Abstract
Background and Objectives
Coronary lesions with mismatched functional and anatomical significance are not uncommon. We assessed the accuracy and predictors of mismatch between fractional flow reserve (FFR) and quantitative coronary angiography (QCA) analyses in patients with coronary lesions.
Subjects and Methods
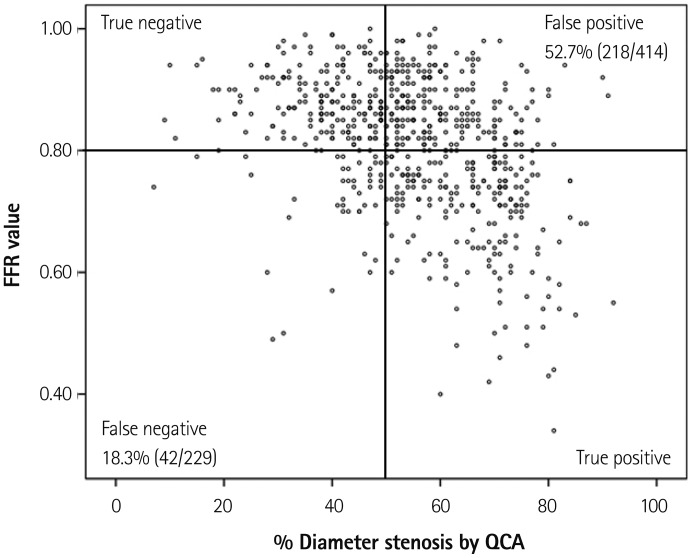
A total of 643 lesions with pre-interventional FFR and QCA measurements were consecutively enrolled and divided into four groups using FFR ≤0.80 and percent diameter stenosis (%DS) ≥50% as cutoffs for functional and anatomical significance, respectively. Accordingly, FFR >0.80 and DS ≥50%, and FFR ≤0.80 and DS <50% defined false-positive (FP) and false-negative (FN) lesions, respectively.
Results
Overall, 40.4% (260/643) of the lesions were mismatched, and 51.7% (218/414) and 18.3% (42/229) were FP and FN lesions, respectively. In a multivariate analysis, independent predictors of FP were non-left anterior descending artery location {odds ratio (OR), 0.36; 95% confidence interval (CI), 0.28-0.56; p<0.001}, shorter lesion length (OR, 0.96; 95% CI, 0.95-0.98; p<0.001), multi-vessel disease (OR, 0.47; 95% CI, 0.30-0.75; p=0.001), and larger minimal lumen diameter by QCA (OR, 2.88; 95% CI,1.65-5.00; p<0.001). Independent predictors of FN were multi-vessel disease (OR, 1.82; 95% CI, 1.24-5.27; p=0.048), aging (OR, 0.96; 95% CI, 0.93-0.99; p=0.034), smoking (OR, 0.36; 95% CI, 0.14-0.93; p=0.034), and smaller reference vessel diameter by QCA (OR, 0.30; 95% CI, 0.10-0.87; p=0.026).
Conclusion
A mismatch between FFR and angiographic lesion severity is not rare in patients with coronary artery disease; therefore, an angiography-guided evaluation could under- or over-estimate lesion severity in specific lesion subsets.
Keywords: Fractional flow reserve, myocardial; Coronary angiography; Coronary artery disease
Introduction
Many percutaneous coronary intervention (PCI) procedures are performed based solely on angiographic criteria, without prior assessment for ischemia. Although quantitative coronary angiography (QCA) analysis more precisely estimates stenotic segment dimensions, coronary stenosis severity calculated by QCA does not always correlate with clinical presentation.1),2) Decision making for revascularization based on angiography alone without noninvasive testing can be difficult for intermediate or ambiguous coronary stenoses.3) Therefore, coronary angiography alone can frequently misdiagnose functional severity in specific lesion subsets.4),5)
Fractional flow reserve (FFR) is a physiological index of ischemia secondary to coronary artery stenosis, and FFR-guided coronary revascularization with drug-eluting stents improves patient outcomes.4),6) We assessed predictors of mismatch between FFR and QCA analysis in patients with coronary lesions.
