Abstract
Objective:
To identify explanatory factors for the association between depression and increased mortality up to 5 years after stroke.
Methods:
In this cohort study, data from the South London Stroke Register (1998–2013) were used. Patients (n = 3,722) were assessed at stroke onset. Baseline data included sociodemographics and stroke severity. Follow-up at 3 months included assessment for depression with the Hospital Anxiety and Depression Scale (scores ≥7 = depression). Associations between depression at 3 months and mortality within 5 years of stroke were estimated with Cox regression models adjusted for age, sex, ethnicity, and stroke severity, and subsequently adjusted for possible explanatory factors for the association. These factors, introduced into the model individually, included comorbidities at baseline, smoking and alcohol use, compliance with medication, treatment with selective serotonin reuptake inhibitors (SSRIs), social support, and activities of daily living at 3 months.
Results:
A total of 1,354 survivors were assessed at 3 months: 435 (32.1%) had depression and 331 (24.4%) died within 5 years. Survivors with depression had a greater risk of mortality (hazard ratio [HR] 1.41 [95% confidence interval (CI) 1.13–1.77]; p = 0.002). The association between depression and mortality was strongest in patients younger than 65 years. Adjustment for comorbidities, smoking and alcohol use, SSRI use, social support, and compliance with medication did not change these associations. SSRIs started after stroke were associated with higher mortality, independently of depression at 3 months (HR 1.72 [95% CI 1.34–2.20]; p < 0.001).
Conclusion:
Depression after stroke is associated with higher mortality, particularly among younger patients. Stroke survivors taking SSRIs have an increased mortality. The association between depression and mortality is not explained by other individual medical factors.
Depression has a prevalence of around 30% in the long term after stroke, with most patients developing their first symptoms shortly after the acute event.1,2 Depression after stroke is more prevalent among those with severe strokes, disability, and cognitive impairment, and has been found to be independently associated with higher mortality.3,4 A number of medical and social factors have been proposed to underlie the relationship between depression and mortality. They include younger age, lifestyle factors such as smoking and heavy alcohol use, lack of compliance with medication, comorbidities such as diabetes and heart failure, use of antidepressants, and social isolation.5–12 These explanatory factors have been reported in studies not specifically investigating stroke survivors5,6,8–11 or presented in the discussion of systematic reviews of depression and risk of mortality after stroke.7,12
Since depression is independently associated with higher mortality, we could also hypothesize that antidepressants may have a positive effect on the long-term prognosis of stroke patients. However, it has been reported that antidepressants are associated with adverse outcomes, including higher risk of stroke and mortality.7,13
A better understanding of the association between depression and mortality would strengthen the evidence for causality, improve the therapeutic approach to stroke survivors with mood disorders, and provide important prognostic information on survival.
This study investigates the association between depression 3 months after stroke and all-cause mortality up to 5 years, and examines the role of potential explanatory factors in this association. The effect of selective serotonin reuptake inhibitors (SSRIs) on mortality, and on the association between depression and mortality, is specifically investigated.
METHODS
The study conformed to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) study design recommendations.14
Patients with first-ever strokes were recruited from the South London Stroke Register (SLSR), a prospective population-based cohort study.15 Data from patients registered in the SLSR between 1998 and 2012 and followed up until June 30, 2013, were used. The definition of stroke proposed by the WHO was used.16 To increase completeness of notification, 16 overlapping referral sources were used.15 SLSR fieldworkers registered patients during the acute phase of stroke. Data on age, sex, and ethnicity (white, black, and other ethnicity) were collected.15 Stroke severity measures were also recorded, including Glasgow Coma Scale score (GCS), categorized as severe (3–8), moderate (9–12), or mild (13–15); levels of impairment; urinary incontinence; and paresis.15 Other data collected at baseline included regular medication taken before stroke, medical history of diabetes, hypertension, congestive heart failure, ischemic heart disease, and atrial fibrillation.
