Abstract
Background:
Oral isotretinoin treatment might influence the levels of vitamin B12 and folic acid.
Aims and Objectives:
The aim of this study is to compare vitamin B12 and folic acid levels in patients with moderate and severe acne vulgaris with those of the healthy control group and to investigate the effect of isotretinoin treatment on these vitamins.
Materials and Methods:
Patients who completed 6 months of isotretinoin therapy for moderate and severe forms of acne vulgaris and a control group consisting of healthy individuals between February 2011 and March 2012 were included in the study. Before isotretinoin therapy and at 6.- months of the therapy, serum vitamin B12 and folic acid levels were measured. In the healthy control group, vitamin B12 and folic acid levels were assessed only once.
Results:
In total, 120 patients with moderate and severe acne vulgaris who completed 6 months isotretinoin therapy and 100 healthy individuals who constituted the control group were included in the study. Pre-treatment vitamin B12 values of the patient group were found to be statistically significantly higher (P = 0.002), but any statistically significant difference was not detected in folic acid measurements (P = 0.566). A statistically significant decrease was detected in post-treatment vitamin B12 and folic acid levels (P < 0.05).
Conclusion:
Vitamin B12/folic acid treatment should be given under medical surveillance before and during isotretinoin therapy. Supplementation of these vitamins should be recommended in cases of their deficiency, so as to decrease the risks of neuropsychiatric and occlusive vascular diseases.
Keywords: Acne, folic acid, isotretinoin, vitamin B12
Introduction
What was known?
Vitamin B12 and folic acid, with their interrelated metabolism, are important vitamins for the maintenance of various metabolic pathways in the body.
Various vitamin supplements, most prominently vitamin B12, could exacerbate existing acne and/or cause the development of acneiform eruptions.
Recent studies have suggested that isotretinoin might influence the metabolism of vitamin B12 and folic acid.
Acne vulgaris is the most prevalent skin disease, affecting 83-95% of the adolescent population.[1] For many years, the relationship between diet and acne has been investigated. More rapid development of acne in individuals consuming a diet with a higher glycemic index has been suggested.[2,3] It has also been reported that various vitamin supplements, most prominently vitamin B12 (cyanocobalamin), could exacerbate existing acne and/or cause the development of acneiform eruptions.[1,4,5] However, recent studies have demonstrated that oral isotretinoin (ISO) treatment, which is effective against the major etiological factors involved in the pathogenesis of acne, might lead to decreases in the levels of vitamin B12 and folic acid.[6,7] Thus, contrary opinions regarding the need for vitamin supplements in patients on ISO treatment have been proposed.[7]
Vitamin B12 and folic acid, with their interrelated metabolism, are important for the maintenance of various metabolic pathways in the body. In cases of deficiency, adverse effects on cardiovascular, neurological, psychological, hematological, gastrointestinal, locomotor (musculoskeletal) and immunological systems may occur.[8]
In this study, vitamin B12 and folic acid levels in patients with moderate and severe acne vulgaris were compared with those of a healthy control group and the effects of ISO treatment on these vitamins were investigated.
Materials and Methods
Study design
In this study, we prospectively followed 175 patients who underwent isotretinoin treatment for 6 months between February 2011 and March 2012 for moderate (Grade 2) or severe (Grade 3-4) acne vulgaris. Our control group was consisting of 100 healthy individuals during the same time period. Patients were consecutively selected. Among the patient group, 120 patients who completed 6 months of ISO therapy were included in the statistical analysis. Pregnant women, nursing women, smokers, patients with migraine, hyperlipidemia, hypervitaminosis A and systemic diseases (hepatic and renal insufficiency, hypertension and metabolic disease) were excluded. Patients using any medication or vitamin supplement were also excluded. Patients were started on ISO therapy at daily doses of 0.6-1 mg/kg and titrated over 6 months to a cumulative dose of at least 120 mg/kg. In the patient and control groups, blood samples were drawn into blank tubes and then tubes with ethylenediaminetetraacetic acid. Routine biochemical parameters were measured using an autoanalyzer (Abbott c8000), vitamin B12 and folic acid levels were assessed using a direct chemiluminescence method and for the evaluation of hematological parameters, a blood cell counter system (Abbott cell dyn 3700) was used. Before ISO therapy and at 6 months of therapy, liver function tests and hemograms were evaluated and serum lipid, vitamin B12 and folic acid levels were measured. In the healthy control group, vitamin B12 and folic acid levels were assessed only once.
