Abstract
Background
Several systematic reviews have been published about the relationship of the use of selective serotonin reuptake inhibitors (SSRIs) and risk of suicidal ideation or behavior but there has been no formal assessment of the quality of these reports.
Aim
Assess the methodological quality of systematic reviews about the relationship of SSRI use and suicidal ideation and behavior; and provide overall conclusions based on this assessment.
Methods
Systematic reviews of RCTs that compared SSRIs to placebo and used suicidal ideation or behavior as a key outcome variable were identified by searching Pubmed, Embase, The Cochrane Library, EBSCO, PsycINFO, Chinese National Knowledge Infrastructure, Chongqing VIP database for Chinese Technical Periodicals, WANFANG DATA, and the Chinese Biological Medical Literature Database. The methodological quality of included reviews was independently assessed by two expert raters using the 11-item Assessment of Multiple Systematic Reviews (AMSTAR) scale.
Results
Twelve systematic reviews and meta-analyses were identified. The inter-rater reliability of the overall AMSTAR quality score was excellent (ICC=0.86) but the inter-rater reliability of 5 of the 11 AMSTAR items was poor (Kappa <0.60). Based on the AMSTAR total score, there was one high-quality review, eight moderate-quality reviews, and three low-quality reviews. The high-quality review and three of the moderate-quality reviews reported a significantly increased risk of suicidal ideation or behavior in the SSRI group compared to the placebo group. Three of the four reviews limited to children and adolescents found a significantly increased risk of suicidal ideation or behavior with SSRI use which was most evident in teenagers taking paroxetine and in teenagers with depressive disorders.
Conclusions
The available evidence suggests that adolescents may experience an increase in suicidal ideation and behavior with SSRI use, particularly those who have a depressive disorder and those treated with paroxetine. However, there are few high-quality reviews on this issue, so some doubt about the evidence remains. The AMSTAR scale may be useful in the ongoing efforts to improve the quality of systematic reviews, but further work is needed on tightening the operational criteria for some of the items in the scale.
Keywords: systematic reviews, methodological quality, AMSTAR, selective serotonin reuptake inhibitors, suicidal ideation, suicidal behavior
Abstract
背景
关于使用选择性5- 羟色胺再摄取抑制剂(SSRIs) 与自杀意念或行为的关系,一些系统综述已发表,但 是对这些报告的质量并没有做过正式的评估。
目的
评估有关使用SSRI 与自杀意念和行为之间关系 的系统综述的方法学质量; 并提供在此评估的基础上 得出的总体结论。
方法
通过检索Pubmed, Embase,Cochrane 图书馆, EBSCO,PsycINFO,中国国家知网,中国科技期刊重庆 维普数据库,万方数据库,和中国生物医学文献数据 库来确定相关的系统综述,这些系统综述纳入了比较 SSRI 类药物与安慰剂、以自杀意念或行为作为关键变 量的随机对照试验。两个专家评估者独自采用多系统 综述11 项评估量表(AMSTAR)对纳入评估的文献进 行方法学质量的评估。
结果
共检出12 篇系统综述和meta 分析。AMSTAR 总体质量评分的评分者信度非常好(ICC=0.86),但 11 个AMSTAR 项目中有5 项的评分者信度较差(Kappa 值<0.60)。根据AMSTAR 总分,仅1 篇为高质量等级, 8 篇为中等质量等级,3 篇为低质量等级。这篇高质 量综述和3 篇中等质量的综述均报告SSRI 组中自杀意 念或行为的风险显著高于安慰剂组。4 篇仅限于儿童 和青少年的综述中有3 篇报道服用帕罗西汀和患有抑 郁症的青少年有显著增加自杀意念或行为的风险。
结论
现有证据表明,青少年使用SSRI 类药物可能会 增加自杀意念和行为的风险,尤其是抑郁症患者和服 用帕罗西汀的患者。但是,相关高质量的综述很少, 所以对这一结论还存有疑问。AMSTAR 量表对于提高 系统综述质量也许是有用的,但对量表中的某些项目 需要严格操作标准。
1. Introduction
Since their invention in the 1980’s,selective serotonin reuptake inhibitors (SSRIs) have been widely used to treat depressive disorders and anxiety disorders.[1] Common side effects include nausea,constipation,headache, anxiety, insomnia, and sweating.[2], [3], [4] Although increased suicidality (usually defined as suicidal ideation or suicidal behavior) has also been reported,[5], [6] the findings have been inconsistent. The first systematic review on the issue in 1991 did not find increased suicidality when comparing individuals treated with SSRIs to those treated with placebos,[7] but another systematic review did find that the use of SSRIs was associated with increased suicidality.[8] In 2004,the United States Food and Drug Administration (FDA) conducted a metaanalysis of 24 randomized controlled trials (RCT) among children and found a two-fold risk of suicidality when comparing individuals in the SSRI group with those in the placebo group.[9] Soon after,the FDA required a black-box warning on the packaging of all SSRI medications to warn of the possibility of exacerbation of depressive symptoms and increase in suicide risk among children,and to call for close monitoring of suicidality in children prescribed SSRIs.[10] In 2005 Gunnell and colleagues conducted a meta-analysis of RCTs submitted by pharmaceutical companies to the United Kingdom Medicines and Healthcare products Regulatory Agency (MHRA) and reported a possible increase of self-harm in adults administered SSRIs (OR=1.57, 95% CI=0.99-2.55), but did not find any increase in suicide risk (OR=0.85, 95% CI=0.20-3.40).[11] In 2006 the United States FDA conducted an analysis using data from 372 RCTs among adults and did not find increased suicide risk associated with SSRIs,but did find evidence of increased suicide risk among the subgroup of young adults 18 to 24 years of age.[12]
In summary,given the varying methodologies employed in the existing systematic reviews and meta-analyses, it is not yet possible to be certain about the relationship of SSRI use and suicide risk. The purpose of systematic reviews and meta-analyses is to provide the best evidence for clinical practice. The value of the summary of the evidence provided in systematic reviews depends on the methodological quality of the reviews,[13] but there has,as yet,been no formal assessment of the quality of the available systematic reviews and meta-analyses about the relationship of SSRIs and suicidality. The current study seeks to evaluate the quality of previous systematic reviews on this topic using the Assessment of Multiple Systematic Reviews scale (AMSTAR).[14]
