Abstract
Background
Studies from Western countries consistently report very high rates of comorbid Antisocial Personality Disorder (ASPD) among individuals with heroin addiction, but the reported proportion of Chinese individuals with heroin addiction who have co-morbid ASPD varies widely, possibly because Chinese clinicians do not consider personality issues when treating substance abuse problems.
Aim
Conduct a meta-analysis of studies that assessed the proportion of Chinese individuals with heroin dependence who have comorbid ASPD.
Methods
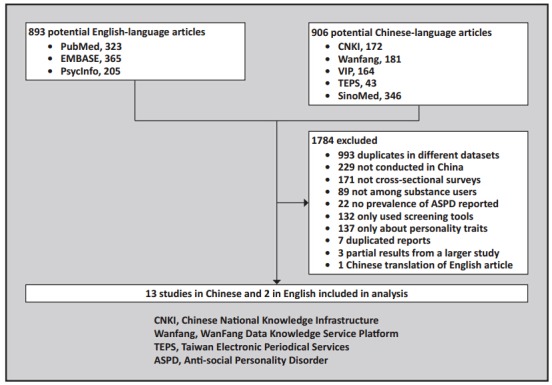
We searched for relevant studies in both Chinese databases (China National Knowledge Infrastructure, Wanfang Data Knowledge Service Platform, Taiwan Electronic Periodical Services) and western databases (PubMed, EMBASE, and PsycInfo). Two authors independently retrieved the literature, identified studies that met pre-defined inclusion and exclusion criteria, assessed the quality of included studies, and extracted the data used in the analysis. Statistical analysis was performed using StatsDirect 3.0 and R software.
Results
The search yielded 15 eligible studies with a total of 3692 individuals with heroin dependence. Only 2 of the studies were rated as high-quality studies. All studies were conducted in rehabilitation centers or hospitals. The pooled lifetime prevalence of ASPD in these subjects was 30% (95%CI: 23%-38%), but the heterogeneity of results across studies was great (I2 =95%, p<0.001). Men had a higher prevalence than women (44% vs. 21%), and injection heroin users had higher prevalence than those who smoked heroin (44% vs. 27%). Studies that were methodologically stronger had higher reported prevalence of ASPD among heroin dependent individuals.
Conclusions
There are substantial methodological problems in the available literature about ASPD in Chinese individuals receiving treatment for heroin dependence, but we estimate that about one-third of them meet criteria for ASPD. Further work is needed to increase clinicians’ awareness of this issue; to compare the pathogenesis, treatment responsiveness and recidivism of those with and without ASPD; and to develop and test targeted interventions for this difficult-to-treat subgroup of individuals with heroin dependence.
Keywords: Antisocial personality disorder, Heroin dependence, prevalence, meta-analysis, China
Abstract
背景
西方国家的研究持续报道海洛因成瘾者共患反 社会人格障碍(Antisocial Personality Disorder,ASPD) 的比率很高,但中国海洛因成瘾者共患ASPD的报道比 率变异很大,可能是因为中国的临床医生在治疗物质 滥用问题时没有考虑人格问题。这份报告对评估中国 海洛因依赖患者共患ASPD比率的研究做了系统分析。
方法
我们检索了中国数据库(中国知网,万方数据 知识服务平台,台湾电子期刊服务网)和西方数据库 (PubMed和EMBASE)的相关研究。两位作者独立检 索文献,确定符合预定纳入和排除标准的文献,评价 纳入研究的文献质量,并提取用于分析的数据。使用 StatsDirect 3.0进行统计分析。
结果
检索到15项符合条件的研究,共有3692例海 洛因依赖患者。其中仅有2项高质量研究。所有的研 究都是在康复中心或医院进行的。 在这些患者中合 并ASPD终生患病率为30%(95%CI:23~38%), 但这些研究结果的异质性很大(I2 =95%, p<0.001)。男性患者的患病率显著高于女性(44%比21%), 注射吸毒患者的患病率显著高于烫吸的患者(44%比 27%)。研究方法较严谨的报道的海洛因依赖者ASPD 患病率较高。
结论
虽然现有的有关中国接受治疗的海洛因依赖患 者共患ASPD的文献存在较大的方法学问题,但据我 们的分析,估计这些患者中大约有三分之一的人是符 合ASPD诊断标准的。进一步需要开展的工作是提高临 床医生对这一问题的认识,比较伴ASPD患者与不伴 ASPD患者的发病机制、治疗效果和复吸情况,制定出 适合这个治疗相对困难的海洛因依赖患者亚群的针对 性的干预措施并加以验证。
1. Background
Antisocial Personality Disorder (ASPD) is a type of personality disorder that usually develops during childhood or early adolescence and persists into adulthood. It is characterized by a failure to conform to social norms, frequent trouble with the law, a lack of empathy or remorse, and dysfunctional interpersonal relationships.[1] ASPD is one of the most common AXISII mental disorders among individuals with opioid addiction. Studies from the Western countries found that 30 to 71% of individuals with heroin addiction have ASPD.[2],[3],[4] Mounting evidence has shown that ASPD is closely associated with violent behaviors and crimes, risky behaviors (e.g., needle sharing and multiple sexual partners), and HIV infection.[5] Furthermore, it has been associated with poorer treatment compliance and outcomes including early dropping out, relapse, suicidal behaviors, use of multiple drugs, comorbidity with other mental disorders, and reduced quality of life.[5],[6],[7],[8],[9],[10] Therefore, clinicians and researchers in Western countries consider the assessment and management of ASPD an important component of the treatment of drug dependence.[2],[3],[9],[11]
In contemporary China, compulsory rehabilitation (including community detoxification, compulsory quarantined detoxification, and community-based rehabilitation) is the primary form of treatment for illegal drug dependence. This is supplemented by voluntary rehabilitation services.[12],[13] By 2012, there were 549, 000 registered illegal drug users in mainland China: 61.6% received compulsory treatment and 38.4% obtained voluntary rehabilitation services.[14] Most of the compulsory services are managed by public security personnel and have limited medical professional staff, so the emphasis is on physical withdrawal with some drug education and vocational rehabilitation but little in the way of psychological interventions.[13],[15] In contrast the voluntary services are primarily managed by psychiatric hospitals so both the inpatient detoxification and outpatient methadone treatment services usually include psychosocial support and training. However, even in these settings, psychiatrists treating individuals with drug problems are largely unaware of the importance of personality disorders in the management of addictions.[16] This seriously undermines the effectiveness of the clinical treatments provided for individuals dependent on heroin and other illicit drugs.
