Abstract
A 47-year-old Indian woman with dark hair developed dramatic alopecia of the occipito-vertical area two weeks after a fluoroscopically-guided endovascular procedure for treatment of cerebral aneurysm. There was spontaneous repopulation of hair in 14 weeks. Neuro-radiological intervention procedures are becoming commoner by the day in India, and the rare but documented possibility of such reactions occurring in patients should be kept in mind by the treating surgeon as well as dermatologist. Necessary counseling regarding this uncommon side-effect is of essence, especially when the radiation dose exceeds 3 Gy. We believe this is the first case ever reported in Indian dermatology literature.
Keywords: Anagen effluvium, cerebral aneurysm, neuro-radiological procedures, radiation, temporary alopecia
Introduction
What was known?
Anagen effluvium is a commonly documented side-effect of radiation therapy. However, it has not been reported with fluoroscopically-guided endovascular procedures.
The rapidly proliferating keratinocytes in the hair matrix are most sensitive to radiation. The insult damages the keratinocytes, which results in thin, weakened hair shaft that is susceptible to trauma.
Complete hair re-growth occurs in a time period between two to four months following the insult.
Fluoroscopy-guided neuro-radiological endovascular procedures for treatment of arteriovenous malformations are getting commonplace in modern health care facilities of India. Temporary alopecia of the scalp is an uncommon but documented side-effect of these procedures, especially when a certain threshold of radiation is exceeded.[1,2,3,4] To the best of our knowledge, this is the first case of temporary alopecia after fluoroscopically-guided coiling procedure for a ruptured cerebral aneurysm being described in a dark haired woman from India.
Case Report
A 47-year-old apparently healthy woman was referred to this clinic (SV) for a dramatic non-scarring hair loss of occipito-vertical region since a month. It became known upon eliciting history that three weeks ago, she developed acute excruciating headache of the nape of the neck, profuse perspiration, vomiting, and lack of consciousness with incontinence. An urgent CT scan showed a ruptured anterior communicating artery aneurysm. A fluoroscopically-guided Guglielmi detachable coil (GDC) coiling procedure as a non-invasive treatment was suggested. A preliminary angiography lasting for two and half hours was done followed by an attempt to perform coiling that lasted unsuccessfully for four hours. Multiple ‘shoots’ had to be taken due to severe vasospasm. After waiting for two days to let the dye drain out, the procedure was attempted again, and coiling was done successfully in two and a half hours. A week later, the patient developed headache, for which another CT scan was done. The headache was attributed to cerbritis, and 24 mg of methylprednisolone was instituted on a slow taper. Methylprednisolone, nemodipine, and phenytoin were instituted during that period. Two weeks later, she noticed clumps of hair falling out initially during combing and then even while spontaneously running her fingers through her hair. There was a 6 × 4 inch-sized, asymptomatic, skin-colored alopecic patch in the occipital area with no erythema, scarring or scaling [Figure 1]. Her hair pull test was positive. Hair was sent for trichogram to an academic hospital in Coimbatore where they demonstrated 80% anagen hair showing dystrophy, the so called ‘bayonet hair.’ [Figure 2]. She had no exclamation mark hairs, poliosis, hair shaft disorders or positive history of similar affliction or atopy in her family. A vascular cause for the hair loss was ruled out by loud arterial pulse palpable in the temporal and occipital arteries. Pressure alopecia due to prolonged supine position was ruled out by absence of fractured hair shafts. She was euthyroid, had no history of taking any other drugs. Her hematologic parameters and endocrinologic profile were normal. A chest X-ray or USG of abdomen did not reveal anything abnormal.
Figure 1.
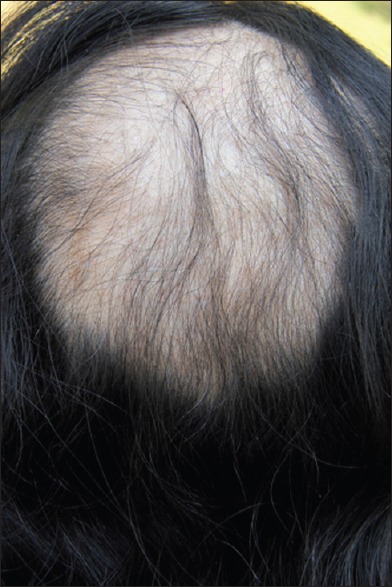
Occipito-vertical alopecia after radiation exposure
Figure 2.
