Abstract
In many circumstances, causing sites of low back pain (LBP) cannot be determined only by anatomical imaging. Combined functional and morphological imaging such as bone scan with single-photon emission computed tomography/computed tomography (SPECT/CT) may be helpful in identifying active lesions. The purpose of this study was to evaluate the usefulness of bone SPECT/CT in localizing the pain site and the treatment of chronic LBP. One hundred seventy-five patients suffering from chronic LBP who underwent SPECT/CT were included, retrospectively. All of the patients received multiple general treatments according to the symptoms, and some of them underwent additional target-specific treatment based on SPECT/CT. Numerical rating scale (NRS) pain score was used to assess the pain intensity. Of 175 patients, 127 showed good response to the given therapies, while the rest did not. Overall, 79.4% of patients with definite active lesions showed good response. Patients with mild active or no lesions on SPECT/CT had relatively lower response rate of 63.0%. Good response was observed by the treatment with the guidance of active lesions identified on SPECT/CT. SPECT/CT could be useful in identifying active lesions in patients with chronic LBP and guiding the clinicians to use adequate treatment.
Graphical Abstract
Keywords: Low Back Pain; Tomography, Emission-Computed, Single-Photon; Tomography, X-Ray Computed; Pain Management; Technetium-99m (Tc-99m), Methylene Diphosphonate (MDP)
INTRODUCTION
Low Back Pain (LBP) is a common health finding causing disability that occurs in most people at some point in their lives. It was estimated that the incidence of a first-ever episode of LBP ranged from 6.3% to 15.4% a year in the general population (1). LBP persists more than three months is considered as chronic (2).
Identifying the origin of pain site in chronic LBP patients is often not easy. There are myriad reasons causing chronic LBP such as disc herniation and/or disruption, spinal stenosis, muscular origin, facet joint pain syndrome, sacroiliac joint disease, and their combinations. Furthermore, in many cases, diagnostic evaluation using anatomical images which points out just anatomical degenerative diseases or change are not helpful to manage chronic LBP, since those kinds of changes can also occur in asymptomatic people (3, 4, 5).
A difficulty to find out an origin of chronic LBP has resulted in variable options of its treatment. A strategy to manage chronic low back pain was proposed consisting of three categories: monotherapy, reductionism, and multidisciplinary treatment (6). While reductionism emphasizes target specific treatment based on pathoanatomical diagnosis using variable imaging devices, multidisciplinary treatment usually focuses the treatment of chronic LBP on its biopsychosocial rehabilitation (6). There have been other strategies to alleviate chronic LBP and surgery would not be very beneficial and be avoided in most of these strategies (7).
Functional imaging such as a bone scan with single-photon emission computed tomography (SPECT) offered diagnostic value which was not provided by planar imaging and anatomical imaging (8). Fusion of SPECT with computed tomography (SPECT/CT) increased the specificity of detecting lesions of the lower vertebral column and provided proper guidance to next step (9). Recently, it has been reported that bone scan with SPECT/CT was useful for identifying pain-inducing focus in the patients with chronic foot and low back pain (10, 11). The reductionism, which means treatment based on bone SPECT/CT findings, will be expected as an effective diagnostic tool in relieving pain (10, 11). In this study, the degree of treatment of low back pain according to the bone SPECT/CT finding was assessed. We evaluated the usefulness of bone SPECT/CT in localizing the pain site for the treatment of chronic LBP.
MATERIALS AND METHODS
Patients
Patients suffering from chronic low back pain and undergoing bone SPECT/CT from the second quarter of 2011 to the third quarter of 2013 were retrospectively included. Among them, multidisciplinary treatment with or without target-specific treatments were performed. Follow up was done until 3 months after the date of the first treatment, which was performed not more than 1 month after bone SPECT/CT. Patients who had any other causes of bone or joint abnormalities during or at the end of follow up were excluded.
Numerical rating scale (NRS) pain score of low back pain
The intensity of low back pain was evaluated by an 11-pointed numerical rating scale (NRS) pain score with no pain scaled as 0 and worst pain as 10 at pre-treatment and during follow up time. The NRS have well documented its reliability, validity and sensitivity to treatments that are expected to affect pain (12, 13). Evidence of temporary or permanent decrease of NRS score ≥ 2 during three month follow-up was considered as positive response to treatment (14, 15).
Treatment of low back pain
Patients were treated with multiple general treatments according to the symptoms. General treatments included: interventional muscle and nerve stimulation (IMNS), trigger point injection (TPI), needle transcutaneous electrical nerve stimulation (TENS), extracorporeal shock wave treatment (ESWT), medication, exercise, epidural steroid injection (ESI), epidural adhesiolysis, etc. Target-specific treatments such as facet joint injection, sacroiliac joint injection, medial branch block, and radiofrequency medial branch neurotomy for facet joint lesions were performed according to the patients' symptom and clinicians' decision. In case of positive finding of SPECT/CT, the treatment level was decided based on the SPECT/CT results. The treatment was performed in accordance with the clinical symptom and physical examination.
