Access to Health-care services refers to the number or proportion of people reporting for medical attention in health-care facilities. Utilization of health services refers to the number or proportion of the consulting patients that are given medical services including medical consultation. Poverty is commonly measured in the form of indices. In absolute terms, the proportion of a given population is said to be basic-needs poor if they fail to meet the expenses of the commodity bundle defined as a necessary consumption to live the minimum standard life in a given economy. Anonymously, food poor people are those unable to afford the basic calorific inputs defined as necessary for human being survival in a given particular economy.
The Problem Context and Issues
Increased vulnerability to cost sharing in public health services has made some countries to review or abandon the policy. The pressure does not exclude Tanzania as it is faced with cost sharing system that has not yet probably registered significant benefits. To date, possible extension of cost sharing to the level of dispensary and health centre is confronted with the challenge that “cost sharing excludes the poor because it lacks an effective system of exemptions and waivers that is necessary to protect vulnerable social groups” Also, concerns are there as to whether the revenue cum benefits generated from cost sharing more than offset the resulting negative effects, particularly exclusion of the poor. There are also emerging challenges as to why one should extend user fees to the grassroots level-health service outlets, and at the same time abolish school fees at primary level. The research concern here is whether extending user fees to primary health facilities in Tanzania will improve services and at the same time ensure universal access to the services particularly by the poor. How much revenue is generated and at what forgone benefits are key issues towards nationwide rollout of the cost-sharing policy in health services. These are issues which have not yet been exhaustively analysed for better understanding of the implications of cost sharing on the grassroots level health facilities. Clearly then, establishing the impact of cost sharing on service utilization in primary health care will give direct implication on the attainment of the government strategy for growth and poverty reduction (MKUKUTA). This is because of the obvious link between health and poverty. Sickness reduces one's capability and activeness in economic undertakings. If sick people are not able to get required medical treatment on the right time, days of illness will be prolonged let alone the risk that the person may die. In either case, poverty is increased. The rural population is particularly at risk because many of them are poor and the choice of provider of medical care is limited. User fees target to improve quality of health care and in due course enhance access to health services. The aim of introducing user fees is to generate funds that can be invested in the health care system to improve quality of health care, making services regularly available and in due course increase access. Also, of prime concern is whether exemptions and waivers effectively protect those social groups, which are considered vulnerable to user fees, particularly at the level of health centre and dispensary.
Vulnerable groups include the poor, children, disabled, etc. This study, therefore, examines the Tanzanian experience with user fees with particular reference to potential exclusions and possibility of extending the fees to primary health facilities. Thus, this study focuses on the following main objective: Provide an evidence-based analysis of the extent to which the anticipated benefits of user fees at the dispensary level have been attained and the disadvantages have been mitigated.
Arguments for and against cost sharing
Health care financing in Tanzania
Tanzania is in the bottom list of the poorest countries (with estimated GDP per capita of $240) with about 80% of its people living in villages in rural settlements. About 38% of the people are below national poverty line. A study by Smith and Rawal in 19927 showed that 80% of people in Tanzania were willing to pay a small fee in medical care, in order to improve the then deteriorating health services. On the basis of the results and the then popular arguments for user fees, the government introduced user fees in health care services in 1993. The studies that were carried out immediately after the introduction of fees show that the rate of drop out was alarming8. Along with the negative impact of user fees, Mushi (2001)9 found that consumers' knowledge on the benefits of health care and their perceptions of quality of medical care have far reaching effects not only on price sensitivity but also on the choice of the provider of health care. Cost sharing in the public health sector has been operational in Tanzania for about thirteen years now. There are good lessons to learn and ill experiences that have been identified in various studies on user fees. The studies include those which have been carried out in and outside Tanzania to assess the impact of the cost-sharing program from the late 1980's onwards. On the basis of the results and the shortfalls of the methodologies employed, we provide a critical review of the contribution of cost sharing in the improvement of the delivery of health services in Tanzania. The review here, which we call impact assessment of cost sharing, is divided into two; review of findings from the early and the more recent studies on cost sharing in Tanzania and those from the recent actual impact assessments by hospital management teams themselves. As it is commonly argued, cost sharing is not the only barrier to accessing health care in Tanzania; there are other more binding constraints, which we also discuss in this report. Of recent is the argument that abolition of cost sharing in health services will improve utilization, particularly by the poor because the exemption and waiver facilities are inefficient. Drawing from the past experience, before introduction of user fees, the reasons that led the government to introduce cost sharing, and the achievements made so far, this study argues critically on the likely effects of abolishing the cost-sharing program in Tanzania. This is further augmented by the experience of other countries in the sub region that have recently abolished user fees in Public health services.