2. Methods
2.1. Search strategies
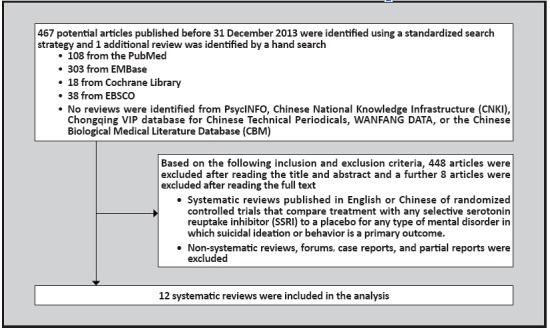
The identification of reviews included in this analysis is shown in Figure 1. Pubmed, Embase, The Cochrane Library, EBSCO, PsycINFO, Chinese National Knowledge Infrastructure,Chongqing VIP database for Chinese Technical Periodicals, WANFANG DATA,and the Chinese Biological Medical Literature Database (CBM) were searched for articles published by December 31,2013 using the following keywords: ‘SSRI’, ‘SSRIs’, ‘antidepressant’, ‘placebo’, ‘suicide’, ‘suicidal’,‘meta-analysis’, ‘systematic review’, ‘citalopram’, ‘escitalopram’, ‘fluoxetine’, ‘fluvoxamine’, ‘paroxetine’, ‘sertraline’. Reference lists of all included studies were hand checked for potential studies.
Figure 1. Identification of included reviews.
2.2. Inclusion and exclusion criteria
All systematic reviews or meta-analyses of RCTs on the effect of SSRIs on the risk of suicide were included if: (a) the main outcome is suicidal ideation and/or suicidal behavior; (b) the control groups included a placebo control; and (c) the sample sizes and the numbers of outcome events were reported. Only articles published in English or Chinese were considered. Based on the recommendations of the ‘Cochrane Handbook for Systematic Reviews of Interventions’,[13] studies that were not about the incidence of adverse effects were excluded. Anthropological studies, non-systematic reviews, research protocols, case reports, and duplicated reports were also excluded.
2.3. Screening of studies
Literature management software (Endnote X5) was used to eliminate duplicated reports. Two of the authors (LW and WY) independently screened all titles and abstracts of studies and read the full-text of remaining studies. Studies were selected based on the aforementioned inclusion and exclusion criteria. The two authors discussed any disagreement about the inclusion of an article and a third author (RJ) was consulted when the two authors did not arrive at a consensus decision.
2.4. Quality evaluation
The Assessment of Multiple Systematic Reviews (AMSTAR) scale[14] was used to assess the methodological quality of the included reviews and meta-analyses. AMSTAR is an 11-item scale (shown in Table 2) developed in 2007 with good inter-rater reliability, face validity, and content validity that has been widely employed for measuring the methodological quality of systematic reviews. Two authors (LW and WY) independently evaluated the quality of included studies based on the AMSTAR scale,[14] rating each of the 11 items on a binary scale (i.e., ‘yes’, ‘no’ or ‘not specified’). Disagreements in the ratings between the two raters were discussed and, if a consensus decision was not reached, a third author (LT) was called into make a final determination. The range of the overall quality score for each review was between 0 and 11.[15], [16] Based on the recommendations of the Canadian Agency for Drugs and Technologies in Health (CADTH),[27] the total score was used to classify the overall quality of each review as high (total score 9 to 11), moderate (score 5 to 8), or low (score 0 to 4).
2.5. Quality evaluation
Two authors (LW and LT) independently extracted relevant information to an Excel (Microsoft Excel 2007) sheet including the name of the authors, year of publication, number of included studies, combined sample size, number of outcome events, age of participants, type of medications, and diagnoses of participants. After independently coding the papers the two authors compared coding sheets and made a consensus decision about the few items that they had coded differently.
2.6. Data analysis
Quality ratings and other information were imported to SPSS 17.0 software for data analysis. Intra-class correlation coefficient (ICC) and Kappa statistics were used to evaluate the agreement of the original quality rating items.[17] Odds ratios (OR) were used to present the difference between groups of participants using SSRIs and groups using placebo. Stratified analyses were conducted based on variables related to the risk of suicide including age, type of medications, and diagnosis.
3. Results
3.1. Study characteristics
As show in Figure 1 the search identified a total of 468 publications, all of which were in English-language journals. Review of the titles and abstracts found that 35 were duplicated reports, 8 were unrelated to the topic of interest,and a further 413 did not meet the inclusion criteria. This left 12 review articles that were included in the subsequent analyses.[7], [8],[11],[18],[19],[20],[21],[22],[23],[24],[25],[26]
shown in Table 1. All 12 articles were published in English from 1991 to 2011; 8 of them were published between 2005 and 2007.[8],[11],[18],[19],[20],[21],[24],[25] Among the 12 reviews,one third were among children and adolescents 19 years of age or younger;[18],[20],[24],[25] one third were among adults;[11],[19],[21],[22] and the remaining one-third did not specify the age range of participants.[7],[8],[23],[26] One review[8] did not specify the specific SSRI assessed; all others indicated the specific medication(s) that were compared to placebos; these included fluoxetine, paroxetine, sertraline, fluvoxamine, citalopram, and escitalopram. Nine of the 12 reviews[7],[8],[18],[19],[20],[21],[22],[24],[25] provided a description of the diagnoses of participants; most of the reviews considered the use of SSRIs in patients with depressive disorders or different types of anxiety disorders.