Imaging acquisition
Bone planar imaging was done 3 hr after injection of approximately 740-925 MBq (20-25 mCi) of technetium-99m methylene diphosphonate (Tc-99m MDP) intravenously followed by SPECT/CT of lumbar spine. SPECT acquisition was performed using low-energy high resolution collimator with 360° orbit, 120 steps (20 sec/step), and 128×128 matrix, while CT part of SPECT/ CT used 16-detector row helical CT with 100 kV, 40 mAs, 1 sec gantry rotation, and reconstructed section thickness of 2.5 mm.
Image interpretation and quantification
Locations/compartments of increased uptake were defined in 4 groups: facet joint, sacroiliac joint, combination, and no active lesion. The uptake positivity was scored by using 3-point scale (no uptake, mild increased uptake and definite positive uptake). The number of lesions in the same compartment and other compartments was also evaluated.
Statistical analyses
Positivity and intensity of uptake and gender were compared between responsive and non-responsive groups by chi-square test. Age, duration of disease, initial NRS, decreased NRS, number of positive lesions, compartment were compared by Mann-Whitney test. Logistic regression analysis was performed to find out which parameters were significant in determining response. A value of P<0.05 was considered statistically significant. All statistical calculation was performed using SPSS software, release 18 (Chicago, IL, USA).
Ethics statement
The study design and exemption of informed consent were approved by the institutional review board of Seoul National University Hospital (IRB No. 1404-149-001). Informed consent was waived by the board.
RESULTS
Patients' characteristics
A total of 175 patients (74 male and 101 female, mean age of 61.0±12.5 yr) suffering from chronic low back pain were included after excluding 6 patients with other causes of bone or joint abnormalities such as fibromyalgia (n=2), myalgia (n=1), peripheral nervous disease (n=1), peripheral vascular disease (n=1), and diabetic polyneuropathy (n=1). All patients were underwent bone SPECT/CT imaging for the purpose of diagnosis and treatment decision. One hundred forty-nine patients were found out to have active