Abstract
Background and Objectives
There is little information about the relationship between the Doppler flow of the ophthalmic artery (OA) and carotid and coronary atherosclerosis. The aim of the investigation was to assess the clinical usefulness of the Doppler flow of the OA to estimate the severity of carotid and coronary atherosclerosis.
Subjects and Methods
The study was a retrospective analysis of the findings in 140 patients (mean age: 60 years, male: 64%) who underwent coronary angiography (CA) for the evaluation of typical angina between July 2010 and October 2011 in our single center. The severity of coronary artery stenosis was based on the Gensini score (GS). Significant coronary artery disease (CAD) was defined as the obstruction of over 75% of the major coronary arteries confirmed with CA. The pulsed Doppler flow of the OA and carotid ultrasound were performed before CA.
Results
The mean systolic velocity/mean diastolic velocity (MSV/MDV), pulsatile index and resistance index in the Doppler flow of the OA were identified as significant and independent correlations with carotid intima-media thickness, and MSV/MDV was identified to have a significant and independent correlation with the GS. MSV/MDV >2.1 was the independent predictor for significant CAD {odds ratio (OR) 3.8, 95% confidence interval (CI) 1.5-9.7, p=0.005} and carotid plaque (OR 2.8, 95% CI 1.1-7.0, p=0.028), after adjustment for CAD-associated factors.
Conclusion
The Doppler flow of the OA might be a useful predictor of the severity of carotid and coronary atherosclerosis.
Keywords: Atherosclerosis, Carotid arteries, Coronary vessels, Ophthalmic artery, Ultrasound
Introduction
Cardiovascular disease is closely related to the development of atherosclerosis with plaque formation on arterial walls.1) The measurement of arterial wall thickness has been used as a surrogate of the extent, severity, and progression of atherosclerosis.2) Carotid intima-media thickness (c-IMT) is a measure of anatomic disease and a significant predictor of acute coronary events associated with cardiovascular risk factors.2),3) Moreover, the c-IMT is associated with car-diovascular disease risk factors and the degree of atherosclerosis.3),4) These findings support that c-IMT measurement could be used as a surrogate marker of atherosclerosis.
For several decades, the retinal vasculature has been proposed as an easily and safely measured surrogate for coronary circulation.5),6),7),8),9) Recently, the hemodynamic Doppler pattern in the ophthalmic artery (OA) has been proposed as a predictor for systemic atherosclerosis, including coronary atherosclerosis.10)
The OA is the first major branch of the internal carotid artery, so changes of blood flow in the OA have provided insight into various vascular disorders, including carotid and coronary artery stenosis.11) There is little information on the relationship between the Doppler flow of the OA and carotid and coronary atherosclerosis. The aim of the investigation was to assess the clinical usefulness of the Doppler flow of the OA for estimating the severity of carotid and coronary atherosclerosis.
Subjects and Methods
Study population
The study was approved by the institutional review board of Daegu Catholic University Medical Center (Daegu, Korea). The study was a retrospective analysis of the findings in 140 patients who underwent coronary angiography (CA) to evaluate typical angina between July 2010 and October 2011 at our single center. A structured interview was performed and a clinical history was obtained in all patients before CA, including: 1) hypertension (blood pressure >140/90 mm Hg or use of antihypertensive agents),12) 2) diabetes (fasting glucose level >126 mg/dL or the need for insulin or oral antidiabetes drugs),13) 3) smoking (previously or currently), and 4) hyperlipidemia (low-density lipoprotein cholesterol >130 mg/dL or use of statins).14)
