Abstract
Hospitals and specialists in the UK are increasingly prescribing and dispensing off-license drugs such as ketamine which are not routinely included in the prescribing record of the general practitioner (GP). We present the case of a 67-year-old woman who developed an episode of uncontrolled raised blood pressure (BP) (224/124 mm Hg) following hospital introduction of oral ketamine for chronic pain. This raised BP was not followed up, and she was then found to be persistently hypertensive in the community some months later. No obvious cause for the patient's increase in BP could be identified. Only on reduction of the ketamine dose and introduction of additional antihypertensive medication, did her BP normalise. We postulate that long-term ketamine use may have been associated with this unexpected and persistent rise in BP. Clinicians should monitor BP closely during ketamine therapy and be wary of new hypertension associated with its long-term use. Further research is needed on the long-term effects of ketamine on BP.
Background
Fifty years on since the discovery of ketamine, the list of clinically beneficial properties of ketamine is growing: the potentiation of opioid analgesia, anti-inflammatory and antitumour actions and preventive effects on recall and awareness during general anaesthesia.1 At subanaesthetic doses ketamine is also used as an analgesic in a wide range of pain settings including chronic neuropathic pain and intractable cancer pain. Although the use of ketamine as an analgesic is now generally accepted, a review of oral ketamine highlighted the limited evidence on the efficacy and safety of ketamine in chronic pain management.2
One aspect of long-term ketamine use that remains understudied is its potential effect on blood pressure. The effects of ketamine are dose-dependent and produce cardiovascular and respiratory stimulation. Intuitively, ketamine pharmacodynamics and observed physical signs by recreational users attending emergency departments suggests the potential to increase blood pressure.3 4 It is these long-term effects of sustained ketamine use in patients with chronic pain (and now more recently as adjunct in treatment-resistant depression) that are less well studied.5
Case presentation
A 67-year-old woman with a background history of lumbar intervertebral disc disease and chronic pain, developed an episode of uncontrolled raised blood pressure (224/124 mm Hg) in late 2012 during a planned lidocaine infusion at a specialised pain clinic and approximately 1 week after starting oral ketamine (initially ketamine 20 mg four times per day, which was increased to 20/20/20/30 mg daily in late October 2012). This raised blood pressure was found to be persistent when she attended for a routine hypertension check at her general practice in mid-February 2013 when her blood pressure was found to be 206/126, confirmed on repeated clinic and home measurement over the next few days.
Investigations
There was no clear reason for her increase in blood pressure identified (normal clinical examination, urinalysis negative for blood and protein, and normal serum creatine, estimated glomerular filtration rate and urinary metanephrines. Thyroid and glucose tests were normal. There was no deterioration of her kidney function when she was started on lisinopril which would rule out renal artery stenosis.
Treatment
Although a diagnosis of hypertension was made in 2008, initially treated with amlodipine 5 mg, then switched to bendroflumethiazide 2.5 mg in December 2011 because of adverse effects, her blood pressures on this single medication at her 6-monthly reviews were well controlled (129/73 in February 2012; 135/78 in August 2012). She was also treated with simvastatin 40 mg and aspirin 75 mg because of a high predicted cardiovascular risk score, and was taking long-term paracetamol and tramadol modified release 200 mg twice a day for pain.
After discussion with the pain service, her ketamine dose was reduced to 10 mg four times per day and she was started on lisinopril which was rapidly titrated to10 mg daily. Her blood pressure fell, but remained >170/110 mm Hg on home monitoring. In early March 2013, her ketamine was discontinued and this was associated with a reduction on blood pressure to ∼160/100 on home monitoring. She was subsequently started on bisoprolol 5 mg.
Outcome and follow-up
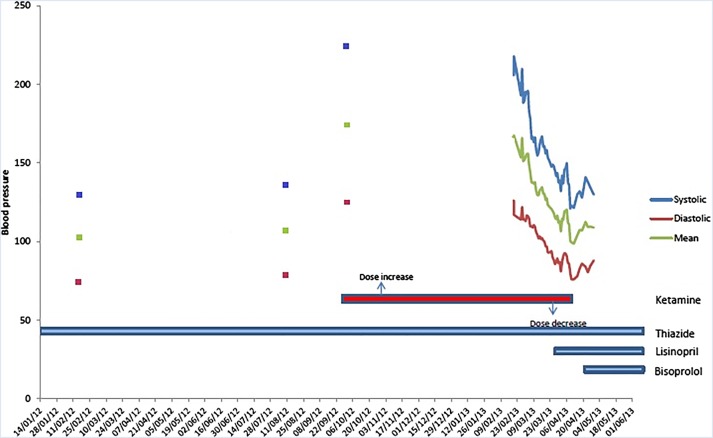
Over the next 6 weeks her blood pressure fell to 125/80 on home monitoring. Withdrawal of lisinopril led an increase in blood pressure to ∼145/85 on home monitoring, and it was restarted. She remains well controlled on bendroflumethiazide 2.5 mg, lisinopril 10 mg and bisoprolol 5 mg with a clinic blood pressure of 131/76 in October 2013. Figure 1 summarises her blood pressure monitoring and treatment over the period in question (figure 1).
Figure 1.
Blood pressure monitoring and treatment.