lesions on bone SPECT/CT, while 26 patients did not. All patients underwent non-target specific treatment (medication, exercise, TPI, IMNS, TENS, ESWT, ESI or combination of them), while 74 patients got 1 or more additional target-specific treatments such as facet joint injection (n=47), sacroiliac joint injection (n=17), medial branch block (n=49), radiofrequency medial branch neurotomy (n=9) or combination of them (n=16) according to the patients' symptom and clinicians' decision. Bone SPECT/CT revealed active lesions of facet joints in 56 (32.0%), sacroiliac joints in 7 (4.0%), combination of the above findings (mostly with facet joint component) in 86 (49.1%), and no active lesions in 26 (14.9%) patients, respectively. Detail characteristics are summarized in Table 1.
Table 1.
Distribution of patient based on responsiveness to treatment given after bone SPECT/CT imaging
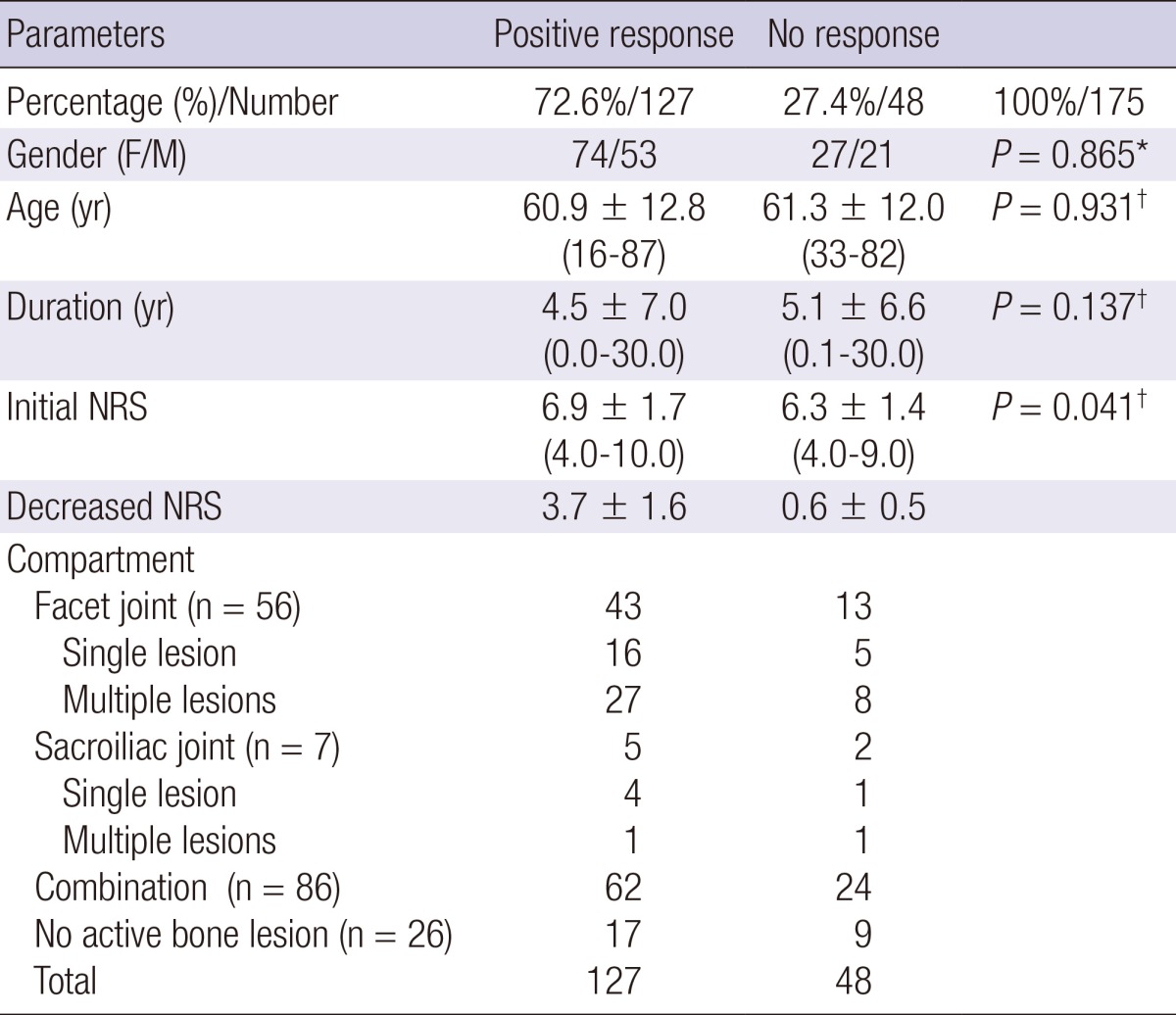
*Fisher's exact test; †Mann-Whitney Test. NRS, numerical rating scale.
Overall response to pain relief treatment
Positive response to treatment was observed in 127 of total 175 patients (72.6%), while non-response to treatment in 48 patients (27.4%). Patients with facet joint lesions showed positive responses in 43 patients of 56 (76.8%). Patients with sacroiliac joint lesions showed response in 5 patients of 7 (71.4%). Patients with at least 2 compartments combination lesions showed 72.1% of positive response in 62 patients of 86 (Table 1).
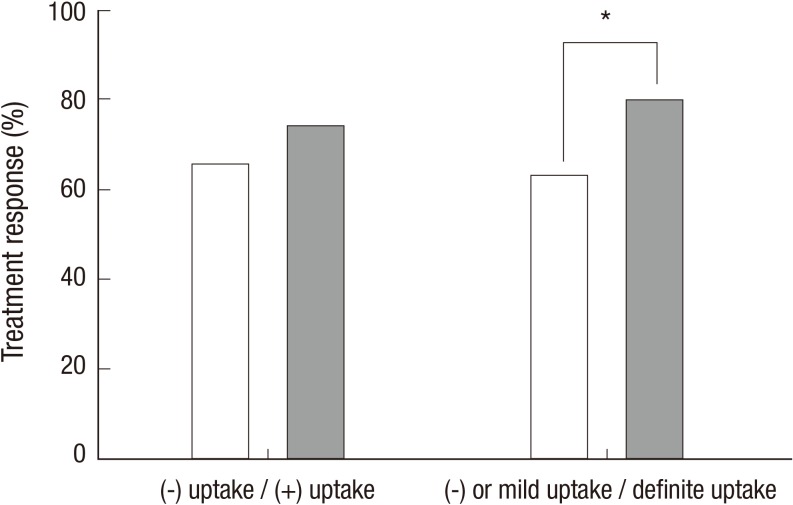
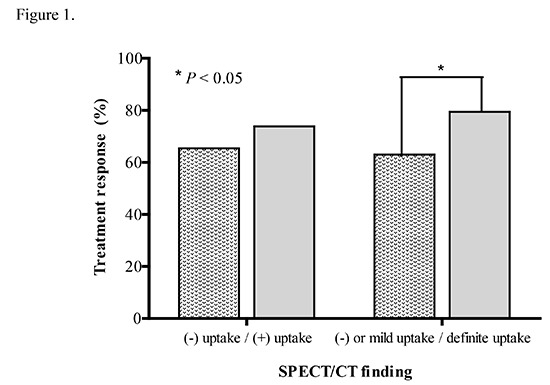
In positive-uptake group including mild or definite positive uptake in SPECT/CT, 73.8% (110 of 149 patients) showed response, while 65.4% (17 of 26 patients) showed response for treatment in no-uptake group (Fig. 1). The response for treatment is slightly higher in the positive-uptake group compared to that of the no-uptake group. This did not show statistical significance (P=0.373). When positive uptake in the SPECT/CT was divided into mild and definite uptake based on tracer intensity, the treatment response of definite uptake group was significantly higher than mild uptake group (63.0% vs. 79.4%, respectively, P=0.017) (Fig. 1).