Review of the recent arguments against cost sharing in Tanzania
Broadly, we distinguish between two sets of studies on the impact of cost sharing; those which were done prematurely during the implementation period - i.e. around the first five years of the programme, and that which were done later after full implementation of the programme - i.e. roughly after the year 2000. As commonly argued in the theory, a sudden price change is associated with demand or consumption shocks that tend to level down overtime. Precisely, this effect is depicted by the early studies on cost sharing in Tanzania, which found that access to health care declined as a result of the introduction of user fees as indicated earlier in Section One. The studies focused on assessment of access to health care from household interviews and opinion survey data. The finding that initially user fees reduce utilization is common in many countries that have introduced cost sharing. This has been described as a sudden price change whose effect sustains for a short period. In Tanzania, this pattern has been confirmed by the results of recent studies on the impact of cost sharing, which we discuss next. Looking now on the results of recent studies on cost sharing, we note that there have been mixed results. On one hand, there are studies whose results indicate that the poor and other vulnerable social groups fail to access health care because of user fees. But on the other hand there are studies whose results suggest that cost sharing is delivering the intended objectives except that the exemption and waiver facilities are inefficient. Also, there have been a number of surveys, which included some interviews to probe on how households cope with reforms in the health sector; their results show that the proportion of households that fail to access health care because of the inability to meet treatment costs is far smaller than that predicted by the early studies on cost sharing. Generally then, the studies which were done immediately after the introduction of user fees in public hospitals indicate that access to health care declined significantly as a result of the programme. However, the more recent studies on the same issues show mixed results but focus more on the failure of the exemption and waiver facilities to protect vulnerable social groups from the negative impact of the policy. Where is the bottom line then? First, we critically look on the methodologies that generate the results and the emerging conclusions. With an exemption of very few, the studies on the impact of cost sharing build their arguments from household surveys designed for that purpose. We note two main weaknesses with the approach and the methodology employed. The government has not yet introduced cost sharing in primary health services which are of great concern to rural communities. The Community Health Fund was by then being piloted in only 16 districts out of 116 i.e. 14% of all districts. By implication, all people access free primary health care except few districts - about 42 out of 116 -that are piloting Community Health Fund (CHF). It follows that the access which should be referred to here is access to public hospitals and not access to basic health services - except the 42 districts. To the contrary, the studies that are purely based on household interviews cum opinion do not control for this dichotomy; they randomly selected respondents from many districts including those which have not yet introduced cost sharing at the primary level facilities. As a result, the findings exaggerate the impact of cost sharing as they bias against those districts which had not yet introduced user fees in dispensaries and health centres at the time of the surveys. This anomaly is even more serious with the findings of the early studies because none of the 116 districts had effectively introduced cost sharing in primary health services before 1999. Second is the single sourced data that explain the impact. Many of the findings of studies on impact of cost sharing are based on opinion survey of households. They do not go beyond to assess changes in utilization in health facilities and mortality rates. These are serious limitations of such studies.