Coronary artery disease (CAD) was diagnosed by CA with projections in multiple views. CA was evaluated by experienced physicians from visual assessment, and the degree of coronary stenosis was determined. The extent and severity of coronary artery stenosis was based on the Gensini score (GS).15) To obtain the GS, the coronary arterial tree was divided into 14 segments, and the degree of stenosis was evaluated in each segment. A score of 1 was given for 1-25% stenosis, 2 for 26-50% stenosis, 4 for 51-75% stenosis, 8 for 76-90% stenosis, 16 for 91-99% and 32 for total occlusion. The score of each segment was then multiplied by a weighting factor that represented the importance of a lesion in that segment. The weighting factor was 5 for a left main lesion; 2.5 for a proximal left anterior descending (LAD) or left circumflex (LCX) lesion; 1.5 for a mid-segment LAD or LCX lesion, 1 for a lesion in the distal LAD, LCX, first diagonal branch, first obtuse marginal branch, right coronary artery, posterior descending artery or septal artery; and 0.5 for a lesion in the second diagonal or obtuse marginal branches. The products in each of the 14 segments were then summed to obtain the final GS. In this study, significant CAD was defined as obstruction of above 75% of the major coronary arteries confirmed in CA. Patients were divided into two groups according to the significance of the CAD; the CAD group and the non-CAD group. Inclusion criteria were patients at least 35 years old presenting for an evaluation of typical angina. Exclusion criteria for the study were patients with 1) previous revascularization, 2) acute myocardial infarction, 3) atrial fibrillation and/or severe ventricular arrhythmia, 4) severe aortic valve regurgitation, severe aortic valve stenosis, and hypertrophic obstructive cardiomyopathy, 5) poor left ventricular contractility (ejection fraction <30%), 6) >50% stenosis in common or internal carotid artery and/or the presence of audible bruits in the orbital area, and 7) retinal detachment and uncontrolled glaucoma.10)
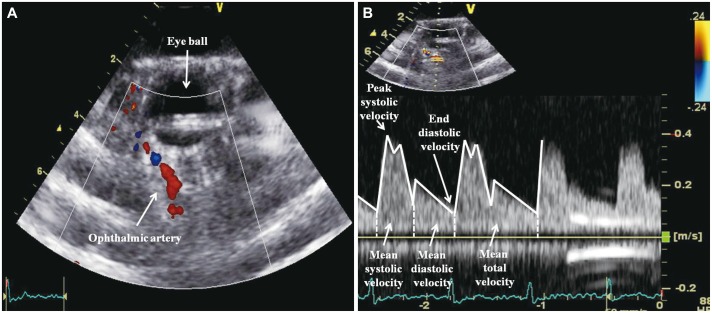
Evaluation of the Doppler flow of the ophthalmic artery
Doppler imaging of the OA was performed by the same operator, who had no knowledge of the clinical characteristics of patients.16) To perform the ultrasound measurement of OA, an M3S-D transducer with frequency range of 1.5-4.0 MHz (Vivid 7, General Electric Medical Systems, Wallingford, CT, USA) was used for this study. After 10 minutes of rest in the supine position followed by a blood pressure measurement, a pad of sterile ophthalmic gel was applied to the closed eyelid, and the probe was positioned gently with minimal pressure. The OA was identified as a large caliber vessel adjacent to the optic nerve. The sample volume marker lay approximately 40-50 mm from the eyelid, and the blood flow velocity of the OA was assessed with pulsed Doppler. Pulsed Doppler spectral analysis of the OA allows the determination of peak systolic velocity (PSV), end-diastolic velocity (EDV), mean systolic velocity (MSV), mean diastolic velocity (MDV), and mean total velocity (MTV) (Fig. 1). MSV, MDV and MTV were defined as the mean of the peak frequency envelope that outlines all the frequency peaks in systolic, diastolic, and all phases, respectively. The pulsatility index (PI) and resistive index (RI) are classical indices of vascular resistance.17) PI and RI were calculated as follows: PI={(PSV-MDV)/MTV}, and RI={(PSV-EDV)/PSV}. To evaluate the hemodynamics of the OA, we calculated the ratio of MSV to MDV (MSV/MDV).
Fig. 1.
The pulsed Doppler flow of the ophthalmic artery (OA). Color Doppler sonogram in the OA (A) and the corresponding spectral Doppler flow waveforms for the OA (B).