Follow-up 3 months after stroke was by postal questionnaire or interview. At follow-up, patients were screened for depression using the Hospital Anxiety and Depression Scale (HADS).17 HADS has been validated in stroke patients, showing good performance both when it is used by an interviewer and when it is self-administered18 (optimum performance when scores above 7 in the HADS depression subscale are used to identify depression: sensitivity 0.82, specificity 0.76).17 No information could be recorded from patients with impaired communication that the SLSR fieldworker judged would give invalid data. Disability was also assessed 3 months after stroke using the Barthel Index19: scores of 0–14 were categorized as severe disability, 15–19 moderate disability, and 20 independent. Other data collected at 3 months included smoking habit (smoker or nonsmoker), weekly alcohol consumption (less than 1 unit, less than 14 units, 14–21 units, more than 21 units), and social support: Do you see as much of your relatives or friends as you would like? (Yes/No). Medication taken regularly was recorded as well at 3 months, including SSRIs (never, started before stroke, or started after stroke), antihypertensive medication, and diabetes medication. Mortality within 5 years of stroke was recorded by the SLSR fieldworkers and verified by the Office for National Statistics.20
Statistical methods.
Cox regression was used to analyze the association between depression at 3 months and all-cause mortality within 5 years of stroke. All models were adjusted for age, sex, ethnicity, and stroke severity measures (GCS, incontinence, and hemiparesis). Different models were constructed with further adjustment for potential explanatory factors for the association. The first model was adjusted for comorbidities at baseline (diabetes, hypertension, congestive heart failure, ischemic heart disease, and atrial fibrillation). All other models were adjusted for potential explanatory factors collected at 3 months. The second model was adjusted for smoking and alcohol consumption, adjustment for treatment of hypertension and diabetes was conducted in the third model, adjustment for social support in the fourth, disability in the fifth, and use of SSRIs at 3 months in the sixth model.
