ABSTRACT
The threat of future influenza pandemics and their potential for rapid spread, morbidity, and mortality has led to the development of pandemic vaccines. We generated seven reassortant pandemic live attenuated influenza vaccines (pLAIVs) with the hemagglutinin (HA) and neuraminidase (NA) genes derived from animal influenza viruses on the backbone of the six internal protein gene segments of the temperature sensitive, cold-adapted (ca) A/Ann Arbor/60 (H2N2) virus (AA/60 ca) of the licensed seasonal LAIV. The pLAIV viruses were moderately to highly restricted in replication in seronegative adults; we sought to determine the biological basis for this restriction. Avian influenza viruses generally replicate at higher temperatures than human influenza viruses and, although they shared the same backbone, the pLAIV viruses had a lower shutoff temperature than seasonal LAIV viruses, suggesting that the HA and NA influence the degree of temperature sensitivity. The pH of HA activation of highly pathogenic avian influenza viruses was greater than human and low-pathogenicity avian influenza viruses, as reported by others. However, pLAIV viruses had a consistently higher pH of HA activation and reduced HA thermostability compared to the corresponding wild-type parental viruses. From studies with single-gene reassortant viruses bearing one gene segment from the AA/60 ca virus in recombinant H5N1 or pH1N1 viruses, we found that the lower HA thermal stability and increased pH of HA activation were associated with the AA/60 M gene. Together, the impaired HA acid and thermal stability and temperature sensitivity likely contributed to the restricted replication of the pLAIV viruses we observed in seronegative adults.
IMPORTANCE There is increasing evidence that the HA stability of influenza viruses depends on the virus strain and host species and that HA stability can influence replication, virulence, and transmission of influenza A viruses in different species. We investigated the HA stability of pandemic live attenuated influenza vaccine (pLAIV) viruses and observed that the pLAIV viruses consistently had a less stable HA than the corresponding wild-type influenza viruses. The reduced HA stability and temperature sensitivity of the pLAIV viruses may account for their restricted replication in clinical trials.
INTRODUCTION
Waterfowl and shorebirds are the reservoir of influenza A viruses in nature and are the pool from which pandemic influenza viruses arise (1, 2). Influenza A viruses are classified into subtypes based on the surface glycoproteins hemagglutinin (HA; 18 subtypes) and neuraminidase (NA; 11 subtypes), and influenza viruses with different combinations of these HA and NA proteins have been identified in birds (1–3). Avian influenza viruses may be transmitted to domestic birds and poultry, as well as a number of mammalian species, including swine, horses, dogs, and humans (1, 2, 4). Avian influenza viruses can be introduced into the human population after reassortment with circulating influenza A viruses or by directly infecting humans (1, 2). Influenza pandemics occur after transmission of animal influenza viruses to humans and if the viruses bearing novel HAs are able to spread from person to person (1, 2, 4).
It is not possible to predict when the next influenza pandemic will occur, or which influenza virus subtype will cause it. Within the past 2 decades, the cross-species transmission of a number of avian influenza viruses of low (H9N2, H7N2, H7N3, and H7N7) and high (H5N1, H7N3, and H7N7) pathogenicity into humans has caused infections of varying severity (5–10). This list now includes the recently emerged H7N9 influenza A virus outbreak in China (11). Thus, it is critical that strategies are developed to prevent or control future influenza pandemics caused by the introduction of novel influenza A viruses into the human population. Vaccines are the most effective strategy to prevent or lessen the severity of influenza.
Seasonal live attenuated influenza vaccine (LAIV) viruses are reassortant viruses that contain six genes from a cold-adapted (ca), temperature-sensitive (ts), attenuated (att) master donor virus (A/Ann Arbor/6/1960) (AA/60 ca) and the HA and NA glycoproteins of the wild-type (wt) virus to which the immune response is targeted (12–17). These vaccines are safe, infectious, immunogenic, nontransmissible, genetically stable, and efficacious (15–17).
Our laboratory in collaboration with MedImmune is exploring the utility of LAIVs as a strategy to protect against influenza viruses of pandemic potential using the AA/60 ca backbone of the licensed seasonal LAIVs because these seasonal vaccines are safe and highly effective. Thus far, we have generated and evaluated vaccines against seven different influenza virus subtypes in preclinical studies and phase I clinical trials in healthy adults (18–29). Although they replicated and were immunogenic and efficacious in mice and ferrets, the pandemic LAIV (pLAIV) viruses did not replicate efficiently in seronegative healthy adults (18–22), although some of the pLAIV viruses (e.g., H9N2 and H7N3) induced a robust immune response in vaccinees (21, 22).
Recent studies suggest that avian and human HAs differ in the pH of HA activation and thermal stability (30). The pH of HA activation can regulate the replication and virulence of influenza viruses in the environment and in different species (31–39), and it has been suggested that the pH of HA activation of H5 influenza viruses may play a role in the reduced infectivity of a highly pathogenic avian influenza (HPAI) vaccine virus in humans (40). The impact of HA stability and the pH of HA activation on replication of the reassortant AA/60 ca-based pLAIV viruses is currently unknown.
The purpose of this study was to explore explanations for the restricted replication observed with the pLAIV viruses in the phase I clinical trials. We evaluated 12 pairs of wt and ca influenza viruses representing seven subtypes derived from human-, avian-, and swine-origin influenza viruses to compare their temperature shutoff, pH of HA activation, and thermal stability. We found that the pLAIV viruses consistently exhibited lower HA thermal stability and increased pH of HA activation that was associated with the AA/60 M gene.
MATERIALS AND METHODS
Viruses.