Experience with user fees in other countries
Usually, there are few people who, in the normal course of events, would willingly consume health care purely for its consumption effects on their utility function. Many studies have defined demand for medical care as the probability that an individual seeks medical care in the event of illness. Two broad categories of literature on public health care financing are identified in this approach. One category looks at fees (user fees and insurance schemes) as an alternative source of additional resources for financing public care. This is essentially because the studies found demand to be price inelastic10; and household willingness to pay was therefore high: implying that small fees could be introduced without huge drop outs. However, recent empirical studies have varied conclusions, although there is a general view that demand for public health care has declined as a result of user fees11. A few studies have shown that the fall in demand was later on reversed12. It is also argued that user fees with reinvestment in quality improve utilization13. The mixed results arising from these studies suggest that the basic problem is still at hand. We are not sure whether poor quality free health services are more preferred in the place of fees for improvement. We don't know yet the actual opportunity cost associated with each method we opt for, let alone the benefits in terms of social welfare.
For example, a study on user fees in Bangladesh14 found that only a small per cent of household resources were spent on health (less than 1% of their stated annual income). The observation that food expenditure accounted for 72% of all household expenditure in approximately one half of Bangladesh households suggested that the small amount spent on health may well be all that is affordable; to spend more may result in withholding of other subsistence resources, which are also essential to health maintenance. It was therefore found that the cost of allopathic medicine deterred families from seeking such care, especially the poorest families.
Experience from Community Health Funds in Tanzania
Parallel with user fees in public health services in Tanzania, the government introduced community health funds (CHF) as a pilot initiative in selected districts in Tanzania. CHF started in 1995 with the general objective of improving the quality of health services in addition to mobilizing additional resources for the provision of the same. The scheme targeted rural population and the informal sector. The operation of CHF differs slightly between districts. In general, households cum individuals are invited to pay a specified annual member ship fee that provides for health services within the terms of contractual arrangements by the two sides involved; the individual and the respective public health service outlets. Those who are either unable or unwilling to participate in the CHF follow the normal cost-sharing programme; that is pay on cash basis at the service outlets. Currently, CHF is operating in more than 42 districts in Tanzania. The experience drawn so far from the initiative is encouraging. We shall briefly discuss two interesting cases of Hanang and Igunga districts. The CHF scheme in Hanang required that each participating member pay a fee of TZS 10,000 (equivalent to US$ 6.25) annually. In return, one gets unlimited access to outpatient services in CHF participating service outlets. The non-participating members are served under the earlier cost sharing programme arrangements. A study by consultants from Abt Associates Inc. in 2002 showed that most community contributions for the health services in Hanang came from user fees and not CHF. Enrolment rates for the CHF were fairly low; it was estimated that compliance with the CHF rates was 2.8% of all households in the district. In addition, CHF contribution to health services was only 20% of the total fees collected from health services. In Igunga, a follow up study shows that revenue from cost sharing had increased remarkably. The study shows further that problems of drug shortage had been resolved once and for all. However, the study indicates that by 1999 only 5% of the targeted families had joined CHF. Similarly, in Singida district, it was only 4.1% who had joined the fund. The current study makes two important contributions with regard to the impact of user fees in health care services. One is to bring out explicitly the impact of user fees at the dispensary level; and second is to match two panels of impacts, the households and health facilities. This will bring out matched impacts of quality and access at the facility cum community level.
Methodology
This study is set out to match household data (collected in 2003) and health care providers' data of 1999 – 2005 for which cost sharing became effective. The data were collected from Iringa and Kilosa districts to include three wards cum communities from each district. The selection of the wards for this study follows the matching household data for Kalenga, Ulanda and Mseke wards in Iringa Rural; and Chanzuru, Kibamba and Ulaya wards. Each of these wards has a primary health care facility which compiles routine information on patients' attendance, consultation, collection of revenue, expenditures from revenues, facility capacity, staffing, exemptions and waivers, medical equipment, availability of drugs, utilization of the medical services, etc.