Fig. 1.
Treatment response according to the intensity of lesions in SPECT/CT. The patients with definite uptake in SPECT/CT have better treatment response compared to the patients with no or mild uptake in SPECT/CT. *P = 0.017 (Pearson chi square).
Number of active lesions had no role in determining response rate (Table 2). There was no difference in response rate between single and multiple lesions groups (P=0.809). Response rates among different compartments in which active lesions located (facet joint, sacroiliac joint and combination) were not significantly different (P=0.815) (Table 3).
Table 2.
Treatment response according to the number of lesions in SPECT/CT
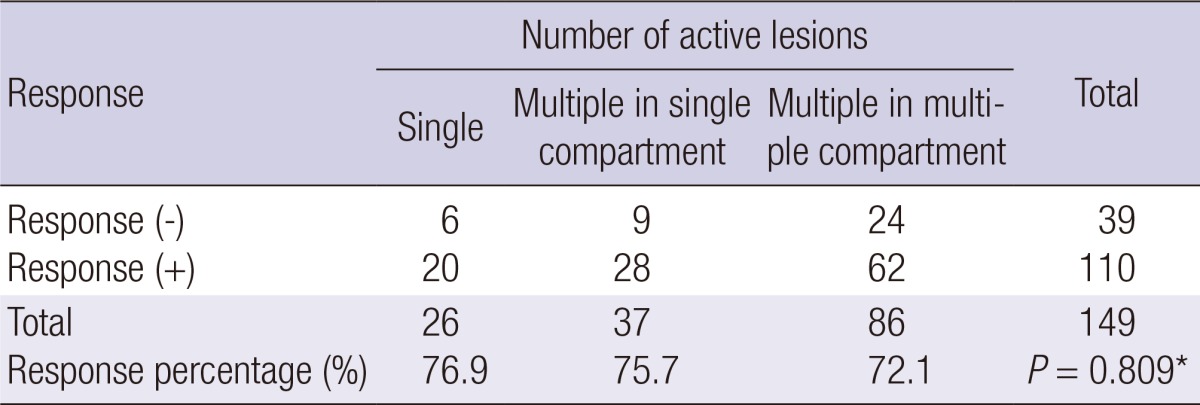
*Fisher's exact test (single lesion vs. multiple lesions).
Table 3.
Treatment response according to the compartment
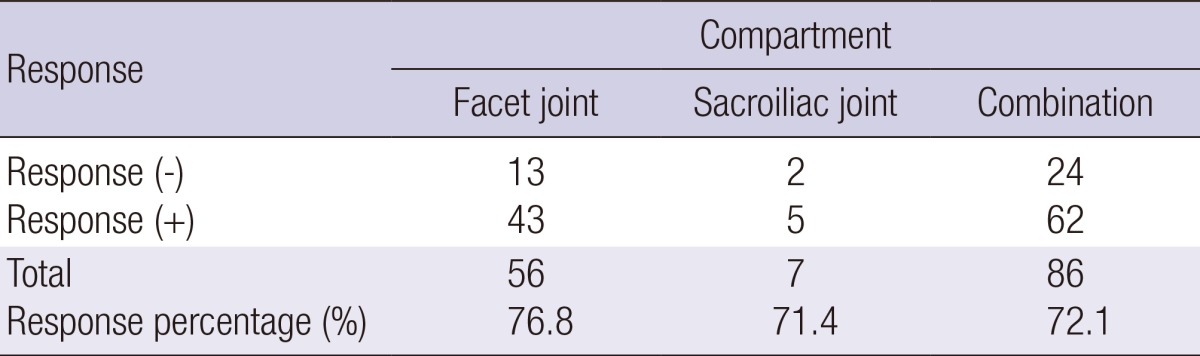
Compartment; facet joint, sacroiliac joint and combination (P=0.815, Fisher's exact test).
In univariate logistic regression analysis, initial NRS and definite positive uptake were regarded as significant predictors for the treatment (P=0.025, 95% CI, 1.031-1.574 and P=0.018, 95% CI, 1.152-4.448 respectively). In multivariate logistic regression analysis, both definite uptake was initial NRS were also regarded as significant predictors (P=0.028, odds ratio, 2.477; 95% CI, 1.103-5.566 and P=0.032, odds ratio, 1.264; 95% CI, 1.021-1.565 respectively). Other parameters (gender, age, duration of low back pain and number of lesions) were not significant (Table 4).
Table 4.