Table 1.
Characteristics of included reviews
| study | trials/ participants |
age range |
SSRIs compared to placebo |
diagnoses considered |
outcome measures |
|---|---|---|---|---|---|
| Beasley 1991[7] |
17/ 2334 |
12-90 | fluoxetine | depression | suicidal acts suicidal ideation |
| Khan 2000[26] |
14/ 6356 |
general population |
paroxetine; sertraline | not specified | suicide suicide attempt |
| Fergusson 2005[8] |
189/ 18,413 |
general population |
not specified | depression | suicide suicide attempt |
| Gunnell 2005[11] |
477/ 40,826 |
adults | fluoxetine; paroxetine; sertraline; fluvoxamine; citalopram; escitalopram |
not specified | suicide self-harm suicidal thoughts |
| Dubicka 2006[24] |
unknown/ 2122 |
6-18 | fluoxetine; paroxetine; sertraline; citalopram |
MDD | suicide attempt self-harm preparatory acts suicidal thought |
| Hammad 2006[25] |
16/ 2970 |
pediatric patients |
fluoxetine; paroxetine; sertraline; fluvoxamine; citalopram |
MDD,OCD,SAD | suicidality |
| Apter 2006[20] |
5/ 1191 |
<18 | paroxetine | MDD,OCD,AD | suicidality |
| Bridge 2007[18] |
27/ 3543 |
<19 | fluoxetine; paroxetine; sertraline; fluvoxamine; and escitalopram or citaloprama |
MDD,OCD,AD | suicide attempt preparatory act suicidal ideation |
| Tauscher- Wisniewski 2007[19] |
53/ 11,448 |
18-65 | fluoxetine | Bulimia,OCD | suicidal behaviors suicidal ideation |
| Beasley 2007[21] |
18/ 3751 |
>18 | fluoxetine | MDD | suicidal behaviors suicidal ideation |
| Stone 2009[23] |
372/ 52,665 |
15-99 | fluoxetine; paroxetine; sertraline; fluvoxamine; citalopram; escitalopram |
not specified | suicidality |
| Carpenter 2011[22] |
61/ 14,911 |
18-64 | paroxetine | depression, OCD,AD,PTSD |
suicidal behaviors suicidal ideation |
SSRI,selective serotonin reuptake inhibitor MDD,major depressive disorder
OCD,obsessive-compulsive disorder AD,anxiety disorder
SAD,social anxiety disorder (subtype of anxiety disorder) PTSD,posttraumatic stress disorder
a in this study results for escitalopram and citalopram were analyzed together,not separately
3.2. Results of quality evaluation
As shown in Table 2, the ICC of the total AMSTAR scores for the 12 reviews between the two evaluating authors was 0.86, which indicates excellent inter-rater reliability in the overall quality assessment. However, 5 of the 11 individual items (items 1, 4, 7, 8, and 9) had Kappa values below 0.60 (the conventional level of ‘fair’ agreement[17]) and 2 items (items 9 and 4) had Kappa values below 0.40,indicating unacceptable agreement. Subsequent analysis of the items with poor inter-rater reliability identified two main causes: (a) the simple description of some of the items were interpreted differently by the two coders; (b) some articles had supplementary webbased materials that was accessed by one of the raters but not by the other rater.
The consensus assessments of the two coders of the 11 items shown in Table 2 indicate a surprising range in the quality of these 12 systematic reviews. Only 1 of the 12 reviews assessed the likelihood of publication bias,[18] only 2 provided a list of studies,[22],[25] only 3 assessed the scientific quality of the included studies,[18],[24],[25] and only 4 performed a comprehensive literature search.[7],[8],[18],[24] On the other hand,11 of the 12 reviews described the characteristics of the included studies,[7],[8],[11],[18],[20],[21],[22],[23],[24],[25],[26] 11 reviews appropriately combined the findings of the included studies,[7],[8],[11],[18], [19],[20],[22],[23],[24],[25],[26] and 10 reviews appropriately considered the scientific quality of included studies when formulating the final conclusions.[7],[8],[11],[18],[20],[21],[23],[24],[25],[26]
Table 2.
