Abstract
Bowen's disease is generally regarded as premalignant dermatoses. The disease affects both skin and the mucosa and has the potential to progress to invasive squamous cell carcinoma. There are descriptions of several histological variants of Bowen's disease like psoriasiform, atrophic, pagetoid, etc. Acantholysis of anaplastic keratinocytes with bullae/cleft formation is described in premalignant condition like actinic keratosis and adenoid variant of squamous cell carcinoma, but there is lack of report describing this phenomena in Bowen's disease. We present a case of unusual acantholytic variant of Bowen's disease with focus of micro-invasive carcinoma.
Keywords: Acantholytic, Bowens’ disease, squamous cell carcinoma
Introduction
What was known?
Bowen's disease is a form of squamous cell carcinoma in situ, which may progress to invasive squamous cell carcinoma. It presents as a solitary, erythematous plaque with crusting and scaling usually on sun-exposed areas and may be mistaken clinically for localized psoriasis or lupus vulgaris.
Bowen's disease (BD) is an in-situ squamous cell carcinoma (SCC), which shows tendency towards lateral spread. If not treated, about 3-5% of this condition can progress into invasive squamous cell carcinoma that can metastatize and may even lead to death. A case of unusual acantholytic variant of Bowen's disease developing micro-invasive squamous cell carcinoma is presented for its rarity.
Case Report
A 44-year-old Indian male presented with a 2-year history of gradually enlarging pigmented skin lesion of his left arm with occasional itching. Physical examination revealed slightly elevated hyperpigmented plaque measuring 6 × 4 cms with well-defined borders and mild scaling over the lateral aspect of his left arm [Figure 1]. There was no associated lymphadenopathy. Patient had used treatment with topical corticosteroids and salicylic acid preparations without relief. An incisional biopsy was taken with a clinical differential diagnosis of Bowen's disease, localized psoriasis, and lupus vulgaris.
Figure 1.

Clinical picture showing large erythematous, crusted plaque on the forearm
Histopathological examination of the incisional biopsy from the lesion showed entire thickness of the epithelium exhibiting atypical keratinocytes with altered polarity, exhibiting marked nuclear pleomorphism, hyperchromasia and increased number of atypical mitosis [Figure 2a and b]. Also seen was intra-epidermal bulla/cleft formation in the suprabasal location and the presence of acantholytic anaplastic keratinocytes within the bulla [Figure 3]. A diagnosis of Bowen's disease-acantholytic variant (squamous cell carcinoma in-situ) was made and a wide excision of the lesion was advised.
Figure 2.
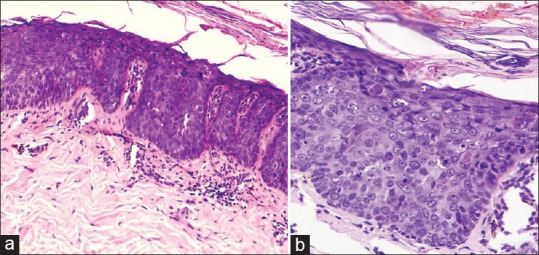
(a) Photomicrograph showing full thickness dysplasia of the epidermis, H and E, ×100. (b) Showing nuclear pleomorphism with altered polarity, increased mitosis and apoptosis, H and E, ×200
Figure 3.
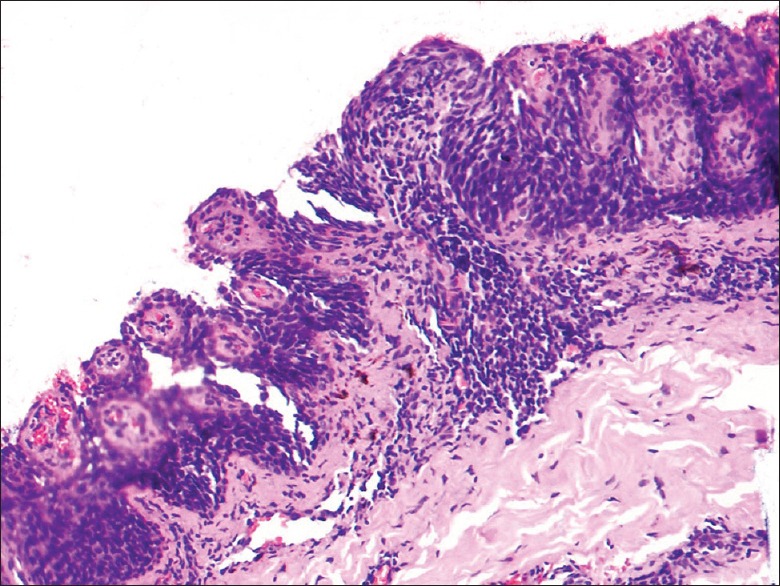
Photomicrograph shows intra epidermal villi formation due to acantholysis, H and E, ×200
Following the diagnosis, patient underwent wide surgical excision of the lesion. Multiple sections from the lesion revealed carcinoma in situ with extension of atypical keratinocytes into the follicular epithelium [Figure 4]. Microscopic invasion of the basement membrane with infiltration by malignant cells of the superficial dermis was noted, surrounded by inflammatory infiltrate and stromal desmoplasia [Figure 5]. A final diagnosis of acantholytic variant of Bowen's disease with micro-invasive squamous cell carcinoma was made.