Discussion
Pain specialists not infrequently use ketamine at subanaesthetic doses to treat therapy-resistant chronic pain syndromes, especially those with a neuropathic pain component.6 However, the evidence for its use in this context is limited and the risk-benefit trade off even more uncertain.7 8 It seems that there are likely different mechanisms of action in play at different dose ranges, with varying effectiveness in different pain conditions and hence also adverse reactions.9
Ketamine used acutely for anaesthesia or recreationally is known to increase blood pressure, sometimes dramatically (due to inhibition of the reuptake of catecholamines), but knowledge about the long-term side effects of oral ketamine for treatment of chronic pain is limited. It is unclear if ketamine caused this patient's blood pressure rise or whether this was a dramatic worsening of her essential hypertension; the persistence of her raised blood pressure and requirement for increased treatment was unexpected, since in acute use ketamine withdrawal leads to blood pressure normalisation. However, she had a very large and otherwise unexplained increase in blood pressure (>80/40 mm Hg rise) from her baseline, and the timing is consistent with ketamine being implicated.
In the UK, general practitioner (GPs) prescribe virtually all drugs taken by people in the community, but hospital-dispensing of rarely used and potentially risky drugs is increasing. Of note in this case is that the identification of ketamine as a potential cause was made by the patient because her ketamine was being prescribed and dispensed by the pain service. Although ketamine was recorded as being dispensed in letters from the hospital to the GP, it had not been entered into the GP prescribing record and was therefore not immediately visible. Unless these drugs are manually entered into GP prescribing systems, they will not trigger electronic interaction checks and may not be considered as the cause of adverse effects.
There is little literature relating to the recording of blood pressure measurements during the long-term use of ketamine for chronic pain10 11 and more recently treatment-resistant depression.5 If blood pressure was recorded, this was only measured during, for example, a ketamine infusion.6 We only found one case series (n=32) that specifically studied the side effects of ketamine over 3 months when used to treat chronic (neuropathic) pain associated with diabetic polyneuropathy and postherpetic neuralgia.12 The study reported no increase in blood pressure in the 23 patients who completed 3 months follow-up. However, this would not preclude oral ketamine causing significant blood pressure rises in a small proportion of susceptible individuals. Further research is needed on the long-term effects of ketamine on blood pressure.
Learning points.
Clinicians should consider regularly measuring the blood pressure of patients who are on long-term ketamine therapy.
If new hypertension is noted during ketamine therapy, then blood pressure should be closely monitored and ketamine treatment reconsidered.
Hospitals and specialists in the UK are increasingly prescribing and dispensing off-license drugs, which increases the risk of misattribution of adverse drug events, requiring careful communication of what is being dispensed by the hospital, and recording of hospital dispensed medication in the general practitioner prescribing record.
Footnotes
Contributors: BG collected and analysed clinical data. OVH performed the literature search and drafted the initial manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hirota K, Lambert DG. Ketamine: new uses for an old drug? Br J Anaesthesia 2011;107:123–6. [DOI] [PubMed] [Google Scholar]
- 2.Blonk MI, Koder BG, van den Bemt PMLA et al. Use of oral ketamine in chronic pain management: a review. Eur J Pain 2010;14:466–72. [DOI] [PubMed] [Google Scholar]
- 3.Weiner AL, Vieira L, McKay CA Jr et al. Ketamine abusers presenting to the emergency department: a case series. J Emerg Med 2000;18:447–51. [DOI] [PubMed] [Google Scholar]
- 4.Ng SH, Tse ML, Ng HW et al. Emergency department presentation of ketamine abusers in Hong Kong: a review of 233 cases. Hong Kong Med J 2010;16:6–11. [PubMed] [Google Scholar]
- 5.Diamond PR, Farmery AD, Atkinson S et al. Ketamine infusions for treatment resistant depression: a series of 28 patients treated weekly or twice weekly in an ECT clinic. J Psychopharmacol 2014;28:536–44. [DOI] [PubMed] [Google Scholar]
- 6.Sigtermans MJ, van Hilten JJ, Bauer MCR et al. Ketamine produces effective and long-term pain relief in patients with complex regional pain syndrome type 1. Pain 2009;145:304–11. [DOI] [PubMed] [Google Scholar]
- 7.Niesters M, Martini C, Dahan A. Ketamine for chronic pain: risks and benefits. Br J Clin Pharmacol 2013;77:357–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bell RF. Ketamine for chronic noncancer pain: concerns regarding toxicity. Curr Opin Support Palliat Care 2012;6:183–7. [DOI] [PubMed] [Google Scholar]
- 9.Persson K. Ketamine in pain management. CNS Neurosci Ther 2013;19: 396–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzgibbon EJ, Hall P, Schroder C et al. Low dose ketamine as an analgesic adjuvant in difficult pain syndromes: a strategy for conversion from parenteral to oral ketamine. J Pain Symptom Manage 2002;23: 165–70. [DOI] [PubMed] [Google Scholar]
- 11.Enarson MC, Hays H, Woodroffe MA. Clinical experience with oral ketamine. J Pain Symptom Manage 1999;17:384–6. [DOI] [PubMed] [Google Scholar]
- 12.Cvrcek P. Side effects of ketamine in the long-term treatment of neuropathic pain. Pain Med 2008;9:253–7. [DOI] [PubMed] [Google Scholar]