Statistical analysis
The SPSS (Statistical Package for Social Sciences) software (version 16 for Windows) was used. For descriptive statistical analyses, median, minimal and maximal values were used. Our data does not show normal distribution. Thus, non-parametric tests are performed, using only median values. For comparisons of the patient and control groups, for numerical values, the Mann-Whitney U-test and for categorical variables, Chi-squared tests were used. For the comparison of measurements obtained before and after treatment, the Wilcoxon test was used. P = 5% was accepted as the cut-off value for statistical significance.
Results
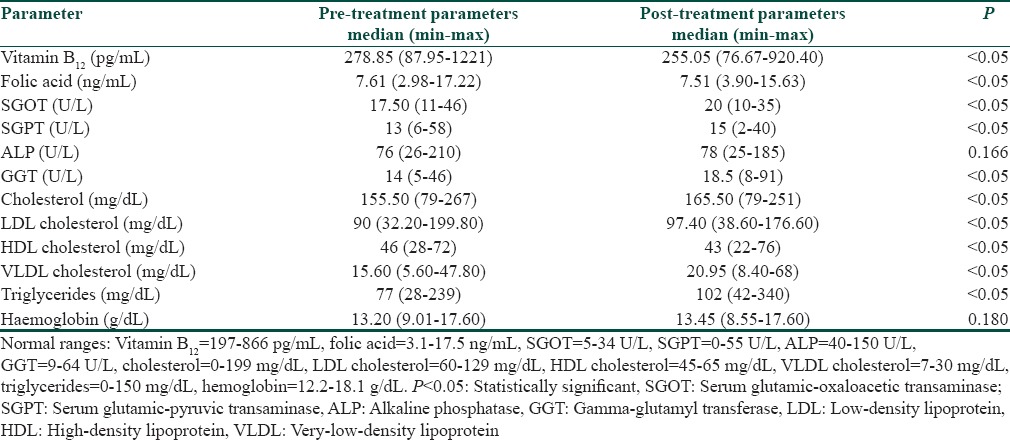
In total, 120 patients (98 women, 22 men; mean age, 20 years; age range, 18-40 years) with moderate and severe acne vulgaris who completed 6 months of ISO therapy and 100 healthy individuals (79 women, 21 men; mean age, 21 years; age range, 18-40 years), who constituted the control group, were included in the study. No statistically significant difference was detected between the patient and healthy control groups in terms of age or gender of the patients (P > 0.05). Pre-treatment vitamin B12 values in the patient group were statistically significantly higher (P < 0.05), but no statistically significant difference was detected in folic acid levels (P = 0.566) [Table 1]. Pre- and post-treatment vitamin B12, folic acid, biochemical parameters and hemoglobin values were compared [Table 2]. A statistically significant decrease was detected in post-treatment vitamin B12 and folic acid levels while a statistically significant increase was noted in post-treatment levels of aspartate aminotransferase, alanine aminotransferase, gamma-glutamyl transferase (GGT), total cholesterol, triglyceride, low-density lipoprotein (LDL) and very LDL (VLDL) (P < 0.05). Significant decreases in post-treatment high-density lipoprotein levels were detected (P < 0.05) while no statistically significant difference in alkaline phosphatase (P = 0.166) or hemoglobin level (P = 0.180) was observed.
Table 1.
Comparison of pre-treatment vitamin B12 and folic acid values
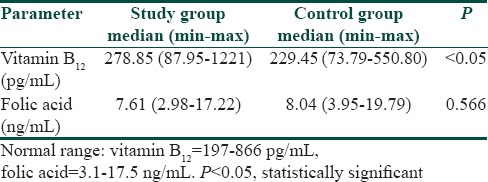
Table 2.