The development of a personality disorder is influenced by multiple biological, psychological, and social factors. The diagnosis of ASPD is based on comparison of an individual’s behaviors with social norms,[1] so there is some difficulty in using western diagnostic criteria to make the diagnosis in China where the norms of acceptable behavior are somewhat different from those of Western countries. Thus the relationship between ASPD and addictive behaviors, and its relevance in the treatment strategies for addictive conditions may be different in China than elsewhere. Moreover, studies from Western countries report that ASPD is more common in male (versus female) heroin users and more common in heroin users who inject heroin (versus those who smoke heroin).[1],[5] It is unknown whether or not similar relationships exist in Chinese heroin users.
The first step in unravelling this puzzle is to estimate the proportion of individuals with heroin dependence in China who have comorbid ASPD. Previous studies in China have reported wide variations in the prevalence of ASPD among individuals with heroin addiction (from 3 to 62%).[17],[18] To help clarify the issue, this paper reports the results of a systematic review and meta-analysis of the prevalence of ASPD among Chinese individuals with current heroin dependence.
2. Methods
2.1. Inclusion and exclusion criteria
The process of identifying studies included in this analysis is shown in Figure 1. Inclusion criteria were: (a) cross-sectional surveys published in English or Chinese; (b) study participants were Chinese individuals with heroin addiction in whom heroin was the primary drug of abuse; and (c) the lifetime diagnosis of ASPD was made using standardized criteria such as those specified in the 4th edition of the Diagnostic and Statistical Manual of the American Psychiatric Association[19] (DSM-IV), the 10th edition of the International Classification of Diseases[20] (ICD-10), or the 3rd edition of the Chinese Classification of Mental Disorders[21] (CCMD-3). All papers that used one of these three diagnostic criteria were considered regardless of whether or not a specific diagnostic instrument was employed to make the diagnosis. Exclusion criteria were: (a) studies that only used screening tools for ASPD without confirming a clinical diagnosis; (b) studies focused on personality traits, not personality disorders; (c) duplicated reports of results from a single site which were included in a multisite report; and (d) translations of original publications. We did not restrict papers to those that used specific methods for diagnosing heroin dependence and made no other restrictions based on the sex, age, or number of drugs of abuse of the participants (as long as heroin was the main drug of abuse).
Figure 1. Identification of papers for meta-analysis.
2.2. Literature retrieval
The following keywords were used to search the China National Knowledge Infrastructure (CNKI, 1979-2014), Wanfang Data Knowledge Service Platform (1990-2014), VIP (1989-2014), SinoMed (1976-2014), Taiwan Electronic Periodical Services (TEPS, 1963-2014), PubMed (1950-2014), EMBASE (1966-2014), and PsycInfo (1887-2014): (heroin OR opiate OR opioids OR abstinence OR narcotic) AND (personality OR personality disorder OR antisocial personality disorder). In order to prevent omission of relevant studies, we also used the following set of keywords: (dependence OR addiction OR abuse OR drug OR methadone) AND (mental disorder OR psychiatric illness OR psychiatric disease OR comorbidity). The reference lists of relevant publications were cross-referenced. All articles published by August 21, 2014 were included. Literature searches were independently conducted by two authors (BZ and XC); there was one article about which they initially disagreed, but after discussion they agreed to include it.
2.3. Data extraction
Using a pre-designed form, two authors (BZ and XC) independently extracted the following information from each included study: name of the first author, year of publication, type of rehabilitation/treatment (compulsory or voluntary), diagnostic criteria for ASPD, assessment tools used for ASPD, sampling procedure, participation rate of potential subjects, sample size, proportion of males in the sample, mean age of the sample, and the prevalence of ASPD in the sample. Information about differences between males and females or the route of administration (injection v. smoking of heroin) was also obtained when available. The inter-rater agreement between the two coders for all recorded items was 100%.
2.4. Quality assessment
The validity of clinical psychiatric studies that involve diagnostic interviews is mainly determined by the representativeness of the sample and the reliability of the diagnostic method.[22],[23] The representativeness of the sample depends on the sampling method, the participation rate of potential subjects, and the sample size. The reliability of the diagnosis is based on the reliability and validity of the diagnostic instrument employed (if any), the training of the interviewers, the inter-rater reliability of the interviewers, and the test-retest reliability of the diagnosis. After consulting several published systematic reviews,[22],[23],[24] we devised the following set of criteria to assess the quality of the included studies.
Three measures were related to the representativeness of the sample.
(a) Sample Size. Coded as ‘unacceptable’ (n<100), or ‘acceptable’ (n≥100). The minimum acceptable sample size of 100 was determined assuming a Type I error of 0.05, an estimated prevalence of 50%, and an acceptable margin of error of 10%.[25],[26],[27]
(b) Sampling Method. Coded as ‘not reported’, ‘unacceptable’ (convenience sampling), or ‘acceptable’ (random or consecutive sampling).
(c) Participation Rate. Coded as ‘not reported’, ‘unacceptable’ (<70% or significant differences between respondents and non-respondents), or ‘acceptable’ (≥70% or no significant differences between respondents and non-respondents). In epidemiological surveys, a response level of 70% is usually considered acceptable.[28]
Four measures discussed in a previous report[23] were used to assess the reliability and validity of the diagnostic assessment process.
(a) Use of Diagnostic Instrument. Coded as ‘acceptable’ (employed a diagnostic instrument) or ‘unacceptable’ (did not employ a diagnostic instrument).
(b) Reliability and Validity of Diagnostic Instrument. Coded as ‘unacceptable’ (no previous demonstration of psychometric characteristics of instrument employed), or ‘acceptable’ (reliability and validity of instrument reported in index study or in prior studies).
(c) Training of Coders’ Coded as ‘not reported’, ‘unacceptable’ (no formal training occurred), or ‘acceptable’ (provided training of coders in use of instrument).
(d) Inter-rater Reliability of Coders. Coded as ‘not reported’, ‘unacceptable’ (not reported for ASPD), or ‘acceptable’ (reported for ASPD).
These parameters were independently assessed by two authors (BZ and XC) with experience in psychiatric epidemiology and training in the conduct of Cochrane systematic reviews. (One of 15 the papers was only assessed by one coder.) When disagreement occurred in an assessment, they discussed their differences to arrive at a consensus assessment.
An overall quality score of ‘low’, ‘uncertain’, or ‘high’ was assigned to each of the 15 papers as follows. If any of the 7 items are coded ‘unacceptable’ the overall quality is rated as ‘low’; if all of the 7 items are coded as ‘acceptable’ the overall quality is coded as ‘high’; if none of the items are coded as ‘unacceptable’ but one or more items are coded as ‘not reported’ the overall quality of the study is coded as ‘uncertain’.