Assessment of Multiple Systematic Reviews (AMSTAR) scale ratings of the 12 included systematic reviews
| AMSTAR criteria | Beasley 1991[7] |
Khan 2000[26] |
Fergusson 2005[8] |
Gunnell 2005[11] |
Dubicka 2006[24] |
Hammad 2006[25] |
Apter 2006[20] |
Bridge 2007[18] |
Tauscher- Wisniewski 2007[19] |
Beasley 2007[21] |
Stone 2009[23] |
Carpenter 2011[22] |
proportion with item present |
kappaa |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was an ‘a priori’ design provided? | Yes | No | Yes | No | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 8/12 | 0.47 |
|
2. Was there duplicate study selection and data extraction? |
Yes | No | Yes | No | No | Yes | Yes | No | No | Yes | Yes | Yes | 7/12 | 0.68 |
|
3. Was a comprehensive literature search performed? |
Yes | No | Yes | No | Yes | No | No | Yes | No | No | No | No | 4/12 | 0.63 |
|
4. Was the status of publication used as an inclusion criterion? |
Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | 8/12 | 0.33 |
| 5. Was a list of studies provided? | No | No | No | No | No | Yes | No | No | No | No | No | Yes | 2/12 | 0.75 |
|
6. Were the characteristics of the included studies provided? |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | 11/12 | 0.63 |
|
7. Was the scientific quality of the included studies assessed and documented? |
No | No | No | No | Yes | Yes | No | Yes | No | No | No | No | 3/12 | 0.47 |
|
8. Was the scientific quality of the included studies used appropriately in formulating conclusions? |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | 10/12 | 0.56 |
|
9. Were the methods used to combine the findings of studies appropriate? |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | 11/12 | 0.25 |
|
10. Was the likelihood of publication bias assessed? |
No | No | No | No | No | No | No | Yes | No | No | No | No | 1/12 | 0.63 |
| 11. Was the conflict of interest stated? | No | No | Yes | Yes | Yes | No | No | Yes | No | No | Yes | Yes | 6/12 | 0.67 |
| Total score (out of 11) | 7 | 3 | 7 | 5 | 8 | 7 | 6 | 9 | 2 | 3 | 7 | 7 | --- | 0.86b |
|
Overall methodological quality (L=low,M=moderate,H=high) |
M | L | M | M | M | M | M | H | L | L | M | M | --- | --- |
a Kappa values for inter-rater reliability of the two independent coders who assessed each of the 11 items for the 12 reviews
b Intraclass correlation coefficient (ICC) assessing the inter-rater reliability of the two independent raters of the total quality score for the 12 reviews
The range in the total AMSTAR score for the 12 reviews was 2 to 9 (theoretical range 0 to 11) and the mean (sd) was 5.92 (2.19). Based on CADTH criteria[27] for categorization of the AMSTAR total score,one study was considered high quality,[18] eight were considered moderate quality,[7],[8],[11],[20],[22],[23],[24],[25] and three were considered poor quality.[19],[21],[26]
3.3. Summary of the results of meta-analyses
The summary of results is shown in Table 3. The high quality review reported a statistically significant higher risk of suicidal ideation or behavior when comparing the SSRI group with the placebo group (pooled OR=1.81, 95%CI=1.13-2.89).[18] Three of the eight moderate quality reviews[8], [20], [25] reported increased risk of suicidal ideation or behavior in the SSRI group compared to the placebo group (pooled OR=2.24 [95%CI=1.05-4.76],[8] 3.86 [95%CI=1.45-10.26],[20] and 1.89 [95%CI=1.16- 3.06][25]). None of the three low-quality reviews[19], [21], [26] reported differences in the risk of suicidal ideation or behavior between the SSRI and placebo groups.
3.3.1. Results stratified by age
One high-quality review[18] and three moderate-quality reviews[18],[20],[25] were focused on SSRI use among children and adolescents; the high-quality review[18] and two of the three moderate-quality reviews[20],[25] reported increased risk of suicidal ideation or behavior in the SSRI group compared to the placebo group. There were two moderate-quality reviews[11],[22] and two low-quality reviews[19],[21] focused on SSRI use in adults; none of them found an increased risk of suicidal ideation or behavior associated with SSRI use.
3.3.2. Results stratified by type of medication
As shown in Table 1,one of the 12 systematic reviews did not specify which SSRI was used,[8] five of the reviews only considered a single SSRI,[7], [19], [20], [21], [22] and the remaining six reviews compared two or more SSRIs to placebo.[11], [18], [23], [24], [25], [26] Six different SSRIs are considered in the reviews: paroxetine is considered in 8 reviews, fluoxetine in 7 reviews, sertraline in 6 reviews, fluvoxamine in 4 reviews, citalopram in 4 reviews, escitalopram in 2 reviews, and citalopram or escitalopram (not separately analyzed) in one review. As shown in Table 3,only two of the SSRIs were associated with elevated risk of suicidal ideation or behavior. One high-quality review[18] and 2 moderate-quality reviews[20], [25] among teenagers using paroxetine reported significantly elevated risk of suicidal ideation or behavior compared to placebo. And one moderate-quality review in adults using fluvoxamine[11] also found elevated risk of suicidal ideation or behavior. None of the other SSRIs considered in the reviews were associated with suicidal ideation or behavior.
3.3.3. Results stratified by diagnoses
As shown in Table 1, three of the included systematic reviews did not specify the diagnosis of the participants;[11],[23],[26] three reviews were restricted to individuals with depressive disorders,[7],[21],[24] and the remaining six reviews considered individuals with a variety of diagnoses.[8],[18],[19],[20],[22],[25] Eight reviews included individuals with depression, five included individuals with obsessive compulsive disorder, four included individuals with anxiety disorders or social anxiety disorder, one included individuals with post-traumatic stress disorder, and one considered individuals with bulimia. As shown in Table 3, only one diagnosis was associated in elevated risk of suicidal ideation or behavior when treated with SSRIs: two of the three moderate-quality systematic reviews of depressed teenagers found that use of SSRIs was significantly associated with increased suicidal ideation or behavior. This effect was not seen in the single high-quality review of depressed teenagers (though there was a trend that suggested an association), in reviews of depressed adults, or in the reviews of any of the other diagnoses considered.
4. Discussion
4.1. Main findings
Over the last decade concern about the possible link between SSRI use and an increased risk of suicide stimulated several large-scale studies that have had a major influence on policies and clinical practice related to the treatment of depression. It is, therefore, concerning to find that only 1 of 12 systematic reviews on this topic - the most scientifically credible information available for making decisions about clinical care - are rated as ‘high-quality’. One is left with uncomfortable questions about the quality of other systematic reviews on topics that have received much less funding and attention but are, nevertheless,being used as justification for changing policies and clinical practice. Our study identified several areas where systematic reviews are lacking,including inadequate description of the search strategy, failure to consider the scientific quality of the included studies, and no discussion of the possibility of publication bias[28], [29], [30], [31] - issues that can seriously compromise the validity of a review. Clearly, the authors of systematic reviews and the journals that publish systematic reviews need be much more rigorous in their evaluation of the methodological quality of the reviews.
