Sir,
Transient acantholytic dermatosis (Grover's disease) was first described as a distinct entity in 1970 by Grover.[1] It usually occurs in middle-aged and elderly people as a discrete pruritic, papular or papulo-vesicular eruption favoring the trunk. The eruption may persist in some patients and the term “papular acantholytic dermatosis” is a preferred term to describe this entity. Heat and sweating are known predisposing factors and leakage of sweat from blocked acrosyringeal ducts may be a contributory factor.[2] However, a contrary viewpoint has been expressed based on finding of more cases during the winters and it has been suggested that Grover's disease is not caused by sweating and heat, but occurs in individuals with a xerotic epidermis with decreased sweat production and is likely to be related to impaired epidermal integrity.[3]
Histologically, it shows focal acantholysis with or without dyskeratosis, which may resemble Darier's disease, pemphigus or Hailey-Hailey disease.[4] A spongiotic variant with some acantholysis within spongiotic foci in the epidermis is another presentation of Grover's disease.[5] Rare cases where the acantholysis was restricted to the acrosyringium have been described.[6,7] The acantholysis in Grover's disease is often focal and may be missed unless several sections are examined.[8]
Although Grover's disease has been commonly reported in the western literature, it seems to be distinctly uncommon in the Indian subcontinent and we could find no reports of Grover's disease in Indian journals devoted to dermatology. A single case report describing Grover's disease in a 22-year-old Nepali man has been published.[9] The only Indian case report of transient acantholytic dermatosis that we could find was of a 55-year-old man with pemphigus foliaceous who developed transient keratotic papules with Darier's disease like histology and which cleared spontaneously in 15 days without treatment.[10]
A 48-year-old male shopkeeper presented with sudden onset of innumerable small (2-3 mm) pruritic erythematous papules with an eroded surface restricted to the abdomen and flanks. At places the lesions had a linear configuration, but mostly were discrete and equally spaced from one another. While few lesions appeared to be related to hair follicles most papules were non-follicular in location [Figures 1 and 2]. There was no history of prolonged exposure to heat or excessive sweating. There was no history of similar eruption in the past nor was there any family history of similar complaints. The eruption had been present for about 1 week before he sought medical treatment as the pruritus and burning sensation were distressing; although, no new lesions were developing.
Figure 1.

Numerous discrete erythematous tiny papules on left side of abdomen
Figure 2.

Lesions on right side of abdomen, some arranged in linear array
A punch biopsy taken from one of the erythematous eroded papules showed acrosyringeal acantholysis and dyskeratosis, which was seen in a concentric fashion involving acrosyringeal keratinocytes at the mid spinous level. There was partial separation of the acrosyringeal keratinocytes with few dyskeratotic cells with pyknotic nuclei and pink cytoplasm [Figures 3–5]. The adjacent epidermis was mildly hyperplastic and showed mild spongiosis with a thickened basket weave horny layer containing occasional parakeratosis [Figure 6]. The upper dermis was mildly edematous and had a moderately dense perivascular infiltrate of lymphocytes and few extravasated erythrocytes.
Figure 3.

Low power view showing acrosyringium at left side of section, hyperplastic epidermis, perivascular lymphocytic infiltrate in dermis. H and E, ×40
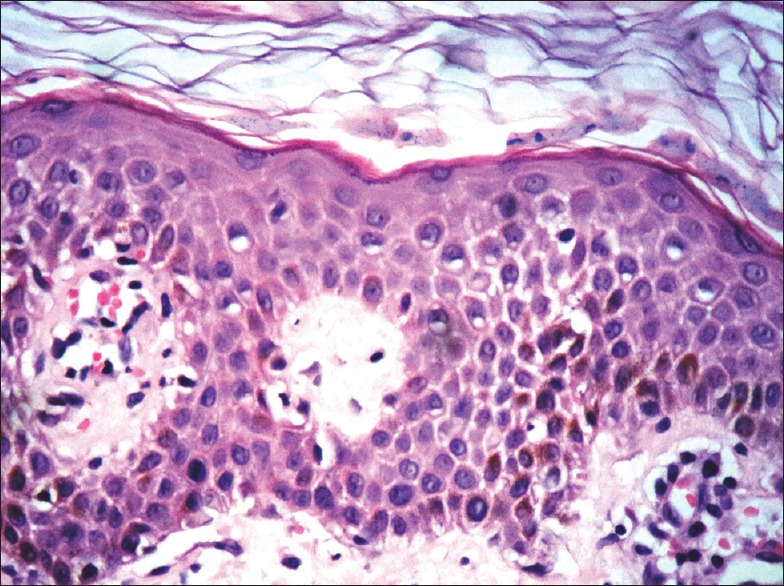
Figure 5.