2.5. Statistical analysis
Meta-analysis was used to produce pooled estimates and their 95% confidence intervals for the prevalence of ASPD in the overall sample and in different subgroups of the sample. Forest plots were used to show the prevalence estimates and the pooled estimates. When there was little evidence of heterogeneity (i.e., I2 ≤50%, heterogeneity p≥0.10), a fixed effect model was used to produce the pooled estimates; otherwise, the random-effect model was used. Subgroup analyses were conducted to explore the origin of heterogeneity in the estimated prevalence of ASPD: comparisons in ASPD prevalence were made based on the year of publication, type of rehabilitation/ treatment (voluntary v. compulsory), criteria used to diagnose ASPD, proportion of males in the sample, mean age of the sample, proportion of intravenous heroin users in the sample, diagnostic assessment procedure (one-stage v. two-stage), and based on each of the 7 measures of study quality. Q-value test was used to assess the significance of differences in ASPD prevalence between these subgroups. Publication bias was assessed using funnel plot and Begg’s/Egger’s tests. Proportions were transformed using the FreemanTukey variant of the arcsine square root transformation or logit transformation (when there is at least one zero cell count).[29] The analyses were conducted using StatsDirect 3.0 (StatsDirect Ltd; Cheshire, UK) and R 3.1.1 (R Development Core Team; Vienna, Austria).
3. Results
3.1. General description of included studies
Fifteen studies with a total of 3692 individuals with heroin dependence were included in the analysis of the results.[17],[18],[25],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41] The basic characteristics of the included studies are shown in Table 1.
Table 1.
Basic description of included studies
| study | location | diagnostic system |
sampling method |
response level (%) |
sample size |
assessment tool |
validity & reliability of tool |
training of coders |
inter-rater reliability |
proportion of males (% |
mean age (year) |
injection users (%) |
ASPD prevalence (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Li 1998[30] a, b | hospital | DSM-Ⅳ | convenience sampling | NR | 30 | PDI-Ⅳ | A | A | A | 66.7 | 29 | 10.0 | 36.7 |
| Chen 1999[18] | prison | DSM-Ⅲ-R | random sampling | NR | 260 | SCID-Ⅱ | A | A | A | 100 | 35 | NR | 34.6 |
| Chen 1999[18] | hospital | DSM-Ⅲ-R | random sampling | NR | NR | SCID-Ⅱ | A | A | A | 100 | 35.2 | NR | 61.7 |
| Zhu 1999[31] a | compulsory rehabilitation center |
DSM-Ⅲ-R | random sampling | NR | 40 | SCID-Ⅱ | A | NR | A | 52.5 | 26.8 | NR | 27.5 |
| Zhang 2000[32] | hospital | CCMD-2-R | convenience sampling | NR | 300 | PSE+ CCMD-2-R |
A | NR | NR | 66.0 | 26.4 | 58.7 | 9.0 |
| Guo 2001[17] | hospital | CCMD-2-R | convenience sampling | NR | 128 | not clear | --- | --- | --- | NR | NR | NR | 3.1 |
| Zhao 2001[25] a, b | compulsory rehabilitation centr |
DSM-Ⅲ-R | convenience sampling | NR | 216 | SCID-Ⅱ | A | A | A | 76.4 | 29 | 72.7 | 47.7 |
| Lu 2005[33] | hospital | DSM-Ⅲ-R | convenience sampling | NR | 113 | SCID-Ⅱ | A | A | NR | 72.7 | 30.1 | 69.1 | 34.5 |
| Deng 2006[34] | compulsory rehabilitation center |
DSM-Ⅳ | convenience sampling | NR | 217 | DIGS+ DSM-Ⅳ |
UA | NR | NR | 83.9 | 30.8 | 67.7 | 14.7 |
| Du 2006[35] a, b | hospital | DSM-Ⅲ-R | convenience sampling | NR | 93 | SCID-Ⅱ | A | A | NR | 77.4 | 30.1 | NR | 41.9 |
| Chiang 2007[36] a | hospital | DSM-Ⅳ | convenience sampling | NR | 155 | MINI | A | A | A | 79.4 | 30.8 | 85.2 | 38.7 |
| Fu 2008[37] | compulsory rehabilitation center |
DSM-Ⅳ | convenience sampling | 72.7 | 298 | PDQ4+ PDI-Ⅳ |
A | A | A | 100 | 32.3 | NR | 21.5 |
| Song 2010[38] | MMT outpatient clinic |
DSM-Ⅳ | random sampling | 85.7 | 90 | SCID-Ⅱ | A | NR | NR | 59.0 | 28 | NR | 33.3 |
| Yang 2011[39] a, b | hospital | DSM-Ⅳ | consecutive sampling | 99 | 120 | SCID-Ⅱ | A | A | A | 92.5 | 33 | 54.2 | 35.8 |
| Yang 2011[39] a, b | compulsory rehabilitation center |
DSM-Ⅳ | consecutive sampling | 99 | 882 | SCID-Ⅱ | A | A | A | 66.9 | 33.2 | 87.9 | 41.4 |
| Xu 2013[40] | MMT outpatient clinic |
DSM-Ⅳ | convenience sampling | NR | 100 | SCID-Ⅱ | A | A | A | 80.0 | 42.4 | NR | 20.0 |
| Xu 2014[41] a, b | MMT outpatient clinic |
DSM-Ⅳ | consecutive sampling | 92.3 | 603 | MINI | A | A | A | 67.2 | 38.1 | 84.0 | 36.8 |
A, acceptable; UA, unacceptable; NR, not reported
MMT, methadone maintenance treatment; PDI-Ⅳ, personality disorder interview; SCID-Ⅱ, structured clinical interview for DSM-Ⅳ axis Ⅱ disorder; PSE, Present State Examination;