The matching household data for the selected primary health care facilities in Iringa (R) and Kilosa came from a survey of health-care utilization and community health fund. The survey, which covered 500 randomly selected households, was carried out at the end of 2003 to assess compliance with the community health fund (CHF) in the selected six wards of the two districts. The sampling protocols ensured a sample of respondent households which is proportional to the total population of the six wards purposefully selected for the study. The main survey questions included incidences of illness in the last twelve months, medical consultation from various sources of providers, utilization of exemption and waver facilities, health seeking behaviour and cost of access to health services, incomes and expenditure, assessment of quality of services of the providers of health services, availability of medicine, general cleanliness, patients' handling, etc. Heads of households were the survey respondents who gave information about themselves and the rest of the members of the household. The data were computerized in the SPSS Program for cleaning and carrying out explorative analysis; and thereafter transferred to the STATA Programme for a more rigorous analysis. From the household data, we compute and find out food-poor versus non-food-poor households using the standard World Bank approach to Household Budget Survey (HBS). We thereafter found out the status of access to health care by each of those groups identified by their status of poverty. Up to this stage, we were able to determine the impact of cost sharing from the consumers' (households) point of view. Second, we compiled data on access to health care, revenue collection and expenditure from the corresponding primary health facilities. These include health centres and dispensaries found in those wards and villages covered by the 2003 household interviews. We made analysis of the facilities' data to assess attendance by the various social groups over time, under-five mortality rates and quality improvements from cost sharing. Cost sharing in Primary Health services became effective in Iringa (R) and Kilosa districts from 1999–2000. Under the program, households have two options of paying their medical bills. One is over-the-counter direct payment by cash upon receipt of services in public health-service outlets; and the second is pre-payment through the Community Health Fund (CHF). Under the latter option, each participating household pays a fixed amount per year to cover all the household medical expenses in public primary health facilities within the district. In the year 2003, for example, the CHF annual premium was Tshs 5,000. Unfortunately, the data on revenue collection by ward is not available. Primary health care units do not employ accountants to prepare and keep records; neither do they keep records of their expenditure from cost sharing revenue. All the revenue is deposited into a common district-level account that is managed by the DMO. Thus, data on cost sharing revenue is mainly available at the district level. Generally, in principle, cost sharing constitutes a barrier to accessing health care because of the price effect. In rural settlements, options for payment of medical bills are two: pay and access health care, or don't pay and seek care from cheaper informal sources including self-care. Private sources of modern health care are rarely available in rural areas. This implies that those who drop out from public health services, as a result of the fees, cannot seek same care elsewhere, they go to inferior sources; and thus we regard them as not being able to access health care. However, there are other reasons why people fail to access health care. These include poor quality of health services, transport costs, etc. These factors can be isolated from each other by examining both health-care seeking behaviour at household level and attendance in the health facilities that serve the respective catchment population. Though however, in principle as quality of health care improves morbidity rates are likely to decline and hence reduce attendance in clinics. Along with the introduction of cost sharing in primary health facilities in Iringa (R) and Kilosa districts, the government has improved public health services delivery by ensuring a more regular inflow of medical supplies at all levels. This has led to a significant improvement in health care services at all levels. Thanks to the effort by our development partners and non-government organizations who are working in the sector. With assured inflow of medical supplies, revenue collected from cost sharing is mainly used to carry out minor renovations, extensions of health facility premises and occasional purchases of medical supplies in case of shortages. However, all the procurements paid from cost sharing revenue must be approved by the respective Health Unit Committee and the District Medical Officer (DMO). We therefore note two main sources of improvement of public health services: the increased regular government medical supplies and the spending from cost sharing revenue. Surely, separation of the two impacts will require more detailed data; both sources of improvement have impact on quality, though however cost sharing induces a negative impact on utilization. The latter is precisely our focus; whether as cost sharing revenue improves quality, attendance cum utilization also increase. To bring out such a relationship, we carry out assessment of service utilization in the selected primary health service outlets concurrently with the assessment of health seeking behaviour and costs for households that attend care in the respective service outlets. The impact of cost sharing is thus analyzed from two fronts. One front is to assess attendance in primary health facilities in the selected districts. This is to examine whether there have been drop outs from usage of primary health facilities as a result of cost sharing. And on the second front, we track drop-outs from the corresponding household data to establish whether the impact is on the poor; and if so what is the magnitude. Of course, as it has been established in many other studies, the answers to the problem are not so direct; there are several analytical problems as we have been pointing out.