How should the methodological quality of systematic reviews be evaluated? This is a relatively new area of concern that has only become a focus of methodological attention over the last decade, so the techniques for doing this are still evolving. The current study employed the Assessment of Multiple Systematic Reviews (AMSTAR) scale,[14],[32] the most promising instrument yet available. In our study we found that independent coders of published reports of systematic reviews could reliably assess the overall quality of the report using the 11-item scale (ICC=0.86). But the interrater reliability of several of the individual items in the scale was weak and it was unacceptable for two items which assess (a) the appropriateness of the method of combining findings across studies and (b) the use of publication status as an inclusion criteria. The difficulty of achieving agreement on these items indicates the need to tighten the operational definitions used to code the items, or the need to change the wording of the items to make them less ambiguous. Further work on the validity and utility of the assessment tool is also needed to determine the appropriateness of the current cutoff scores for ‘high’,‘moderate’, and ‘low’ methodological quality and to develop strategies for using the information obtained from this assessment of the quality of systematic reviews to inform policy and clinical decisions.
What can be concluded from this evaluation of the quality of systematic reviews on the relationship of SSRI use and suicidal ideation and behavior? Given that only one of the 12 systematic reviews considered was classified as ‘high-quality’ it is necessary to be somewhat cautious when interpreting the results. Nevertheless, it is reassuring that the high-quality review and 3 of the 8 moderate-quality reviews (but none of the 3 lowquality reviews) came to the same conclusion: SSRI use is associated with an elevated risk of suicidal ideation or behavior. Interpretation of the stratified analyses is difficult because of differences in the number of studies and in the number of participants in the studies in different age groups, using different types of SSRIs, and with different diagnoses. Nevertheless, the general picture is clear: the elevated risk of suicidal ideation and behavior associated with SSRIs is most evident in children and adolescents, particularly those with depressive disorders and those being treated with paroxetine. This conclusion supports the findings of the United States FDA report that highlighted the moderating influence of age and a diagnosis of depression on the relationship between SSRI use and the risk of suicidal ideation and behaviors.[9] Our findings are also consistent with those of the British drug regulatory agency which highlighted the risk of self-harm and suicidal behavior among children treated with paroxetine.[34]
4.2. Limitations
There are several potential limitations that need to be considered.
(a) The search strategy did not identify a single review about this important topic from China. All identified reports were in English from highincome countries so it is uncertain whether or not the results would hold true in low- and middle-income countries where the use of SSRIs,the help-seeking for depression and other mental disorders,and the demographic pattern of suicidal behavior may be quite different.
(b) The measure of quality employed in the study, the AMSTAR scale, is the best currently available measure, but the poor inter-rater reliability of some of the items indicates that further work is needed to improve the reliability and validity of the measure. Reviewers using these criteria need to decide a priori whether or not ancillary web-based materials of included articles will be considered when making the quality determination.
(c) The sample sizes available for several of the stratified analyses shown in Table 3 were relatively small, so there were several cases in which an odds ratio of over 2 was not statistically significant. These may be Type II errors. Larger samples in these specific cohorts would be needed to resolve the issue.
Table 3.
Overall and stratified results of 12 included systematic reviews
| study ID | age group | SSRI | placebo | odds ratio (95%CI) |
quality of reviewa |
|---|---|---|---|---|---|
| events / total | events / total | ||||
| OVERALL RESULTS | |||||
| Beasley 1991[7] | not specified | 30 / 1765 | 16 / 569 | 0.60 [0.32,1.10] | M |
| Khan 2000[26] | not specified | 56 / 5016 | 13 / 1340 | 1.15 [0.63,2.11] | L |
| Fergusson 2005[8] | not specified | 27 / 10,557 | 9 / 7856 | 2.24 [1.05,4.76]b | M |
| Gunnell 2005[11] | adults | 175 / 23,804 | 107 / 17,022 | 1.17 [0.92,1.49] | M |
| Dubicka 2006[24] | teenagers | 56 / 1135 | 36 / 987 | 1.37 [0.89,2.10] | M |
| Hammad 2006[25] | teenagers | 51 / 1554 | 25 / 1416 | 1.89 [1.16,3.06]b | M |
| Apter 2006[20] | teenagers | 22 / 642 | 5 / 549 | 3.86 [1.45,10.26]b | M |
| Bridge 2007[18] | teenagers | 52 / 1839 | 27 / 1704 | 1.81 [1.13,2.89]b | H |
| Tauscher-Wisniewski 2007[19] | adults | 41 / 7066 | 26 / 4382 | 0.98 [0.60,1.60] | L |
| Beasley 2007[21] | adults | 233 / 2200 | 197 / 1551 | 0.81 [0.67,1.00] | L |
| Stone 2009[23] | not specified | 205 / 31,440 | 141 / 21,225 | 0.98 [0.79,1.22] | M |