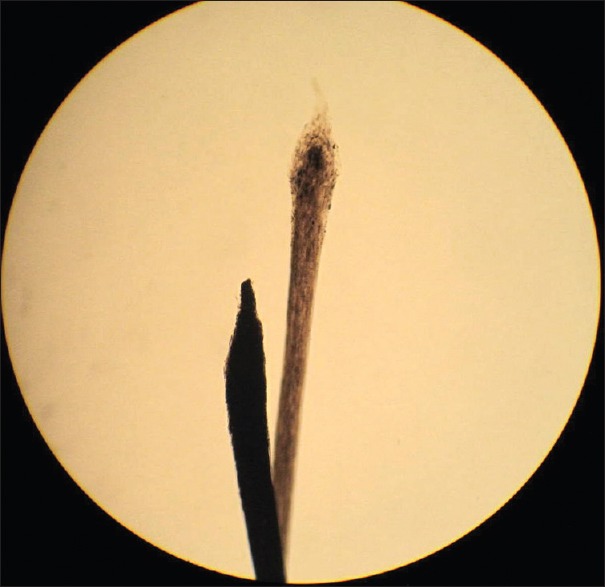
Anagen hair with the pointed distal end to the left and Telogen hair to the right
Diagnosis of fluoroscopic endovascular catheterization-induced alopecia was made. After a period of 14 weeks of observation and no active treatment, she showed significant re-growth of dark hair [Figure 3].
Figure 3.

Near total re-growth in 14 weeks
Discussion
Flouroscopically-guided endovascular procedures are becoming increasingly common all over the globe. While dermatologists have since long been consulted for hair loss following radiotherapy of tumors, there are only few reports of temporary hair loss following fluoroscopic endovascular procedures in dermatologic literature.[1,2,3,4] Other than radiation oncology, the maximum radiation exposure comes from equipment used for non-invasive interventions such as these.[1] The two commonest temporary side-effects of such procedures, erythema, and temporary hair loss are termed ‘deterministic’ and are indicative of a certain threshold of irradiation, below which the phenomenon would not be seen.[1] The probability of encountering such a side-effect would increase as the dose exceeds the threshold. The time between the exposure and appearance of clinical symptoms depend on the cell turnover rate. In tissues such as hair follicle with its rapid turnover rate, the effect is seen relatively quickly.[1] It is thought that irradiation doses exceeding 3 Gy are followed by such a hair loss during fluoroscopic procedures.[1,2,4,5,6,7] An estimated 7% of such radiological interventions are said to reach the threshold set for temporary hair loss by the International Commission on Radiological Protection.[2] According to the interventionalist, it would have grossly exceeded 3 Gy because the procedure turned out to be a very long one with prolonged exposure to the radiation owing to the difficulty in negotiating the loop through the site of pathology.
Fluoroscopy-related radiation-induced skin and hair reactions are rare and unanticipated. Dermatologists are sometimes the first to see them. It is not unusual for the patient to skip the history of radiation exposure because they are unaware of the fact that the procedure they have undergone involves radiation exposure and have not been forewarned by the interventionalist. Severity of radiation-induced temporary alopecia is largely dependent on the dose, total duration of irradiation, interval between irradiations (dose fractionation where applicable), the size of the skin area irradiated, the angle of irradiation, all affect the expression and severity of the injury.[1] One of the commonest working positions during GDC coiling procedure is posteroanterior, which explains the occipito-vertical hair loss in this patient. Scalp is supposed to be least sensitive to ionizing radiation.[1] Loss of scalp hair can occur at relatively lower doses when compared with doses at which other body hair is lost.[1] It is maximum in light-colored hair.[1] Our patient with jet black hair developing this dramatic hair loss is suggestive of gross excess of radiation. The rapidly dividing keratinocytes in the hair matrix are most sensitive to radiation. The radiation insult damages these keratinocytes and diminishes the growth of the growing hair shaft. Anagen effluvium occurs if the injury is sufficient to cause cessation of cell division. This results in thin, weakened hair shaft that is susceptible to trauma when it reaches the surface of scalp. Hair breakage in anagen effluvium occurs within days to weeks (1-3 weeks) following insult to the follicle. Microscopic hair examination shows that the distal hair shaft is dystrophic with a rapidly tapering configuration called the ‘bayonet hair.’ Tapered hair can arise in any process that inhibits the cell division in the hair matrix.[8] Since 90% of hair on the scalp is in growing phase, anagen effluvium has the potential to cause almost complete alopecia.[5,6,7]