Carotid ultrasound
Carotid ultrasound examination was also performed in all patients. The c-IMT was defined as the greatest axial thickness in IMT at the carotid arteries. Carotid plaque was defined as a local thickening of the c-IMT of >50% compared to the surrounding vessel wall, a c-IMT >1.5 mm, or local thickening >0.5 mm.2)
Statistical analysis
All statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS) package for Windows version 17.0 (SPSS Inc., Chicago, IL, USA). The levels of normally distributed continuous variables were expressed as mean±standard deviation. Differences in frequencies were analyzed using the chi-square test. Differences in continuous variables between two groups were examined using the independent t-test. Univariate linear relationships between key variables were tested using Pearson's correlation coefficient. Mutivariate linear regression analysis was used to evaluate independent factors for the c-IMT. The best cut-off for diagnosing carotid plaque and significant CAD was defined as that yielding the highest sensitivity and specificity in the receiver-operating characteristic (ROC) curve.18) P<0.05 was considered statistically significant.
Results
Clinical, laboratory, angiographic and ultrasonographic characteristics
Baseline clinical and laboratory characteristics are shown in Table 1. The overall patient group consisted of 90 men (64.3%) and 50 women (35.7%) with a mean age of 60.4±9.9 years (median age: 60.5 years). The incidence of hypertension and diabetes were 43.6% and 32.1%, respectively. There were no differences of clinical and laboratory characteristics between the CAD group and the non-CAD group.
Table 1.
Clinical and laboratory characteristics
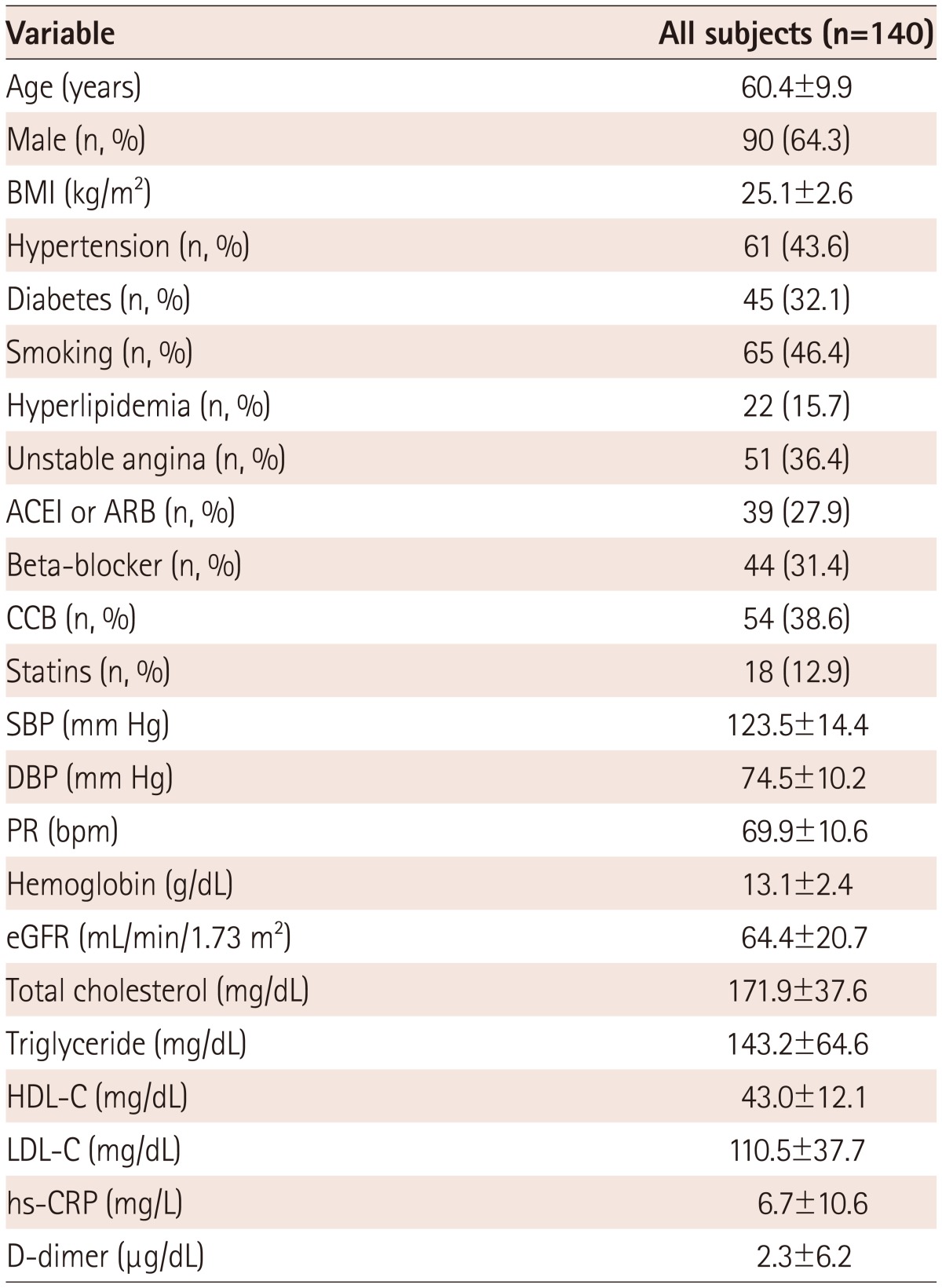
BMI: body mass index, ACEI: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker, CCB: calcium channel blocker, SBP: systolic blood pressure, DBP: diastolic blood pressure, PR: pulse rate, eGFR: estimated glomerular filtration rate, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, hs-CRP: high-sensitivity C-reactive protein
Quantitative coronary angiographic characteristics combined with the GS are shown in Table 2. The patients with significant CAD (>75% stenosis) were 51 (36.4%). Among the 51 patients, one-vessel disease was about one-third (39.2%) and two-vessel disease was about two-thirds (60.8%) of the population. In this study, the patients with three-vessel disease or left main disease were excluded. Among the 140 patients, the sum of stenotic segments was 214. Among the 214 segments, 104 (48.6%) showed significant CAD. In the analysis of the GS, the mean value of the GS was 25.2.
Table 2.
Gensini score and quantitative coronary angiographic analysis
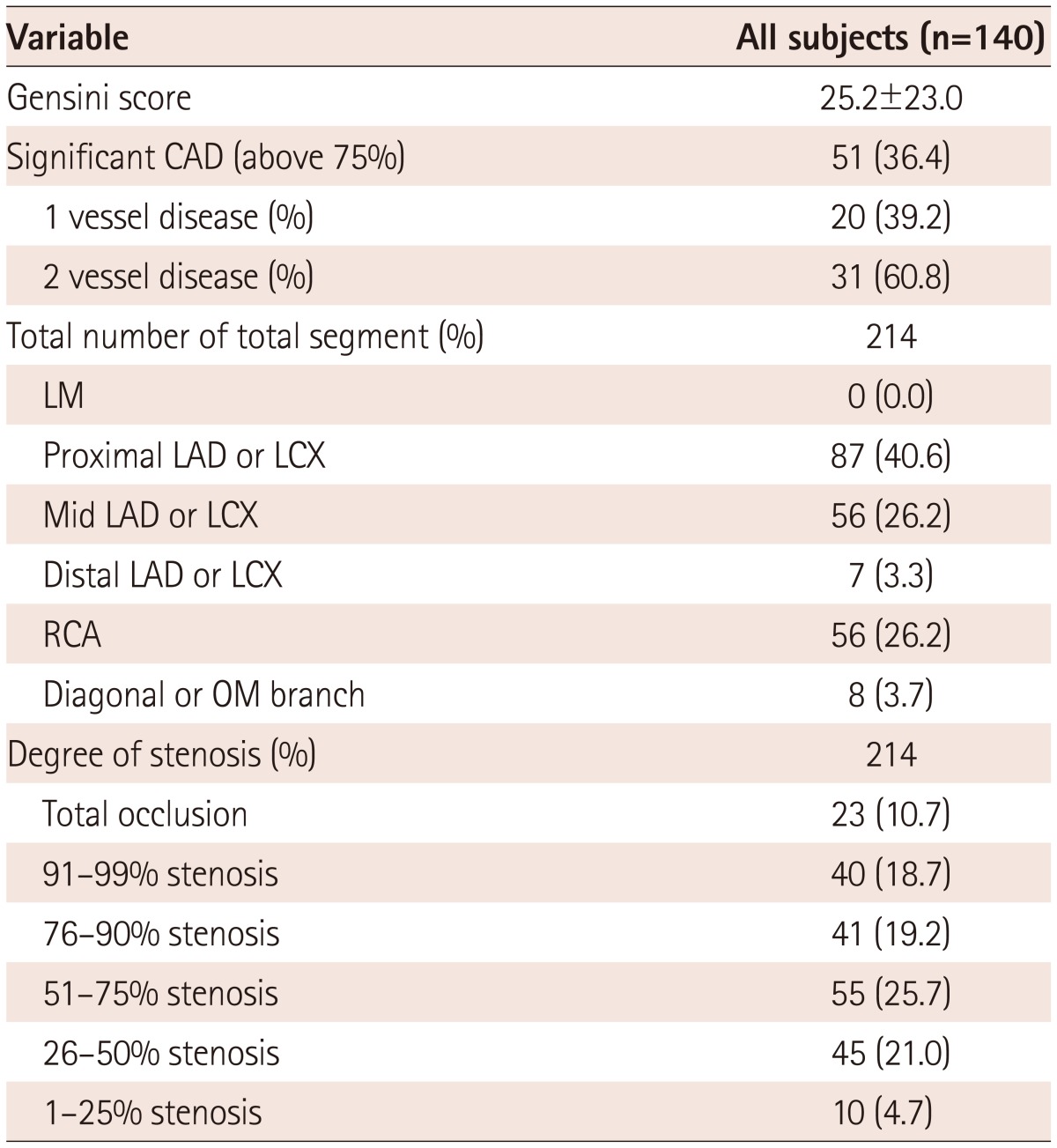
CAD: coronary artery disease, LM: left main coronary artery, LAD: left anterior descending coronary artery, LCX: left circumflex coronary artery, RCA: right coronary artery, OM: obtuse marginal coronary artery
Ultrasonographic characteristics are shown in Table 3-1. In the echocardiographic characteristics, the left ventricular ejection fraction (LV EF) tended to decrease more in the CAD group than in the non-CAD group. In the carotid ultrasound parameters, c-IMT and the incidence of carotid plaque were significantly higher in the CAD group than in the non-CAD group. In the Doppler flow of the OA, EDV and MDV were significantly lower in the CAD group than in the non-CAD group. MSV/MDV, PI, and RI were significantly higher in the CAD group than in the non-CAD group. Correlations between the Doppler flow of the OA are shown in Table 3-2. MSV/MDV showed a significantly positive correlation with RI and PI. However, MSV/MDV showed a significantly negative correlation with EDV and MDV.
