Abstract
Background:
The pathergy test (PT) is important in the diagnosis of Behçet's disease (BD). However, misinterpretation of the test might cause false-positive or false-negative results. Therefore, immunopathologic and histopathologic tests are recommended with PT.
Aims and Objectives:
The aim of this study is to determine histopathologic findings of positive pathergy reaction at BD.
Materials and Methods:
This study was performed on 23 patients with BD. All patients were in active period of the disease. After 48 h from the injection, biopsy was performed on positive pathergy lesions.
Results:
Of the specimen from positive PT lesions of patients with BD, nine revealed mixed type inflammatory cell infiltration (39.1%), two revealed lobular panniculitis without vasculitis (8.7%), two revealed neutrophil rich infiltration (8.7%), and five revealed lymphocyte rich infiltration (21.7%) at the subcutaneous tissue. Mixed type inflammatory cell infiltration (43.4%), endothelial swelling and thickening (17.3%), erythrocyte extravasation (26.0%), perivascular cell infiltration (13.0%), lymphocytic vascular reaction (8.6%), lymphocytic vasculitis (13.0%), and leukocytoclastic vasculitis (21.7%) were detected in dermis by histopathologic examinations. There was no statistically significant difference between histopathologic findings and sex, family history, and systemic involvement except uveitis.
Conclusion:
This is an exceptional study since it is the first study that determines subcutaneous tissue findings of positive pathergy reaction in Behçet patients. In our study, uveitis was found to be statistically significant in the patients who had vasculitis in dermis. It can be a clue for prediction of disease severity and course. Further, studies that include wide number of patients will better illuminate the correlation between subcutaneous tissue findings and disease severity and clinical course.
Keywords: Behçet's disease, histopathologic, subcutaneous
Introduction
What was known?
The pathergy test is important in the diagnosis of Behçet's disease.
Misinterpretation of pathergy test might cause false-positive or false-negative results.
Behçet's disease (BD) is a chronic multisystem disease characterized by oral and genital aphthae; arthritis; cutaneous lesions; and ocular, gastrointestinal, and neurologic manifestations. It was first described by the Turkish dermatologist Hulusi Behçet in 1937 as “recurrent oral aphthous ulcers, genital ulcers and ‘hypopyon-uveitis’”. Unfortunately, there is no specific laboratory test to diagnose BD. All the criteria for BD recognized by the International BD Study Group are based on clinical signs and symptoms, except for the pathergy test (PT).[1,2,3,4] Therefore, PT is important in diagnosis of BD. In the literature, there are a few studies about dermal histopathologic findings of PT.[5,6,7] However, subcutaneous histopathologic findings of PT have never been reported to date.
The aim of this study is to determine histopathologic findings of positive pathergy reaction. In addition, histopathologic evaluation of PT has been compared with clinical evaluation.
Materials and Methods
This study was performed on 23 patients with BD (14 female and nine male), their ages ranged between 18-60 years. BD was diagnosed by using the International Study Group Criteria. All of the Behçet patients were in active period of the disease and had two of the disease symptoms at least. The patients did not use colchicine, steroids, or nonsteroidal antiinflammatory drugs (NSAIDs) for at least 10 days before the test. Disposable/sharp needles of type 20 G No. 1 were used in the tests. Hairless and avascular regions in the flexor parts of both forearms were selected as test regions. The occurrence of erythema without any induration was considered as “negative” and the occurrence of papules and pustules was considered as “positive.” After 48 h from the injection, biopsy was performed on positive pathergy lesions of Behçet's patients for histopathological examination.
Statistical analysis
Results are expressed as mean ± standard deviation (SD) or frequency (%). Chi-square test was used for comparing histopathological findings and P < 0.05 was considered to be statistically significant.
Results
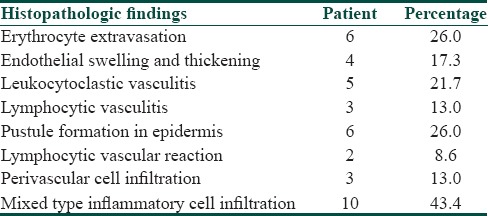
Of the specimen from positive PT lesions of patients with BD, nine revealed mixed type inflammatory cell infiltration (39.1%) [Figure 1], two revealed lobular panniculitis without vasculitis [Figure 2] (8.7%), two revealed neutrophil rich infiltration (8.7%), and five revealed lymphocyte rich infiltration (21.7%) at the subcutaneous tissue. Five revealed normal fat tissue findings (21.7%) [Table 1]. There was no statistically significant difference between subcutaneous tissue findings and sex, family history, and systemic involvement. In dermis, ten (43.4%) revealed mixed type inflammatory cell infiltration, three (13.0%) revealed perivascular cell infiltration, two (8.6%) revealed lymphocytic vascular reaction, four (17.3%) revealed endothelial swelling and thickening, and six (26.0%) revealed erythrocyte extravasation. Six (26.0%) showed pustule formation [Figure 3] in epidermis and five were subcorneal, and one was intraepidermal. Also, eight revealed vasculitis (34.7%) out of which three (13.0%) were lymphocytic vasculitis and five (21.7%) were leukocytoclastic vasculitis [Figure 4 and Table 2]. There was no statistically significant difference between dermal histopathologic findings and sex, family history, and systemic involvement except ocular involvement. Uveitis was found to be statistically significant in the patients who revealed vasculitis (P = 0.012).
Figure 1.