Results and Discussions
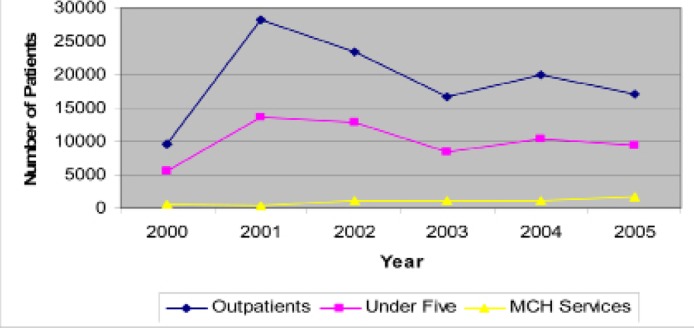
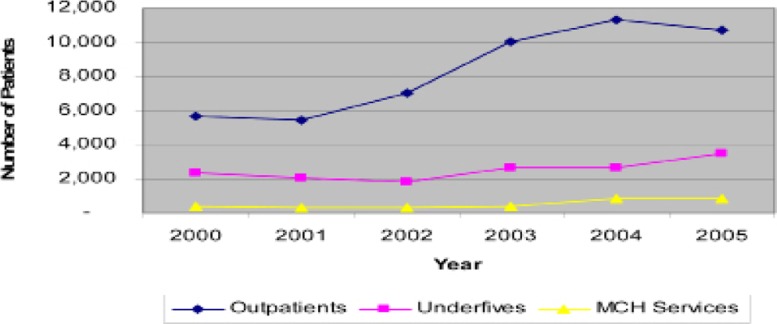
Figures 1 & 2 depict attendance by category of patients in the selected primary health facilities in Iringa (R) and Kilosa for the last six years. Kilosa indicates a continuously rising attendance in MCH services, but a more sharply rising attendance for outpatients and under-five for the year 2001 before declining in the subsequent years.
Figure 2.
Patients attendance by social groups in Kilosa district council
MCH and under-five medical services in public health units are usually free of charge as per the cost sharing policy document. Under normal circumstances then, the declining attendance for the under-five should not be due to cost sharing. Even though, the sharp increase noted in Kilosa came when the fees were in place, and thus the declining pattern since 2002 does not reflect an impact from cost sharing; it is a descending pattern that went to normalize attendance basing on the year 2000. However, we also observe further from Figure 1 that in general, attendance by all categories of clients stand at higher points in 2005 compared to the year 2000 when cost sharing became effective. The rates of attendance by all categories of patients had almost doubled by the year 2005. In Figure 2, we observe a continuously rising attendance of all categories of clients in Iringa. In fact, the increase in the number of outpatients, the user-fee paying category, recorded the highest jump. Definitely, there are several logical conclusions that we can make from the trends even before going to analyze the household data.