Subjects and Methods
Patient population and study design
A total of 673 patients (893 lesions), who underwent coronary angiography and an invasive physiological evaluation using a pressure wire before intervention between May 2006 and June 2012, were consecutively screened for the current analysis. In total, 462 patients with 643 lesions were finally included (Table 1) based on the following criteria. All patients had at least one target vessel with >30% stenosis diameter measured by QCA analysis and were not eligible for enrollment if they had: 1) undergone primary or emergent PCI for acute coronary syndrome, 2) prior coronary artery bypass graft surgery, 3) multiple lesions in the same epicardial artery, 4) lesions treated previously by PCI, 5) previous infarcted lesion, 6) left main disease, primary myocardial disease, or a major life threatening illness, or 7) contraindications to adenosine, aspirin, or clopidogrel. All lesions were divided into four groups: true positive (TP), FFR ≤0.80 and diameter stenosis (DS) ≥50%; false positive (FP), FFR >0.80 and DS ≥50%; true negative (TN), FFR >0.80 and DS <50%; and false negative (FN), FFR ≤0.80 and DS <50%. DS was measured by QCA analysis. Clinical risk factors and lesion characteristics were compared between the FP and TP groups, and between the FN and TN groups (Table 2). The study outcomes were the incidence and predictors of coronary lesions with a function-anatomy mismatch.
Table 1.
Baseline characteristics
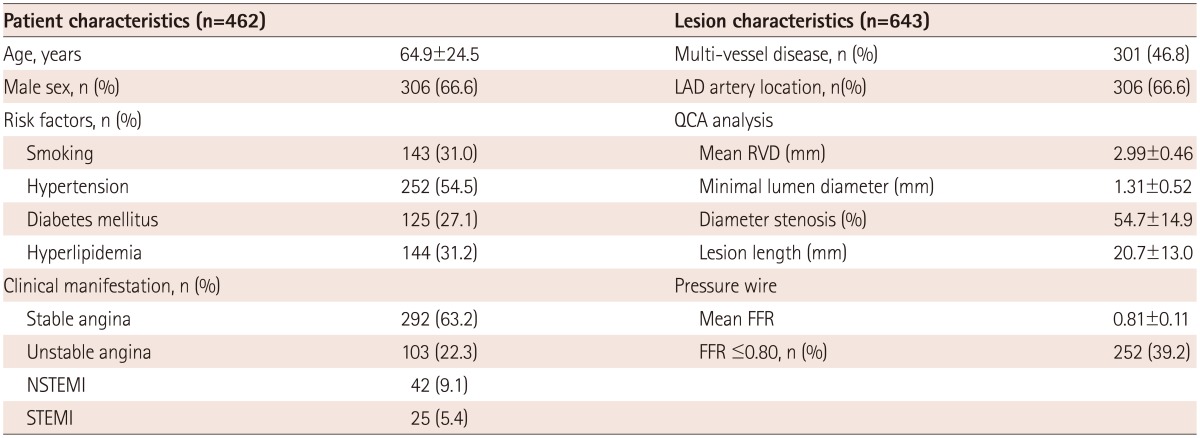
NSTEMI: non ST-segment elevation myocardial infarction, STEMI: ST-segment elevation myocardial infarction, LAD: left anterior descending, QCA: quantitative coronary analysis, RVD: reference vessel diameter, MLD: minimal lumen diameter, FFR: fractional flow reserve
Table 2.