Comparison of pre- and post-treatment biochemical parameters
Discussion
In the medical literature, the argument that especially vitamin B12 supplements exacerbate acne vulgaris has been proposed multiple times.[4,5,9] In our study, higher pre-treatment vitamin B12 levels, versus the control group, support the assertion that vitamin B12 plays a role in the etiopathogenesis of acne vulgaris. However, vitamin B12 and folic acid, with their interrelated metabolism, are important vitamins in various metabolic pathways, including the homocysteine (Hcy) pathway. Vitamin B12 and folic acid are cofactors of the methyltransferase enzyme and with their deficiency, hyperhomocysteinemia is seen.[6,7] In recent years, hyperhomocysteinemia has been appreciated as an important risk factor for cardiovascular diseases. The idea that an increased plasma Hcy level is an independent risk factor for endothelial dysfunction and coronary artery disease (CAD) has become a current issue.[10,11] Increased plasma Hcy level is also a risk factor for cerebrovascular and peripheral vascular diseases, in addition to CAD.[12,13,14] Furthermore, vitamin B12, folic acid and related increases in the levels of Hcy have been associated with many neuropsychiatric diseases. These include bipolar disorder, paranoid psychosis, depression, schizophrenia, Alzheimer's disease and Parkinson's disease.[15,16] In addition to these cardiovascular, neurological and psychological effects, Hcy also exerts adverse effects on hematological, gastrointestinal, locomotor (musculoskeletal) and immunological systems.[8]
ISO is an effective treatment agent, used frequently both at present and over the last 15 years, for the treatment of moderate and severe acne patients, especially those 15-24 years of age.[6] Despite its high therapeutic success rates, it also has many side-effects, especially teratogenicity.[17] As recent studies have suggested, ISO influences the metabolism of vitamin B12, folic acid and Hcy.[1,6,7] However, this issue remains controversial. In a study of 28 acne patients, Schulpis et al. demonstrated increased Hcy values after 45 days of ISO therapy, with no statistically significant difference in vitamin B12 or folic acid levels.[18] In another study of 74 acne patients, after 45 days of ISO therapy, no change was observed in vitamin B12 or folic acid levels while Hcy levels increased[19], as was also reported by Schulpis et al.[18] In both of these studies, ISO treatment was cut short and it was suggested that the hyperhomocysteinemia seen during ISO therapy, which developed secondary to hepatic dysfunction, was associated with the inhibition of the cystathionine-β-synthase enzyme.[18] In another study of 20 young and 20 old healthy individuals, Chanson et al. reported that ISO therapy lasting for 28 days decreased folic acid levels without changing Hcy concentrations.[6] From another point of view, ISO may induce decreases in vitamin B12 and folic acid levels, increasing the risk of hyperhomocysteinemia. Indeed, Karadag et al. reported that following 4 months ISO treatment of 66 acne patients, vitamin B12 and folic acid level decreased, while Hcy values increased.[7] This study stressed that long-term ISO therapy caused hepatic dysfunction, followed by vitamin B12 and folic acid deficiencies, due to its cumulative effects, suggesting an important role in Hcy metabolism. Furthermore, many studies have noted that in addition to increasing the lipid profile, hyperhomocysteinemia as a consequence of vitamin B12 and folic acid deficiency might increase the risk of CAD.[7] Therefore, vitamin supplementation has been suggested to prevent any potential deficiency during ISO therapy. However, the mechanism (s) leading to vitamin deficiency during ISO therapy has/have not yet been determined. In our study, 120 patients who received ISO therapy were followed for longer periods (6 months) than in previous reports. In our study, although values were in the normal range, our results were similar to those reported by Karadag et al. and statistically significant decreases in vitamin B12 and folic acid levels were detected. Furthermore, similar to previous studies, compared with baseline values, significant increases in the levels of post-treatment biochemical parameters (serum glutamic-oxaloacetic, serum glutamic-pyruvic transaminase, GGT, cholesterol, LDL, VLDL, triglycerides) were noteworthy.
Vitamin B12 and folic acid deficiencies may also be associated with a number of psychiatric diseases.[16] These diseases resemble the psychological side-effects that are sometimes seen in ISO therapy.[20,21,22,23] Although conclusive information regarding the etiopathogenesis of the psychological side-effects that might emerge during ISO therapy is lacking, the role of retinoic acid receptors and the impact of retinoids that enter the central nervous system on serotonergic neurons, leading to the development of affective disorders, has been suggested.[24] However, in studies of the neuropsychiatric side-effects of ISO, no role of vitamin B12 and folic acid levels has yet been reported. Karadag's investigation and our study have revealed that long-term use of ISO might decrease vitamin B12 and folic acid levels. Although no study of the mechanism by which ISO induces vitamin B12 and folic acid deficiency has yet been reported, we suggest that long-term use of ISO might decrease intestinal absorption of vitamin B12 and folic acid. This should be assessed in future studies.