Most explanatory variables, including depression, had some missing data. A separate category was assigned, e.g.: Paresis 0 (No), 1 (Yes), and 2 (Missing). Sensitivity analysis was conducted to compare estimates obtained when the category for missing data was included and when it was not included. Most estimates were consistent with those based on complete data so the results obtained using missing data categories were reported. Any differences observed between estimates obtained with and without the missing data category were presented. Further testing of the robustness of the results was conducted using mortality at 3 years as the outcome. Any differences between the associations with mortality at 3 and 5 years were reported.
Interactions between age and depression, and between age and antidepressants, were tested. Where a significant interaction was observed, the models' results for the main effects and for the interactions were reported separately.
Standard protocol approvals, registrations, and patient consents.
Patients or their relatives gave written informed consent to the SLSR fieldworkers at the moment of registration. The ethics committees of Guy's and St. Thomas' Hospital National Health Service Foundation Trust, King's College Hospital Foundation, National Hospital for Nervous Diseases, Queen's Square Hospital, St. George's Hospital, and Westminster Hospital approved the study.
RESULTS
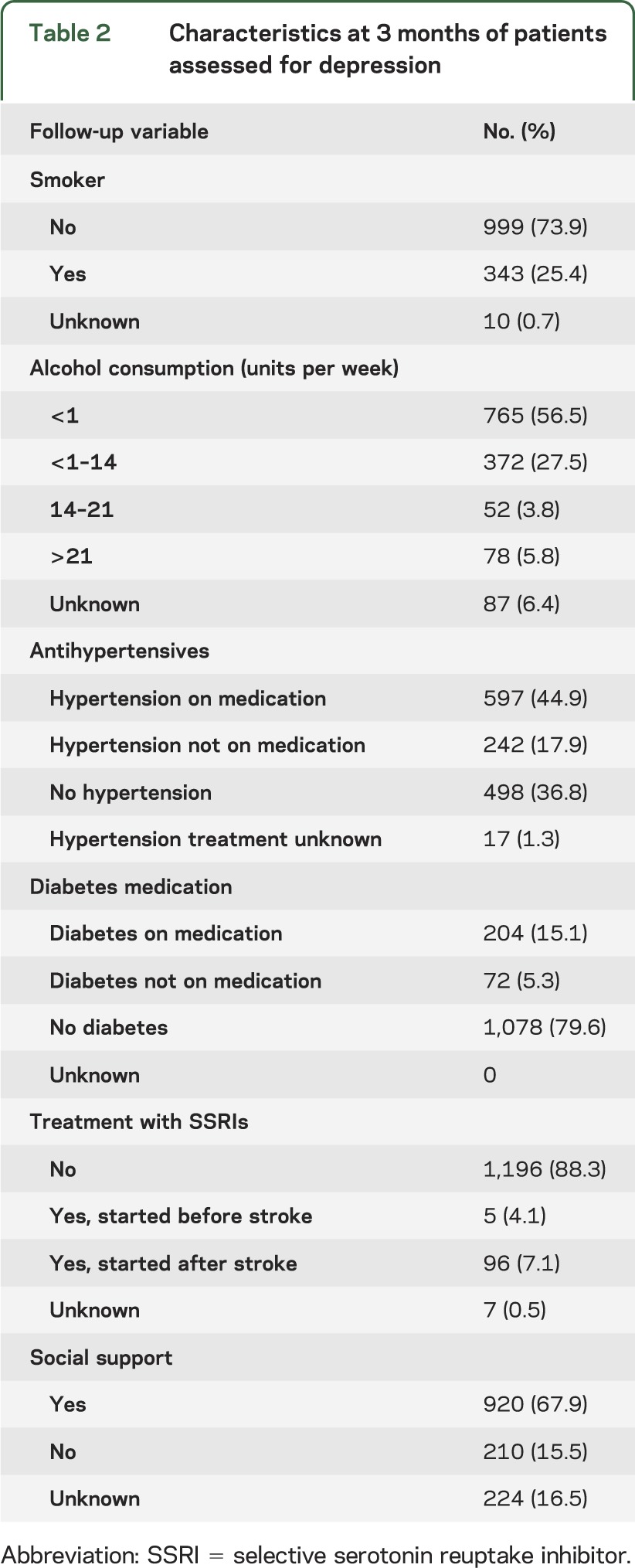
Of the 3,722 patients recruited by the SLSR between 1998 and 2012, 1,068 (28.7%) died before the 3-month assessment and 956 (25.7%) were lost to follow-up at 3 months. Among the 1,698 (45.6%) patients who were followed up, 1,354 (79.7%) were able to complete the HADS, 435 (32.1%) of them were categorized as depressed, and 331 (24.4%) had died within 5 years. A total of 25 (5.7%) of the patients with depression were taking SSRIs at the time of stroke, 67 (15.4%) started taking them after stroke, and 132 (30.3%) died within 5 years of stroke. The prevalence of depression was not significantly different by age (<65/≥65) or sex categories. The baseline and follow-up characteristics of these patients are presented in tables 1 and 2.
Table 1.
Baseline characteristics of patients assessed for depression at 3 months
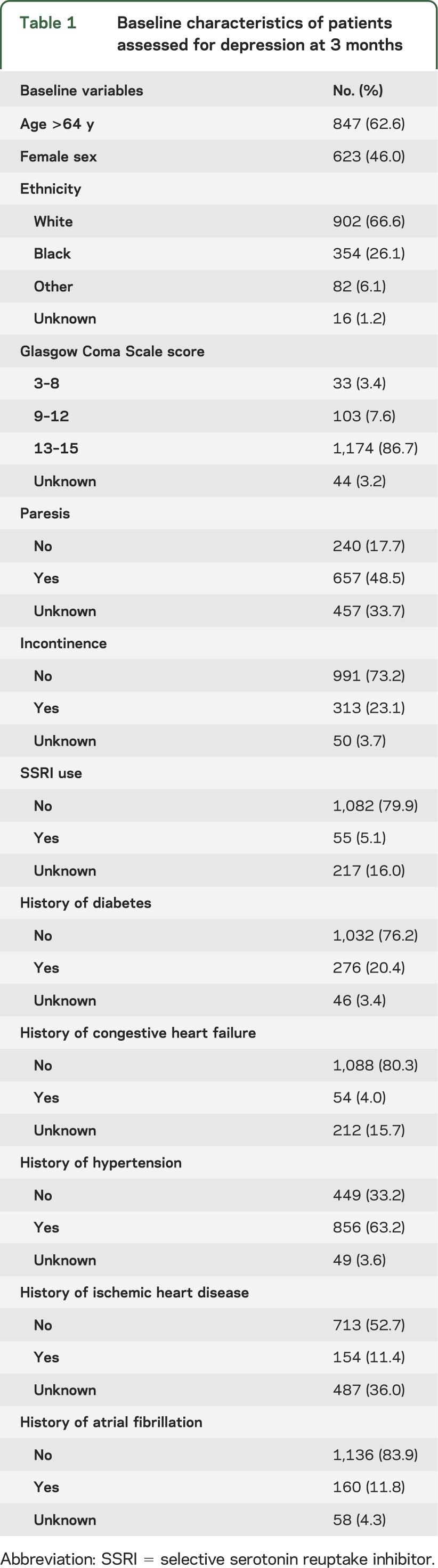
Table 2.