Univariate and multivariate logistic regression analysis of treatment response
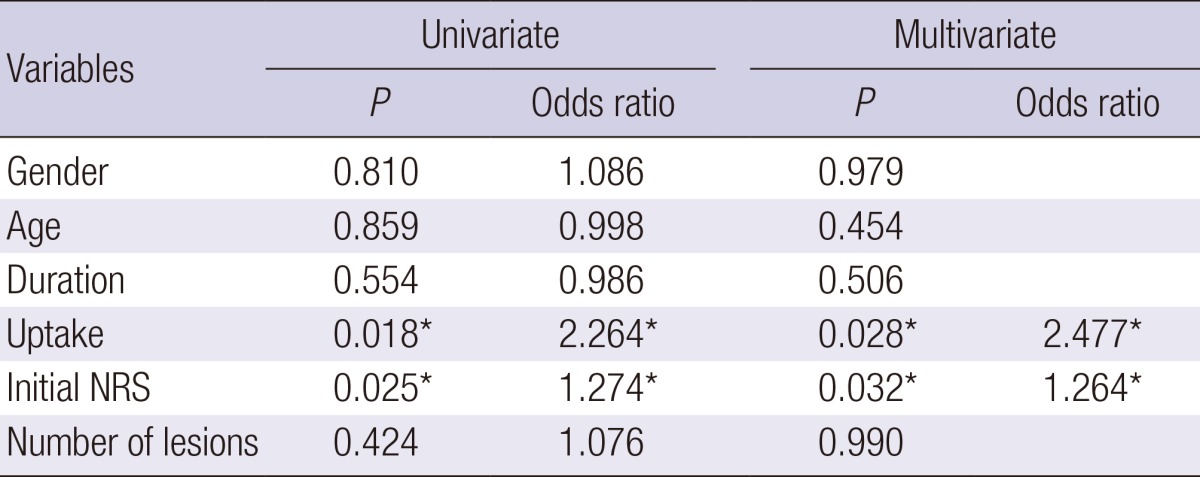
*P values indicate statistically significant differences. NRS, numerical rating scale.
In no active lesion with response group, the clinical diagnosis after the end of follow up was internal derangement of disc, failed back surgery syndrome, and spinal stenosis of lumbar spine. While, in no active lesion without response group the clinical diagnosis was spinal stenosis of lumbar spine and facet joint syndrome.
Initial NRS before treatment between responsive and non-responsive group was different (P=0.041). The score of responsive group was higher than that of non-responsive group. No significant difference is observed in NRS before treatment between definite uptake and other subgroup in responsive group (P=0.901) and non-responsive group (P=0.635). NRS decrease after treatment between uptake and non-uptake subgroup in both responsive group and non-responsive group were also not significantly different (P=0.841 and 0.345, respectively) (Table 5).
Table 5.
Numerical rating scale change in patients with low back pain
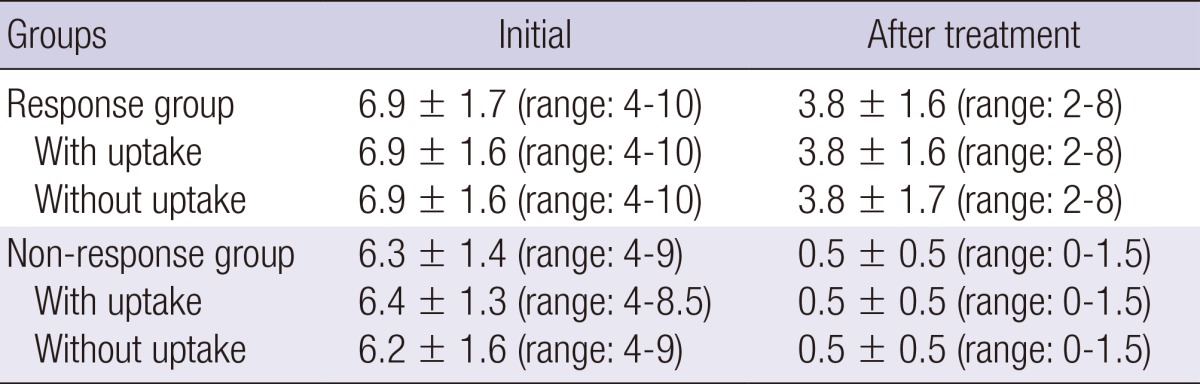
P values>0.05.
Response to treatment of regional target-specific pain control according to the active sites on bone SPECT/CT
The percentage of patients having target specific treatment in the definite positive uptake group was 90.2% (92 patients of total 102 patients). Of 73 patients with no or mild uptake on SPECT/CT, 44 patients were treated with target specific management (60.3%). Overall, 134 of 175 patients had target specific treatment. In the 134 patients with target specific treatment, 99 patients showed positive response for the treatment (73.9%). However 27 of 41 patients (65.9%) having only general treatment also showed positive response. No significant difference was observed between both groups (P=0.596).
Considering the patients with target specific treatment (134 patients), the group of definite uptake showed 82.6% of positive response (76 of 92 patients). On the contrary, the groups of no or mild uptake showed 54.8% of positive response (23 of 42 patients). These results showed that the treatment response rate of the definite uptake group was significantly higher than that of no or mild uptake group (P=0.001) (Table 6).
Table 6.