Conclusions
Systemic retinoids have been used for more than 30 years in the treatment of follicular and keratinisation disorders, ichthyosiform dermatosis, cutaneous neoplasias, various systemic cancers and genetic and acquired immune system diseases.[25] This study demonstrated that after a 6 months treatment, ISO can result in decreases in vitamin B12 and folic acid levels. The failure to identify this effect in short-term studies suggests that the cumulative effect of ISO induces decreases in vitamin levels. Thus, especially in patients receiving more than one course of ISO therapy, vitamin B12/folic acid decreases and related side-effects might be encountered more frequently.
Also, as an outcome of our study, we suggest the following. Because vitamin B12 supplements may cause or exacerbate acne, their unnecessary use should be avoided. Vitamin B12/folic acid treatment should be given under medical surveillance before and during ISO therapy. Supplementation of these vitamins should be recommended in cases of their deficiency, so as to decrease the risks of neuropsychiatric and occlusive vascular diseases. These suggestions are not contradictory, but may also not be fully compatible when evaluated in detail.
What is new?
Higher pre-treatment vitamin B12 levels, versus the control group, support the assertion that vitamin B12 plays a role in the etiopathogenesis of acne vulgaris.
Furthermore, this study demonstrated that after a 6 months treatment, isotretinoin can result in decreases in vitamin B12 and folic acid levels.
Supplementation of vitamin B12/folic acid should be recommended in cases of their deficiency in patients under isotretinoin therapy.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Jasim ZF, McKenna KE. Vitamin B 12 and folate deficiency anaemia associated with isotretinoin treatment for acne. Clin Exp Dermatol. 2006;31:599. doi: 10.1111/j.1365-2230.2006.02144.x. [DOI] [PubMed] [Google Scholar]
- 2.Melnik BC. Diet in acne: Further evidence for the role of nutrient signalling in acne pathogenesis. Acta Derm Venereol. 2012;92:228–31. doi: 10.2340/00015555-1358. [DOI] [PubMed] [Google Scholar]
- 3.Danby FW. Nutrition and acne. Clin Dermatol. 2010;28:598–604. doi: 10.1016/j.clindermatol.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 4.Sherertz EF. Acneiform eruption due to “megadose” vitamins B6 and B12. Cutis. 1991;48:119–20. [PubMed] [Google Scholar]
- 5.Dupré A, Albarel N, Bonafe JL, Christol B, Lassere J. Vitamin B-12 induced acnes. Cutis. 1979;24:210–1. [PubMed] [Google Scholar]
- 6.Chanson A, Cardinault N, Rock E, Martin JF, Souteyrand P, D’Incan M, et al. Decreased plasma folate concentration in young and elderly healthy subjects after a short-term supplementation with isotretinoin. J Eur Acad Dermatol Venereol. 2008;22:94–100. doi: 10.1111/j.1468-3083.2007.02386.x. [DOI] [PubMed] [Google Scholar]
- 7.Karadag AS, Tutal E, Ertugrul DT, Akin KO. Effect of isotretinoin treatment on plasma holotranscobalamin, vitamin B12, folic acid, and homocysteine levels: Non-controlled study. Int J Dermatol. 2011;50:1564–9. doi: 10.1111/j.1365-4632.2011.05027.x. [DOI] [PubMed] [Google Scholar]
- 8.Snow CF. Laboratory diagnosis of vitamin B12 and folate deficiency: A guide for the primary care physician. Arch Intern Med. 1999;159:1289–98. doi: 10.1001/archinte.159.12.1289. [DOI] [PubMed] [Google Scholar]
- 9.Jansen T, Romiti R, Kreuter A, Altmeyer P. Rosacea fulminans triggered by high-dose vitamins B6 and B 12. J Eur Acad Dermatol Venereol. 2001;15:484–5. doi: 10.1046/j.1468-3083.2001.00308.x. [DOI] [PubMed] [Google Scholar]
