Sir,
Urticaria is a disease characterized by development of wheals (hives), angioedema, or both. This needs to be differentiated from wheals caused by skin prick test, anaphylaxis autoinflammatory syndromes, and hereditary angioedema. Acute spontaneous urticaria is defined as spontaneous wheals of less than 6 weeks’ duration. Acute urticaria is often treated with antihistamines, steroids, and topical anti pruritic lotions.
The aim of our study was to evaluate the efficacy of an additional 5-day course of oral prednisolone when compared with levocetirizine alone in the management of acute urticaria.
Inclusion criteria were adults more than 17 years, present urticarial episode of less than 5 days duration, and active urticarial lesions at the time of presentation. Exclusion criteria were history of chronic urticaria or dermographism, children, wheezing or fever, pregnancy and lactation, use of antihistamines or oral corticosteroids within 5 days of first consultation, history of diabetes, hypertension or active peptic ulcer disease, and refusal of informed consent.
This was randomized single blind non-cross-over study at the teaching hospital. Patients were randomized into two groups. The first group received levocetirizine (5 mg) twice a day and prednisolone (10-20 mg) twice a day for the first 5 days. Prednisolone was given in the dose of 0.3 mg/kg body weight. The second group received only levocetirizine 5 mg twice a day. Levocetirizine was continued for 6 weeks in both the groups. Detailed history with complete physical examination was done in all the patients. Urticaria Activity Score (UAS) was calculated on days 0, 2, and 5 of treatment.
The UAS measures two symptoms – number of wheals and intensity of itching – each on a 0-3 scale each day. The UAS was recorded by each patient daily and was obtained from the patients weekly. The number of wheals was scored from 0 to 3 where 0 – no wheals; 1 – less than 20 wheals; 2 – 20-50 wheals; 3 – >50 wheals almost covered large confluent areas of wheals. Severity of itch was scored as 0 – none; 1 – mild; 2 – moderate; and 3 – severe. One has to add both of these scores, namely for both the number of wheals and the severity of itch, on a given day for each of the days in a given week to get the weekly UAS. The average daily UAS thereby ranged from 0 to 6.[1]
Results were as follows [Table 1].
Table 1.
Demographic classification of patients
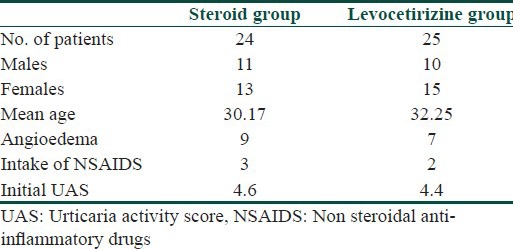
Total 49 (21 males and 28 females, mean age 31.21 years) patients were recruited over a 9-month period from January 2013 to September 2013. UAS was 4.6 and 4.4 in both the groups at the time of presentation. The UAS score came down in both the groups but more in the steroid group than in levocetirizine group [Table 2]. Complete blood count showed anemia in two patients.
Table 2.
UAS Scores in two groups
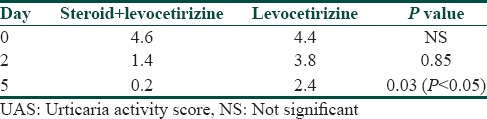
A paired t-test was used to analzse statistical significance. At day 5 UAS came down to 0.2 in the steroid group and 2.4 in the levocetirizine group. This difference was statistically significant (P-value less than 0.5). At the end of 6 weeks three patients from the steroid group and eight patients from the levocetirizine group continued to get hives. Side effects were noted in the steroid group in form gastro-intestinal side effects in three patients and sedation in 2 patients. The levocetirizine group had sedation as a side effect in two patients.
Antihistamines are drug of choice in acute urticaria. However they are relatively slow acting. The anti-inflammatory effect of steroids helps in faster relief of symptoms.
Steroids when added with antihistamines may reduce symptoms faster in acute urticaria and induce quick remission. In our study, UAS was significantly less in the steroid group at the end of 5 days. Also control of symptoms was better in the steroid group as evidenced by the UAS. At the end of 6 weeks, there were fewer active patients in the steroid group.
Studies were conducted to evaluate the efficacy of prednisolone when added with antihistamines for the management of acute urticaria and found that addition of prednisolone improved symptoms and clinical response of the patients.[2,3]
Limitations of our study were as follows: cause of urticaria was not identified; the study was single blinded with limited number of patients. Thus we feel that adding steroids in the initial phase, unless there are known contraindications, would improve symptoms faster and improve the overall quality of life.
References
- 1.Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau A, et al. Dermatology Section of the European Academy of Allergology and Clinical Immunology; Global Allergy and Asthma European Network; European Dermatology Forum; World Allergy Organization. EAACI/GA (2) LEN/EDF/WAO guideline: Definition, classification and diagnosis of urticaria. Allergy. 2009;64:1417–26. doi: 10.1111/j.1398-9995.2009.02179.x. [DOI] [PubMed] [Google Scholar]
- 2.Pollack CV, Jr, Romano TJ. Outpatient management of acute urticaria: The role of prednisone. Ann Emerg Med. 1995;26:547–51. doi: 10.1016/s0196-0644(95)70002-1. [DOI] [PubMed] [Google Scholar]
- 3.Zuberbier T, Iffländer J, Semmler C, Henz BM. Acute urticaria: Clinical aspects and therapeutic responsiveness. Acta Derm Venereol. 1996;76:295–7. doi: 10.2340/0001555576295297. [DOI] [PubMed] [Google Scholar]