DIGS, Diagnostic Interview For Genetic Studies; MINI, Mini-International Neuropsychiatric Interview; PDQ4, personality questionnaire-4; ASPD, antisocial personality disorder
aonly reported sex-specific prevalence
bonly reported prevalence by route of administration
Two studies from Taiwan were published in English,[18],[36] the remaining 13 studies from mainland China were published in Chinese. Settings included outpatient methadone maintenance clinics (3 studies),[38],[40],[41] hospitals (8 studies),[17],[18],[30],[32],[33],[35],[36],[39] and compulsory rehabilitation centers (6 studies);[18],[25],[31],[34],[37],[39] two studies included both voluntary and compulsory rehabilitation centers.[18],[39]
Three studies adopted a two-stage diagnostic procedure (i.e., screening and then diagnosis),[31],[34],[37] and the rest used a one-stage diagnostic procedure. One study determined the clinical diagnosis without the use of a standardized assessment tool,[17] one study used the ‘Diagnostic Interview for Genetic Studies’ without providing data on the validity and reliability of the assessment tool,[31] and the remaining 13 studies used well-recognized diagnostic tools. Four of the 14 studies that used diagnostic instruments did not clarify whether or not coders were provided training in the use of the instrument.[31],[32],[34],[38] Only 5 studies[31],[32],[33],[34],[35],[38] reported inter-rater reliability between the coders. Overall, the diagnostic assessment was rated as ‘reliable’ --for 8 of the 15 studies.[18],[25],[30],[36],[37],[39],[40],[41]
Four studies reported participation rates from 73 to 99%;[37],[38],[39],[41] 6 studies used consecutive or random sampling;[18],[31],[36],[38],[39],[41] and 4 studies were smallscale studies (n<100).[30],[31],[35],[38] Only 2 studies enrolled samples that were considered representative of the population of interest (Chinese individuals with heroin dependence).[39],[41] The overall quality rating for the 15 studies was rated ‘high’ for two studies,[39],[41] ‘uncertain’ for 2 studies,[18],[36] and ‘poor’ for 11 studies.[17],[25],[30],[31],[32],[33],[34],[35],[37],[38],[40]
3.2. Meta-analysis of the prevalence of antisocial personality disorder among individuals with heroin dependence in China
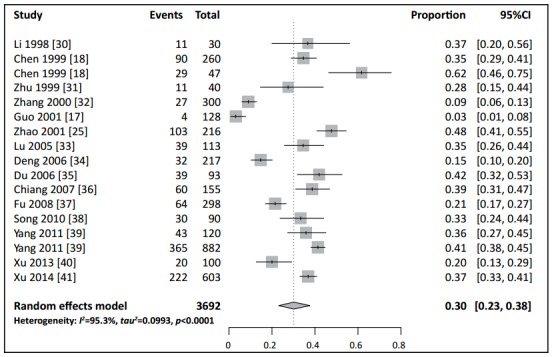
Meta-analysis of the results shown in Figure 2 found a high level of heterogeneity in the prevalence of ASPD in the 15 included studies (p<0.001, I2 =95.3%). Therefore, a random-effect model was used to generate the pooled estimate of the prevalence of ASPD among Chinese individuals with heroin dependence: 30% (95%CI= 23%, 38%) (Figure 2).
Figure 2. Forest plot of prevalence of antisocial personality disorder among Chinese individuals with heroin dependence.
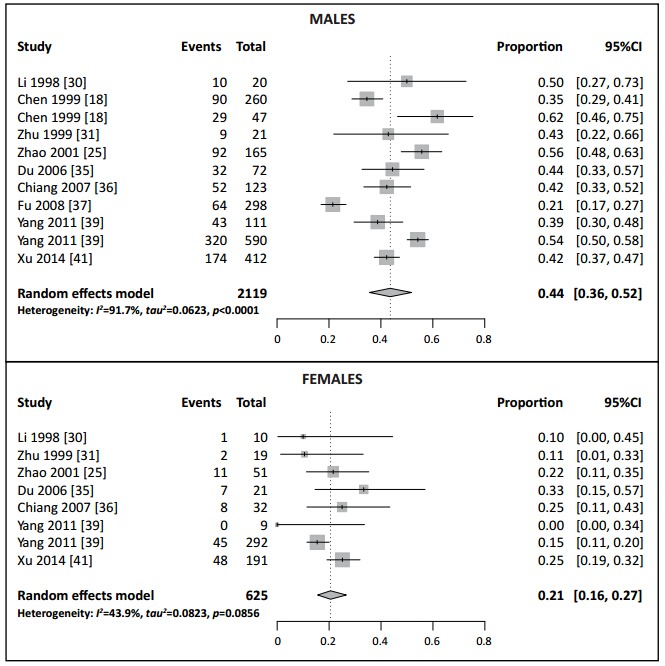
As shown in Figure 3, the 9 studies that reported the prevalence of ASPD among males were also quite heterogeneous (I2 =91.7% and p<0.001), so the random effect model was employed to estimate the pooled prevalence of 44% (95%CI=36%, 52%). The corresponding pooled estimate from the 7 studies that reported ASPD prevalence in females with heroin dependence was 21% (95%CI=16%, 27%;I2 =43.9%, p=0.086). Thus males who were heroin dependent were significantly more likely to have comorbid ASPD than females who were heroin dependent (test for subgroup differences Chi-squared=133.26, p<0.001).
Figure 3. Forest plot of prevalence of antisocial personality disorder among heroin dependent individuals by sex.
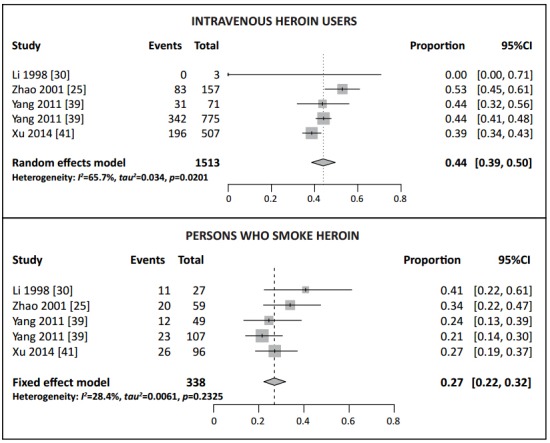
The pooled prevalence for intravenous heroin users and those who smoke heroin are shown in Figure 4. The pooled estimate for intravenous users based on the random effect model was 44% (95%CI=39%, 50%; I2 =65.7%, p=0.020). The prevalence results from the 4 studies of individuals who smoked heroin were not highly heterogeneous (I2 =28.4%, p=0.233), so a fixedeffect model was used to estimate the pooled ASPD prevalence of 27% (95%CI=22%, 32%). Thus intravenous heroin users were significantly more likely to have comorbid ASPD than individuals who smoked heroin (test for subgroup differences Chi-squared=28.96, p<0.001).
Figure 4. Forest plot of prevalence of antisocial personality disorder among heroin dependent individuals by method of heroin use.
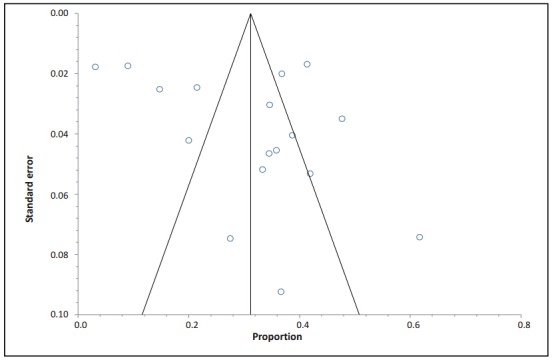
3.3. Publication bias among included studies
The p-values of the Begg’s test and Egger’s test were 0.90 and 0.15 for the 15 studies. The funnel plot (Figure 5) showed a generally symmetric distribution of the studies. We conclude that there was no significant publication bias among the included studies.