Characteristics at 3 months of patients assessed for depression
Subjects with depression showed higher mortality within 5 years (hazard ratio [HR] 1.41 [95% confidence interval (CI) 1.13–1.77]; p = 0.002). A significant interaction between age and depression was observed, and consequently the results were stratified by age. In patients under 65 years of age, the association between depression and mortality was stronger than in those 65 years or over (HR 3.29 [95% CI 1.75–6.19]; p < 0.001). Among patients 65 or over, mortality was still increased, but the difference between those with and without depression was not statistically significant (HR 1.24 [95% CI 0.98–1.59]; p = 0.074) (table 3). Adjustment for comorbidities, smoking and alcohol use, management of hypertension and diabetes, social support, and use of SSRIs did not change the associations between depression and mortality (table 3).
Table 3.
Association between depression 3 months after stroke and mortality at 5 years
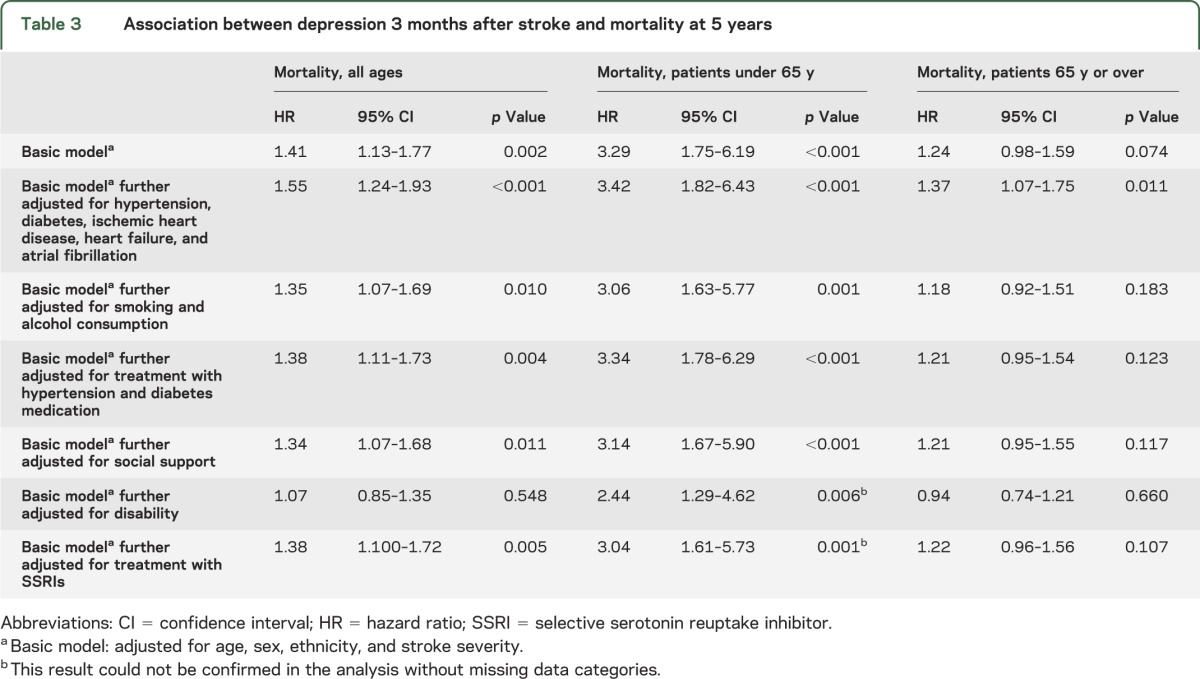
Twenty-one (38.2%) of those on SSRIs at baseline and 36 (37.5%) on SSRIs at 3 months died within 5 years. There was a not significant increase of mortality among those who were on SSRIs before stroke (HR 1.25 [95% CI 0.85–1.83]; p = 0.250). However, SSRIs started after stroke were independently associated with a significant increase in mortality within 5 years of stroke (HR 1.72 [95% CI 1.34–2.20]; p < 0.001). No significant interaction between age and antidepressants was identified.
