Abstract
Subacute cutaneous lupus erythematosus (SCLE) is a type of lupus erythematosus having distinct characteristic clinical, serologic, and genetic features. Other than the commonly occurring papulosquamous and annular polycyclic lesion, rarely it may present as erythema multiformae, toxic epidermo necrolysis like lesion (Rowell syndrome), erythroderma, and generalized poikiloderma. Herein, we report a case of SCLE presenting as erythroderma.
Keywords: Erythroderma, subacute cutaneous lupus erythematosus
Introduction
What was known?
Subacute cutaneous lupus erythematosus is a type of lupus erythematosus having distinct characteristic clinical, serologic, and genetic features.
Subacute cutaneous lupus erythematosus (SCLE) is a type of lupus erythematosus having distinct characteristic clinical, serologic, and genetic features. It occurs over the photo exposed areas and heals without scarring. It has intermittent recurrence of skin disease activity over long periods of time without significant progression to systemic involvement.[1] Antibodies to the Ro/SS-A antigen is closely associated with this group.[2] Among the various clinical presentations erythrodermic SCLE is very rare. Herein, we report such a case.
Case Report
A 58-year-old male presented with scaly lesions all over the body since 1 year. The lesions, which were scaly and itchy, were initially present over the face. Later, the scaling progressed to involve the extremities, trunk and back over a period of 2-3 months. Symptoms were more aggravated on exposure to sun. He also complained of multiple painful pustular lesions over the abdomen and extremities. Patient was a known case of diabetes on treatment for over 1 year.
On examination, diffuse scaling was present all over the body, more pronounced over the scalp, chest and back, fine scales were present over the face. Sparing of certain areas of abdomen was noted. Punched out ecthymatous lesions were present over abdomen, lower limb, which were tenders to touch [Figure 1].
Figure 1.

Diffuse scaling over the back with areas of normal skin over the lower back, echthymatous ulcers also seen
Haematological investigations were within normal limits. Random blood glucose was 210 mg/dl. Renal and liver function test and serum calcium were normal. Ultrasound abdomen, electrocardiogram and chest X-ray did not reveal any abnormality. Culture sensitivity revealed Staphylococcus aureus, sensitive to amoxicillin and ceftriaxone. On histopathology, the epidermis showed loss of rete pattern, and brisk mononuclear infiltrate present at dermo-epidermo junction with vacuolization of the basal keratinocyte with formation of clefts in certain areas. Focal pigment incontinence was observed [Figure 2].
Figure 2.
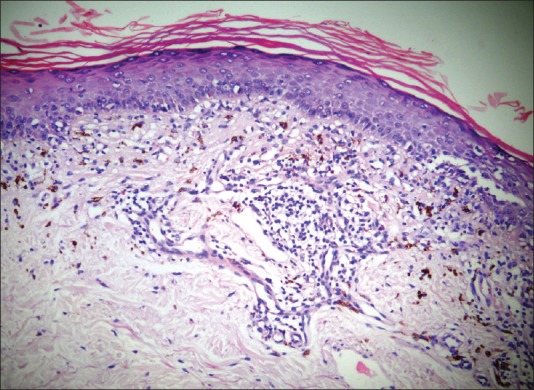
The epidermis showed loss of rete pattern and brisk mononuclear infiltrate present at dermo-epidermo junction with vacuolization of the basal keratinocyte. Focal pigment incontinence also seen (H and E, ×10)
Immunofluorescence assay revealed anti nuclear antibody positive in 1:320 titre with speckled nucleoli, suggestive of anti-SS-A/Ro pattern. Other investigations like skin scrapping for KOH, scabies mite, blood for human immunodeficiency virus and venereal disease research laboratory was negative. Though there was no apparent cause of erythroderma in our patient, the photoexacerbation of skin lesions, histopathological picture of interface dermatitis and immunofluorescence findings of a positive anti-SS-A/Ro pattern helped us in confirming SCLE as the cause of erythroderma. The patient was started on systemic antihistamines and antibiotics. Furthermore, topical betamethasone lotion and moisturisers were advised over the scaly lesions [Figure 3]. The patient showed good improvement after 2 weeks of this treatment.
Figure 3.