Table 3-1.
Ultrasonographic characteristics
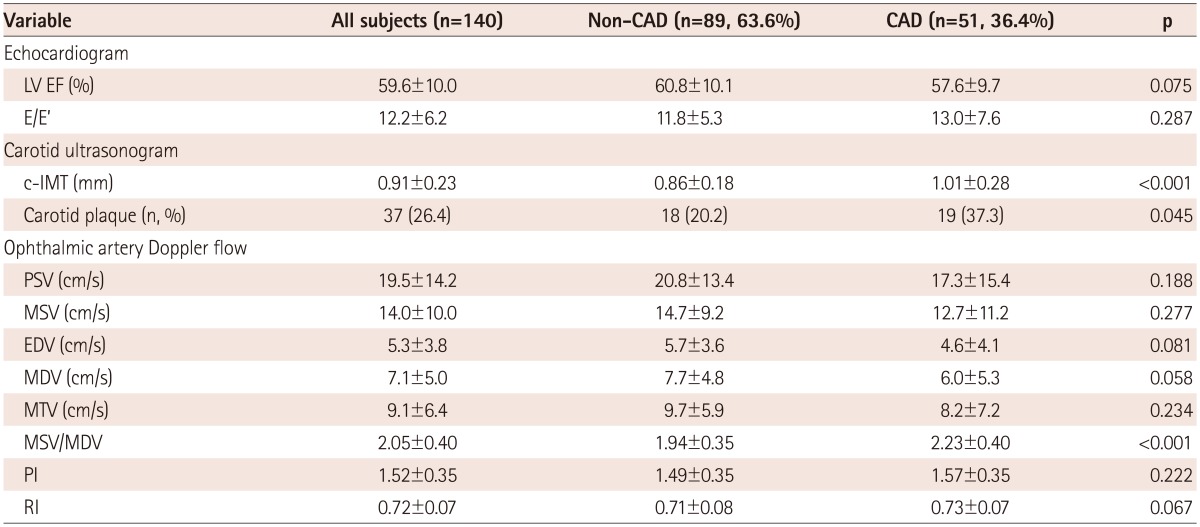
CAD: coronary artery disease, LV: left ventricular, EF: ejection fraction, c-IMT: carotid intima-media thickness, PSV: peak systolic velocity, MSV: mean systolic velocity, EDV: end-diastolic volume, MDV: mean diastolic velocity, MTV: mean total velocity, PI: pulsatility index, RI: resistive index
Table 3-2.
Pearson's correlation coefficients for the relationship among parameters in ophthalmic artery Doppler
*p<0.05, †p<0.01. PSV: peak systolic velocity, MSV: mean systolic velocity, EDV: end-diastolic velocity, MDV: mean diastolic velocity, MTV: mean total velocity, PI: pulsatility index, RI: resistive index
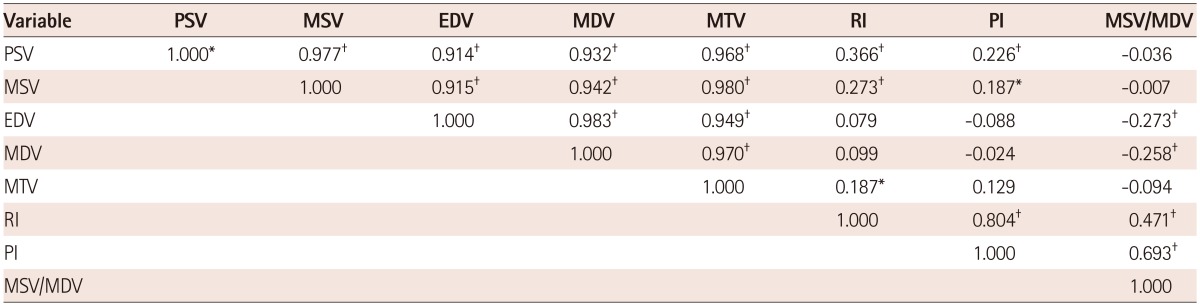
Correlation between the carotid intima-media thickness and the clinical, laboratory, and ultrasonographic parameters
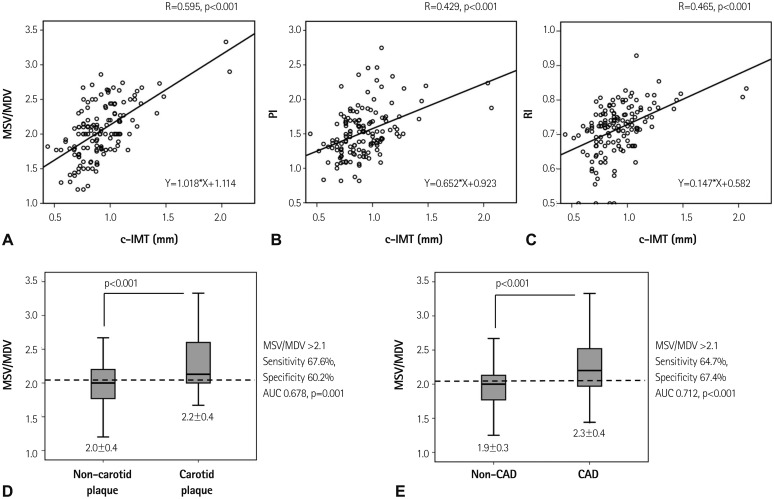
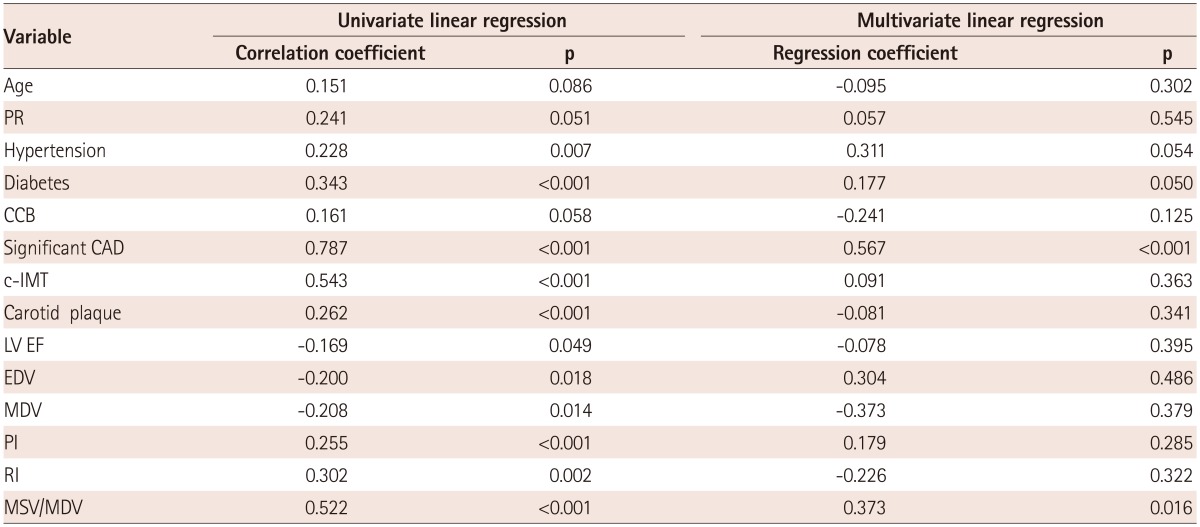
The correlation between the c-IMT and clinical, laboratory, and ultrasonographic parameters is shown in Table 4. In the correlation between the c-IMT and clinical parameters, the c-IMT is significantly positively correlated with age, pulse rate, GS, and the presence of hypertension, diabetes, calcium channel blockers, significant CAD, and carotid plaque. In the correlation between the c-IMT and laboratory parameters, it was found that the c-IMT did not correlate significantly with laboratory