The pairs of wt and ca influenza A viruses used in the present study included the following strains: A/California/7/09 (CA/09) (pH1N1), A/California/10/78 (CA/78) (H1N1), A/Ann Arbor/6/60 (AA/60) (H2N2), A/swine/Missouri/4296424/06 (sw/MO/06) (H2N3), A/Panama/99 (PA/99) (H3N2), A/Washington/897/80 (WA/80) (H3N2), A/Hong Kong/213/03 (HK/03) (H5N1), A/Vietnam/1203/04 (VN/04) (H5N1), A/teal/Hong Kong/W312/97 (teal/HK/97) (H6N1), A/chicken/British Columbia/CN-6/04 (BC/04) ca and A/chicken/British Columbia/CN-7/04 (wt) (H7N3), A/Netherlands/219/03 (NL/03) (H7N7), and A/chicken/Hong Kong/G9/97 (ck/HK/G9/97) (H9N2).
Teal/HK/97 was obtained from the influenza virus repository at St. Jude Children's Research Hospital, Memphis, TN. BC/CN-7/04 was provided by John Pasick, Canadian Food Inspection Agency, Winnipeg, Canada. HK/03, VN/04, NL/03, and CA/09 were provided by Nancy Cox and Alexander Klimov, Influenza Division, Centers for Disease Control and Prevention. Sw/MO/06 was provided by Juergen Richt (formerly Agricultural Research Service, USDA, Ames, IA). AA/60 was provided by MedImmune (Mountain View, CA). The ca viruses were derived as previously described and were manufactured and provided by MedImmune (23–29). The HA sequences of the reverse genetics derived ca viruses were identical to the wt virus sequences.
All viruses were propagated in the allantoic cavity of 9- to 11-day-old embryonated specific-pathogen-free hen's eggs. The wt and ca viruses used in the present study were passaged fewer than four times. Eggs inoculated with wt or ca viruses were incubated at 35 or 33°C, respectively. Allantoic fluid was harvested at 48 to 72 h postinoculation for all seasonal and low-pathogenicity avian and swine wt and ca viruses and 24 h after inoculation for highly pathogenic avian influenza viruses. The viruses were tested for hemagglutinating activity and stored at −80°C until use. The titer of each virus was determined with serial dilutions of virus in MDCK cells, and the 50% tissue culture infectious dose (TCID50) was calculated by the method developed by Reed and Muench (41).
SGR viruses.
Reassortant viruses were generated by using the eight-plasmid reverse genetics system (29, 42). The single-gene reassortant (SGR) viruses were generated by reverse genetics, by cotransfecting seven plasmids derived from either the VN/04 or CA/09 wt viruses and one of the six AA/60 ca internal gene plasmids or the AA/60 wt M gene plasmid into cocultured 293T and MDCK cells. The HA and NA sequences of the SGR viruses were confirmed by sequencing viral RNA.
Temperature shutoff plaque assay.
MDCK cells cultured to 100% confluence in six-well plates were inoculated with 100 μl of the wt and ca influenza viruses that were 10-fold serially diluted in L-15 medium from 10−1 to 10−8. The inoculum was incubated with the cells for 1 h at room temperature on a rocker. After 1 h, 3 ml of 2× L-15 media (supplemented with 1 M HEPES buffer, 7.5% NaHCO3, 200 mM l-glutamine, antibiotic/antimycotic, 0.5% phenol red) in an equal volume of 1.6% agarose (SeaKem) was added to each well, and the samples were left for 5 to 10 min until the agarose had hardened. The cell culture plates were then placed in weighted, water-tight metal containers and submerged in large water baths for 4 days at various temperatures (32, 35, 36, 37, 37.5, 38, 38.5, and 39°C). The temperature accuracy of the water baths is ±0.01°C. The plates were removed, the monolayers were stained with 0.8% crystal violet (Sigma), the plaques were counted, and the titers were expressed in PFU. The temperature shutoff was defined as the temperature at which at least a 100-fold reduction in PFU titer was observed compared to the titer at the permissive temperature of 32°C.
Activation pH syncytium assay.
The syncytium assay was performed as previously described (35–37). Briefly, Vero cells grown in six-well plates at 37°C were inoculated with the wt and ca viruses at a multiplicity of infection of 3. After 3 h, the monolayer was treated with trypsin and overlaid for 5 min with 100 μl of 0.1 M MES (2-(N-morpholino)ethanesulfonic acid) pH buffers from pH 4.9 to 6.0 (Hampton Research) with a 0.1 pH unit resolution. The buffer was neutralized using Dulbecco modified Eagle medium supplemented with 10% fetal bovine serum and 1% glutamine, and cells were incubated at 37°C for an additional 2 h. The cells were fixed and stained with a Hema 3 stat pack staining kit according to the manufacturer's protocol. The presence or absence of syncytium formation (three or more nuclei within a multinucleated cell) was observed under the microscope, and the highest pH at which syncytium formation was seen was recorded.
Hemolysis assay.
The hemolysis assay was performed as previously described (43). Briefly, viruses that were standardized to 128 HA units/50 μl were diluted 1:4 in a 1% human red blood cell (hRBC) suspension (Siemens) and then incubated on ice for 1 h. The erythrocytes were pelleted by centrifugation (72 × g for 10 min), and the supernatant was removed. Next, 200 μl of 0.1 M MES pH buffers from pH 4.9 to 6.0 (Hampton Research) in 0.1-U increments were added and incubated for 1 h at 37°C. The suspension was centrifuged again to pellet the hRBCs, 50 μl of the supernatant was transferred to 96-well plates (three replicates for each pH value), and the optical density was measured at 405 nm to measure the amount of hemoglobin released by hemolysis induced by virus-cell fusion. The reported results are means ± the standard deviations (SD) of three replicates at the indicated pH value.
Thermostability assay.
A previously described protocol was followed (44). Briefly, the wt and ca viruses were standardized to 128 HA units by diluting stock viruses in phosphate-buffered saline (PBS). The viruses were then incubated at 50°C in a water bath for various time intervals (0, 15, 30, 60, 120, 180, and 240 min). Next, 100 μl of heat treated virus was transferred to 96-well plates in quadruplicate and 2-fold serially diluted in 50 μl of PBS. The hemagglutination activity was tested by adding 50 μl of 0.5% turkey RBCs to each well, followed by incubation for 45 min to 1 h at room temperature. In separate experiments, the residual viral infectivity after heat treatment at 50°C was determined by titration on MDCK cells.