Comparisons according to anatomical and functional significance
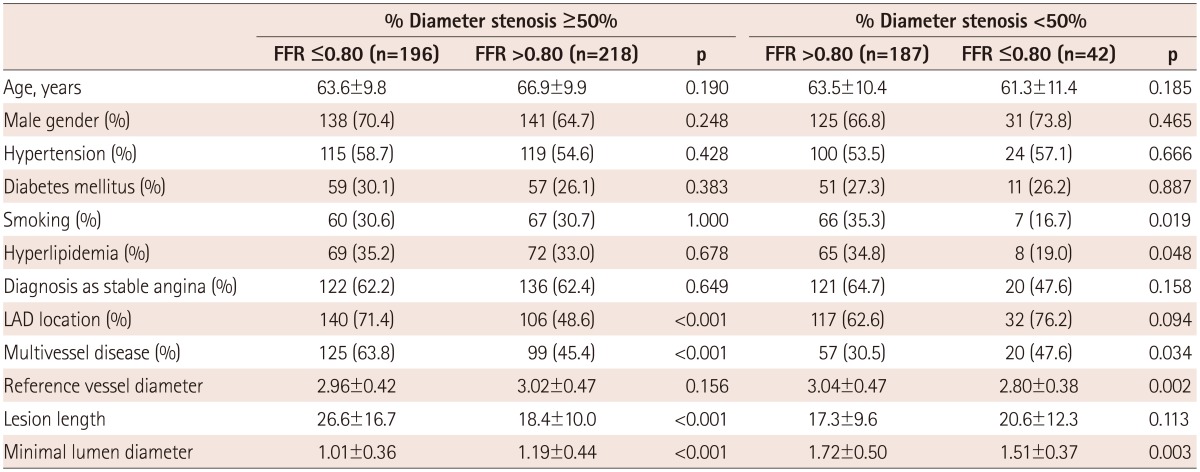
Values are number of patients (%) and mean±standard deviation. FFR: fractional flow reserve, LAD: left anterior descending
Fractional flow reserve
Fractional flow reserve was defined as the ratio between mean distal coronary pressure and mean aortic pressure, measured simultaneously at maximal hyperemia. Coronary pressure was measured using a 0.014-in sensor-tipped PCI guidewire (Pressure Wire, RADI Medical Systems, Uppsala, Sweden; Saint Jude Medical, Sylmar, CA, USA). The wire was introduced through a 6- or 7-Fr guiding catheter, equalized, and advanced distal to the stenosis as described previously. The FFR value was checked after administering adenosine to induce maximal hyperemia, either intravenously (≥40 µg/kg/min) or into a coronary artery (≥40 µg in the right, or ≥80 µg in the left coronary artery).7),8)
Angiographic analyses
The QCA analysis was performed in the core laboratory at Keimyung University Dongsan Medical Center by an experienced observer who was blinded to the FFR value. Reference vessel diameter (RVD), minimal lumen diameter (MLD), and lesion length (LL) were measured using the guiding catheter for calibration and an edge detection system (CAAS 5.7 QCA system, Pie Medical, Maastricht, The Netherlands), and percent DS (%DS) was calculated.
Statistical analyses
Results are expressed as mean±standard deviations for continuous variables and frequencies for categorical variables. Comparisons of continuous variables were performed using Student's t-test. Analysis of discrete variables was performed using the chi-square test. Multiple logistic regression analysis was used, and variables with a univariate value of p<0.20 and historically proven risk factors were incorporated into the multivariate models. All statistical analyses were performed using SPSS ver. 19.0.0 (IBM, Armonk, NY, USA) and a p<0.05 was considered significant.
Results
Baseline characteristics
A total of 462 patients (643 de novo lesions), who underwent coronary angiography and FFR assessment, were consecutively enrolled. Baseline clinical and angiographic characteristics are summarized in Table 1. The incidence of diabetes was 27%. Left anterior descending artery (LAD) lesions accounted for 67% of the lesions. Mean FFR at maximal hyperemia was 0.81±0.11. FFR ≥0.80 was seen in 37.0% of lesions.