Markedly reduced scaling seen over the back after 1 week of treatment
Discussion
Sontheimer et al. in 1979 first described SCLE as a specific subset of lupus erythematosus, which differed from later based on clinical, histological, and immunological parameters.[3] This subset, which comprises approximately 10% of the patients with lupus erythematosus, have either non-scarring papulosquamous (two-third) or annular polycyclic (one-third) lesion.[2] Approximately 50% of patients with SCLE have four or more American Rheumatologic Association criteria for systemic lupus erythematosus of which arthritis is the most common manifestation.[4]
Erythematous macules or plaques over photo exposed sites like upper back, shoulder, extensor aspect of the arms, V areas of the neck are the first presentation in SCLE. These lesions later evolve into hyperkeratotic papulosquamous or annular/polycyclic plaques, which resolve leaving a grey white hypopigmentation and telangiectasia. The pigmentary changes usually resolve completely. When the face is involved, it is most often the lateral face with sparing of central and malar area.[1] SCLE can also be associated with diffuse non-scaring alopecia, mouth ulceration, (especially of the palate) reticular livedo, periungual telangiectasia, and Raynaud's phenomenon.[2] SCLE may occur in the course of PUVA treatment of psoriasis, radiation therapy, interferon therapy and also associated with breast cancer, meningioma, hepatocellular carcinoma, Hodgkin's disease, lung cancer, prostate cancer, and squamous cell carcinoma of head and neck.[2] Very rarely it is present as erythema multiforme, toxic epidermal necrolysis like lesion (Rowell syndrome), erythroderma and generalized poikiloderma.[2]
Exfoliative dermatitis or erythroderma is commonly associated with psoriasis and dermatitis. This presentation of SCLE is very rare with only three cases reported till date.[4,5,6] Therefore, a diagnosis of SCLE should be suspected in those cases of erythroderma in whom there is no apparent cause, if the history suggests a relation to UV light exposure and if the histologic findings reveal interface dermatitis.[4] In our case, extensive scaling probably indicates exacerbation of pre-existing papulosquamous type of SCLE following sun exposure.
Histopathologically SCLE frequently presents as interface dermatitis, with foci of vacuolar alteration of basal keratinocytes alternating with areas of lichenoid dermatitis. Dermal changes include oedema, prominent mucin deposition and sparse mononuclear cell infiltration usually limited to the area around blood vessel and peri-adnexal structure in upper one-third of the dermis.[1] Most cases of SCLE are positive for antibodies to the Ro/SS-A antigen.[7] Similar findings were seen in our patient. Treatment includes topical sunscreens, moderate potency steroids, pimecrolimus, and topical tacrolimus. Systemic steroids and hydroxychloroquine can be given in severe cases.
In conclusion, SCLE should be one of the differential diagnosis in patients with erythroderma associated with exacerbation following sun exposure.
What is new?
SCLE presenting as erythroderma has been reported in only three cases worldwide till date. No such case has been reported from India.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Costner IM, Sontheimer RD. Lupus erythematous. In: Klauswolff, Goldsmith LA, Katz SI, Gilchrist BA, Paller AS, Leffell DJ, editors. Fitz Patrick Dermatology in General Medicine. 7th ed. New York: McGraw Hill; 2008. pp. 1522–9. [Google Scholar]
- 2.Goodfield MJ, Jones SK, Vealae DJ. The connective tissue diseases. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rooks Textbook of Dermatology. 8th ed. UK: Wiley Blackwell; 2010. pp. 51.21–3. [Google Scholar]
- 3.Sontheimer RD, Thomas JR, Gilliam JN. Subacute cutaneous lupus erythematosus: A cutaneous marker for a distinct lupus erythematosus subset. Arch Dermatol. 1979;115:1409–15. [PubMed] [Google Scholar]
- 4.Mutasim DF. Severe subacute cutaneous lupus erythematosus presenting with generalized erythroderma and bullae. J Am Acad Dermatol. 2003;48:947–9. doi: 10.1067/mjd.2003.244. [DOI] [PubMed] [Google Scholar]
- 5.DeSpain J, Clark DP. Subacute cutaneous lupus erythematosus presenting as erythroderma. J Am Acad Dermatol. 1988;19:388–92. doi: 10.1016/s0190-9622(88)70184-x. [DOI] [PubMed] [Google Scholar]
- 6.Kalavala M, Shah V, Blackford S. Subacute cutaneous lupus erythematosus presenting as erythroderma. Clin Exp Dermatol. 2007;32:388–90. doi: 10.1111/j.1365-2230.2007.02410.x. [DOI] [PubMed] [Google Scholar]
- 7.LeFeber WP, Norris DA, Ryan SR, Huff JC, Lee LA, Kubo M, et al. Ultraviolet light induces binding of antibodies to selected nuclear antigens on cultured human keratinocytes. J Clin Invest. 1984;74:1545–51. doi: 10.1172/JCI111569. [DOI] [PMC free article] [PubMed] [Google Scholar]