Statistical analysis.
The significance of difference between any two groups was assessed by a nonparametric Mann-Whitney test using Prism (GraphPad Software). P values of <0.05 are considered significant.
RESULTS
Cold-adapted viruses exhibit lower HA acid stability and thermostability than those of wt viruses.
The pH of HA activation is the pH at which the HA protein undergoes an irreversible conformational change that facilitates fusion of the viral envelope with the endosomal membrane (45, 46). The pH of HA activation differs between influenza virus subtypes and strains, ranging from approximately pH 4.6 to pH 6.0 (30, 47). The pH of HA activation was determined for all of the wt and ca virus pairs to evaluate whether differences existed in the activation pH of the HA proteins of the wt viruses and their ca counterparts and among the pLAIVs representing different influenza virus subtypes. The pH of HA activation was calculated by identifying the highest pH at which syncytium formation was observed in influenza virus-infected cells.
Human and low-pathogenicity avian influenza (LPAI) wt viruses had a pH of HA activation that ranged from 5.0 to 5.4, while the H5 and H7 HPAI viruses had a pH of HA activation ranging from 5.6 to 5.8 (Table 1). These results are consistent with previous reports (35–37). For each pair of viruses, the pH of HA activation of the ca virus exceeded that of its wt counterpart by at least 0.2 pH units (Table 1). The overall difference between the 12 wt and ca viruses was statistically significant (P < 0.05), as was the difference between each wt and ca virus pair. Thus, ca viruses were less acid stable than wt viruses.
TABLE 1.
pH of HA activation of wild-type and cold-adapted viruses
| Virus | Species of origin | Subtype | wt or ca | pHa |
pH of HA activation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 5.0 | 5.1 | 5.2 | 5.4 | 5.6 | 5.8 | 6.0 | |||||
| CA/09 | Swine | pH1N1 | wt | + | + | + | – | – | – | – | 5.2 |
| ca | + | + | + | + | – | – | – | 5.4 | |||
| CA/78 | Human | H1N1 | wt | + | + | – | – | – | – | – | 5.1 |
| ca | + | + | + | + | – | – | – | 5.4 | |||
| AA/60 | Human | H2N2 | wt | + | + | + | – | – | – | – | 5.2 |
| ca | + | + | + | + | – | – | – | 5.4 | |||
| sw/MO/06 | Swine | H2N3 | wt | + | + | – | – | – | – | – | 5.1 |
| ca | + | + | + | + | – | – | – | 5.4 | |||
| WA/80 | Human | H3N2 | wt | + | – | – | – | – | – | – | 5.0 |
| ca | + | + | + | + | – | – | – | 5.4 | |||
| PA/99 | Human | H3N2 | wt | + | + | – | – | – | – | – | 5.1 |
| ca | + | + | + | + | – | – | – | 5.4 | |||
| HK/03 | Avian HPAI | H5N1 | wt | + | + | + | + | + | – | – | 5.6 |
| ca | + | + | + | + | + | + | – | 5.8 | |||
| VN/04 | Avian HPAIb | H5N1 | wt | + | + | + | + | + | – | – | 5.6 |
| ca | + | + | + | + | + | + | – | 5.8 | |||
| teal/HK/97 | Avian LPAI | H6N1 | wt | + | + | + | – | – | – | – | 5.2 |
| ca | + | + | + | + | + | – | – | 5.6 | |||
| NL/03 | Avian HPAIb | H7N7 | wt | + | + | + | + | + | + | – | 5.8 |
| ca | + | + | + | + | + | + | + | 6.0 | |||
| ck/CN-7/BC/04 | Avian HPAIb | H7N3 | wt | + | + | + | + | + | – | – | 5.6 |
| ca | + | + | + | + | + | + | – | 5.8 | |||
| ck/HK/G9/97 | Avian LPAI | H9N2 | wt | + | + | + | + | – | – | – | 5.4 |
| ca | + | + | + | + | + | – | – | 5.6 | |||
+ or − indicates the presence or absence of syncytia, respectively.
The wt viruses were HPAI viruses; their ca counterparts were genetically modified by removing the multibasic cleavage site or were derived from highly related LPAI viruses.
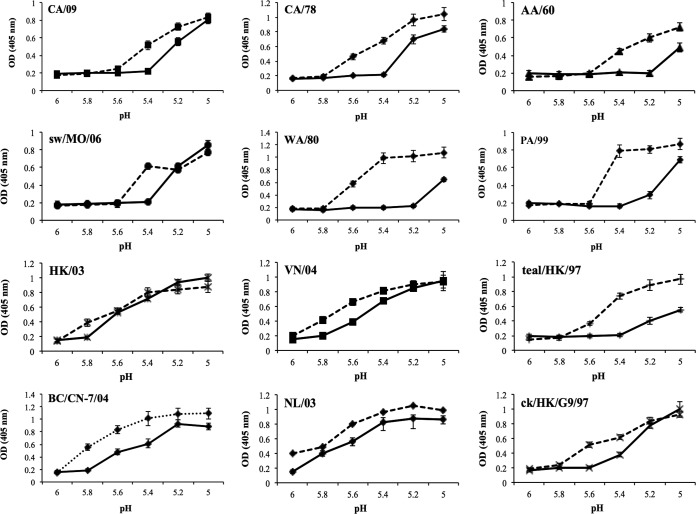
The pH of HA activation was also determined for each virus by a hemolysis assay in which release of hemoglobin is measured when the virus fuses with red blood cells at the pH of HA activation. Hemolysis occurred at a higher pH in the ca viruses compared to their wt counterparts, confirming the results of the syncytium assay (Fig. 1) that ca viruses are less acid stable than wt viruses.
FIG 1.
pH of HA activation of wt and ca viruses as determined by hemolysis. The amount of hemoglobin released by hemolysis induced by virus-cell fusion was measured to calculate the pH of HA activation for pairs of wt and ca viruses. For each graph, the solid lines represent the wt viruses, and the dotted lines represent the ca viruses. The results shown indicate means ± the SD of three replicates at the indicated pH value. OD, optical density.