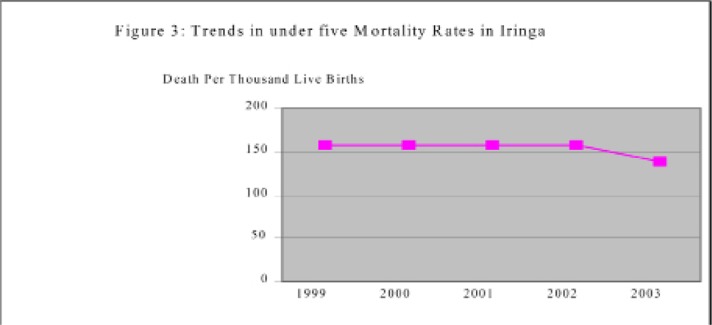
The first conclusion from our analysis of facilities data is that we do not observe a decline in attendance that is directly a result of the cost sharing program. However, in the early years of the program, price shocks reduced attendance which is thereafter levelled up with time. Secondly, the trends suggest that in general there are no households which have been cut off completely from public health services. The average increase with time in both Iringa (R) and Kilosa suggests that even the poor have been taken on-board-but this require further evidence from mortality rates and household data as we indicate in the nextsections. Third is the effectiveness of the waiver and exemption mechanisms. Waivers in public health facilities are discretional short term entitlements to free medical care. These are usually granted by the respective facility management teams; they target patients who for some known reasons fail to pay their medical bills in public health facilities. Exemptions are statutory entitlements, and thus are non-negotiable, that benefit under-fives children and maternal cases. Patients' attendance by the various social groups, as noted in Figure One and Two, does not depict a declining trend; in fact, by the end of 2005, all groups had their attendance increased as compared to the year 2000. By implication then, these results do not suggest that exemptions are totally ineffective as we will give further evidence in the coming sections. Under-five mortality rate is now commonly used as an indicator of the performance of the health sector and the health of the general population. Studies have confirmed strong relationship between under-five mortality rates and the health of the general population. If cost sharing constitutes a barrier to health care we would expect mortality rates for children to worsen and thus the health of the general population. This situation is not depicted in this study, at least for Iringa district whose data for under-five mortality is available.
The trend shows that mortality rate for under-fives remained the same after the introduction of cost sharing; in fact in 2003 a slight improvement was recorded. The trend provides evidence that quality of health care and access to it did not decline after the introduction of cost sharing. The interviewed health facilities indicated several achievements with regard to quality of health care that directly relate to the introduction of cost sharing. The first is improved availability of drugs. Revenue from cost sharing is used to purchase drugs when the usual monthly drug kit supplied by the government runs out before the end of the month. Second is minor rehabilitations including expansion of physical facilities. This has led to an improvement in the physical structures of public health care delivery units. Third is payment of bills for consumption of utilities and security guard for the health facilities. These also include casual employment of staff for cleaning up the facilities. These are services which are not regularly paid for by the central government. In some areas, for example Ulaya ward in Kilosa, communities have managed to build a patients ward for MCH services This include installation of regular water supply. But important also on quality improvement is control and resource management dimension that is associated with cost sharing. With fees, both the clinical staff and clients become somehow more efficient in the management of resource. The clinical staffs have to account for every tablet received as they submit financial reports on procurement and sales. On the other hand, clients have become more careful first in the decision to consult, and second on the prescription and drugs they buy from hospital pharmacies. This has discouraged abuse of health facilities. The financial contributions also inculcate a sense of ownership and responsibility from the catchment population. These are aspects of quality that are difficult to attain in a free public health care regime. However, there are also several reported problems with regard to the cost sharing policy. These include poor management of the funds collected from cost-sharing, inability to pay for some of the consulting patients, complementary services like competent clinical staff that would make cost sharing more effective are not in place across all primary health facilities. These are problems cum challenges that compromise the achievements of the policy.
Results of the Analysis of the Matching Household Data
The research claim of this paper, as stated earlier, is that impact assessment of user fees on access to public health care has to take both the provider and the household data on board. Facilities have records on utilization, revenue and expenditure from cost sharing. On the other hand, we cannot establish which type of families and individuals that are denied health care unless we interview and analyse household information on illness and health care. This is precisely the idea of matching facility and household data. The analysis of data from public dispensaries and health centres above does not provide a distinction between poor and non-poor segments of the population in question. Further, we cannot qualify the increasing attendance with certainty that the poor are on board. Surely then, we need deeper analysis to explain the upward trends in consultations in primary health facilities in the selected areas. This is what we do next. The matching household data for the selected primary health care facilities in Iringa (R) and Kilosa come from a survey on health-care utilization and community health fund. The survey, which covered 500 households, was carried out in the end of 2003 to assess compliance with the community health fund (CHF) in the selected six wards of the two districts. This study analysed the data to find out and compare the matching evidence of the impact of cost sharing on access to public primary health care.