Mixed inflammatory cell infiltration in the dermis (H and E, 20 × 10)
Figure 2.

Lobular panniculitis without vasculitis (H and E, 20 × 10)
Table 1.
Subcutaneous histopathologic findings of positive pathergy test

Figure 3.

Epidermal pustule formation (H and E, 4 × 10)
Figure 4.

Leukocytoclastic vasculitis (H and E, 20 × 10)
Table 2.
Dermal histopathologic findings of positive pathergy test
Discussion
Pathergy is the term used to describe hyperreactivity of skin that occurs in response to minimal trauma.[8] The PT first reported by Blobner[9] is the skin hyperreactivity associated with erythema, papules, or pustules which is induced by intradermal prick in some patients with BD.
The clinical use of PT is very important in the diagnosis of BD. On the other hand, misinterpretation of test might cause false-positive or false-negative results. For that reason, immunopathologic and histopathologic tests are recommended with PT.[5] However, there is also controversy about the histopathology of pathergy reaction. Some authors claim mixed infiltration, while authors report neutrophilic infiltration with leukocytoclastic vasculitis.[10,11,12] A possible explanation for this discrepancy may be the different methods used to induce lesions (needle prick, histamine injection, etc.), variations in biopsy time, and ethnic origin of patient.[10]
The histopathologic result of PT depends on the time of biopsy. In the first 6 h, polymorphonuclear leukocytes are dominant in inflammatory exudate. After 24 h, mononuclear cell infiltration in dermal vessels, edema in vessel endothelium, and edema and leukocytoclasia in reticular dermis are seen.[13,14] Leukocytoclastic vasculitis and neutrophilic vascular reactions also occur after 24 h. Lymphocytic vasculitis and lymphocytic perivascular infiltrations are found later.[10,15,16,17] In histopathology of the PT, presence of vasculitis and neutrophilic vascular reaction are definitive but not a requirement. The perivascular and periadnexal lymphohistiocytic infiltration of varying intensity and their penetration in deep dermis and moderate neutrophilic infiltration in dermis are also important findings.[15]
In our study, mixed type inflammatory cell infiltration, lobular panniculitis without vasculitis, neutrophil rich infiltration, and lymphocyte rich infiltration were found to be the subcutaneous histopathologic findings of positive PT in BD. In the literature; panniculitis, lobular or mixed septal, and lobular in pattern was shown in erythema nodosum-like lesions of BD. Vasculitis was noted in most erythema nodosum-like lesions in BD.[18] In our study, lobular panniculitis observed in two patients; but interestingly, there was evidence of vasculitis. Up to now, although many studies have investigated clinical and histopathologic findings of PT, panniculitis among the histopathologic findings in PT has never been reported.
In our study; mixed type inflammatory cell infiltration, endothelial swelling and thickening, erythrocyte extravasation, perivascular cell infiltration, and lymphocytic vascular reaction were detected in dermis by histopathologic examinations. These findings were consistent with the literature.[5,6,11] Uveitis was found to be statistically significant in patients in whom vasculitis was observed. On the light of this finding, the patients that vasculitis was revealed should be more alert against the development of uveitis.
This is an exceptional study since it is the first study that determines the subcutaneous tissue findings of positive pathergy reaction in Behçet patients. No correlation has been found between histopathologic findings and disease severity and clinical course. Minority of the number of patients in this study could lead to this conclusion. However, uveitis was found to be statistically significant in patients who had vasculitis in dermis. It can be a clue for prediction of disease severity and course. Further studies that include wide number of patients will better illuminate the correlation between histopathologic findings and disease severity and clinical course.
What is new?