Figure 5. Funnel plot of publication bias among the 15 included studies.
3.4. Source of heterogeneity
The results of the subgroup analyses are shown in Table 2. The pooled prevalence of ASPD was significantly different in the different strata of several of the parameters considered. In addition to the relationship of ASPD prevalence to gender and method of heroin use (described above), the prevalence of ASPD was significantly higher in studies conducted in Taiwan (v. those conducted in mainland China), in studies that used diagnostic instruments (v. the study that used a clinical diagnosis), in studies that used DSM diagnostic criteria (v. CCMD criteria), in studies with a one-step diagnostic procedure (v. a two-stage diagnosis), in studies that used random or consecutive sampling (v. convenience sampling), and in the two studies that were classified as high-quality (v. the 11 studies classified as poor-quality).
Table 2.
Subgroup analysis of the source of heterogeneity of included studies
| factor | number of studies |
sample size |
number of cases |
heterogeneity [I2] % (p-value) |
pooled prevalence % (95%CI) |
Q | p |
|---|---|---|---|---|---|---|---|
| publication year | |||||||
| 1998~2005 | 8 | 1227 | 353 | 93.9 (<0.001) | 29.1 (18.7, 42.3) | 0.005 | 0.941 |
| 2006~2014 | 7 | 2465 | 836 | 91.8 (<0.001) | 29.7 (23.3, 37.0) | ||
| region | |||||||
| mainland China | 13 | 2230 | 1010 | 93.5 (<0.001) | 26.9 (20.8, 34.0) | 5.477 | 0.019 |
| Taiwan, China | 2 | 462 | 179 | 82.7 (0.003) | 43.1 (31.4, 55.7) | ||
| type of treatment | |||||||
| compulsory | 6 | 1913 | 665 | 94.4 (<0.001) | 30.3 (21.5, 40.9) | 0.033 | 0.856 |
| voluntary | 11 | 1779 | 524 | 92.0 (<0.001) | 29.1 (21.3, 38.5) | ||
| diagnostic system | |||||||
| DSM-III-R~IV | 13 | 3264 | 1158 | 87.8 (<0.001) | 34.2 (29.2, 39.6) | 14.161 | <0.001 |
| CCMD-2-R | 2 | 428 | 31 | 76.2 (0.040) | 5.9 (2.1, 15.5) | ||
| mean age (year)b | |||||||
| 26.4~30.1 | 7 | 882 | 260 | 93.1 (<0.001) | 31.1 (19.6, 45.5) | 0.030 | 0.863 |
| 30.8~38.1 | 8 | 2682 | 925 | 91.9 (<0.001) | 32.4 (25.9, 39.6) | ||
| diagnostic procedure | |||||||
| one-stage | 12 | 2877 | 1066 | 82.7 (<0.001) | 35.4 (30.7, 40.4) | 13.448 | <0.001 |
| two-stage | 3 | 815 | 123 | 88.5 (<0.001) | 14.5 (8.6, 23.4) | ||
| sample size | |||||||
| 30~93 | 6 | 420 | 163 | 63.7 (<0.001) | 39.2 (31.3, 47.8) | 6.059 | 0.014 |
| 100~882 | 11 | 3272 | 1026 | 95.0 (<0.001) | 25.4 (19.0, 33.1) | ||
| sampling method | |||||||
| consecutive or random sampling | 6 | 2197 | 850 | 62.6 (0.009) | 38.2 (34.3, 42.3) | 6.483 | 0.011 |
| convenience sampling | 9 | 1495 | 339 | 94.6 (<0.001) | 22.1 (13.7, 33.5) | ||
| participation rate (%) | |||||||
| 72.7~99.0 | 4 | 1993 | 724 | 89.2 (<0.001) | 33.6 (26.9, 41.0) | 0.949 | 0.330 |
| not reported | 11 | 1699 | 465 | 93.6 (<0.001) | 27.6 (19.3, 37.9) | ||
| use of assessment tools | |||||||
| yes | 14 | 3564 | 1185 | 92.1 (<0.001) | 31.9 (26.2, 38.1) | 25.233 | <0.001 |
| no | 1 | 128 | 4 | --- | 3.1 (1.2, 8.0) | ||
| assessment tool | |||||||
| SCID-II | 7 | 1861 | 749 | 67.1 (0.002) | 39.7 (35.1, 44.4) | 7.313 | 0.007 |
| othersa | 7 | 1703 | 436 | 94.3 (<0.001) | 23.3 (15.2, 33.9) | ||
| validity/reliability of assessment tool | |||||||
| acceptable | 13 | 3347 | 1153 | 90.7 (<0.001) | 33.4 (27.8, 39.5) | 20.730 | <0.001 |
| not reported | 4 | 647 | 100 | 90.8 (<0.001) | 19.0 (10.0, 33.1) | ||
| inter-rater reliability of coders | |||||||
| yes | 9 | 2715 | 1018 | 86.1 (<0.001) | 35.9 (30.6, 41.6) | 2.031 | 0.154 |
| not reported | 5 | 813 | 167 | 94.2 (<0.001) | 24.1 (13.1, 40.1) | ||
| overall quality of studyb | |||||||
| high | 2 | 1605 | 630 | 46.9 (0.152) | 39.3 (36.9, 41.7) | reference | --- |
| uncertain | 2 | 415 | 150 | 0.0 (0.401) | 36.2 (31.7, 40.9) | 0.755 | 0.385 |
| low | 11 | 1672 | 409 | 93.6 (<0.001) | 26.0 (17.7, 36.4) | 5.815 | 0.016 |
CI, confidence interval
aincludes MINI, “PSE+CCMD-2-R”, “DIGS+DSM-Ⅳ” and “PDQ4+PDI-Ⅳ”
bsee description of method of determining overall quality in the methods section
4. Discussion
4.1. Main findings
This meta-analysis summarized studies reporting the prevalence of ASPD among individuals with heroin dependence in China. We found that 30% of individuals with heroin dependence had comorbid ASPD and that the prevalence was higher in men than in women and higher in intravenous heroin users than in those who smoked heroin. This overall 30% prevalence is similar to that reported in two studies from the United States (30% and 35%)[3],[42] and one study from Switzerland (31%),[43] but lower than that reported in two studies from Australia (61% and 71%)[2],[4] and in three other studies from the United States (55%, 45%, and 60%).[44],[45],[46],[47] Therefore, the prevalence of ASPD among individuals with heroin dependence in China hovers on the lower end of the prevalence range reported in other, primarily high-income, countries.