| Carpenter 2011[22] | adults | 83 / 8958 | 65 / 5953 | 0.85 [0.61,1.17] | M |
| RESULTS STRATIFIED BY TYPE OF SSRI | |||||
| Fluoxetine | |||||
| Beasley 1991[7] | not specified | 30 / 1765 | 16 / 569 | 0.60 [0.32,1.10] | M |
| Dubicka 2006[24] | teenagers | 18 / 358 | 12 / 321 | 1.36 [0.65,2.88] | M |
| Hammad 2006[25] | teenagers | 18 / 358 | 11 / 321 | 1.49 [0.69,3.21] | M |
| Bridge 2007[18] | teenagers | 18 / 410 | 11 / 372 | 1.51 [0.70,3.23] | H |
| Beasley 2007[21] | adults | 233 / 2200 | 197 / 1551 | 0.81 [0.66,1.00] | L |
| Tauscher-Wisniewski 2007[19] | adults | 41 / 7066 | 26 / 4382 | 0.98 [0.60,1.60] | L |
| Stone 2009[23] | not specified | 81 / 7180 | 67 / 4814 | 0.81 [0.58,1.12] | M |
| Paroxetine | |||||
| Khan 2000[26] | not specified | 45 / 2963 | 8 / 554 | 1.05 [0.49,2.25] | L |
| Gunnell 2005[11] | adults | 66 / 8481 | 55 / 5808 | 0.82 [0.57,1.18] | M |
| Dubicka 2006[24] | teenagers | 14 / 378 | 7 / 285 | 1.53 [0.61,3.84] | M |
| Hammad 2006[25] | teenagers | 16 / 641 | 4 / 548 | 3.48 [1.16,10.48]b | M |
| Apter 2006[20] | teenagers | 22 / 642 | 5 / 549 | 3.86 [1.45,10.26]b | M |
| Bridge 2007[18] | teenagers | 16 / 641 | 4 / 548 | 3.48 [1.16,10.48]b | H |
| Stone 2009[23] | not specified | 50 / 9919 | 29 / 6972 | 1.21 [0.77,1.92] | M |
| Carpenter 2011[22] | adults | 83 / 8958 | 65 / 5953 | 0.85 [0.61,1.17] | M |
| Sertraline | |||||
| Khan 2000[26] | not specified | 11 / 2053 | 5 / 786 | 0.84 [0.29,2.43] | L |
| Gunnell 2005[11] | adults | 30 / 7169 | 21 / 5108 | 1.02 [0.58,1.78] | M |
| Dubicka 2006[24] | teenagers | 5 / 189 | 2 / 184 | 2.47 [0.47,12.91] | M |
| Hammad 2006[25] | teenagers | 5 / 281 | 3 / 279 | 1.67 [0.39,7.04] | M |
| Bridge 2007[18] | teenagers | 5 / 320 | 3 / 318 | 1.67 [0.39,7.03] | H |
| Stone 2009[23] | not specified | 18 / 6363 | 18 / 6363 | 0.51 [0.28,0.93] | M |
| Fluvoxamine | |||||
| Gunnell 2005[11] | adults | 49 / 4186 | 24 / 3396 | 1.66 [1.02,2.72]b | M |
| Hammad 2006[25] | teenagers | 2 / 57 | 0 / 63 | 5.72 [0.27,121.72] | M |
| Bridge 2007[18] | teenagers | 2 / 120 | 0 / 128 | 5.42 [0.26,114.10] | H |
| Stone 2009[23] | not specified | 22 / 2187 | 13 / 1828 | 1.42 [0.71,2.82] | M |
| Citalopram | |||||
| Gunnell 2005[11] | adults | 22 / 1320 | 10 / 622 | 1.04 [0.49,2.20] | M |
| Dubicka 2006[24] | teenagers | 19 / 210 | 15 / 197 | 1.21 [0.60,2.45] | M |
| Hammad 2006[25] | teenagers | 10 / 217 | 7 / 205 | 1.37 [0.51,3.66] | M |
| Stone 2009[23] | not specified | 24 / 2661 | 7 / 1371 | 1.77 [0.76,4.13] | M |
| Escitalopram | |||||
| Gunnell 2005[11] | adults | 8 / 2648 | 4 / 2088 | 1.58 [0.47,5.25] | M |
| Stone 2009[23] | not specified | 10 / 3130 | 5 / 2604 | 1.67 [0.57,4.88] | M |
| Escitalopram or Citalopramc | |||||
| Bridge 2007[18] | teenagers | 11 / 348 | 9 / 338 | 1.19 [0.49,2.92] | H |
| RESULTS STRATIFIED BY TYPE OF MENTAL DISORDER | |||||
| Depressive disorders | |||||
| Beasley 1991[7] | not specified | 30 / 1765 | 16 / 569 | 0.60 [0.32,1.10] | M |
| Fergusson 2005[8] | not specified | 17 / 5306 | 8 / 4370 | 1.75 [0.76,4.06] | M |
| Dubicka 2006[24] | teenagers | 56 / 1135 | 36 / 987 | 1.37 [0.89,2.10] | M |
| Hammad 2006[25] | teenagers | 44 / 1070 | 24 / 963 | 1.68 [1.01,2.78]b | M |
| Apter 2006[20] | teenagers | 18 / 378 | 5 / 285 | 2.80 [1.03,7.63]b | M |
| Bridge 2007[18] | teenagers | 45 / 1201 | 26 / 1096 | 1.60 [0.98,2.61] | H |
| Beasley 2007[21] | adults | 233 / 2200 | 197 / 1551 | 0.81 [0.67,1.00] | L |
| Carpenter 2011[22] | adults | 66 / 3720 | 47 / 2260 | 0.85 [0.58,1.24] | M |
| Obsessive-compulsive disorder | |||||
| Hammad 2006[25] | teenagers | 4 / 319 | 1 / 297 | 3.76 [0.42,33.82] | M |
| Apter 2006[20] | teenagers | 1 / 99 | 0 / 107 | 3.27 [0.13,81.31] | M |
| Bridge 2007[18] | teenagers | 4 / 362 | 1 / 339 | 3.78 [0.42,33.96] | H |
| Tauscher-Wisniewski 2007[19] | adults | 5 / 421 | 3 / 144 | 0.56 [0.13,2.39] | L |
| Carpenter 2011[22] | adults | 5 / 698 | 4 / 416 | 0.74 [0.20,2.78] | M |
| Anxiety disorder | |||||
| Hammad 2006[25] | teenagers | 3 / 165 | 0 / 156 | 6.74 [0.35,131.58] | M |
| Apter 2006[20] | teenagers | 3 / 165 | 0 / 157 | 6.78 [0.35,132.41] | M |
| Bridge 2007[18] | teenagers | 3 / 276 | 0 / 269 | 6.90 [0.35,134.17] | H |
| Carpenter 2011[22] | adults | 8 / 2939 | 8 / 2243 | 0.76 [0.29,2.03] | M |
| Post-traumatic stress disorder | |||||
| Carpenter 2011[22] | adults | 3 / 698 | 6 / 510 | 0.36 [0.09,1.46] | M |
| Bulimia | |||||
| Tauscher-Wisniewski 2007[19] | adults | 18 / 722 | 8 / 410 | 1.28 [0.55,2.98] | L |
SSRI,selective serotonin reuptake inhibitor; CI,confidence interval
a methodological quality categorized as high (H),moderate (M), or low (L)
b statistically significant difference in number of suicidal events between SSRI and placebo
c in this study results for escitalopram and citalopram were analyzed together, not separately
(d) Different studies considered in the reviews used different methods of assessing the outcome measure. Most studies used the United States FDA definition of suicide-related events[35] to measure suicide, suicidal ideation,and suicidal behaviors, while a minority of studies[20], [21] use the single suicide-related item from the Hamilton Depression Scale (HAMD)[36] which asks about suicidal ideation.