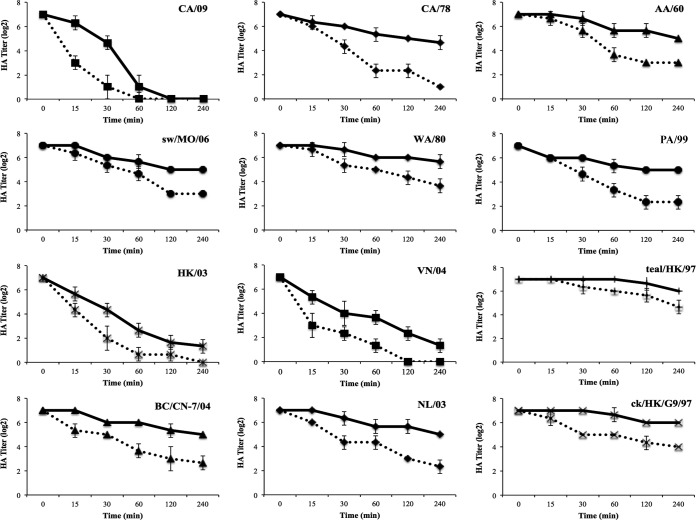
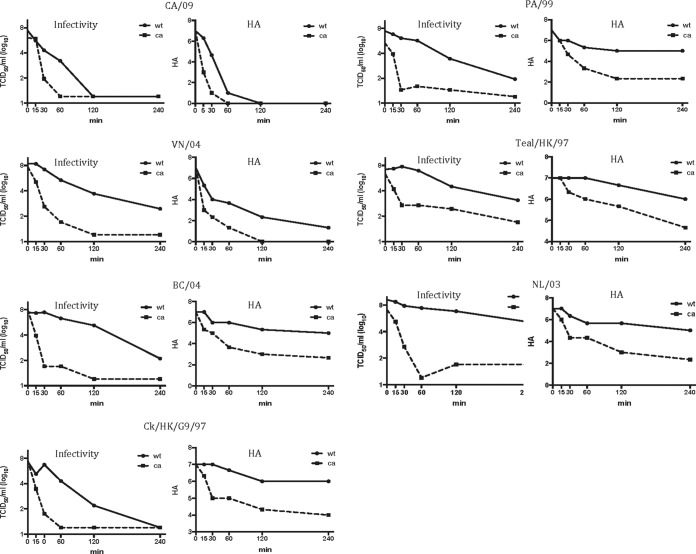
Heat treatment of influenza viruses at a neutral pH can induce the fusogenic form of the HA protein, allowing the use of a thermostability assay as a measure of HA stability (40, 48, 49). wt and ca viruses were incubated at 50°C for various durations, after which the loss of hemagglutination activity was determined. The HA titer of the ca viruses decreased more rapidly than that of the wt viruses, suggesting that the HA protein of the ca viruses has lower thermal stability than corresponding wt viruses (Fig. 2). The effect of incubation at 50°C for various durations on viral infectivity was also evaluated for selected viruses to determine whether the loss in hemagglutinating activity was associated with a function of the HA. The CA/09, PA/99, VN/04, teal/HK/97, BC/04, NL/03, and ck/HK/G9/97 wt and ca viruses were incubated at 50°C as described above, and residual virus titers were determined. The kinetics of the loss of infectivity and loss of HA activity of these viruses were similar (Fig. 3). Overall, these assays demonstrate that the HAs of ca viruses are less acid and heat stable than the HA of the corresponding wt viruses.
FIG 2.
HA protein thermal stability of wt and ca viruses. The hemagglutination activity (HA titer) was measured for pairs of wt and ca LAIV viruses that were incubated at 50°C for various time intervals. For each graph, the solid lines represent the wt viruses, and the dotted lines represent the ca viruses. The HA titers shown indicate means ± the SD of three replicates at the indicated time points.
FIG 3.
Comparison of the effect of heat treatment on viral infectivity and HA. The viral infectivity was measured for selected pairs of wt and ca LAIV viruses that were incubated at 50°C for various time intervals. These data were compared to data obtained with an HA thermostability study (shown in Fig. 2). For each graph, the solid lines represent the wt viruses, and the dotted lines represent the ca viruses.
The AA/60 M gene confers decreased HA stability.
With the exception of the ca H5N1, H7N3, and H7N7 pLAIV viruses, in which the multibasic amino acid motif in the connecting peptide of the HA of the highly pathogenic wt viruses was deleted, the HA proteins for each pair of wt and ca viruses were identical. Thus, the decreased stability of the HA protein is not likely to be due to changes in the HA. Instead, it is likely that a functional relationship between the HA and one or more of the AA/60 ca internal protein genes determines the decreased HA stability. Therefore, we sought to identify which AA/60 ca internal protein gene(s) was responsible for the decreased HA stability of these viruses. SGR viruses were constructed that were comprised of seven genes from the CA/09 wt or VN/04 wt virus and a single internal protein gene from the AA/60 ca virus. A VN/04 SGR virus expressing the AA/60 ca PB2 gene alone could not be rescued, so a virus expressing both PB1 and PB2 genes of AA/60 ca was generated, and this was compared to the VN/04 wt-AA/60 ca PB1 virus to identify potential effects of the AA/60 ca PB2 gene.
The pH of HA activation was determined for all of the CA/09 wt and VN/04 SGRs with the syncytium assay (Table 2). In both cases, the introduction of the AA/60 ca M gene into the wt virus resulted in decreased HA acid stability to the same extent as that of the VN/04 and CA/09 pLAIV viruses bearing all six internal protein genes of the AA/60 ca virus (Table 2). However, the other five internal protein genes of the AA/60 ca virus appeared to have no effect on the pH of HA activation (Table 2). These results suggest that the introduction of the AA/60 ca M gene alone can cause an increase in the pH of HA activation, resulting in decreased HA acid stability.
TABLE 2.