Prevalence of angiographic and functional mismatch
The optimal cutoff value of angiographic %DS for predicting FFR ≤0.80 was 53% (area under the curve, 0.73; 95% CI, 0.69-0.77; p<0.001), with sensitivity of 61% and specificity of 75%. The overall incidence of function-anatomy mismatched lesions was 40.4% (260/643 lesions). Although angiographic %DS significantly correlated with FFR (p<0.001, r=-0.40), FFR >0.80 as FP was seen in 218 (52.7%) among the 414 lesions with angiographic %DS ≥50%. In contrast, FFR ≤0.80 as FN was found in 42 (18.3%) among the 229 lesions with DS <50% (Fig. 1). Furthermore, if only intermediate lesions (%DS, 30-70%) were included, 43.5% (219/503) were mismatched; the FP rate was 60.9%, and the FN rate was 18.4%.
Fig. 1.
Incidence of mismatched lesions.
Predictors of angiographic and functional mismatch
The FP group had lower proportions of LAD location and multi-vessel disease (MVD), shorter LL, and larger MLD, whereas the FN group had lower frequencies of smoking and hyperlipidemia, higher frequency of MVD, and smaller mean RVD and MLD (Table 2). The multivariate analysis included the following factors; age, sex, history of hypertension, smoking, diabetes, hyperlipidemia, MVD, LAD, degree of RVD, MLD, and LL. The analysis revealed that independent predictors for FP were non-LAD artery location (OR, 0.36; 95% CI, 0.28-0.56; p<0.001), shorter LL (OR, 0.96; 95% CI, 0.95-0.98; p<0.001), MVD (OR, 0.47; 95% CI, 0.30-0.75; p=0.001), and larger MLD by QCA (OR, 2.88; 95% CI, 1.65-5.00; p<0.001). Independent predictors for FN were MVD (OR, 1.82; 95% CI, 1.24-5.27; p=0.048), aging (OR, 0.96; 95% CI, 0.93-0.99; p=0.034), smoking (OR, 0.36; 95% CI, 0.14-0.93; p=0.034), and smaller RVD by QCA (OR, 0.30; 95% CI, 0.10-0.87; p=0.026) (Table 3 and 4).
Table 3.
Predictors of false positive between fractional flow reserve (FFR) and quantitative coronary angiography (QCA)
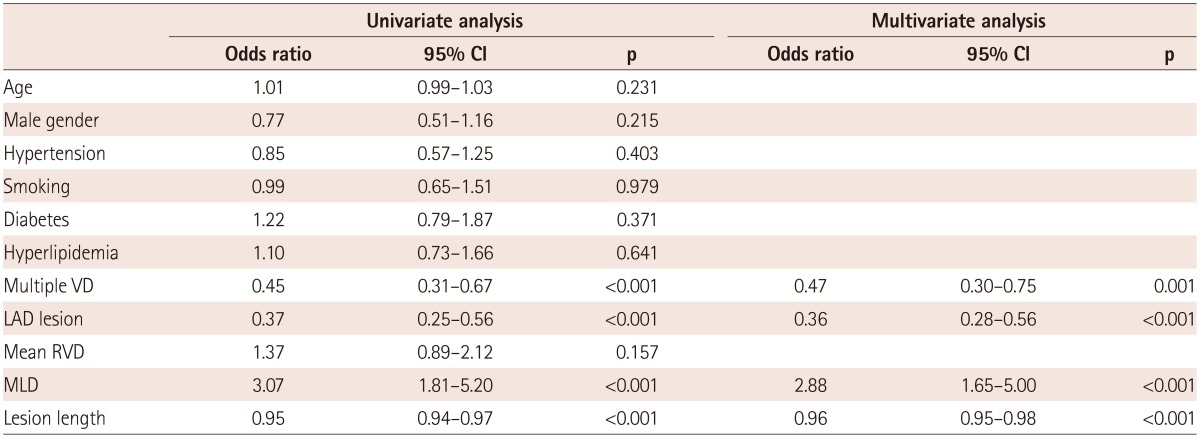
VD: vessel disease, LAD: left anterior descending, RVD: reference vessel diameter, MLD: minimal lumen diameter
Table 4.