(e) Suicidal ideation has a weak association with suicidal behavior - particularly in youth—while prior suicide attempt is, by far, the strongest predictor of subsequent death by suicide. Thus, these are two distinct types of events, but most studies considered in the included reviews combine these two phenomena as the target outcome, primarily because the low rate of suicide attempt makes it difficult to achieve statistical power. Collapsing these two types of events in the analysis weakens the clinical utility of the results.
(f) It was not possible to stratify results by several other potentially important variables including the time in the course of treatment (suicide risk may be greatest during the early stages of treatment[11]),and the dose of the SSRI.
4.3. Implications
We found a surprisingly wide range in the methodological quality of systematic reviews about the relationship of SSRI use and risk of suicidal ideation and behavior. This highlights the importance of routinely assessing the quality of systematic reviews - assumed to provide ‘gold standard’ information - and of working to improve the quality of systematic reviews about this issue and about other issues of policy or clinical importance. After consideration of the quality of the available systematic reviews,our overall findings are in line with the recommendations of the United States and British drug regulatory agencies: the use of SSRIs is associated with an increase in suicidal ideation or behavior,but this increased risk is primarily limited to children and adolescents,particularly those who have depression and those who are treated with paroxetine.
Biography

Wei Li graduated with a Bachelor degree of Medicine from Hebei Medical University in 2012. He is currently a Master’s student in Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine. His main research interests include basic and clinical aspects of generalized anxiety disorder and other anxiety disorders, and the conduct of systematic reviews.
Funding Statement
The study was supported by the National Science Foundation (grant number: 30970901) and the East China Normal University MRI key laboratory.
Acknowledgement: The authors thank professor Michael Phillips for providing valuable suggestions for the revision of this manuscript.
Conflict of interest: Authors declare no conflict of interest related to this article.
References
- 1.Stafford RS, MacDonald EA, Finkelstein SN, et al. Nationalpatterns of medication treatment for depression, 1987 to 2001. Prim Care Companion J Clin Psychiatry. 2001;3(6):232–235. doi: 10.4088/pcc.v03n0611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cipriani A, La Ferla T, Furukawa TA, Signoretti A, Nakagawa A, Churchill R, et al. Sertraline versus other antidepressiveagents for depression. Cochrane Database Syst Rev. 2010;4 doi: 10.1002/14651858.CD006117.pub4. CD006117. [DOI] [Google Scholar]
- 3.Omori IM, Watanabe N, Nakagawa A, Cipriani A, Barbui C, McGuire H, et al. Fluvoxamine versus other anti-depressiveagents for depression. Cochrane Database Syst Rev. 2010;3 doi: 10.1002/14651858.CD006114.pub2. CD006114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shen YC. [Psychiatry] Beijing: People’s Health Publishing House; 2009. pp. 880–907. Chinese. [Google Scholar]
- 5.Masand P, Gupta S, Dewan M. Suicidal ideation related tofluoxetine treatment. N Engl J Med. 1991;324(6):420. doi: 10.1056/nejm199102073240616. [DOI] [PubMed] [Google Scholar]
- 6.Teicher MH, Glod C, Cole JO. Emergence of intense suicidalpreoccupation during fluoxetine treatment. Am J Psychiatry. 1990;147(2):207–210. doi: 10.1176/ajp.147.2.207. [DOI] [PubMed] [Google Scholar]
- 7.Beasley CM Jr, Dornseif BE, Bosomworth JC, Sayler ME, Rampey AH Jr, Heiligenstein JH, et al. Fluoxetine andsuicide: a meta-analysis of controlled trials of treatment fordepression. BMJ. 1991;303(6804):685–692. doi: 10.1136/bmj.303.6804.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fergusson D, Doucette S, Glass KC, Shapiro S, Healy D, Hebert P, et al. Association between suicide attempts andselective serotonin reuptake inhibitors: systematic reviewof randomised controlled trials. BMJ. 2005;330(7488):396. doi: 10.1136/bmj.330.7488.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Food and Drug Administration(FDA) [Internet] [cited 25 February 2014];Relationship between psychotropic drugs and pediatric suicidality: review and evaluation of clinical data. 2014 Available from: http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-10-TAB08-Hammads-Review.pdf .
- 10.U.S. Food and Drug Administration(FDA) [Internet] [cited 20 February 2014];FDA Statement on Recommendations of the Psychopharmacologic Drugs and Pediatric AdvisoryCommittees. 2014 Available from: http://www.fda.gov/newsevents/newsroom/pressannouncements/2004/ucm108352.htm .