The M gene of the AA/60 ca virus confers an increase in the pH of HA activation
| Subtype | Virus | pHa |
pH of HA activation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 5.1 | 5.2 | 5.4 | 5.6 | 5.7 | 5.8 | 6.0 | |||
| pH1N1 | CA/09 wt | + | + | – | – | – | – | – | 5.2 |
| CA/09 ca | + | + | + | – | – | – | – | 5.4 | |
| CA/09 (AA/60 ca PB2) | + | + | – | – | – | – | – | 5.2 | |
| CA/09 (AA/60 ca PB1) | + | + | – | – | – | – | – | 5.2 | |
| CA/09 (AA/60 ca PA) | + | + | – | – | – | – | – | 5.2 | |
| CA/09 (AA/60 ca M) | + | + | + | – | – | – | – | 5.4 | |
| CA/09 (AA/60 ca NP) | + | + | – | – | – | – | – | 5.2 | |
| CA/09 (AA/60 ca NS) | + | + | – | – | – | – | – | 5.2 | |
| H5N1 | VN/04 wt | + | + | + | + | – | – | – | 5.6 |
| VN/04 ca | + | + | + | + | + | + | – | 5.8 | |
| VN/04 (AA/60 ca PB2) | + | + | + | + | – | – | – | 5.6 | |
| VN/04 (AA/60 ca PB2+PB1) | + | + | + | + | – | – | – | 5.6 | |
| VN/04 (AA/60 ca PA) | + | + | + | + | – | – | – | 5.6 | |
| VN/04 (AA/60 ca M) | + | + | + | + | + | + | – | 5.8 | |
| VN/04 (AA/60 ca NP) | + | + | + | + | – | – | – | 5.6 | |
| VN/04 (AA/60 ca NS) | + | + | + | + | – | – | – | 5.6 | |
+ or − indicates the presence or absence of syncytia, respectively.
Next, we determined whether the decreased HA acid stability observed with the introduction of the AA/60 ca M gene was due to a constellation effect of a gene from the AA/60 virus in the background of the CA/09 or VN/04 viruses, the presence of the single coding mutation within the M gene of the AA/60 ca virus, or both by using previously constructed VN/04 reassortant viruses (50) on AA/60 wt or ca backbones. We explored this possibility because the phenotype associated with any influenza virus gene segment may be altered when it occurs in the context of a different set of associated gene segments in a reassortant influenza virus due to interactions between gene segments. These gene constellation effects can be separate from the effect of point mutations and may ameliorate or enhance the latter. The presence of the AA/60 wt backbone resulted in a slight increase in the pH of HA activation (0.1 pH units) compared to that for the VN/04 wt virus, while the presence of the AA/60 ca backbone resulted in a larger increase in the pH of HA activation (at least 0.2 pH units), likely due to the presence of the AA/60 M gene (Table 3). The presence or absence of the multibasic cleavage site had no apparent effect on the HA acid stability of the VN/04 recombinant viruses. The results with the VN/04 reassortants suggest that both the presence of the AA/60 wt M gene and the mutation in the AA/60 ca M gene affect the pH of HA activation.
TABLE 3.
pH of HA activation of H5N1 reassortant viruses
| Virus | pHa |
pH of HA activation | ||||
|---|---|---|---|---|---|---|
| 5.6 | 5.7 | 5.8 | 5.9 | 6.0 | ||
| VN/04 wt | + | – | – | – | – | 5.6 |
| rVN/04 wtb | + | – | – | – | – | 5.6 |
| rVN/04 ΔMBSc | + | – | – | – | – | 5.6 |
| rVN/04/AA wt | + | + | – | – | – | 5.7 |
| rVN/04/AA wt ΔMBS | + | + | – | – | – | 5.7 |
| rVN/04/AA ca | + | + | + | – | – | 5.8 |
| rVN/04/AA ca ΔMBS (VN/04 ca) | + | + | + | + | – | 5.9 |
+ or − indicates the presence or absence of syncytia, respectively.
The rVN/04 wt virus was generated by reverse genetics using all eight wt VN/04 gene segments.
MBS, multibasic cleavage site.
These results were confirmed using the AA/60 wt M and AA/60 ca M SGR viruses (Table 4). For the VN/04 viruses, the presence of the AA/60 wt M gene resulted in an increase of 0.3 U in the pH of HA activation, while the introduction of the AA/60 ca M gene resulted in a larger increase of 0.4 U (Table 4). For the CA/09 viruses, an increase of 0.1 U occurred after the introduction of the AA/60 wt M gene and 0.2 U with the AA/60 ca M gene (Table 4). These results were confirmed by a hemolysis assay (data not shown). Together, these results suggest that the decreased HA stability observed with the ca viruses is a result of a constellation effect with a further contribution from the presence of the point mutation at nucleotide 969, resulting in an Ala-to-Ser change at amino acid residue 86 of the M2 gene, in the AA/60 ca M gene.
TABLE 4.
Effect of AA/60 M wt and ca genes on the pH of HA activation
| Subtype | Virus | pHa |
pH of HA activation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 5.1 | 5.2 | 5.3 | 5.4 | 5.6 | 5.7 | 5.8 | 5.9 | 6.0 | |||
| H5N1 | VN/04 wt | + | + | + | + | + | – | – | – | – | 5.6 |
| VN/04 ca | + | + | + | + | + | + | + | + | + | 6.0 | |
| VN/04 (AA/60 M wt) | + | + | + | + | + | + | + | +b | – | 5.9 | |
| VN/04 (AA/60 M ca) | + | + | + | + | + | + | + | + | + | 6.0 | |
| pH1N1 | CA/09 wt | + | + | – | – | – | – | – | – | – | 5.2 |
| CA/09 ca | + | + | + | + | – | – | – | – | – | 5.4 | |
| CA/09 (AA/60 M wt) | + | + | + | – | – | – | – | – | – | 5.3 | |
| CA/09 (AA/60 M ca) | + | + | + | + | – | – | – | – | – | 5.4 | |
+ or − indicates the presence or absence of syncytia, respectively.
The number of syncytia was greatly reduced at pH 5.9.