Predictors of false negative between fractional flow reserve (FFR) and quantitative coronary angiography (QCA)
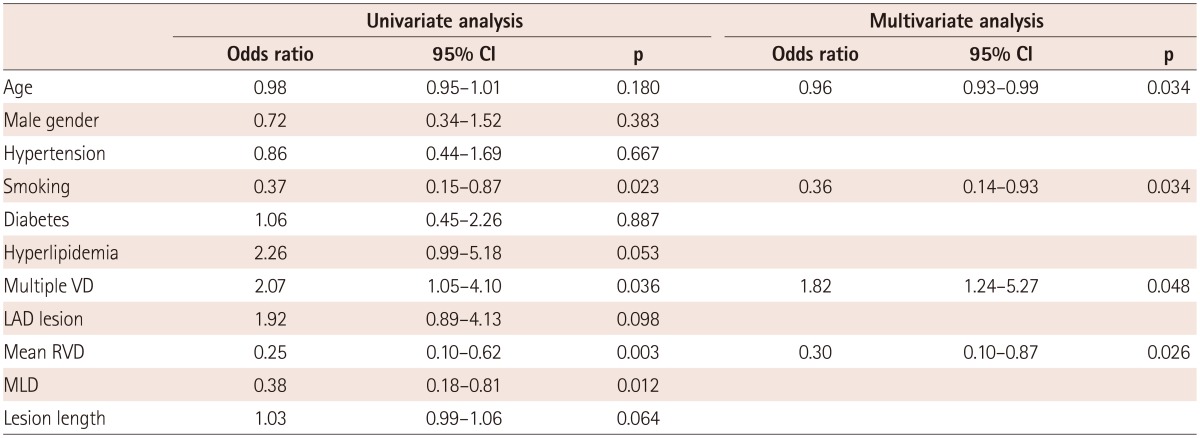
VD: vessel disease, LAD: left anterior descending, RVD: reference vessel diameter, MLD: minimal lumen diameter
Discussion
The major findings of the study were: 1) anatomical-functional mismatch was not rare, with FP and FN mismatch between QCA and FFR of 52.7% and 18.3%, respectively, 2) an estimate of lesion severity should be performed considering several clinical and angiographic factors, such as age, cardiovascular risk factors, disease extent, and lesion location, and 3) although QCA is more reliable than a visual estimate, precise characterization of lesion severity should include confirmation by a functional evaluation in specific lesion subsets.
Despite the development of many noninvasive imaging tests, coronary angiography remains an unsurpassed tool for cardiologists to perform revascularization.9) Although QCA more precisely assesses the dimensions of a stenotic segment,1) QCA-calculated severity does not always correlate with clinical presentation of related symptoms.2)
The most important factor related to outcome in a patient with coronary artery disease is the presence and extent of inducible ischemia.10),11) FFR is an accurate and lesion-specific index to indicate whether a particular stenosis or coronary segment is responsible for ischemia.12),13),14)
In this study, the overall mismatch between QCA and FFR was not rare and was detected in 40.4% (260/643) of lesions. Among the 414 lesions with angiographic DS ≥50%, 218 (52.7%) were in the FP category after the functional assessment. In contrast, among the 229 lesions with DS <50%, 42 (18.3%) were FN. Our findings are similar to those in a recent study by Park et al.,15) who reported a 57% incidence for FP and 16% for FN. In addition, unlike the previous study, our new data analysis indicated that extents of diseased vessel were predictors of FP and FN. Therefore, FFR-guided PCI reduces the over- or under-estimation of angiographic lesion severity, particularly for intermediate and ambiguous lesions. In the highly effective drug-eluting stent era, confirming functional severity of lesions that cannot be ignored for revascularization can help prevent future adverse events.