Two studies from foreign countries[3],[43] reported ASPD prevalence estimates of 34.1% and 32.9% among males, and of 22.4% and 16.7% among females; the pooled prevalence among males in our study (44%) is higher compared to these two studies but the pooled prevalence among females (20%) is similar. The prevalence of ASPD among injection heroin users in our study (44%) is similar to that previously reported in the United States and Australia (36% and 44%).[47],[48],[49] One possible explanation for differences in overall ASPD prevalence among heroin dependent individuals between China and other countries is that the proportions of males and intravenous heroin users in the samples may differ cross-nationally.
Previous studies in the United States reported a lifetime prevalence of ASPD of 3.6% in the general population.[50] In contrast, the reported prevalence in the general Chinese population in 1998 was only 0.01%.[51] If these community based estimates are accurate, the crude relative risk of lifetime ASPD among heroin dependent individuals in China is much greater than that in the United States (3000:1 v. 10:1).
The diagnosis of ASPD requires the presence of both conduct problems before adulthood and antisocial behaviors during adulthood. Thus, individuals with a history of conduct problems during childhood or adolescence who subsequently abuse heroin will meet ASPD diagnostic criteria if, as is frequently the case, heroin dependence is associated with any type of antisocial behavior. Individuals with long-term heroin dependence often develop antisocial behaviors related to drug seeking (e.g., legal problems, theft, and aggressive behaviors); it is also possible that the emergence of such problems is the result of the effects of heroin on the central nervous system.[4] It is also possible that there are causal loops between drug dependence, ASPD, and behavioral problems. For example, there is evidence that type B personality disorder is a risk factor of drug dependence,[52],[53] and individuals with drug dependence are more likely to have behavioral problems or commit crimes.[54]
Our finding of a higher prevalence of ASPD among males than females with heroin dependence is consistent with previous studies.[3],[5],[43],[47] Possible reasons include higher levels of testosterone, which has been associated with higher levels of aggression and impulsiveness.[55] There are several possible explanations for the higher ASPD prevalence among intravenous heroin users versus those who smoke heroin. Darke and colleagues[4] found that intravenous drug users with ASPD were more likely than those without ASPD to share needles; this lack of consideration of consequences - a characteristic of ASPD - may be more prevalent in those who inject heroin than in those who smoke heroin.
Subgroup analysis found that in addition to differences by gender and by the proportion of intravenous heroin users in the sample, several other variables are associated with the reported prevalence of ASPD among Chinese individuals with heroin dependence. Studies that used DSM criteria had higher reported prevalence than those that used CCMD criteria and smaller studies had higher reported prevalence than larger studies. Generally speaking, the reported prevalence of comorbid ASPD among heroin dependent individuals was higher in studies of higher quality - that is, studies that used structured diagnostic instruments, that used random or consecutive sampling rather than convenience sampling, that had >70% participation by eligible subjects, that provided training to examiners, and so forth. However, even after stratifying the studies, substantial heterogeneity remained within each strata of study, so there remain other factors that are influencing ASPD prevalence that were not identified.
4.2. Limitations
The main limitations of this study are that (a) 11 of the 15 included studies were rated as low quality; and (b) there was very substantial heterogeneity in the estimated ASPD prevalence across studies, even after stratifying the studies by several potential predictors of heterogeneity. Subgroup analysis found lower prevalence estimates in low-quality studies, so it is possible that the reported overall pooled estimate under-estimates the true prevalence. The heterogeneity of results suggests that further standardization of methods and sample selection will be needed to arrive at better estimates. Studies focusing on understanding the reasons for this heterogeneity may help identify unique elements of personality disorders and substance abuse in China that can explain the much higher relative risk of ASPD among heroin dependent individuals in China versus that seen in high-income countries (crudely estimated as 3000:1 versus 10:1, a 300-fold difference).
Our combined sample had a 1:1 ratio of voluntary versus involuntary patients, whereas the ratio in mainland China overall is about 1:2,[14] so the study sample may not be representative of all individuals who receive treatment for heroin abuse in the country. However, we found no significant difference in ASPD prevalence between those treated in voluntary versus involuntary settings, so it is unlikely that this lack of representativeness affected the relevance of our pooled estimate. And our 70% cutoff score for assessing selection bias may be too generous; accepting a 30% non-participation rate could potentially obscure important biases in the sample if, for example, individuals with personality disorders were much less likely to participate.
4.3. Implications
This study found that despite very low reported prevalence of ASPD in the Chinese community, ASPD is common among Chinese individuals with heroin dependence. The overall pooled prevalence of about 30% is similar to the prevalence seen among heroin dependent individuals in other countries. Also similar to other countries, the prevalence of ASPD in China is higher in males with heroin dependence (v. females) and in intravenous heroin users (v. those who smoke heroin). ASPD is associated with worse clinical outcomes and higher rates of recidivism among individuals with substance abuse problems, so clinicians should regularly screen individuals with heroin dependence and other substance abuse problems for ASPD and, when present, tailor their management strategies accordingly. The quality of epidemiological studies about the prevalence of personality disorder among individuals with substance abuse problems in China needs to improve and new research is needed that focuses on understanding the relevance of the very high relative risk of ASPD among heroin dependent individuals and on developing effective strategies for treating individuals in China with comorbid substance abuse and personality disorders.
Biography

Dr. Baoliang Zhong attained his PhD from the Department of Psychiatry, Chinese University of Hong Kong in 2014 after he obtained his Master of Science and Bachelor of Medicine from the School of Public Health, Peking University Health Science Center in 2008 and 2006. He has been an attending doctor at the Department of Scientific Research and Education, affiliated Mental Health Center of Tongji Medical College of Huazhong University of Science and Technology since 2008 where he is currently the Deputy Chief of the Department. His main research interest is public health and mental health.
Funding Statement
This analysis was supported by Wuhan City Health Bureau (WG11D03 and WG11A02).
Footnotes
Conflict of interest: Authors declare no conflict of interest related to this manuscript.