Treatment response according to the target specific pain control
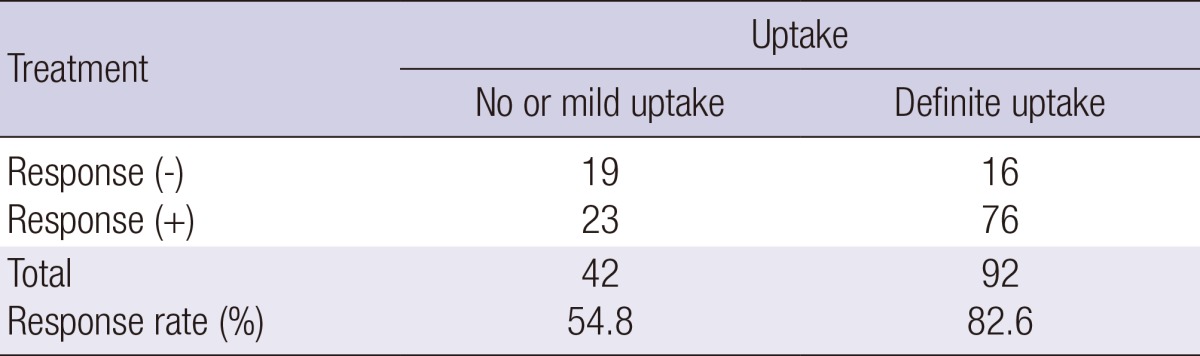
P=0.001, Pearson chi square
DISCUSSION
In this study, the active lesion on bone SPECT/CT and initial NRS were found as the parameter that can predict outcome of treatment. The patients with definite positive finding on SPECT/CT had good response for the treatment compared to those with no or mild uptake. The higher the initial NRS, the better outcome for the treatment had the patient. Other parameters such as gender, age, duration of back pain, number of active lesions and location had no role for the disease prognosis.
Patients with definite facet joint uptake on SPECT/CT showed good responses. This result is consistent with the previously reported result. Koh et al. reported that 79% of patients with positive facet joint lesions on SPECT/CT had good response to the treatment (16). This finding is already well known. Holder et al. (17) stated that the real value of bone SPECT was to find out suitable patients to undergo facet joint injection procedure. This statement was based on the high negative predictive value of bone SPECT (100%), while negative predictive value of planar imaging was 93%. Other studies stated similar findings. Dolan et al. (18) showed that bone SPECT improved the finding of metabolically active facet joints, directing to local steroid injection and better clinical outcome. McDonald et al. (19) also found that SPECT/CT was useful in showing the localization of active lesions in all 37 patients and facet joint injections were performed based on these findings. These studies suggest that SPECT/CT finding in patients with low back pain may be a prognostic factor. Our results were in accordance with these findings. The patients with definite uptake in SPECT/CT would have a favorable prognosis. Hence, the physicians should consider the SPECT/CT finding for the therapeutic decision of the patient with low back pain.
Patients with sacroiliac (SI) joint lesions also showed good response to treatment in our study. In clinical setting, determining sacroiliac joint as the cause of low back pain is not easy. One of the reasons was the uncertainty of the innervations of the joint (20). Different authors suggested different innervations, such as from sacral dorsal rami (21, 22), lumbosacral nerve root (23), and sacroiliac ligament (24). Murata et al. (25) illustrated sensory nerve fibers supplying the dorsal side originating from the dorsal root ganglions of the lower lumbosacral levels (from L4 to S2), while the ventral side from the dorsal root ganglions of the lumbar to sacral levels (from L1 to S2). Erosions and sclerosis are the findings of radiologic imaging of sacroiliitis due to inflammatory spondyloarthropathy. Inflammatory spondyloarthropathy should be present for imaging to detect painful SI joint syndrome (20). Slipman et al. (26) reported that abnormal bone scan findings were only found in small number (13%) of patients who were responsive to SI joint injection, despite the high specificity of 100%. Therefore, we suggest that SPECT/CT may be a useful tool for the diagnosis and treatment of patients with sacroiliac joint lesions.
It is well known that active lesion (increased uptake) reflects bone remodeling. Immunohistochemical analysis revealed that osteoblastic activity in facet joints was found in both ankylosing spondylitis and osteoarthritis cases suggesting that bone remodeling/formation had a role in physiological repair function (27). Ratcliffe et al. (28) also found similar finding that bone remodeling was proved to be increased in patient with osteoarthritis. Woo et al. (29) showed that in patients with ankylosing spondylitis, response to treatment with etanercept was followed by increase of bone formation markers (bone alkaline phosphatase, osteocalcine) and decrease of matrix metalloproteinase-3 (MMP-3), although with unchanged bone resorption marker (C-telopeptide of type-I collagen/CTX). The above studies and this current study showed that the response rate in patients with definite positive uptake was significantly higher than in those of no or mild uptake on bone scan. Thus, we can postulate that active lesion found on bone scan, which reflects bone remodeling (formation), is more potential to be responsive to treatment than lesion without uptake (30, 31).