In the multivariate analysis, lesion location, extent of diseased vessels, RVD, MLD, LL, aging, and smoking were associated with mismatched lesions. A non-LAD lesion could be an important predictor of angiographic overestimation in the current study. The large burden of myocardium in the LAD territory compared with that of other major coronary arteries could be an explanation for this phenomenon. Proximal LAD lesions are associated with significantly lower FFR values and a higher rate of positive FFR compared to those in the left circumflex and right coronary arteries.16) A significant inverse correlation is observed between the FFR value and the amount of jeopardized myocardium.
The extent of diseased vessels physiologically affects coronary stenosis. MVD was a predictor of FN lesions in the current analysis. Because of possible diffuse disease, MVD has a lower FFR than single-vessel disease (SVD) for a given degree of stenosis. Furthermore, nonculprit lesions in MVD could be underestimated by QCA due to the diffusivity of a stenotic culprit lesion, compared with a similar stenotic SVD.
Lesion severity can be underestimated at a younger age compared to that in the elderly, which could be explained by a stronger response to adenosine and better microvascular circulation compared to those in the elderly.17) Smoking as an inverse predictor of FN could also be explained by microvascular dysfunction.
Because MLD and LL are main determinants of functional significance in coronary lesions,14) larger MLD and shorter LL for a given stenosis could have been the cause for angiographic overestimation in the current study. Although it appears significant angiographically, a larger MLD guarantees blood flow in the corresponding territory. Not surprisingly, lesion length can also affect lesion severity. Lesion length is an important geometric variable positively correlated with the trans-stenotic pressure gradient. In contrast, an angiographic assessment could lead to underestimating relatively diffuse coronary disease or small artery disease.
Use of the FFR value in a functional evaluation of coronary artery disease can prevent under- or overestimating using an angiographic-only assessment. Baseline risk factors such as aging and smoking, and angiographic factors such as extent of diseased vessels, MLD, RVD, and LL should be carefully considered when evaluating coronary lesion severity. Nevertheless, it may be difficult to determine the functional significance of the indicated lesion. Therefore, a lesion-based functional evaluation such as FFR should be applied in specific situations.
Limitations
Several limitations of this study should be mentioned. First, this study was performed retrospectively in a single center on a relatively small population, thereby possibly not devoid of selection bias. However, the large number of lesions analyzed could partly overcome the latter limitation. Second, we could not co-evaluate functional status of other vessels, which could have affected the lesion's FFR value in MVD. Third, factors regarding coronary dominancy that can affect coronary functional status were not evaluated. Fourth, intravascular ultrasound (IVUS) was not analyzed. IVUS more accurately shows lesion severity. However, in another comparative study, about 30% of lesions were still under- or overestimated by IVUS criteria compared with that of FFR, as in our study.18) Fifth, we used various adenosine administration methods, which could have lead to under- or overestimating lesion severity by FFR. Finally, clinical outcomes could not be evaluated in our study.
Conclusion
Mismatch between function assessed by FFR and anatomy by angiography is not rare in patients with coronary artery disease. FP FFR was more common in patients with a non-LAD artery location, SVD, shorter lesion length and larger MLD, FN FFR in MVD, aging, smoking, and smaller reference vessel diameter. Therefore, an angiographic-only dedicated lesion evaluation in the catheterization room might under- or overestimate actual coronary lesion severity.