References
- 1.Glenn A, Johnson A, Raine A. Antisocial personality disorder: a current review. Curr Psychiatry Rep. 2013;15(12):427. doi: 10.1007/s11920-013-0427-7. [DOI] [PubMed] [Google Scholar]
- 2.Darke S, Williamson A, Ross J, Teesson M, Lynskey M. Borderline personality disorder antisocial personality disorder and risk-taking among heroin users: findings from the Australian Treatment Outcome Study (ATOS) Drug Alcohol Depend. 2004;74(1):77–83. doi: 10.1016/j.drugalcdep.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Grella C, Karno M, Warda U, Niv N, Moore A. Gender and comorbidity among individuals with opioid use disorders in the NESARC study. Addict Behav. 2009;34(6-7):498–504. doi: 10.1016/j.addbeh.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Darke S, Hall W, Swift W. Prevalence symptoms and correlates of antisocial personality disorder among methadone maintenance clients. Drug Alcohol Depend. 1994;34(3):253–257. doi: 10.1016/0376-8716(94)90164-3. [DOI] [PubMed] [Google Scholar]
- 5.Neufeld K, Kidorf M, Kolodner K, King V, Clark M, Brooner R. A behavioral treatment for opioid-dependent patients with antisocial personality. J Subst Abuse Treat. 2008;34(1):101–111. doi: 10.1016/j.jsat.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooner R, Greenfield L, Schmidt C, Bigelow G. Antisocial personality disorder and HIV infection among intravenous drug abusers. Am J Psychiatry. 1993;150(1):53–58. doi: 10.1176/ajp.150.1.53. [DOI] [PubMed] [Google Scholar]
- 7.Black D, Gunter T, Loveless P, Allen J, Sieleni B. Antisocial personality disorder in incarcerated offenders: Psychiatric comorbidity and quality of life. Ann Clin Psychiatry. 2010;22(2):113–120. [PubMed] [Google Scholar]
- 8.Fassino S, Daga G, Delsedime N, Rogna L, Boggio S. Quality of life and personality disorders in heroin abusers. Drug Alcohol Depend. 2004;76(1):73–80. doi: 10.1016/j.drugalcdep.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Moos R, Moos B, Finney J. Predictors of deterioration among patients with substance-use disorders. J Clin Psychol. 2001;57(12):1403–1419. doi: 10.1002/jclp.1105. [DOI] [PubMed] [Google Scholar]
- 10.King V, Kidorf M, Stoller K, Carter J, Brooner R. Influence of antisocial personality subtypes on drug abuse treatment response. J Nerv Ment Dis. 2001;189(9):593–601. doi: 10.1097/00005053-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Samuel D, LaPaglia D, Maccarelli L, Moore B, Ball S. Personality disorders and retention in a therapeutic community for substance dependence. Am J Addict. 2011;20(6):555–562. doi: 10.1111/j.1521-0391.2011.00174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yan W, Wang X. [Evaluation for our current Modalities and thinking for the reform of future direction] Zhongguo Yao Wu Yi Lai Xing Za Zhi. 2004;13(4):312–314. Chinese. [Google Scholar]
- 13.Xie C. [The development and challenges of Chinese drug model in new era] Zhongguo Ren Ming Gong An Da Xue Xue Bao (She Hui Ke Xue Ban) 2013;162:45–46. Chinese. [Google Scholar]
- 14.National Narcotics Control Commission Office, Ministry of Public Security Bureau Narcotics. [cited 2014 June 21];[Chinese anti-drug report in 2013] 2014 Chinese. Available from: http://www.mps.gov.cn/n16/n80209/n80481/n804535/3815337.html .
- 15.Yang M, Mamy J, Zhou L, Liao YH, Wang Q, Weewoobudul V, et al. Gender differences in prevalence and correlates of antisocial personality disorder among heroin dependent users in compulsory isolation treatment in China. Addict Behav. 2014;39(3):573–579. doi: 10.1016/j.addbeh.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Tong J. [Psychological consoling and treatment of personality disorders] Beijing: Peking University Medical Press; 2008. Chinese. [Google Scholar]
- 17.Guo Q, Li L. [Mental disorders with heroin addicts] Zhongguo Yao Wu Lan Yong Fang Zhi Za Zhi. 2001;6:23–24. Chinese. [Google Scholar]
- 18.Chen C, Tsai S, Su L, Yang T, Tsai C, Hwu H. Psychiatric comorbidity among male heroin addicts: differences between hospital and incarcerated subjects in Taiwan. Addiction. 1999;94(6):825–832. doi: 10.1046/j.1360-0443.1999.9468256.x. [DOI] [PubMed] [Google Scholar]
- 19.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 20.World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization; 1993. [Google Scholar]
- 21.Chinese Society of Psychiatry. [The Chinese Classification and Diagnostic Criteria of Mental Disorders Version 3 (CCMD-3)]. Jinan: Chinese Society of Psychiatry; 2001. Chinese. [Google Scholar]
- 22.Walker J, Holm-Hansen C, Martin P, Sawhney A, Thekkumpurath P, Beale C, et al. Prevalence of depression in adults with cancer: a systematic review. Ann Oncol. 2013;24(4):895–900. doi: 10.1093/annonc/mds575. [DOI] [PubMed] [Google Scholar]
- 23.Zhong B, Zhang J, He M, Huang Y, Chen H. [Methodology improvement in China mental disorders epidemiological surveys from 1950 to 2008] Zhonghua Jing Shen Ke Za Zhi. 2010;43(4):235–240. Chinese. [Google Scholar]
- 24.Zhong B, Liu T, Chiu H, Chan S, Hu CY, Hu XF, et al. Prevalence of psychological symptoms in contemporary Chinese ruralto-urban migrant workers: an exploratory meta-analysis of observational studies using the SCL-90-R. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1569–1581. doi: 10.1007/s00127-013-0672-4. [DOI] [PubMed] [Google Scholar]
- 25.Zhao M, Yang X, Zhao Y, Hao W, Yang D. [Psychiatric comorbidity among heroin dependent patients] Zhongguo Yao Wu Yi Lai Xing Za Zhi. 2001;10(3):192–194. Chinese. [Google Scholar]
- 26.Naing L, Winn T, Rusli B. Practical issues in calculating the sample size for prevalence studies. Archives of Orofacial Sciences. 2006;1:9–14. [Google Scholar]
- 27.Fleiss J, Levin B, Paik M. Statistical Methods for Rates and Proportions. Third Edition. New York: John Wiley & Sons; 2003. [Google Scholar]