Mixed type inflammatory cell infiltration, lobular panniculitis without vasculitis, neutrophil rich infiltration, and lymphocyte rich infiltration were found to be histopathologic findings of positive pathergy test in Behçet's disease.
Panniculitis among histopathologic findings in the pathergy test has never been reported.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Ghate JV, Jorizzo JL. Behçet's disease and complex aphthosis. J Am Acad Dermatol. 1999;40:1–18. doi: 10.1016/s0190-9622(99)70523-2. [DOI] [PubMed] [Google Scholar]
- 2.Criteria for diagnosis of Behcet's disease. International Study Group for Behcet's disease. Lancet. 1990;335:1078–80. [PubMed] [Google Scholar]
- 3.Mittal R, Chopra A, Handa F. Sutton's aphthae and Behçet's syndrome. Indian J Dermatol. 1985;30:17–21. [PubMed] [Google Scholar]
- 4.Cimen F, Yildirmak ST, Ergen A, Cakmak M, Dogan S, Yenice N, et al. Serum lipid, lipoprotein and oxidatively modified low density lipoprotein levels in active or inactive patients with Behçet's disease. Indian J Dermatol. 2012;57:97–101. doi: 10.4103/0019-5154.94273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karadag AS, Akbay G, Aydın M, Astarcı M, Eksioglu M. Comparison of clinical and histopathologic findings of pathergy test with disposable/sharp and nondisposable/blunt needles in Behçet's Disease. Turk J Med Sci. 2009;39:47–51. [Google Scholar]
- 6.Akmaz O, Erel A, Gürer MA. Comparison of histopathologic and clinical evaluations of pathergy test in Behçet's disease. Int J Dermatol. 2000;39:121–5. doi: 10.1046/j.1365-4362.2000.00884.x. [DOI] [PubMed] [Google Scholar]
- 7.Dilşen N, Koniçe M, Aral O, Ocal L, Inanç M, Gül A. Comparative study of the skin pathergy test with blunt and sharp needles in Behcet's disease: Confirmed specificity but decreased sensitivity with sharp needles. Ann Rheum Dis. 1993;52:823–5. doi: 10.1136/ard.52.11.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Varol A, Seifert O, Anderson CD. The skin pathergy test: Innately useful? Arch Dermatol Res. 2010;302:155–68. doi: 10.1007/s00403-009-1008-9. [DOI] [PubMed] [Google Scholar]
- 9.Blobner F. Zur rezidivierenden. Hypopyon-Iritis. Z Augenheilk. 1937;91:129–39. [Google Scholar]
- 10.Ergun T, Gürbüz O, Harvell J, Jorizzo J, White W. The histopathology of pathergy: A chronologic study of skin hyperreactivity in Behçet's disease. Int J Dermatol. 1998;37:929–33. doi: 10.1046/j.1365-4362.1998.00474.x. [DOI] [PubMed] [Google Scholar]
- 11.Jorizzo JL, Solomon AR, Cavallo T. Behçet's syndrome. Immunopathologic and histopathologic assessment of pathergy lesions is useful in diagnosis and follow-up. Arch Pathol Lab Med. 1985;109:747–51. [PubMed] [Google Scholar]
- 12.Haim S, Sobel JD, Friedman-Birnbaum R, Lichtig C. Histological and direct immunofluorescence study of cutaneous hyperreactivity in Behçet's disease. Br J Dermatol. 1976;95:631–6. doi: 10.1111/j.1365-2133.1976.tb07036.x. [DOI] [PubMed] [Google Scholar]
- 13.Haim S. The pathogenesis of lesions in Behçet's disease. Dermatologica. 1979;158:31–7. doi: 10.1159/000250740. [DOI] [PubMed] [Google Scholar]
- 14.Jorizzo JL, Abernethy JL, White WL, Mangelsdorf HC, Zouboulis CC, Sarica R, et al. Mucocutaneous criteria for the diagnosis of Behçet's disease: An analysis of clinicopathologic data from multiple international centers. J Am Acad Dermatol. 1995;32:968–76. doi: 10.1016/0190-9622(95)91333-5. [DOI] [PubMed] [Google Scholar]
- 15.Jorizzo JL, Solomon AR, Zanolli MD, Leshin B. Neutrophilic vascular reactions. J Am Acad Dermatol. 1988;19:983–1005. doi: 10.1016/s0190-9622(88)70264-9. [DOI] [PubMed] [Google Scholar]
- 16.Chun SI, Su WP, Lee S. Histopathologic study of cutaneous lesions in Behçet's syndrome. J Dermatol. 1990;17:333–41. doi: 10.1111/j.1346-8138.1990.tb01653.x. [DOI] [PubMed] [Google Scholar]
- 17.Ergun T, Gürbuz O, Dogusoy G, Mat C, Yazici H. Histopathologic features of the spontaneous pustular lesions of Behçet's syndrome. Int J Dermatol. 1998;37:194–6. doi: 10.1046/j.1365-4362.1998.00276.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim B, LeBoit EP. Histopathologic features of erythema nodosum-like lesions in Behçet's disease: A comparison with erythema nodosum focusing on the role of vasculitis. Am J Dermatopathol. 2000;22:379–90. doi: 10.1097/00000372-200010000-00001. [DOI] [PubMed] [Google Scholar]