Animal-origin ca viruses (pLAIV viruses) have a lower shutoff temperature than human-origin ca viruses.
The presence of ca and ts mutations in the internal gene segments of the AA/60 ca-based LAIV viruses permits efficient virus replication at 32 or 33°C but shuts off viral replication at 39°C (51, 52). This restricts replication of the LAIV virus primarily to the upper respiratory tract, where temperatures are cooler, and this is believed to contribute to the attenuation of the vaccine virus in humans (15, 51, 53, 54). The exact shutoff temperatures for the pLAIV viruses were not known, nor were differences in shutoff temperatures among influenza viruses of different subtypes or different origins. Our aim was to see whether pLAIV viruses that were restricted in replication in adults had a different shutoff temperature than seasonal LAIV viruses.
To identify differences, plaque assays were performed to measure virus titers at several temperatures between 32 and 39°C. The shutoff temperatures are summarized in Table 5. As expected, all of the ca viruses were restricted in replication at 39°C, while the wt viruses replicated efficiently (Table 5). However, differences were observed among the different ca viruses. Cold-adapted pLAIV viruses bearing a swine-orgin (H2N3) or avian-origin (H5, H6, H7, and H9 viruses) HA had a lower shutoff temperature of 37.5°C than that for ca viruses with a human-origin HA (H1N1, H2N2, and H3N2), which exhibited a shutoff temperature of 38 or 39°C. Moreover, all of the human-origin ca viruses, except PA/99, had some plaques at 39°C, suggesting that these viruses are able to replicate to some degree at 39°C. In contrast, plaques were not seen at temperatures above 37.5°C for swine- and avian-origin ca pLAIV viruses. Thus, it appears that swine- and avian-origin ca pLAIV viruses have a more restricted temperature range of replication than that of human-origin LAIV viruses.
TABLE 5.
Shutoff temperatures of cold-adapted influenza viruses
| Virus | Subtype | Origin | Temp shutoff (°C)a | Presence of plaques at 39°C |
|---|---|---|---|---|
| CA/09 | pH1N1 | Human | 38 | Yes |
| CA/78 | H1N1 | Human | 38 | Yes |
| AA/60 | H2N2 | Human | 38 | Yes |
| PA/99 | H3N2 | Human | 38 | No (38.5°C) |
| WA/80 | H3N2 | Human | 39 | Yes |
| HK/03 | H5N1 | Avian | 37.5 | No |
| VN/04 | H5N1 | Avian | 37.5 | No |
| teal/HK/97 | H6N1 | Avian | 37.5 | No |
| ck/BC/04 | H7N3 | Avian | 37.5 | No |
| NL/03 | H7N7 | Avian | 37.5 | No |
| ck/HK/G9/97 | H9N2 | Avian | 37.5 | No |
| sw/MO/06 | H2N3 | Swine | 37.5 | No |
All wild-type viruses showed a temperature shutoff at temperatures above 39°C.
DISCUSSION
There is increasing evidence that HA stability of influenza viruses depends on the virus strain and host species and that HA stability can influence the replication, virulence, and transmission of influenza A viruses in different species (31–34, 38, 39). We were interested in exploring these reports because we have generated pLAIVs representing seven different HA subtypes derived from viruses isolated from different animal hosts, all on the backbone of the AA/60 ca virus, and have found that the infectivity of the pLAIV viruses for seronegative adults was unexpectedly restricted though seasonal LAIV viruses on the same backbone infect and replicate in the upper respiratory tract of seronegative adults and children. In agreement with other reports, we found that the HA stability of wild-type HPAI viruses was lower than that of human and LPAI viruses. However, irrespective of the origin of the HA and NA gene segments, we consistently observed that the pLAIV viruses had a less stable HA than the corresponding wt viruses. The M gene segment of the AA/60 ca virus confers this phenotype through a combination of gene constellation effects and a point mutation in the AA/60 ca M gene. In addition, we found a modestly more restricted temperature range of replication for avian- and swine-origin pLAIV viruses than for human-origin ca LAIV viruses on the same backbone. Together, the reduced HA acid and thermal stability and temperature sensitivity may account for the observed restricted replication of the pLAIV viruses in adults.
Human influenza viruses are more resistant to physical factors, such as low pH or elevated temperature exposure, than HPAI viruses (40). Our findings are consistent with reported data that human and LPAI viruses have pHs of HA activation that range from 5.1 to 5.4 and that the pH of HA activation for most human influenza viruses is lower than that of avian isolates of the same subtype (32). In contrast, HPAI viruses have a pH of HA activation ranging from 5.6 to 6.0 and are thus less stable in an acidic environment (40, 55). This phenotype is likely shaped by both host and viral determinants (31, 32, 35–37, 40). Changes in the pH of fusion and HA acid stability may allow influenza viruses to adapt to different hosts and cells (56, 57) and to develop resistance to antiviral agents that raise endosomal pH at high concentrations (43, 58–61).
The impact that differences in the acid stability of the HA protein have on influenza virus replication and virulence depends on the host species (31). In ducks, a high pH of fusion (pH 5.6 to 5.9) was essential for infectivity, shedding, and transmission of HPAI H5N1 viruses, and viruses with mutations that significantly increased or decreased the pH of HA activation were avirulent and nontransmissible (36). In chickens, an increase in the pH of activation of the H5 HA protein from 5.3 to 5.7 or 6.0 was associated with greater pathogenicity (37). In contrast, efficient infection of mammals appears to be associated with a lower optimum pH of HA activation (31, 32, 39, 40, 44). An H5N1 mutant virus with a decreased pH of HA activation that was attenuated in ducks, exhibited greater growth and virulence in mice, while mutations that destabilized HA acid stability attenuated viral replication in the respiratory tract of mice (31, 36, 37). In addition, an acid-stabilizing mutation enhanced replication of an H5N1 influenza virus in the upper respiratory tract of ferrets (32). Recombinant viruses containing the H5 HA from HPAI H5N1 viruses that were capable of transmitting efficiently via respiratory droplet between ferrets had a mutation that increased H5 HA stability (44). However, enhancement of HA stability alone is insufficient to confer HPAI H5N1 virus transmissibility in ferrets and requires additional mutations that confer α2,6-receptor binding specificity and removal of a glycosylation site within the head domain (32, 44). A mutation in the HA2 stalk region of the 2009 pH1N1 virus that has emerged, and is now predominant worldwide, increases HA pH and thermal stability, and viruses with this mutation showed increased infectivity in ferrets (39). This supports the idea that these factors are important for viral fitness in humans (39).