- 28.Mundy D. Solution corner: a question of response rate. Science Editor. 2002;25(1):25–26. [Google Scholar]
- 29.Stuart A, Ord J. Kendall’s Advanced Theory of Statistics (6th edition). London: Edward Arnold; 1994. [Google Scholar]
- 30.Li H, Liu C. [Preliminary investigations on the antisocial personality of heroin addicts] Huaxi Yi Xue. 1998;13(2):140–141. Chinese. [Google Scholar]
- 31.Zhu Z, Liu X. [Research of the heroin addicts combined personality disorder] Zhongguo Xing Wei Yi Xue Ke Xue. 1999;8(3):228–229. Chinese. [Google Scholar]
- 32.Zhang CL, Zhang JQ. [Heroin dependence and mental disorders] Xuzhou Yi Xue Yuan Xue Bao. 2000;20(3):228–229. Chinese. [Google Scholar]
- 33.Lu GH, Du J, Zhao M, Xu H, Zhu M, Xie B. [Comorbidity analysis among heroin dependent patients] Zhongguo Yao Wu Lan Yong Zhi Liao Za Zhi. 2005;11(6):326–328. Chinese. [Google Scholar]
- 34.Deng Y. [Association of psychiatric comorbidity in Chinese heroin dependence patients with polymorphisms in the serotonin transporter promote gene(Thesis)]. Kunming Medical College: 2006. Chinese. [Google Scholar]
- 35.Du J, Zhao M, Xie B, Lu GH, Xu H, Wang QY, et al. [Personality disorders and gender difference in heroin dependence] Shanghai Arch Psychiatry. 2006;18(1):17–19. doi: 10.3969/j.issn.1002-0829.2006.01.005. Chinese. [DOI] [Google Scholar]
- 36.Chiang S, Chan H, Chang Y, Sun H, Chen W, Chen C. Psychiatric comorbidity and gender difference among treatment-seeking heroin abusers in Taiwan. Psychiatry Clin Neurosci. 2007;61(1):105–111. doi: 10.1111/j.1440-1819.2007.01618.x. [DOI] [PubMed] [Google Scholar]
- 37.Fu W, Que M, Kong M, Zhao XF, Wang XY, Guo LL, et al. [Investigation of positivity rate of personality disorder in drug abuse] Suzhou Da Xue Xue Bao: Yi Xue Ban. 2008;28(5):779–781,784. Chinese. [Google Scholar]
- 38.Song H, Qiu J, Dai Y. [A survey on the comorbidity of heroin addicts and personality disorders] Lin Chuang Jing Shen Yi Xue Za Zhi. 2010;20(4):258–259. Chinese. [Google Scholar]
- 39.Yang M. [Prevalence rates and related factors of co-occurring mental disorders and other substance use disorders among heroin-dependent patients][PhD thesis]. Changsha: Central South University; 2011. Chinese. [Google Scholar]
- 40.Xu H, Li Y, Zhang J, Xie MY, Chen GL, Liu YH, et al. [Comorbidity of psychiatric disorder in individuals with methadone maintenance treatment] Zhongguo Yao Wu Yi Lai Xing Za Zhi. 2013;22(3):197–199. Chinese. [Google Scholar]
- 41.Xu Y, Zhong B, Zhu J, Liu T. [Prevalence and characteristics of antisocial personality disorder among heroin dependent patients with methadone maintenance treatment: a crosssectional survey] Zhongguo Yao Wu Yi Lai Xing Za Zhi. 2014;23(1):56–59. Chinese. [Google Scholar]
- 42.Khantzian E, Treece C. DSM-Ⅲ psychiatric diagnosis of narcotic addicts. Recent findings. Arch Gen Psychiatry. 1985;42(11):1067–1071. doi: 10.1001/archpsyc.1985.01790340045007. [DOI] [PubMed] [Google Scholar]
- 43.Frei A, Rehm J. Co-morbidity: psychiatric disorder of opiate addicts at entry into heroin-assisted treatment. Psychiatr Prax. 2002;29(5):251–257. doi: 10.1055/s-2002-32712. [DOI] [PubMed] [Google Scholar]
- 44.Kosten T, Rounsaville B, Kleber H. DSM-Ⅲ personality disorders in opiate addicts. Compr Psychiatry. 1982;23(6):572–581. doi: 10.1016/0010-440x(82)90050-5. [DOI] [PubMed] [Google Scholar]
- 45.Kosten TA, Kosten TR, Rounsaville B. Personality disorders in opiate addicts show prognostic specificity. J Subst Abuse Treat. 1989;6(3):163–168. doi: 10.1016/0740-5472(89)90003-2. [DOI] [PubMed] [Google Scholar]
- 46.Craig R. Prevalence of personality disorders among cocaine and heroin addicts. Subst Abus. 2000;21(2):87–94. doi: 10.1080/08897070009511421. [DOI] [PubMed] [Google Scholar]
- 47.Brooner R, Bigelow G, Strain E, Schmidt C. Intravenous drug abusers with antisocial personality disorder: increased HIV risk behavior. Drug Alcohol Depend. 1990;26(1):39–44. doi: 10.1016/0376-8716(90)90081-O. [DOI] [PubMed] [Google Scholar]
- 48.Brooner R, Schmidt C, Felch L, Bigelow G. Antisocial behavior of intravenous drug abusers: implications for diagnosis of antisocial personality disorder. Am J Psychiatry. 1992;149(4):482–487. doi: 10.1176/ajp.149.4.482. [DOI] [PubMed] [Google Scholar]
- 49.Darke S, Kaye S, Finlay-Jones R. Antisocial personality disorder psychopathy and injecting heroin use. Drug Alcohol Depend. 1998;52(1):63–69. doi: 10.1016/S0376-8716(98)00058-1. [DOI] [PubMed] [Google Scholar]
- 50.Compton W, Conway K, Stinson F, Colliver J, Grant B. Prevalence correlates and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66(6):677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- 51.Zhang W, Shen Y, Li SR. [Epidemiological investigation on mental disorders in 7 areas of China] Zhonghua Jing Shen Ke Za Zhi. 1998;31(2):69–71. Chinese. [Google Scholar]
- 52.Trull T, Waudby C, Sher K. Alcohol tobacco and drug use disorders and personality disorder symptoms. Exp Clin Psychopharmacol. 2004;12(1):65–75. doi: 10.1037/1064-1297.12.1.65. [DOI] [PubMed] [Google Scholar]
- 53.Cohen P, Chen H, Crawford T, Brook J, Gordon K. Personality disorders in early adolescence and the development of later substance use disorders in the general population. Drug Alcohol Depend. 2007;88(Suppl 1):S71–S84. doi: 10.1016/j.drugalcdep.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Copur M, Turkcan A, Erdogmus M. Substance abuse, conduct disorder and crime: assessment in a juvenile detention house in Istanbul, Turkey. Psychiatry Clin Neurosci. 2005;59(2):151–154. doi: 10.1111/j.1440-1819.2005.01350.x. [DOI] [PubMed] [Google Scholar]
- 55.Montoya E, Terburg D, Bos P, van-Honk J. Testosterone, cortisol, and serotonin as key regulators of social aggression: A review and theoretical perspective. Motiv Emot. 2012;36(1):65–73. doi: 10.1007/s11031-011-9264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