The data indicate that 56.6% of all the members of interviewed households reported at least one episode of illness in the last twelve months. Of those reporting illness, 52% were not entitled exemptions in public health facilities. The data has information on household consumption, similar to that compiled by the World Bank Household Budget Survey (HBS). From the data, we computed household poverty profiles based on adult equivalent scales. The results indicate that 16% of the sample households are poor. Of the poor cohort, 46% reported illness last twelve months. The analysis showed further that of all reporting illness in the sample, 13% are poor. And of all the non-poor, 59% reported illness for the last twelve months. We note from this analysis that the non-poor report higher morbidity rates than the poor, and hence, by default, they consume more health care than the poor. Analysis of data indicate further that of all the households reporting illness in the sample, 21% did not consult public nor private allopathic sources of medical care; and we do not observe significant differences between the poor and the non-poor.
But more interesting in this paper, are those who did not seek care (the 21%). What were the reasons for not seeking care? How this observation is related to the previous results from the analysis of the facility data? We observe in Table 1 that the major hindrance to accessing health care is transport cost. About 22.7% of those with major illness failed to access health care because they had no money to pay for transport. These include both the poor and the non-poor. Travelling costs accounted for a substantial expenditure in accessing health facilities because of the travelling distance. This can be higher than the anticipated cost of treatment and thus making access to health services exorbitantly high. Of all who did not consult for medical care, 4.5% did so because they did not have money to pay for the expected treatment. And majority of these were the poor though are a small number in absolute dimension. The Table indicates further that majority of those poor households who did not seek medical consultation did so because they considered the respective illness as minor. This is in fact 75% of all the non-consulting poor people. How then do we explain the results of the analysis of the health facilities' and households' data? First we find that the overall negative impact of user fees on access to health care is 4.5% of the reasons why people do not consult in the event of illness. Analogously, the impact on the poor is 12.5% for those reporting illness in the last twelve months. However, this effect was not observed at the facility level, which suggests that the impact of quality on attendance would offset the negative impact of user fees if the exemption and waiver facilities are fully functional. But at the same time, the quality effect that originates from the on-going government effort and the spending from the user-fee revenue has increased consultation in public medical facilities particularly by the non-poor. The positive effect on attendance more than offsets the negative effect for the non-poor. This suggests that there are a few households who cannot access medical care in public health facilities because of the fees. This calls for further improvement of the waver mechanisms to make the quality effect fully inclusive of all social groups.
Table 1.
Reasons for not seeking medical care
| Stated reason | Percent of non-poor stating (n = 248) |
Percent of poor stating (n = 80) |
Percent of all who didn't seek care (n = 60) |
| Minor illness | 40.6 | 75 | 43.8 |
| No one to accompany the sick |
10.6 | 9.7 | |
| Could not afford to pay for medical services |
3.8 | 12.5 | 4.5 |
| Lack of money to pay for transport |
24.4 | 6.3 | 22.7 |
| Chronic diseases | 8.7 | 6.3 | 8.5 |
| Other reasons | 11.9 | 10.8 |
Concluding Remarks and Implication of the Results
The claim of this study was that the impact of cost sharing on quality and utilization of health services should be approached from both the provider and the clients cum households. The analyses in this paper are based on the two sides. We collected data on selected primary health care units in Kilosa and Iringa districts. We then analysed the data to look on the trends of patients' attendance by various social groups. Along with the trends, we analysed mortality rates as proxy to the general health of the population and quality of health care. The combined analysis of the facilities' and mortality data was matched with analysis of matching household data from the catchment communities. The results of the analyses indicate that quality of primary health care has improved. Attendance and hence utilization in health facilities has also increased. Mortality rate, at least for Iringa, has not worsened. By implication then, cost sharing appears to have a positive impact on the provision of primary health care, except for a few cases that fail to consult because of the fees. An appropriately managed exemption facility is likely to eliminate the negative impact.