- 10.Humphrey LL, Fu R, Rogers K, Freeman M, Helfand M. Homocysteine level and coronary heart disease incidence: A systematic review and meta-analysis. Mayo Clin Proc. 2008;83:1203–12. doi: 10.4065/83.11.1203. [DOI] [PubMed] [Google Scholar]
- 11.Kazemi MB, Eshraghian K, Omrani GR, Lankarani KB, Hosseini E. Homocysteine level and coronary artery disease. Angiology. 2006;57:9–14. doi: 10.1177/000331970605700102. [DOI] [PubMed] [Google Scholar]
- 12.Casas JP, Bautista LE, Smeeth L, Sharma P, Hingorani AD. Homocysteine and stroke: Evidence on a causal link from mendelian randomisation. Lancet. 2005;365:224–32. doi: 10.1016/S0140-6736(05)17742-3. [DOI] [PubMed] [Google Scholar]
- 13.Pianka P, Almog Y, Man O, Goldstein M, Sela BA, Loewenstein A. Hyperhomocystinemia in patients with nonarteritic anterior ischemic optic neuropathy, central retinal artery occlusion, and central retinal vein occlusion. Ophthalmology. 2000;107:1588–92. doi: 10.1016/s0161-6420(00)00181-0. [DOI] [PubMed] [Google Scholar]
- 14.Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA. 1995;274:1049–57. doi: 10.1001/jama.1995.03530130055028. [DOI] [PubMed] [Google Scholar]
- 15.Quadri P, Fragiacomo C, Pezzati R, Zanda E, Forloni G, Tettamanti M, et al. Homocysteine, folate, and vitamin B-12 in mild cognitive impairment, Alzheimer disease, and vascular dementia. Am J Clin Nutr. 2004;80:114–22. doi: 10.1093/ajcn/80.1.114. [DOI] [PubMed] [Google Scholar]
- 16.Sen S, Durat G, Atasoy I. Mental and neurological disorders related to vitamin B 12 and folic acid deficiencies. [Turk Klin Biyokimya Derg] 2009;7:31–6. [Google Scholar]
- 17.Zouboulis CC, Piquero-Martin J. Update and future of systemic acne treatment. Dermatology. 2003;206:37–53. doi: 10.1159/000067821. [DOI] [PubMed] [Google Scholar]
- 18.Schulpis KH, Karikas GA, Georgala S, Michas T, Tsakiris S. Elevated plasma homocysteine levels in patients on isotretinoin therapy for cystic acne. Int J Dermatol. 2001;40:33–6. doi: 10.1046/j.1365-4362.2001.00146.x. [DOI] [PubMed] [Google Scholar]
- 19.Polat M, Lenk N, Bingöl S, Oztaş P, Ilhan MN, Artüz F, et al. Plasma homocysteine level is elevated in patients on isotretinoin therapy for cystic acne: A prospective controlled study. J Dermatolog Treat. 2008;19:229–32. doi: 10.1080/09546630701846079. [DOI] [PubMed] [Google Scholar]
- 20.Behnam B, Taheri R, Ghorbani R, Allameh P. Psychological impairments in the patients with acne. Indian J Dermatol. 2013;58:26–9. doi: 10.4103/0019-5154.105281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bachmann C, Grabarkiewicz J, Theisen FM, Remschmidt H. Isotretinoin, depression and suicide ideation in an adolescent boy. Pharmacopsychiatry. 2007;40:128. doi: 10.1055/s-2007-972575. [DOI] [PubMed] [Google Scholar]
- 22.Marqueling AL, Zane LT. Depression and suicidal behavior in acne patients treated with isotretinoin: A systematic review. Semin Cutan Med Surg. 2007;26:210–20. doi: 10.1016/j.sder.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Kaymak Y, Taner E, Taner Y. Comparison of depression, anxiety and life quality in acne vulgaris patients who were treated with either isotretinoin or topical agents. Int J Dermatol. 2009;48:41–6. doi: 10.1111/j.1365-4632.2009.03806.x. [DOI] [PubMed] [Google Scholar]
- 24.O’Reilly KC, Trent S, Bailey SJ, Lane MA. 13-cis-Retinoic acid alters intracellular serotonin, increases 5-HT1A receptor, and serotonin reuptake transporter levels in vitro. Exp Biol Med (Maywood) 2007;232:1195–203. doi: 10.3181/0703-RM-83. [DOI] [PubMed] [Google Scholar]
- 25.Lowenstein EB, Lowenstein EJ. Isotretinoin systemic therapy and the shadow cast upon dermatology's downtrodden hero. Clin Dermatol. 2011;29:652–61. doi: 10.1016/j.clindermatol.2011.08.026. [DOI] [PubMed] [Google Scholar]