Acknowledgments
This study was supported by a grant from The Korean Society of Cardiology in 2013 and by a grant from the Scholar Research Grant of Keimyung University in 2012.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Reiber JH, van der Zwet PM, Koning G, et al. Accuracy and precision of quantitative digital coronary arteriography: observer-, short-, and medium-term variabilities. Cathet Cardiovasc Diagn. 1993;28:187–198. doi: 10.1002/ccd.1810280301. [DOI] [PubMed] [Google Scholar]
- 2.Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995;92:2333–2342. doi: 10.1161/01.cir.92.8.2333. [DOI] [PubMed] [Google Scholar]
- 3.Fischer JJ, Samady H, McPherson JA, et al. Comparison between visual assessment and quantitative angiography versus fractional flow reserve for native coronary narrowings of moderate severity. Am J Cardiol. 2002;90:210–215. doi: 10.1016/s0002-9149(02)02456-6. [DOI] [PubMed] [Google Scholar]
- 4.Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703–1708. doi: 10.1056/NEJM199606273342604. [DOI] [PubMed] [Google Scholar]
- 5.Melikian N, De Bondt P, Tonino P, et al. Fractional flow reserve and myocardial perfusion imaging in patients with angiographic multivessel coronary artery disease. JACC Cardiovasc Interv. 2010;3:307–314. doi: 10.1016/j.jcin.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Pijls NH, Van Gelder B, Van der Voort P, et al. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995;92:3183–3193. doi: 10.1161/01.cir.92.11.3183. [DOI] [PubMed] [Google Scholar]
- 7.Nam CW, Hur SH, Koo BK, et al. Fractional flow reserve versus angiography in left circumflex ostial intervention after left main crossover stenting. Korean Circ J. 2011;41:304–307. doi: 10.4070/kcj.2011.41.6.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim JE, Koo BK. Fractional flow reserve: the past, present and future. Korean Circ J. 2012;42:441–446. doi: 10.4070/kcj.2012.42.7.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pijls NH, Sels JW. Functional measurement of coronary stenosis. J Am Coll Cardiol. 2012;59:1045–1057. doi: 10.1016/j.jacc.2011.09.077. [DOI] [PubMed] [Google Scholar]
- 10.Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11:171–185. doi: 10.1016/j.nuclcard.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Metz LD, Beattie M, Hom R, Redberg RF, Grady D, Fleischmann KE. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography: a meta-analysis. J Am Coll Cardiol. 2007;49:227–237. doi: 10.1016/j.jacc.2006.08.048. [DOI] [PubMed] [Google Scholar]
- 12.Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993;87:1354–1367. doi: 10.1161/01.cir.87.4.1354. [DOI] [PubMed] [Google Scholar]
- 13.De Bruyne B, Baudhuin T, Melin JA, et al. Coronary flow reserve calculated from pressure measurements in humans. Validation with positron emission tomography. Circulation. 1994;89:1013–1022. doi: 10.1161/01.cir.89.3.1013. [DOI] [PubMed] [Google Scholar]
- 14.Koo BK, Yang HM, Doh JH, et al. Optimal intravascular ultrasound criteria and their accuracy for defining the functional significance of intermediate coronary stenoses of different locations. JACC Cardiovasc Interv. 2011;4:803–811. doi: 10.1016/j.jcin.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Park SJ, Kang SJ, Ahn JM, et al. Visual-functional mismatch between coronary angiography and fractional flow reserve. JACC Cardiovasc Interv. 2012;5:1029–1036. doi: 10.1016/j.jcin.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Leone AM, De Caterina AR, Basile E, et al. Influence of the amount of myocardium subtended by a stenosis on fractional flow reserve. Circ Cardiovasc Interv. 2013;6:29–36. doi: 10.1161/CIRCINTERVENTIONS.112.971101. [DOI] [PubMed] [Google Scholar]
- 17.Kim HS, Tonino PA, De Bruyne B, et al. The impact of sex differences on fractional flow reserve-guided percutaneous coronary intervention: a FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) substudy. JACC Cardiovasc Interv. 2012;5:1037–1042. doi: 10.1016/j.jcin.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 18.Kang SJ, Ahn JM, Han S, et al. Sex differences in the visual-functional mismatch between coronary angiography or intravascular ultrasound versus fractional flow reserve. JACC Cardiovasc Interv. 2013;6:562–568. doi: 10.1016/j.jcin.2013.02.016. [DOI] [PubMed] [Google Scholar]