It is clear that the range of the pH of HA activation that is optimal for infection of mammals differs from the pH that is optimal for avian species, and increasing HA acid stability may represent a potential for mammalian adaptation (30, 36, 39). Our finding of a consistently increased pH of HA activation with AA/60 ca-based LAIV representing a variety of influenza virus subtypes suggests that the restricted replication observed with the AA/60 ca pLAIV viruses might be partly due to the decreased HA stability of these viruses. The higher pH of HA activation of the avian ca pLAIV viruses may not be optimal for efficient infectivity and may lead to restricted replication in humans. The acid instability of the ca pLAIV viruses may be more relevant in influenza viruses that have not yet adapted to humans because seasonal LAIV and the pH1N1 LAIV are clearly effective vaccines despite reduced acid stability of these ca viruses compared to that of the corresponding wt viruses. In their evaluation of a live attenuated H5N1 virus vaccine based on a deletion in the NS1 protein, Krenn et al. suggested that decreased HA acid stability played a critical role in the reduced infectivity of the vaccine virus in mice (40).
The decrease in pH and heat stability of the HA in our pLAIV viruses appears to involve the M gene segment. The M gene encodes two proteins, M1 and M2, and both are believed to interact with the HA protein (62–67). Previous studies have shown that the M2 protein plays a role in HA surface expression, transport, and pH stability (62, 63, 68), and an inverse correlation has been reported between M2 protein activity and HA pH stability (63). Differences in M2 activity of the pLAIV viruses compared to that of the corresponding wt virus may have a detrimental effect on the acid stability of the pLAIV viruses. The pLAIV viruses may be more suited to replication in cells with a higher endosomal pH (69). It is apparent from our study and others that the compatibility between HA and M requires an optimal functional interaction (63).
The effect of the M gene on HA stability of pLAIV viruses results from a combination of a gene constellation effect and the presence of a point mutation in the AA/60 ca M gene. The alanine-to-serine mutation at amino acid 86 of the cytoplasmic region of the M2 protein is the only difference between the AA/60 wt and ca M genes (70). An alignment of the M2 proteins of the viruses used in our study shows that the human influenza viruses encode an alanine at this position, whereas influenza viruses with an M2 protein of an animal origin encode a valine at this position. It is possible that this amino acid difference between human- and animal-origin M2 proteins significantly affects the HA stability of these viruses. A gene constellation effect can result from an incompatibility between the HA gene of certain influenza viruses and the AA/60 M gene. Grambas et al. showed that an acid-unstable HA protein from a highly pathogenic H7 influenza virus was incompatible with an M2 protein bearing mutations that attenuated its activity and, conversely, that certain M2 proteins were only compatible with an acid-stable HA (63). Perhaps the M2 protein of AA/60, which comes from an acid-stable H2N2 influenza virus, is less compatible with the HAs derived from acid-unstable viruses, such as H5 and H7 HPAI viruses, resulting in restricted replication.
LAIVs are administered intranasally to deliver the vaccine directly into the respiratory tract. Normal human airway epithelium is slightly acidic (pH 5.5 to 6.9) due to submucosal gland secretions that act as a primary innate defense mechanism against pathogens (71–73). The degree of acidification depends on submucosal gland distribution and might differ between species (40, 74). Acid secretion into the airways increases after irritation, inflammation, or influenza virus infection, decreasing the pH in the nasal passages down to a pH of 5.2 (31, 40, 75, 76). For effective viral replication, influenza viruses require a certain level of stability toward inactivating factors, such as acidic pH, heat, and chemical denaturants that promote the conformational change of HA into its fusogenic form, leading to viral inactivation (40, 48). An optimal range for the pH of HA activation is required that is low enough to avoid inactivation in the environment or in mildly acidic tissues (35, 77) but high enough to allow membrane fusion to occur before the virus is trafficked to the lysosome (35, 78). Influenza virus mutations that increase the pH of HA activation increase the susceptibility of the virus to acid inactivation (31). The higher pH of HA activation and decreased HA acid and heat stability of the pLAIV viruses may make them more susceptible to inactivation in the extracellular acidic environment of the respiratory tract or during transport to the cell surface if intracellularly cleaved HA proteins become prematurely triggered, limiting their replication efficiency in the human respiratory tract (31, 36, 61).
It may be possible to increase the replication of pLAIV viruses by introducing stabilizing mutations into the HA without modifying the AA/60 M gene. Several investigators have introduced mutations into the HA1 and HA2 subunits to increase the acid and heat stability of the HA protein, resulting in enhanced replication in mammals (31, 32, 35, 36, 39, 40). These residues have been mapped to various regions of the HA, including the fusion peptide pocket (35, 43, 59, 79), the coiled-coil regions of the HA2 subunit (35, 43, 59), the interface between the HA1 and HA2 subunits (35, 39, 43), and the vestigial esterase subdomain of the HA1 receptor-binding domain (37). Reassortant H5N1 viruses with an increased HA stability induced higher titers of neutralizing antibodies and a more robust systemic and local antibody response in mice than those for viruses with an unstable HA (40).
Overall, it is likely that the greater degree of temperature sensitivity and the HA stability contribute to the restricted replication of pLAIV viruses as observed in phase I clinical trials in seronegative healthy adults. The ability to generate effective pLAIVs is important in preparing for future influenza pandemics, and it may be worth modifying specific sites in the pLAIV viruses to enhance their replication in humans.
ACKNOWLEDGMENTS
This research was performed as part of a Cooperative Research and Development Agreement (CRADA no. AI-0155) between the Laboratory of Infectious Diseases, NIAID, and MedImmune.