parameters. In the correlation between the c-IMT and the echocardiographic parameters, the c-IMT was significantly positively correlated with E/E'. In the correlation between the c-IMT and the Doppler flow of the OA, the c-IMT was significantly negatively correlated with EDV and MDV. However, the c-IMT was significantly positively correlated with MSV/MDV, PI, and RI (Fig. 2A-C). The clinical and ultrasonographic parameters that correlated with the c-IMT, were entered into a multivariate logistic linear regression. Among several parameters, MSV/MDV, PI, and RI were identified as significant and independent factors of the c-IMT (Table 4).
Table 4.
Univariate and multivariate linear regression for the c-IMT
c-IMT: carotid intima-media thickness, PR: pulse rate, CCB: calcium channel blocker, CAD: coronary artery disease, EDV: end-diastolic velocity, MDV: mean diastolic velocity, PI: pulsatility index, RI: resistive index, MSV: mean systolic velocity
Fig. 2.
Correlation between the carotid intima-media thickness (c-IMT) and the Doppler flow of the ophthalmic artery. Mean systolic velocity/mean diastolic velocity (MSV/MDV), pulsatility index (PI), and resistive index (RI) were significantly correlated with the c-IMT (A-C). The optimal cut-off value of MSV/MDV for the prediction of carotid plaque (D) and significant coronary artery disease (CAD) defined as coronary artery stenosis greater than 75% (E). AUC: area under the curve.