The analysis without missing data gave estimates that were consistent with the ones obtained with missing data categories. There were 2 exceptions: in patients under 65, the association between depression and mortality when adjusting for disability, and when adjusting for SSRI use at 3 months, became not significant in the analysis without missing data. The analysis with mortality at 3 years as an outcome gave results that were consistent with the ones obtained when mortality at 5 years was used.
DISCUSSION
Depression is associated with an increased mortality in the long term after stroke and this association is stronger among younger stroke survivors. Comorbidities, smoking and alcohol intake, management of hypertension and diabetes, disability, social support, and treatment with SSRIs do not affect the association between depression and mortality. SSRIs started after stroke were independently associated with higher mortality up to 5 years after the acute event.
This study has strengths and limitations. One limitation is the loss to follow-up, associated with stroke cohort studies of elderly survivors. Part of the missing data were due to the inability of some patients with cognitive or communication impairment to respond to the follow-up questionnaires. The regression analysis with and without categories for missing data suggests that while some sociodemographic groups are more likely to be missing than others, this had little impact when analyzing the association between depression and mortality. The SLSR is a large population-based cohort of stroke patients with long-term follow-up. It provides the least biased sampling frame, and good statistical power, allowing for an in-depth investigation of the nature of the association between depression and mortality in the long term after stroke. The assessment of depression with a screening scale instead of a diagnostic tool may represent a limitation. A recent review suggested that another depression scale could be more accurate than HADS. However, the authors of this review also reported that further research is needed to confirm the optimal tool for identifying depression after a stroke since a limited number of heterogeneous studies are available.17 This study did not take prestroke depression into account, which can increase subsequent stroke mortality.7 Nonetheless, prestroke depression also predicts depression after stroke,21 which may be what leads to higher mortality in the long term after stroke. Some studies have investigated the association between depression and mortality in patients with other conditions,5,6,8–11 and another one focused on depression-executive-dysfunction syndrome to explain the association between depression and mortality after stroke.22 One strength of this study, adding to the evidence presented by previous literature, is the observation of a range of clinical and social explanatory factors for the association between depression and long-term mortality after stroke. Social support was measured with a single not validated question. Even though this question has been used before, giving plausible results,23,24 it would have been better to have a validated and more accurate measure for social support.
The onset of depression at an older age may be associated with a lower rate of relapse and better response to treatment and this may explain the different association between depression and mortality in each age category.8
The association between depression and higher mortality is independent of the medical factors analyzed in this article. Other factors, including the neurologic, sociologic, psychological, endocrine, immunologic, and inflammatory disorders observed in depressed patients,6,7 may be more explanatory of the association between depression and mortality after stroke. Unmeasured case mix variables could also be affecting part of these findings. It may also be that the association between depression and mortality is multifactorial and no individual factor can explain it completely.
The association between SSRIs and increased mortality may be explained because patients who take SSRIs have more severe depression.7,10 An alternative explanation could be that the use of SSRIs at 3 months is associated with depression shortly after stroke, which is strongly associated with recurrent episodes of depression that may increase mortality in the long term.4,24 Another possibility is that SSRIs have side effects that increase mortality in the long term. Antidepressants have been shown to improve mood in patients with physical diseases and specifically in stroke patients.25,26 However, previous studies on the nonpsychological effects of antidepressants report contradictory results. There are 2 systematic reviews reporting an association between SSRIs and a reduced mortality of patients with acute cardiovascular events,27 and a limited but significant improvement in dependence, disability, and neurologic impairment in the first few years after stroke.28 Most studies included in these reviews had short follow-up; therefore, the long-term negative effects of SSRIs may not have been observed. A large cohort study observing more than 60,000 primary care patients in the United Kingdom reported that SSRIs were associated with increased risk of falls, strokes, ischemic heart disease, self-harm, fractures, and all-cause mortality.13 The association between SSRIs and mortality may also be affected by the time in which the medication is taken. While our results show that SSRI use after stroke is associated with mortality in the long term, another study found an association between prestroke SSRI use and increased mortality within a year of the acute event.29 While SSRIs may be a useful tool in the management of stroke, their safety in the long term needs further research.