As long as quality primary health care is regularly available and accessible, economic activities at household level will be smoothened; more regular labour force will be available for regular agricultural production as days of illness and walking distances are reduced. Poor quality of primary health facilities will imply that sick people walk long distances in search of health care or stay long before attending care. This increases poverty. The government is not yet able to fully finance all medical requirements at the primary level. At the moment, community contributions appear to be the only reliable and sustainable long term financing option.
Figure 3.
shows under-five mortality rates for Iringa between 1999 and 2003.
References
- 1.Mwabu G, Mwangi W. Health –Care Financing in Kenya: A Simulation of Welfare Effects of User Fees. Social Science and Medicine J. 1986;22:763–767. doi: 10.1016/0277-9536(86)90228-5. [DOI] [PubMed] [Google Scholar]
- 2.Hongoro C, Chandiwana S. A study financed by UNICEF in collaboration with Harare Blair Research Laboratory and Ministry of Health and Child Welfare. 1994. The Effects of Enforcement of User Fees on the Health-Care Delivery System in Zimbabwe. [Google Scholar]
- 3.Litvack J, Bodart C. User Fees plus Quality Equals Improved Access to Health Care: Results of a field Experiment in Cameroon. Social Science and Medicine J. 1993;37:369–383. doi: 10.1016/0277-9536(93)90267-8. [DOI] [PubMed] [Google Scholar]
- 4.Mbugua JK, Bloom G H, Segall M. The Impact of User Charges on Vulnerable Groups: The Case of Kibweziin Rural Kenya. Social Science and Medicine J. 1995;41(6):829–835. doi: 10.1016/0277-9536(94)00400-n. [DOI] [PubMed] [Google Scholar]
- 5.Husein A K, Mujinja P G M. Impact of User Charges on Government Health Facilities in Tanzania”. East African Med J. 1997;74(12):751–757. [PubMed] [Google Scholar]
- 6.Leonard K, Mlinga G. “Bypassing Health centres in Tanzania: Revealed Preferences for Quality” A Conference Paper. CSAE, University of Oxford; 2000. Apr, (2000) [Google Scholar]
- 7.Smith B, Rawal P. Health Sector Financing Study for the Government of Tanzania. Report on the Potential for Cost Sharing - First Report. 1992 [Google Scholar]
- 8.Mushi D. A Case Study of Selected Regions. Research Report submitted to CDR-Copenhagen and the Economic Research Bureau of the University of Dar es Salaam; 1996. Cost Sharing in Health Services in Tanzania: Preliminary Impact on Quality, Affordability and Accessibility. [Google Scholar]
- 9.Mushi D. Demand and welfare in Health Care: Effects of asymmetric information and user charges. 2001. PhD Thesis Oxford University. [Google Scholar]
- 10.Heller P. A Model of the Demand for Medical and Health Services in Peninsular Malaysia. Social Science and Medicine J. 1982;16:267–284. doi: 10.1016/0277-9536(82)90337-9. [DOI] [PubMed] [Google Scholar]
- 11.Mwabu G, Mwanzia J, Liambila W. User Charges in Government Health Facilities in Kenya: Effects on Attendance and Revenue’. Health Policy and Planning J. 1995;10(2):164–170. doi: 10.1093/heapol/10.2.164. [DOI] [PubMed] [Google Scholar]
- 12.Waddington C, Enyimayew K. A Price to pay: the impact of user charges in Ashanti-Akin District, Ghana”. Health Planning and Management J. 1989;4:17–47. [Google Scholar]
- 13.Griffin C. Welfare Gains from User Charges for Government Health Services. Health Policy and Planning J. 1992;7(2):177–180. doi: 10.1093/heapol/7.2.177. [DOI] [PubMed] [Google Scholar]
- 14.Stanton B, Clemence J. User Fees for Health Care in Developing Countries: A Case Study of Bangladesh”. Social Science and Medicine J. 1989;29:1199–1205. doi: 10.1016/0277-9536(89)90363-8. [DOI] [PubMed] [Google Scholar]