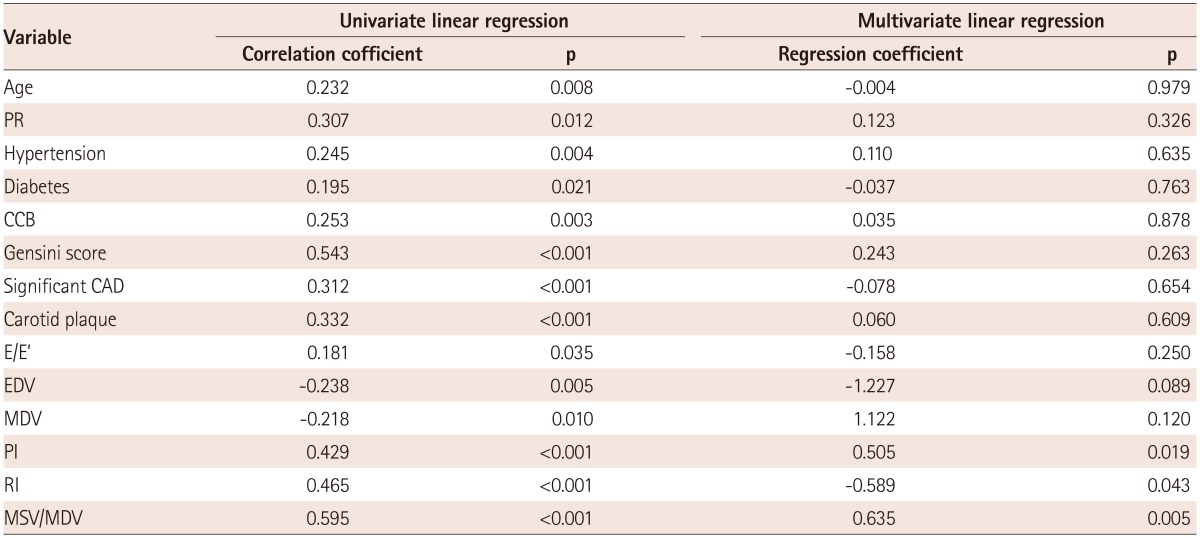
Correlation between the Gensini score and the clinical, laboratory, and ultrasonographic parameters
Correlation between the GS and clinical, laboratory, and ultrasonographic parameters is shown in Table 5. In the correlation between the GS and clinical parameters, the GS was significantly positively correlated with c-IMT and the presence of hypertension, diabetes, significant CAD, and carotid plaque. The GS did not correlate significantly with laboratory parameters. The GS was significantly negatively correlated with LV EF. In the correlation between the GS and the Doppler flow of the OA, the GS was significantly negatively correlated with EDV and MDV. However, the GS was significantly positively correlated with MSV/MDV, PI, and RI. The clinical and ultrasonographic parameters that correlated with the GS, were entered into multivariate a logistic linear regression. Among several parameters, MSV/MDV and the presence of significant CAD were identified as significant and independent factors of the GS (Table 5).
Table 5.
Univariate and multivariate linear regression for the Gensini score
PR: pulse rate, CCB: calcium channel blocker, CAD: coronary artery disease, c-IMT: carotid intima-media thickness, LV EF: left ventricular ejection fraction, EDV: end-diastolic velocity, MDV: mean diastolic velocity, PI: pulsatility index, RI: resistive index, MSV: mean systolic velocity
Clinical value of mean systolic velocity/mean diastolic velocity as predictor for carotid plaque and significant coronary artery disease
In ROC curve, the optimal cut-off value of MSV/MDV for the prediction of carotid plaque was 2.1, with a relatively low sensitivity of 67.6% and specificity of 60.2. The optimal cut-off value of MSV/MDV for the prediction of significant CAD is 2.1, with a relatively low sensitivity of 64.7% and specificity of 67.4% (Fig. 2D and E).
Discussion
In our study, we demonstrated a close relationship between the Doppler flow of the OA, the c-IMT, and the GS. MSV/MDV, PI, and RI in the Doppler flow of the OA were significantly and independently correlated with c-IMT. Also, MSV/MDV significantly and independently correlated with the GS. Although there was low sensitivity and specificity in the prediction of significant CAD and carotid plaque, patients with MSV/MDV >2.1 are 3.8-fold higher than the patients with MSV/MDV ≤2.1 for the prediction of CAD after adjustment for CAD-associated factors. Also, in the prediction of carotid plaque, the patients with MSV/MDV >2.1 were 2.8-fold higher than the patients with MSV/MDV ≤2.1 after adjustment for CAD-associated factors. On the basis of these results, the patients with high MSV/MDV values may reflect the severity of coronary atherosclerosis, and carotid plaque.
A few studies have reported normal velocity values of the Doppler flow of the OA.19) In the measurement of the OA, the transducer with ultrasound Doppler high frequency of higher than 7 MHz of ultrasound was generally used because the OA is a superficial artery. In transducers with ultrasounds higher than 7 MHz, normal velocity values of PSV have been reported as 31.4-39.6 cm/second, and normal velocity values of EDV were reported as 8.2-10.6 cm/second. In addition, the normal velocity value of RI was reported as 0.77.19) Normal velocity values of MSV, MDV, MTV, and PI have not yet been reported. In our study, mean values of PSV and EDV were 19.5 cm/second and 5.3 cm/second, respectively. The mean value of RI was 0.72. There are several reasons for the difference between the mean value in PSV and EDV. First, the transducer used in our study was a cardiac probe with a low frequency range of 1.5-4.0 MHz, which was both a useful and simple way to take an OA measurement after the echocardiogram. Due to the difference of the transducer's frequency, the mean value of OA parameters in our study is lower than the mean value of OA parameters in previous studies.19) Second, the mean age of our study (60 years) was 10 years older than mean age of previous studies (50 years).19) The Doppler flow of the OA decreases with age. Therefore, the difference of mean age could affect the low mean value in the Doppler of the OA. However, RI, such as the ratio of OA parameters, was similar to a previous study.19) On this basis, that ratios were consistent with previous studies, the MSV/MDV would be similar to previous studies.19) Therefore, in our study, the MSD/MDV ratio was more important than the values of PSV, EDV, MSV, and MDV.
Risk factors for coronary atherosclerosis, such as age, hypertension, diabetes, cigarette smoking, hyperlipidemia, chronic kidney disease, and others, have been well established in both the literature and clinical practice as ways to identify and treat susceptible individuals.20),21),22),23),24),25) However, there continues to be interest in finding methods and other markers that will allow us to further risk-stratify patients. Retinal vasculature imaging and the Doppler flow of the OA have been cited as potential other markers for this purpose. In several studies, the retinal vasculature has been proposed as an easily and safely measured surrogate for the coronary circulation.5),6),7),8),9) However, the studies about the relationship between the Doppler flow of the OA and systemic atherosclerosis, including carotid and coronary atherosclerosis, are minimal and conclusions remain unclear.