Clinicians should consider the poorer prognosis of stroke survivors with depression, particularly if they are young, acknowledging that no individual medical factor can explain this association. Further studies could address the association between depression and specific causes of death such as cardiovascular disease. The significantly increased mortality among those who take SSRIs should also be considered when managing depression in stroke survivors. Depression and its associated outcomes require periodic clinical assessment as well as effective and safe interventions in the long term after stroke.
Supplementary Material
GLOSSARY
- CI
confidence interval
- GCS
Glasgow Coma Scale score
- HADS
Hospital Anxiety and Depression Scale
- HR
hazard ratio
- SLSR
South London Stroke Register
- SSRI
selective serotonin reuptake inhibitor
Footnotes
Editorial, page 1998
AUTHOR CONTRIBUTIONS
C.D.A.W. and A.G.R. secured the funding. L.A., S.A., S.L.C., C.D.A.W., and A.G.R. designed the study. L.A. collected part of the data. L.A., S.A., and S.L.C. conducted the analysis. L.A., S.A., S.C., C.D.A.W., and A.G.R. cowrote the paper.
STUDY FUNDING
Funded by Guy's and St Thomas' Hospital Charity, The Stroke Association, Department of Health HQIP Grant, UK, and National Institute for Health Research Programme Grant (RP-PG-0407-10184). C.D.A.W. acknowledges financial support from the Department of Health via the National Institute for Health Research (NIHR) Biomedical Research Centre award to Guy's & St Thomas' NHS Foundation Trust in partnership with King's College London. C.D.A.W. is an NIHR Senior Investigator. This article presents independent research commissioned by the NIHR under its Programme Grants for Applied Research funding scheme (RP-PG-0407-10184). The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke 2005;36:1330–1340. [DOI] [PubMed] [Google Scholar]
- 2.Ayerbe L, Ayis S, Crichton S, Wolfe CD, Rudd AG. The natural history of depression up to 15 years after stroke: the South London Stroke Register. Stroke 2013;44:1105–1110. [DOI] [PubMed] [Google Scholar]
- 3.Hackett ML, Anderson CS. Predictors of depression after stroke: a systematic review of observational studies. Stroke 2005;36:2296–2301. [DOI] [PubMed] [Google Scholar]
- 4.Ayerbe L, Ayis S, Crichton S, Wolfe CD, Rudd AG. The long-term outcomes of depression up to 10 years after stroke: the South London Stroke Register. J Neurol Neurosurg Psychiatry 2014;85:514–521. [DOI] [PubMed] [Google Scholar]
- 5.Kamphuis MH, Geerlings MI, Giampaoli S, Nissinen A, Grobbee DE, Kromhout D. The association of depression with cardiovascular mortality is partly explained by health status: The FINE Study. J Affect Disord 2009;114:184–192. [DOI] [PubMed] [Google Scholar]
- 6.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999;99:2192–2217. [DOI] [PubMed] [Google Scholar]
- 7.Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA 2011;306:1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell AJ, Izquierdo de Santiago A. Prognosis of depression in the elderly in comparison with adult age: is there a significant clinical difference? [in Spanish]. Actas Esp Psiquiatr 2009;37:289–296. [PubMed] [Google Scholar]
- 9.Rapp MA, Gerstorf D, Helmchen H, Smith J. Depression predicts mortality in the young old, but not in the oldest old: results from the Berlin Aging Study. Am J Geriatr Psychiatry 2008;16:844–852. [DOI] [PubMed] [Google Scholar]
- 10.Zuluaga MC, Guallar-Castillon P, Rodriguez-Pascual C, Conde-Herrera M, Conthe P, Rodriguez-Artalejo F. Mechanisms of the association between depressive symptoms and long-term mortality in heart failure. Am Heart J 2010;159:231–237. [DOI] [PubMed] [Google Scholar]