Smoking, malnutrition, pre-existing autoimmune and connective tissue disorders like diabetes, hyperthyroidism, scleroderma, rheumatoid arthritis, and systemic lupus erythematosus predispose patients to the development of severe radiation effects in an unpredictable manner.[5] The cause is not known, and the association of SLE is still debated. Drugs that increase radiosensitivity include actinomycin D, doxorubicin, bleomycin, 5-fluorouracil, and methotrexate, mitoxantrone, 5-fluorourcil, cyclophosphamide, paclitaxel, docetaxel, and possibly tamoxifen. 2
Hair loss can be very embarrassing for a woman. In this case, it was literally adding insult to injury considering she had just recovered from a life-threatening situation. Fortunately, unassisted re-population of hair in 2-4 months is the most likely outcome and, therefore, a gentle handholding and confidence building are all that is required. Interventionalists should explain this possibility to patients in whom such a deterministic dose has been exceeded to avoid distress.[3] Fortunately, at such doses, there are very few chances of a serious or irreversible long-term consequence. However, all dermatologists should be aware of the association of hair loss with prolonged fluoroscopic endovascular procedures where the deterministic dose has been exceeded. The absorbed skin dose should be recorded on the patient's charts or medical record.[4,6,7] It is recommended that this dose be taken into account if the patient requires a future procedure involving exposure to ionizing radiation. Minimizing the effective dose to achieve the therapeutic goal is the aim, and efforts are on to reach that goal.[1,3,4]
What was new?
Fluoroscopically-guided interventional procedures are now performed fairly commonly in advanced tertiary care centers in India. Dermatologists who saw radiation-induced dermatoses until recently will now increasingly start seeing side-effects to the skin and hair due to these procedures, which is the second commonest cause of radiation exposure after radiotherapy.
Temporary alopecia of the scalp is a well-known early side-effect of ionizing radiation, which is emitted during the fluoroscopic-guided interventional procedures and is seen when a dose of 3 Gy is exceeded. Other factors that play a role include total duration of irradiation, interval between irradiations, size of the skin area irradiated, and the angle of irradiation.
The resultant alopecia is due to anagen effluvium, and there is complete spontaneous re-growth in about 2-4 months.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Mooney RB, McKinstry CS, Kamel HA. Absorbed dose and deterministic effects to patients from interventional neuroradiology. Br J Radiol. 2000;73:745–51. doi: 10.1259/bjr.73.871.11089467. [DOI] [PubMed] [Google Scholar]
- 2.Gavagan L, Ti J, Thornton J. Is hair loss a reality in neuro-interventional radiology? Radiat Prot Dosimetry. 2011;147:68–71. doi: 10.1093/rpd/ncr270. [DOI] [PubMed] [Google Scholar]
- 3.Wen CS, Lin SM, Chen Y, Chen JC, Wang YH, Tseng SH. Radiation-induced temporary alopecia after embolization of cerebral arteriovenous malformations. Clin Neurol Neurosurg. 2003;105:215–7. doi: 10.1016/s0303-8467(03)00007-6. [DOI] [PubMed] [Google Scholar]
- 4.Hayakawa M, Moritake T, Kataoka F, Takigawa T, Koguchi Y, Miyamoto Y, et al. Direct measurement of patient's entrance skin dose during neurointerventional procedure to avoid further radiation-induced skin injuries. Clin Neurol Neurosurg. 2010;112:530–6. doi: 10.1016/j.clineuro.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Balter S, Hopewell JW, Miller DL, Wagner LK, Zelefsky MJ. Fluoroscopically guided interventional procedures: A review of radiation effects on patients› skin and hair. Radiology. 2010;254:326–41. doi: 10.1148/radiol.2542082312. [DOI] [PubMed] [Google Scholar]
- 6.López V, López I, Ricart JM. Temporary alopecia after embolization of an arteriovenous malformation. Dermatol Online J. 2012;18:14. [PubMed] [Google Scholar]
- 7.Marti N, Lopez V, Pereda C, Martin JM, Montesinos E, Jorda E. Radiation-induced temporary alopecia after embolization of cerebral aneurysms. Dermatol Online J. 2008;14:19. [PubMed] [Google Scholar]
- 8.Stroud JD. Hair-shaft anomalies. Dermatol Clin. 1987;5:581–94. [PubMed] [Google Scholar]