The OA is the first major branch of the internal carotid artery, and it divides into many branches within the orbital area.11) Doppler imaging of the OA was recently made possible by improvements in Doppler equipment. Changes in the Doppler flow readings of the OA have provided new insights into various vascular disorders, including ocular vascular disease, carotid artery stenosis, and metabolic disorders.19) The technical reproducibility of OA Doppler imaging was well-established in the ophthalmological field with sufficient observer experience.26),27) The OA is representative of the peripheral arteries and confers anatomical advantages for detecting the Doppler flow because of the absence of ultrasonic-positive obstacles such as bones and fat tissues, the good sonolucency of the eyeball, and the near-vertical angle of the OA to the transducer, which differs from the parallel-signaling of the carotid artery.19) Hemodynamic Doppler flow of the OA may reflect peripheral vascular resistance and systemic atherosclerosis, with previous reports showing atherosclerotic changes in retinal arteries through Doppler imaging.8),9) Also, the hemodynamic Doppler flow in the OA may reflect the severity of diabetes retinopathy.28) Fukuda et al.29) showed that the MSV/MDV in the Doppler flow of the OA is closely related with the age and severity of diabetic retinopathy. However, in patients without DM, studies about the relationship between the Doppler flow of the OA and the carotid and coronary atherosclerosis are few and the correlation remains unclear.
In carotid atherosclerosis, ultrasound evaluation of the carotid artery accurately diagnoses carotid artery stenosis. The c-IMT is well correlated with pathological measurements. And, the c-IMT is a potent predictor of myocardial infarction and stroke. For each 0.1 mm increase in common c-IMT, the risk of acute myocardial infarction increases by 11%.3) The c-IMT is a feature of arterial wall aging that is not synonymous with subclinical atherosclerosis; however, it is related to it because the cellular and molecular alterations that underlie intima-media thickening have been implicated in the development, progression, or both, of atherosclerosis.2) However, additional images may provide further information on the hemodynamics of the internal carotid artery, including the Doppler flow of the OA. The Doppler flow of the OA may reflect the hemodynamics of proximal carotid stenosis, the flow direction of the OA, and the possibility of a hemodynamically significant lesion distal to the bifurcation of the carotid artery.11) Regarding the relation of the Doppler flow of the OA and carotid atherosclerosis, studies of carotid artery stenosis have shown a decrease in blood flow velocities in the central retinal artery, the OA, or both, when the stenosis was greater than 70% although the sensitivity was low and reverse flow occurred in 92% of occlusions, but only in 47% of severe stenosis cases, as we observed.30) Furthermore, high levels of RI in the Doppler flow of the OA seem to reflect diminished arterial compliance caused by systemic atherosclerosis.14) The results of these studies confirm the need for careful examination of the carotid artery in cases of low velocities found in the OA Doppler flow. Conversely, measurement of the OA Doppler flow in carotid artery stenosis could be valuable in evaluating the distal consequences of such stenosis and in relating chronic ischemic ocular syndrome to the presence of a severe carotid artery stenosis.19) In our study, MSV/MDV, RI, and PI offered useful predictions for carotid atherosclerosis, and MSV/MDV was a useful predictor for carotid plaque.
Regarding the relation of the Doppler flow of the OA to coronary atherosclerosis, atherosclerotic changes in retinal arteries are potential markers of systemic cardiovascular disease.8),9) Recently, Maruyoshi et al.10) reported that high MSV/MDV levels on the Doppler flow of the OA could reflect the presence of CAD, defined as coronary artery stenosis greater than 75%, and, were a potentially useful parameter for CAD screening. In our study, high values of MSV/MDV may reflect the coronary atherosclerosis severity, and might be associated with significant CAD.
There are several limitations to this study. First, the number of subjects was limited due to the retrospective nature of the study, and because it took place in a single center. Although our patient population was homogeneous, it represents a small percentage of the patients with CAD. In addition, our study was cross-sectional, and therefore, the clinical usefulness of our findings is relatively limited. Second, normal reference values in the Doppler flow of the OA are not yet known. The OA includes the extra-cranial artery; however, the carotid and coronary arteries are include the intra-cranial artery. The lack of a normal reference value and the effect due to the different anatomical location should be verified by further investigation. Third, this study did not include medical interventions. Fourth, this study did not include the vascular changes of the retina. Retinal arterial changes are associated with systemic atherosclerosis. In particular, hypertensive and diabetic retinopathy are closely linked to systemic atherosclerosis. The relationship between the vascular changes on the retina and the Doppler flow of the OA should be verified by further investigation. A more reproducible technique and large-scale studies with normal reference value are required to increase the clinical applicability of the Doppler flow of the OA for the prediction of carotid and coronary atherosclerosis.