- 11.Ye S, Muntner P, Shimbo D, et al. Behavioral mechanisms, elevated depressive symptoms, and the risk for myocardial infarction or death in individuals with coronary heart disease: the REGARDS (Reason for Geographic and Racial Differences in Stroke) study. J Am Coll Cardiol 2013;61:622–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bartoli F, Lillia N, Lax A, et al. Depression after stroke and risk of mortality: a systematic review and meta-analysis. Stroke Res Treat 2013;2013:862978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 2011;343:d4551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gallo V, Egger M, McCormack V, et al. Strengthening the Reporting of Observational Studies in Epidemiology–Molecular Epidemiology (STROBE-ME): an extension of the STROBE Statement. PLoS Med 2011;8:e1001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heuschmann PU, Grieve AP, Toschke AM, Rudd AG, Wolfe CD. Ethnic group disparities in 10-year trends in stroke incidence and vascular risk factors: the South London Stroke Register (SLSR). Stroke 2008;39:2204–2210. [DOI] [PubMed] [Google Scholar]
- 16.Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 1976;54:541–553. [PMC free article] [PubMed] [Google Scholar]
- 17.Meader N, Moe-Byrne T, Llewellyn A, Mitchell AJ. Screening for poststroke major depression: a meta-analysis of diagnostic validity studies. J Neurol Neurosurg Psychiatry 2014;85:198–206. [DOI] [PubMed] [Google Scholar]
- 18.Aben I, Verhey F, Lousberg R, Lodder J, Honig A. Validity of the Beck Depression Inventory, Hospital Anxiety and Depression Scale, SCL-90, and Hamilton Depression Rating Scale as screening instruments for depression in stroke patients. Psychosomatics 2002;43:386–393. [DOI] [PubMed] [Google Scholar]
- 19.Wolfe CD, Taub NA, Woodrow EJ, Burney PG. Assessment of scales of disability and handicap for stroke patients. Stroke 1991;22:1242–1244. [DOI] [PubMed] [Google Scholar]
- 20.UK Government. Office for National Statistics. Available at: www.statistics.gov.uk. Accessed December 20, 2013. [Google Scholar]
- 21.Ayerbe L, Ayis S, Wolfe CD, Rudd AG. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry 2013;202:14–21. [DOI] [PubMed] [Google Scholar]
- 22.Melkas S, Vataja R, Oksala NK, et al. Depression-executive dysfunction syndrome relates to poor poststroke survival. Am J Geriatr Psychiatry 2010;18:1007–1016. [DOI] [PubMed] [Google Scholar]
- 23.Harari D, Coshall C, Rudd AG, Wolfe CD. New-onset fecal incontinence after stroke: prevalence, natural history, risk factors, and impact. Stroke 2003;34:144–150. [DOI] [PubMed] [Google Scholar]
- 24.Ayerbe L, Ayis S, Rudd AG, Heuschmann PU, Wolfe CD. Natural history, predictors, and associations of depression 5 years after stroke: the South London Stroke Register. Stroke 2011;42:1907–1911. [DOI] [PubMed] [Google Scholar]
- 25.Rayner L, Price A, Evans A, Valsraj K, Higginson IJ, Hotopf M. Antidepressants for depression in physically ill people. Cochrane Database Syst Rev 2010;3:Cd007503. [DOI] [PubMed] [Google Scholar]
- 26.Hackett ML, Anderson CS, House A, Xia J. Interventions for treating depression after stroke. Cochrane Database Syst Rev 2008;4:Cd003437. [DOI] [PubMed] [Google Scholar]
- 27.Pizzi C, Rutjes AW, Costa GM, Fontana F, Mezzetti A, Manzoli L. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am J Cardiol 2011;107:972–979. [DOI] [PubMed] [Google Scholar]
- 28.Mead GE, Hsieh CF, Lee R, et al. Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery. Cochrane Database Syst Rev 2012;11:Cd009286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ried LD, Jia H, Feng H, et al. Selective serotonin reuptake inhibitor treatment and depression are associated with poststroke mortality. Ann Pharmacother 2011;45:888–897. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