In this current study, we proved that bone SPECT/CT was useful in the management of patients with chronic low back pain. In cases with facet joint arthropathy, bone SPECT/CT could be used to guide the clinician to use target specific treatment such as medial branch block. In some cases, bone SPECT/CT showed the abnormality of the involved bone and guide to use other modality to investigate bone and the related tissue (spinal cord, nerve, disc, etc.) in more detail to lead to target specific treatments if needed. For temporary pain control, in many cases non-target specific treatments were enough. This may explain the non-different response rates between target specific and non-target specific treatments in all sub-groups, although this may also be caused by the too-low number of patients in each sub-group.
Limitation of this study was the small number of patients suffering from other than facet joint arthropathy, as well as no-uptake lesions. The patient groups had heterogeneous lesions in low back and underwent variable combined treatment. This was also limitation of this retrospective study. Further study focusing on each compartment abnormality and each treatment may be needed for validation. The efficacy of the treatment was assessed during the 3 months after the initial treatment. In this study, long term effect of the treatment was not evaluated. The long term correlation between the SPECT/CT finding and treatment is needed.
Bone SPECT/CT is useful in identifying active lesions in patients with chronic low back pain and guiding the clinicians to use target specific treatment of pain control. In cases of active lesions identified on SPECT/CT, good response of pain control can be expected by the guidance of adequate location in target specific treatment. It also guided the use of other modalities to investigate bone and related tissues (spinal cord, nerve, disc, etc) in more detail.
In conclusion, treatment management based on bone SPECT/CT findings can be considered to be effective on pain control in patients with chronic low back pain.
ACKNOWLEGEMENTS
Fellowship of Koh Chang Soon Program is an international training project of Seoul National University College of Medicine in order for the promotion of nuclear medicine practice in developing countries, following the immortal spirit of the late professor Chang Soon Koh; Innovative Thinking and Harmonization.
Footnotes
This work was supported by Research Settlement Fund for the new faculty of Seoul National University and a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI14C1072).
The authors declare no competing financial interest.
References
- 1.Hoy D, Brooks P, Blyth F, Buchbinder R. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–781. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318:291–300. doi: 10.1056/NEJM198802043180506. [DOI] [PubMed] [Google Scholar]
- 3.Powell MC, Wilson M, Szypryt P, Symonds EM, Worthington BS. Prevalence of lumbar disc degeneration observed by magnetic resonance in symptomless women. Lancet. 1986;2:1366–1367. doi: 10.1016/s0140-6736(86)92008-8. [DOI] [PubMed] [Google Scholar]
- 4.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 5.Jarvik JJ, Hollingworth W, Heagerty P, Haynor DR, Deyo RA. The Longitudinal Assessment of Imaging and Disability of the Back (LAIDBack) Study: baseline data. Spine (Phila Pa 1976) 2001;26:1158–1166. doi: 10.1097/00007632-200105150-00014. [DOI] [PubMed] [Google Scholar]
- 6.Bogduk N, McGuirk B. Medical management of acute chronic low back pain : an evidence-based approach. Amsterdam; Boston: Elsevier; 2002. pp. 173–174. [Google Scholar]
- 7.Last AR, Hulbert K. Chronic low back pain: evaluation and management. Am Fam Physician. 2009;79:1067–1074. [PubMed] [Google Scholar]
- 8.Ryan PJ, Evans PA, Gibson T, Fogelman I. Chronic low back pain: comparison of bone SPECT with radiography and CT. Radiology. 1992;182:849–854. doi: 10.1148/radiology.182.3.1531544. [DOI] [PubMed] [Google Scholar]
- 9.Even-Sapir E, Flusser G, Lerman H, Lievshitz G, Metser U. SPECT/multislice low-dose CT: a clinically relevant constituent in the imaging algorithm of nononcologic patients referred for bone scintigraphy. J Nucl Med. 2007;48:319–324. [PubMed] [Google Scholar]
- 10.Kretzschmar M, Wiewiorski M, Rasch H, Jacob AL, Bilecen D, Walter MA, Valderrabano V. 99mTc-DPD-SPECT/CT predicts the outcome of imaging-guided diagnostic anaesthetic injections: a prospective cohort study. Eur J Radiol. 2011;80:e410–e415. doi: 10.1016/j.ejrad.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Carstensen MH, Al-Harbi M, Urbain JL, Belhocine TZ. SPECT/CT imaging of the lumbar spine in chronic low back pain: a case report. Chiropr Man Therap. 2011;19:2. doi: 10.1186/2045-709X-19-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Turk DC, Melzack R. Handbook of pain assessment. 3rd ed. New York: Guilford Press; 2011. pp. 19–44. [Google Scholar]