Figure 4.
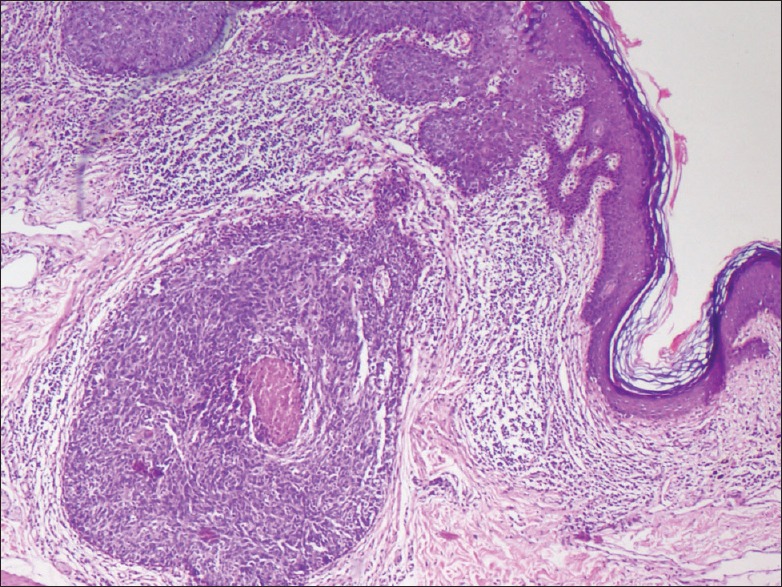
Photomicrograph shows dysplasia involving the epithelium of hair follicles in the dermis, H and E, ×100
Figure 5.
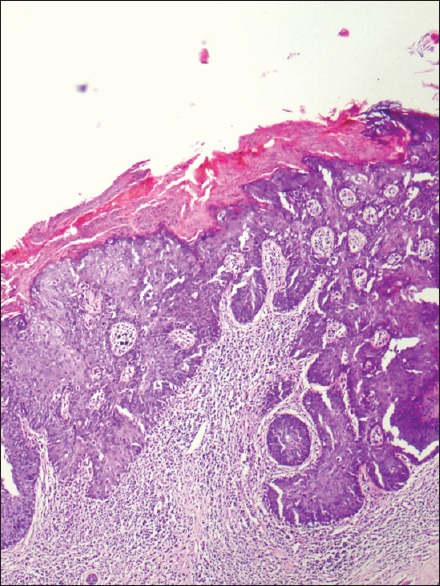
Photomicrograph shows disruption of basement membrane and invasion of dermis by malignant squamous cells surrounded by dense inflammatory infiltrate and stromal desmoplasia, H and E, ×200
Discussion
In 1912, Bowen reported a study of two cases of chronic atypical epithelial proliferation to which he gave the designation of precancerous dermatosis.[1] BD is most commonly seen in elderly individuals and presents clinically as a macule, papule, or a plaque. Most lesions appear as scaly, crusted, or fissured erythematous plaque. The borders are usually well demarcated from the surrounding skin, and the size may range from few millimeters to several centimeters in size. For most of the cases, the time of onset from symptoms to diagnosis is 5-6 years. It usually occurs in sun-exposed areas, but can also occur in ano-genital region, oral mucosa, nail bed, and conjunctiva. In the skin, Bowen's disease is associated with sun exposure, but in anal and genital region, high risk HPV genotypes are implicated in the etiology.[2]
Usually BD is a solitary lesion, but in 10% to 20% it occurs at multiple sites. The risk of progression into an invasive carcinoma is 3% to 5% in extragenital lesions and about 10% in genital lesions.[3] BD is very common in the Caucasian population with an incidence of 1.42 per 1,000 in some populations. BD has also been reported in association with underlying systemic malignancy.[4]
Histological examination of the lesion is important in order to identify whether it is benign or malignant. It also helps in differentiating lesions due to actinic keratosis, basal cell carcinoma, squamous cell carcinoma, seborrheic keratosis, psoriasis, and eczema.[3]
BD is characterized histologically by hyperkeratosis, parakeratosis, and acanthosis with thickened and elongated rete ridges. Scattered atypical cells and frequent mitoses are present. The keratinocytes show loss of maturity and polarity, giving the epidermis a disordered or “windblown” appearance. The dermal epidermal junction is intact, which distinguishes BD from invasive SCC. There may be a moderate inflammatory infiltrate of lymphocytes and histiocytes. Several histological subtypes such as psoriasiform, atrophic, epidermolytic and acantholytic, pagetoid variants are described.[5] Fitzpatrick describes this phenomenon in Bowen's disease; however, there is paucity of reports describing acantholytic variant of Bowen's disease.[5] Both Bowen's disease and actinic keratosis are intraepidermal squamous cell carcinomas with potential progression to invasive squamous cell carcinoma. Histologically, Bowen's disease shows highly atypical cancer cells with clumping with complete disorder throughout the epidermis, while actinic keratosis shows milder degree of atypia of keratinocytes without full thickness involvement. BD can also be differentiated from bowenoid AK by the presence of dysplasia involving the follicular epithelium.[6] Acantholysis due to lack of cohesion between keratinocytes with the formation of intra-epidermal bullae and clefts has been described in a wide variety of benign and malignant skin diseases such as actinic keratosis, paget's disease, melanocytic nevi, adenoid squamous cell carcinoma, and others.
