Abstract
A venous lake, sometimes referred to as senile hemangioma of the lips is usually a solitary, non-indurated, soft, compressible, blue papule occurring due to dilatation of venules. It is commonly found on sun-exposed surfaces of the face and ears. We describe a 46 year-old male who presented with this clinical picture on the lower lip.
Keywords: Senile hemangioma of the lips, venous lake, venules
Introduction
What was known?
The average age of presentation of the senile hemangioma has been reported to be 65 years. Actinic skin damage often occurs around venous lakes, as they have a shared aetiology.
Venous lakes, also known as “Phlebectases”[1] are small (0.2-1 cm), generally solitary, soft, compressible, violaceous, papules commonly found on sun-exposed areas, predominantly the vermilion border of the lips, and ears. Lesions generally occur among the elderly[2]. The importance lies in the fact that they may mimic nodular melanoma and pigmented basal cell carcinoma, but the lack of induration, slow growth, and lightening of appearance upon diascopy suggest against these differentials, and in favor of a vascular lesion. Additionally, lack of pulsation distinguishes this lesion of the lower lip from a tortuous segment of the inferior labial artery.
Case History
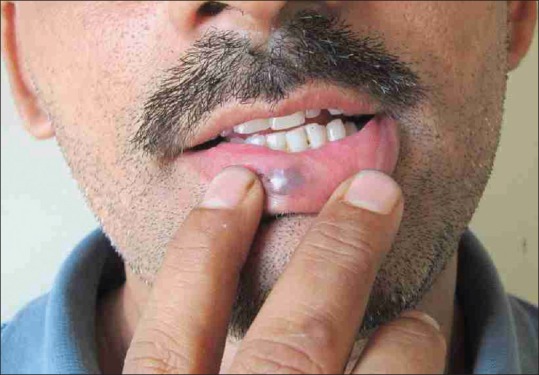
A 46 year old male patient presented with an 8 month history of a single, painless, bluish swelling over the lower lip which began as a pea sized lesion and gradually increased to the present size. Patient strongly denied any history of trauma at the site. No history of bleeding spontaneously or following minimal trauma could be elicited. On physical examination, a single, violaceous, soft, compressible, non-indurated, non-pulsatile papule was present on the lower lip [Figures 1 and 2]. On diascopy, the lesion could be emptied of most of its blood content and lightened [Figure 3]. After exclusion of other possible etiologic factors, venous lake was diagnosed. Patient was treated with cryotherapy with application of liquid nitrogen by dipstick method with one 10-second freeze-thaw cycle with a 1-mm margin [Figure 4]. This was done at biweekly intervals. Some improvement was obtained following 12 weeks of therapy.
Figure 1.
Minimal improvement at 12 weeks of cryotherapy
Figure 2.

Single, violaceous, soft, compressible,non-indurated papular lesion on the lower lip
Figure 3.

The lesion was emptied of most of its blood content and lightened with prominent telangiectatic vessels on diascopy
Figure 4.

Application of liquid nitrogen by dipstick method with a 1-mm margin
Discussion
Venous lake, also known as Bean-Walsh angioma, was first described in 1956 by Bean and Walsh, who also noted the compressibility and predilection for sun-exposed skin, especially the ears of elderly patients.[3] A venous lake is basically an acquired form of vascular ectasia. No racial predilection has been documented. Bean and Walsh reported that 95% of venous lakes were observed in males.[3] The disproportionate male distribution may be related to occupational sun exposure, hair length and hairstyles pattern differences among the males and females.
The cause is unknown; however it is thought to be associated with sun exposure, leading to a telangiectasias in the dermis. Venous lake has been reported only in adults and usually occurs in patients older than 50 years. The average age of presentation for venous lakes has been reported to be 65 years.
The typical presentation is a slow-growing asymptomatic, violaceous, soft, well demarcated, compressible, papulonodule up to 1 cm in diameter with a smooth surface. Compression often causes emptying of the blood content. Venous lakes typically are distributed on the sun-exposed surfaces of the face and neck, especially on the helix and antihelix of the ear and the posterior aspect of the pinna and vermilion border of the lower lip. Actinic skin damage often occurs around venous lakes as they have a shared aetiology. However in our patient, signs of actinic damage were not evident.
They are of little clinical significance, except that they can be confused with melanomas and pigmented basal cell carcinomas. On diascopy, these conditions can be easily differentiated from venous lakes as they do not change color. Epiluminescence techniques can also be used to differentiate venous lake from melanocytic neoplasms as the former when observed under the dermatoscope, has a homogenous reddish-blue to reddish-black color and no pigment network structures.
Blood laboratory studies are not usually indicated in the evaluation of venous lakes and other lesions of this type. Histopathologic examination often aids in confirmation of the clinical diagnosis of venous lakes. Either a great, dilated venule or multiple dilated spaces lined with a single layer of flattened endothelial cells and a thin wall of fibrous tissue filled with red blood cells are present without any elastic tissue or smooth muscle in the vessel wall. Thrombosis is sometimes present.
The prognosis is excellent. Assuring the patient of the benign nature of the lesion forms an important portion of the management. Treatment usually is performed for cosmetic reasons.
Surgical treatment by cryosurgery, electrosurgery, sclerotherapy, and excision have all been reported to be successful forms of therapy for venous lakes.[4]
What is new?
Senile hemangiomas do not exclusively occur on sun damaged skin. The age of presentation of the lesion can vary considerably.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.James, William, Berger Timothy, Elston Dirk. 10th ed. Saunders; 2005. Andrews’ Diseases of the Skin: Clinical Dermatology; p. 588. [Google Scholar]
- 2.Rapini, Ronald P, Bolognia, Jean L, Jorizzo Joseph L. Vol. 2. St. Louis: Mosby; 2007. Dermatology; p. 1624. [Google Scholar]
- 3.Bean WB, Walsh JR. Venous lakes. AMA Arch Derm. 1956;74:459–63. doi: 10.1001/archderm.1956.01550110003002. [DOI] [PubMed] [Google Scholar]
- 4.Neumann RA, Knobler RM. Venous lakes (Bean-Walsh) of the lips-treatment experience with the argon laser and 18 months follow-up. Clin Exp Dermatol. 1990;15:115–8. doi: 10.1111/j.1365-2230.1990.tb02045.x. [DOI] [PubMed] [Google Scholar]