High power view showing dyskeratotic cells with pyknotic nuclei, partially separated acantholytic acrosyringeal cells. H and E, ×400
Figure 6.
Hyperplastic epidermis with mild spongiosis, few extravasated erythrocytes and some parakeratosis. H and E, ×400
Figure 4.

Medium power view showing acrosyringium with acantholysis and dyskeratosis affecting the acrosyringeal keratinocytes at the mid spinous level. H and E, ×100
Based on the clinical presentation of discrete severely pruritic erythematous eroded papules on the trunk and focal acrosyringeal acantholysis on histology a diagnosis of Sudoriferous acrosyringeal acantholytic variant of Grover's disease was made and the patient was started on capsule doxycycline 100 mg twice daily, topical beclomethasone cream and oral levocetirizine 5 mg twice daily for the pruritus.
On follow-up at 2 weeks, there was satisfactory improvement in the pruritus and the rash had subsided by 25%. Continuation of the medication was advised for another 2 weeks, but the patient was lost to further follow-up.
Grover's disease appears to be distinctly uncommon in India as we could not find any case reports published in Indian journals. It may be an under-recognized entity, especially because the histological picture can be very variable and biopsy may not reveal the pathological findings unless several sections are examined. Our case fits in very well with the clinical description of Grover's disease with innumerable discrete erythematous pruritic eroded papules on the trunk in a middle-aged man. The histological picture of acrosyringeal acantholysis is very rare with only six cases described in world literature.[5,6]
We report this case to draw attention to this uncommon condition, which has received very little attention in Indian dermatological literature. Given our hot and humid climate, it may not be unreasonable to expect that cases of Grover's disease are missed due to lack of awareness of this entity or inability to demonstrate the typical histological findings associated with Grover's disease.
References
- 1.Grover RW. Transient acantholytic dermatosis. Arch Dermatol. 1970;101:426–34. [PubMed] [Google Scholar]
- 2.Hu CH, Michel B, Farber EM. Transient acantholytic dermatosis (Grover's disease).A skin disorder related to heat and sweating. Arch Dermatol. 1985;121:1439–41. [PubMed] [Google Scholar]
- 3.Scheinfeld N, Mones J. Seasonal variation of transient acantholytic dyskeratosis (Grover's disease) J Am Acad Dermatol. 2006;55:263–8. doi: 10.1016/j.jaad.2006.01.029. [DOI] [PubMed] [Google Scholar]
- 4.Chalet M, Grover R, Ackerman AB. Transient acantholytic dermatosis: A reevaluation. Arch Dermatol. 1977;113:431–5. [PubMed] [Google Scholar]
- 5.Davis MD, Dinneen AM, Landa N, Gibson LE. Grover's disease: Clinicopathologic review of 72 cases. Mayo Clin Proc. 1999;74:229–34. doi: 10.4065/74.3.229. [DOI] [PubMed] [Google Scholar]
- 6.Hashimoto K, Moiin A, Chang MW, Tada J. Sudoriferous acrosyringeal acantholytic disease. A subset of Grover's disease. J Cutan Pathol. 1996;23:151–64. doi: 10.1111/j.1600-0560.1996.tb01289.x. [DOI] [PubMed] [Google Scholar]
- 7.Antley CM, Carrington PR, Mrak RE, Smoller BR. Grover's disease (transient acantholytic dermatosis): Relationship of acantholysis to acrosyringia. J Cutan Pathol. 1998;25:545–9. doi: 10.1111/j.1600-0560.1998.tb01738.x. [DOI] [PubMed] [Google Scholar]
- 8.Fernández-Figueras MT, Puig L, Cannata P, Cuatrecases M, Quer A, Ferrándiz C, et al. Grover disease: A reappraisal of histopathological diagnostic criteria in 120 cases. Am J Dermatopathol. 2010;32:541–9. doi: 10.1097/DAD.0b013e3181c80cf9. [DOI] [PubMed] [Google Scholar]
- 9.Dwari BC, Ghosh A, Bajracharya S, Gupta S, Chaudhary N. Transient acantholytic dermatosis (Grover's disease): A case report. J Pak Assoc Dermatologists. 2007;17:112–5. [Google Scholar]
- 10.Manjare AK, Ghate SS, Jerajani HR. Transient acantholytic dermatos is associated with pemphigus foliaceus. Int J Dermatol. 2012;51:1389–91. doi: 10.1111/j.1365-4632.2010.04762.x. [DOI] [PubMed] [Google Scholar]