Various treatment modalities such as surgery, curettage, cautery, cryotherapy, and topical therapies are widely in use for the treatment of this disease. Surgical excision is generally considered the treatment of choice for most lesions of this disease, if the size and location of the lesion permit, with a cure rate of 95%.[7] However, some studies report potential drawbacks of surgical excision with a high potential for incomplete excision and persistent disease, even after complete excision in some patients, and a high morbidity rate.[8] Topical agents like 5-FU and Imiqiumod can give good results and should be applied for 4-16 weeks once daily. Whether acantholytic variant of Bowen's disease behaves differently from the usual type is not clear due to paucity of reports on this unique variant of Bowen's disease.
What is new?
A uncommon histological variant – Acantholytic Bowen's disease is presented for its rarity, and differentiation from acantholytic variant of actinic keratosis is discussed.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Lee MM, Wick MM. Bowen's disease. CA-A Cancer Journal for Clinicians. 1990;40:237–42. doi: 10.3322/canjclin.40.4.237. [DOI] [PubMed] [Google Scholar]
- 2.Kettler AH, Rutledge M, Tschen, Buffone G. Detection of human papillomavirus in nongenital Bowen's disease by in situ DNA hybridization. Arch Dermatol. 1990;126:777–81. [PubMed] [Google Scholar]
- 3.Kao GF. Carcinoma arising in Bowen's disease. Arch Dermatol. 1986;122:1124–6. [PubMed] [Google Scholar]
- 4.Epstein E. Association of Bowen's disease with visceral cancer. Arch Dermatol. 1960;82:349–51. doi: 10.1001/archderm.1960.01580030043005. [DOI] [PubMed] [Google Scholar]
- 5.Duncan KO, Geisse JK, Leffell DJ. Epithelial precancerous lesions. In: Goldsmith LA, Katz SI, Gilchrest BA, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill; 2012. pp. 1261–83. [Google Scholar]
- 6.Bagazgoitia L, Cuevas J, Juarranz A. Expression of p53 and p16 in actinic keratosis, bowenoid actinic keratosis and Bowen's disease. J Eur Acad Dermatol Venereol. 2010;24:228–30. doi: 10.1111/j.1468-3083.2009.03337.x. [DOI] [PubMed] [Google Scholar]
- 7.Cox NH, Eedy DJ, Morton CA. Guidelines for management of Bowen›s disease. British associaton of dermatologists. Br J Dermatol. 1999;141:633–41. doi: 10.1046/j.1365-2133.1999.03100.x. [DOI] [PubMed] [Google Scholar]
- 8.Brown SR, Skinner P, Tidy J, Smith JH, Sharp F, Hosie KB. Outcome after surgical resection for high-grade anal intraepithelial neoplasia (Bowen's disease) Br J Surg. 1999;86:1063–6. doi: 10.1046/j.1365-2168.1999.01184.x. [DOI] [PubMed] [Google Scholar]