- 11.Gunnell D, Saperia J, Ashby D. Selective serotonin reuptakeinhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA’s safety review. BMJ. 2005;330(7488):385. doi: 10.1136/bmj.330.7488.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laughren TP. [cited 20 March 2014];Briefing document for 13 December meeting of Psychopharmacologic Drugs Advisory Committee. 2014 Available from: http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4272b1-index.htm .
- 13.JPT CHH, Green S. Cochrane Handbook for SystematicReviews of Interventions version 5.1.0 [updated March 2011] The Cochrane Collaboration; 2011. [Google Scholar]
- 14.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shea BJ, Bouter LM, Peterson J, Boers M, Andersson N, Ortiz Z, et al. External validation of a measurement toolto assess systematic reviews (AMSTAR) PLoS One. 2007;2(12):e1350. doi: 10.1371/journal.pone.0001350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sequeira-Byron P, Fedorowicz Z, Jagannath VA, Sharif MO. An AMSTAR assessment of the methodological qualityof systematic reviews of oral healthcare interventions. J Appl Oral Sci. 2011;19(5):440–447. doi: 10.1590/S1678-77572011000500002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li CB, He YL, Zhang MY. [Reasonable application of the consistency test methods] Shanghai Arch Psychiatry. 2000;12(4):228–230. Chinese. [Google Scholar]
- 18.Bridge JA, Iyengar S, Salary CB, Barbe RP, Birmaher B, Pincus HA, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683–1696. doi: 10.1001/jama.297.15.1683. [DOI] [PubMed] [Google Scholar]
- 19.Tauscher-Wisniewski S, Disch D, Plewes J, Ball S, Beasley CM. Evaluating suicide-related adverse events in clinicaltrials of fluoxetine treatment in adults for indicationsother than major depressive disorder. Psychol Med. 2007;37(11):1585–1593. doi: 10.1017/S0033291707001146. [DOI] [PubMed] [Google Scholar]
- 20.Apter A, Lipschitz A, Fong R, Carpenter DJ, Krulewicz S, Davies JT, et al. Evaluation of suicidal thoughts andbehaviors in children and adolescents taking paroxetine. J Child Adolesc Psychopharmacol. 2006;16(1-2):77–90. doi: 10.1089/cap.2006.16.77. [DOI] [PubMed] [Google Scholar]
- 21.Beasley CM.Jr, Ball SG, Nilsson ME, Polzer J, Tauscher-Wisniewski S, Plewes J, et al. Fluoxetine and adult suicidality revisited: an updated meta-analysis using expanded data sources from placebo-controlled trials. J Clin Psychopharmacol. 2007;27(6):682–686. doi: 10.1097/jcp.0b013e31815abf21. [DOI] [PubMed] [Google Scholar]
- 22.Carpenter DJ, Fong R, Kraus JE, Davies JT, Moore C, Thase ME. Meta-analysis of efficacy and treatment-emergent suicidality in adults by psychiatric indication and age subgroup following initiation of paroxetine therapy: a complete set of randomized placebo-controlled trials. J Clin Psychiatry. 2011;72(11):1503–1514. doi: 10.4088/JCP.08m04927blu. [DOI] [PubMed] [Google Scholar]
- 23.Stone M, Laughren T, Jones ML, Levenson M, Holland PC, Hughes A, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;339:b2880. doi: 10.1136/bmj.b2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dubicka B, Hadley S, Roberts C. Suicidal behaviour in youths with depression treated with new-generationantidepressants: meta-analysis. Br J Psychiatry. 2006;189:393–398. doi: 10.1192/bjp.bp.105.011833. [DOI] [PubMed] [Google Scholar]
- 25.Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63(3):332–339. doi: 10.1001/archpsyc.63.3.332. [DOI] [PubMed] [Google Scholar]
- 26.Khan A, Warner HA, Brown WA. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: an analysis of the Food and Drug Administration database. Arch Gen Psychiatry. 2000;57(4):311–317. doi: 10.1001/archpsyc.57.4.311. [DOI] [PubMed] [Google Scholar]
- 27.Interventions Directed to Consumers. [cited 20 February 2014];Canadian Agency for Drugs and Technologies in Health (CADTH) 2014 Available from: http://www.cadth.ca/en/resources/rx-for-change/interventions-consumers .
- 28.Egger M, Davey Smith G, Schneider M, Minder C. Bias inmeta-analysis detected by a simple graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dickersin K. The existence of publication bias and risk factorsfor its occurrence. JAMA. 1990;263(10):1385–1389. doi: 10.1001/jama.1990.03440100097014. [DOI] [PubMed] [Google Scholar]
- 30.Stern JM, Simes RJ. Publication bias: evidence of delayedpublication in a cohort study of clinical research projects. BMJ. 1997;315(7109):640–645. doi: 10.1136/bmj.315.7109.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–1129. doi: 10.1016/S0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- 32.Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62(10):1013–1020. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 33.Soutullo C, Figueroa-Quintana A. When do you prescribe antidepressants to depressed children? Curr Psychiatry Rep. 2013;15(7):366. doi: 10.1007/s11920-013-0366-3. [DOI] [PubMed] [Google Scholar]
- 34.U.K. Department of Health Advisory. [cited 15 February 2014];Questions and Answers Seroxat (Paroxetine) 2014 Available from: http://www.mhra.gov.uk/home/groups/pl-p/documents/websiteresources/con2023718.pdf .
- 35.U.S. Food and Drug Administration(FDA) [cited 22 February 2014];FDASuicidality Classification Project. 2014 Available from: www.fda.gov/ohrms/dockets/ac/04/slides/2004-4065S1_06_FDA-Posner.ppt .
- 36.Hamilton M, Figueroa-Quintana A. Development of a rating scale for primarydepressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]