- 14.Manejias EM, Hu J, Tatli Y, Lutz GE. Lumbar zygapophysial joint radiofrequency denervation: a long-term clinical outcome study. HSS J. 2008;4:180–187. doi: 10.1007/s11420-008-9082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sloman R, Wruble AW, Rosen G, Rom M. Determination of clinically meaningful levels of pain reduction in patients experiencing acute postoperative pain. Pain Manag Nurs. 2006;7:153–158. doi: 10.1016/j.pmn.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Koh WU, Kim SH, Hwang BY, Choi WJ, Song JG, Suh JH, Leem JG, Shin JW. Value of Bone Scintigraphy and Single Photon Emission Computed Tomography (SPECT) in Lumbar Facet Disease and Prediction of Short-term Outcome of Ultrasound Guided Medial Branch Block with Bone SPECT. Korean J Pain. 2011;24:81–86. doi: 10.3344/kjp.2011.24.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holder LE, Machin JL, Asdourian PL, Links JM, Sexton CC. Planar and high-resolution SPECT bone imaging in the diagnosis of facet syndrome. J Nucl Med. 1995;36:37–44. [PubMed] [Google Scholar]
- 18.Dolan AL, Ryan PJ, Arden NK, Stratton R, Wedley JR, Hamann W, Fogelman I, Gibson T. The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol. 1996;35:1269–1273. doi: 10.1093/rheumatology/35.12.1269. [DOI] [PubMed] [Google Scholar]
- 19.McDonald M, Cooper R, Wang MY. Use of computed tomography-single-photon emission computed tomography fusion for diagnosing painful facet arthropathy. Technical note. Neurosurg Focus. 2007;22:E2. doi: 10.3171/foc.2007.22.1.2. [DOI] [PubMed] [Google Scholar]
- 20.Tuite MJ. Facet joint and sacroiliac joint injection. Semin Roentgenol. 2004;39:37–51. doi: 10.1016/j.ro.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Grob KR, Neuhuber WL, Kissling RO. [Innervation of the sacroiliac joint of the human] Z Rheumatol. 1995;54:117–122. [PubMed] [Google Scholar]
- 22.Fortin JD, Kissling RO, O'Connor BL, Vilensky JA. Sacroiliac joint innervation and pain. Am J Orthop (Belle Mead NJ) 1999;28:687–690. [PubMed] [Google Scholar]
- 23.Frymoyer JW, Ducker TB. The Adult spine : principles and practice. New York: Raven Press; 1991. pp. 143–150. [Google Scholar]
- 24.Vilensky JA, O'Connor BL, Fortin JD, Merkel GJ, Jimenez AM, Scofield BA, Kleiner JB. Histologic analysis of neural elements in the human sacroiliac joint. Spine (Phila Pa 1976) 2002;27:1202–1207. doi: 10.1097/00007632-200206010-00012. [DOI] [PubMed] [Google Scholar]
- 25.Murata Y, Takahashi K, Yamagata M, Takahashi Y, Shimada Y, Moriya H. Origin and pathway of sensory nerve fibers to the ventral and dorsal sides of the sacroiliac joint in rats. J Orthop Res. 2001;19:379–383. doi: 10.1016/S0736-0266(00)90017-2. [DOI] [PubMed] [Google Scholar]
- 26.Slipman CW, Sterenfeld EB, Chou LH, Herzog R, Vresilovic E. The value of radionuclide imaging in the diagnosis of sacroiliac joint syndrome. Spine (Phila Pa 1976) 1996;21:2251–2254. doi: 10.1097/00007632-199610010-00013. [DOI] [PubMed] [Google Scholar]
- 27.Appel H, Maier R, Loddenkemper C, Kayser R, Meier O, Hempfing A, Sieper J. Immunohistochemical analysis of osteoblasts in zygapophyseal joints of patients with ankylosing spondylitis reveal repair mechanisms similar to osteoarthritis. J Rheumatol. 2010;37:823–828. doi: 10.3899/jrheum.090986. [DOI] [PubMed] [Google Scholar]
- 28.Ratcliffe A, Seibel MJ. Biochemical markers of osteoarthritis. Curr Opin Rheumatol. 1990;2:770–776. doi: 10.1097/00002281-199002050-00014. [DOI] [PubMed] [Google Scholar]
- 29.Woo JH, Lee HJ, Sung IH, Kim TH. Changes of clinical response and bone biochemical markers in patients with ankylosing spondylitis taking etanercept. J Rheumatol. 2007;34:1753–1759. [PubMed] [Google Scholar]
- 30.Chun IK, Cheon GJ, Paeng JC, Kang KW, Chung JK, Lee DS. Detection and Characterization of Parathyroid Adenoma/Hyperplasia for Preoperative Localization: Comparison Between (11)C-Methionine PET/CT and (99m)Tc-Sestamibi Scintigraphy. Nucl Med Mol Imaging. 2013;47:166–172. doi: 10.1007/s13139-013-0212-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hong CM, Ahn BC, Choi SY, Kim DH, Lee SW, Kwon TG, Lee J. Implications of three-phase bone scintigraphy for the diagnosis of bisphosphonate-related osteonecrosis of the jaw. Nucl Med Mol Imaging. 2012;46:162–168. doi: 10.1007/s13139-012-0144-x. [DOI] [PMC free article] [PubMed] [Google Scholar]