In conclusion, the Doppler flow of the OA might reflect the severity of carotid and coronary atherosclerosis. In particular, high values of the MSV/MDV might reflect the severity of systemic atherosclerosis with the carotid and coronary atherosclerosis. In addition, high values of the MSV/MDV might be associated with carotid plaque and significant CAD. On the basis of this result, the Doppler flow of the OA might be useful to evaluate CAD and systemic atherosclerosis. Nevertheless, before its clinical utilization, further studies are required to corroborate its value.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Burger-Kentischer A, Göbel H, Kleemann R, et al. Reduction of the aortic inflammatory response in spontaneous atherosclerosis by blockade of macrophage migration inhibitory factor (MIF) Atherosclerosis. 2006;184:28–38. doi: 10.1016/j.atherosclerosis.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 2.Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. quiz 189-90. [DOI] [PubMed] [Google Scholar]
- 3.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 4.Zielinski T, Dzielinska Z, Januszewicz A, et al. Carotid intima-media thickness as a marker of cardiovascular risk in hypertensive patients with coronary artery disease. Am J Hypertens. 2007;20:1058–1064. doi: 10.1016/j.amjhyper.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 5.Ralph RA. Prediction of cardiovascular status from arteriovenous crossing phenomena. Ann Ophthalmol. 1974;6:323–326. [PubMed] [Google Scholar]
- 6.Michelson EL, Morganroth J, Nichols CW, MacVaugh H., 3rd Retinal arteriolar changes as an indicator of coronary artery disease. Arch Intern Med. 1979;139:1139–1141. [PubMed] [Google Scholar]
- 7.Gillum RF. Retinal arteriolar findings and coronary heart disease. Am Heart J. 1991;122(1 Pt 1):262–263. doi: 10.1016/0002-8703(91)90796-k. [DOI] [PubMed] [Google Scholar]
- 8.Wong TY, Klein R, Klein BE, Tielsch JM, Hubbard L, Nieto FJ. Retinal microvascular abnormalities and their relationship with hypertension, cardiovascular disease, and mortality. Surv Ophthalmol. 2001;46:59–80. doi: 10.1016/s0039-6257(01)00234-x. [DOI] [PubMed] [Google Scholar]
- 9.Tedeschi-Reiner E, Strozzi M, Skoric B, Reiner Z. Relation of atherosclerotic changes in retinal arteries to the extent of coronary artery disease. Am J Cardiol. 2005;96:1107–1109. doi: 10.1016/j.amjcard.2005.05.070. [DOI] [PubMed] [Google Scholar]
- 10.Maruyoshi H, Kojima S, Kojima S, et al. Waveform of ophthalmic artery Doppler flow predicts the severity of systemic atherosclerosis. Circ J. 2010;74:1251–1256. doi: 10.1253/circj.cj-09-0866. [DOI] [PubMed] [Google Scholar]
- 11.Hu HH, Sheng WY, Yen MY, Lai ST, Teng MM. Color Doppler imaging of orbital arteries for detection of carotid occlusive disease. Stroke. 1993;24:1196–1203. doi: 10.1161/01.str.24.8.1196. [DOI] [PubMed] [Google Scholar]
- 12.European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–1053. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 13.ADA Statement. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36:67–74. doi: 10.2337/dc13-S067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 15.Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606. doi: 10.1016/s0002-9149(83)80105-2. [DOI] [PubMed] [Google Scholar]
- 16.Lieb WE, Cohen SM, Merton DA, Shields JA, Mitchell DG, Goldberg BB. Color Doppler imaging of the eye and orbit. Technique and normal vascular anatomy. Arch Ophthalmol. 1991;109:527–531. doi: 10.1001/archopht.1991.01080040095036. [DOI] [PubMed] [Google Scholar]
- 17.Yatsuka Y, Matsukubo S, Tsutsumi K, Kotegawa T, Nakamura K, Nakano S. Ophthalmic artery flow velocity after physical exercise in healthy men. Jpn J Ophthalmol. 1996;40:103–110. [PubMed] [Google Scholar]
- 18.Metz CE, Herman BA, Shen JH. Maximum likelihood estimation of receiver operating characteristic (ROC) curves from continuously-distributed data. Stat Med. 1998;17:1033–1053. doi: 10.1002/(sici)1097-0258(19980515)17:9<1033::aid-sim784>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 19.Tranquart F, Bergès O, Koskas P, et al. Color Doppler imaging of orbital vessels: personal experience and literature review. J Clin Ultrasound. 2003;31:258–273. doi: 10.1002/jcu.10169. [DOI] [PubMed] [Google Scholar]
- 20.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 21.Pearson TA, Blair SN, Daniels SR, et al. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106:388–391. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 22.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 23.Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 24.Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 25.Dzau VJ, Antman EM, Black HR, et al. The cardiovascular disease continuum validated: clinical evidence of improved patient outcomes: part I: Pathophysiology and clinical trial evidence (risk factors through stable coronary artery disease) Circulation. 2006;114:2850–2870. doi: 10.1161/CIRCULATIONAHA.106.655688. [DOI] [PubMed] [Google Scholar]
- 26.Matthiessen ET, Zeitz O, Richard G, Klemm M. Reproducibility of blood flow velocity measurements using colour decoded Doppler imaging. Eye (Lond) 2004;18:400–405. doi: 10.1038/sj.eye.6700651. [DOI] [PubMed] [Google Scholar]
- 27.Németh J, Kovács R, Harkányi Z, Knézy K, Sényi K, Marsovszky I. Observer experience improves reproducibility of color Doppler sonography of orbital blood vessels. J Clin Ultrasound. 2002;30:332–335. doi: 10.1002/jcu.10079. [DOI] [PubMed] [Google Scholar]
- 28.Päivänsalo M, Pelkonen O, Rajala U, Keinanen-Kiukaanniemi S, Suramo I. Diabetic retinopathy: sonographically measured hemodynamic alterations in ocular, carotid, and vertebral arteries. Acta Radiol. 2004;45:404–410. doi: 10.1080/02841850410005246. [DOI] [PubMed] [Google Scholar]
- 29.Fukuda M, Suzuki A, Okamoto N, Tsubakimori S. Investigation of Doppler ultrasound waveform indices in the ophthalmic artery: comparison between results in normal and diabetic eyes. Folia Ophthalmol Jpn. 1999;50:218–223. [Google Scholar]
- 30.Päivänsalo M, Riiheläinen K, Rissanen T, Suramo I, Laatikainen L. Effect of an internal carotid stenosis on orbital blood velocity. Acta Radiol. 1999;40:270–275. doi: 10.3109/02841859909175553. [DOI] [PubMed] [Google Scholar]