This research was supported in part by the Intramural Research Program of the NIH, NIAID.
Footnotes
Published ahead of print 13 August 2014
REFERENCES
- 1.Luke CJ, Subbarao K. 2006. Vaccines for pandemic influenza. Emerg. Infect. Dis. 12:66–72. 10.3201/eid1201.051147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobasa D, Kawaoka Y. 2005. Emerging influenza viruses: past and present. Curr. Mol. Med. 5:791–803. 10.2174/156652405774962281. [DOI] [PubMed] [Google Scholar]
- 3.Tong S, Zhu X, Li Y, Shi M, Zhang J, Bourgeois M, Yang H, Chen X, Recuenco S, Gomez J, Chen LM, Johnson A, Tao Y, Dreyfus C, Yu W, McBride R, Carney PJ, Gilbert AT, Chang J, Guo Z, Davis CT, Paulson JC, Stevens J, Rupprecht CE, Holmes EC, Wilson IA, Donis RO. 2013. New world bats harbor diverse influenza A viruses. PLoS Pathog. 9:e1003657. 10.1371/journal.ppat.1003657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. 1992. Evolution and ecology of influenza A viruses. Microbiol. Rev. 56:152–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, Orr WK, Shortridge KF. 1999. Human infection with influenza H9N2. Lancet 354:916–917. [DOI] [PubMed] [Google Scholar]
- 6.Eames KT, Webb C, Thomas K, Smith J, Salmon R, Temple JM. 2010. Assessing the role of contact tracing in a suspected H7N2 influenza A outbreak in humans in Wales. BMC Infect. Dis. 10:141. 10.1186/1471-2334-10-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tweed SA, Skowronski DM, David ST, Larder A, Petric M, Lees W, Li Y, Katz J, Krajden M, Tellier R, Halpert C, Hirst M, Astell C, Lawrence D, Mak A. 2004. Human illness from avian influenza H7N3, British Columbia. Emerg. Infect. Dis. 10:2196–2199. 10.3201/eid1012.040961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fouchier RA, Schneeberger PM, Rozendaal FW, Broekman JM, Kemink SA, Munster V, Kuiken T, Rimmelzwaan GF, Schutten M, Van Doornum GJ, Koch G, Bosman A, Koopmans M, Osterhaus AD. 2004. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc. Natl. Acad. Sci. U. S. A. 101:1356–1361. 10.1073/pnas.0308352100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Subbarao K, Klimov A, Katz J, Regnery H, Lim W, Hall H, Perdue M, Swayne D, Bender C, Huang J, Hemphill M, Rowe T, Shaw M, Xu X, Fukuda K, Cox N. 1998. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279:393–396. 10.1126/science.279.5349.393. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. 2003. Update: influenza activity–United States and worldwide, 2002-03 season, and composition of the 2003-04 influenza vaccine. MMWR Morb. Mortal. Wkly. Rep. 52:516–521. [PubMed] [Google Scholar]
- 11.Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, Xu X, Lu H, Zhu W, Gao Z, Xiang N, Shen Y, He Z, Gu Y, Zhang Z, Yang Y, Zhao X, Zhou L, Li X, Zou S, Zhang Y, Li X, Yang L, Guo J, Dong J, Li Q, Dong L, Zhu Y, Bai T, Wang S, Hao P, Yang W, Zhang Y, Han J, Yu H, Li D, Gao GF, Wu G, Wang Y, Yuan Z, Shu Y. 2013. Human infection with a novel avian-origin influenza A (H7N9) virus. N. Engl. J. Med. 368:1888–1897. 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- 12.Maassab HF, Bryant ML. 1999. The development of live attenuated cold-adapted influenza virus vaccine for humans. Rev. Med. Virol. 9:237–244. . [DOI] [PubMed] [Google Scholar]
- 13.Ambrose CS, Luke C, Coelingh K. 2008. Current status of live attenuated influenza vaccine in the United States for seasonal and pandemic influenza. Influenza Other Respir. Viruses 2:193–202. 10.1111/j.1750-2659.2008.00056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. 2011. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP). 2011. MMWR Morb. Mortal. Wkly. Rep. 60:1128–1132. [PubMed] [Google Scholar]
- 15.Murphy BR, Coelingh K. 2002. Principles underlying the development and use of live attenuated cold-adapted influenza A and B virus vaccines. Viral Immunol. 15:295–323. 10.1089/08828240260066242. [DOI] [PubMed] [Google Scholar]
- 16.Luke C, Lakdawala SS, Subbarao K. 2012. Influenza vaccine-live. In Plotkin SA, Orenstein WA, Offit PA. (ed), Vaccines: expert consult—online and print, 6th ed. Elsevier/Saunders, Philadelphia, PA. [Google Scholar]
- 17.Buonagurio DA, Bechert TM, Yang CF, Shutyak L, D'Arco GA, Kazachkov Y, Wang HP, Rojas EA, O'Neill RE, Spaete RR, Coelingh KL, Zamb TJ, Sidhu MS, Udem SA. 2006. Genetic stability of live, cold-adapted influenza virus components of the FluMist/CAIV-T vaccine throughout the manufacturing process. Vaccine 24:2151–2160. [DOI] [PubMed] [Google Scholar]
- 18.Talaat KR, Karron RA, Liang PH, McMahon BA, Luke CJ, Thumar B, Chen GL, Min JY, Lamirande EW, Jin H, Coelingh KL, Kemble GW, Subbarao K. 2013. An open-label phase I trial of a live attenuated H2N2 influenza virus vaccine in healthy adults. Influenza Other Respir. Viruses 7:66–73. 10.1111/j.1750-2659.2012.00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Talaat KR, Karron RA, Luke CJ, Thumar B, McMahon BA, Chen GL, Lamirande EW, Jin H, Coelingh KL, Kemble G, Subbarao K. 2011. An open label phase I trial of a live attenuated H6N1 influenza virus vaccine in healthy adults. Vaccine 29:3144–3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karron RA, Talaat K, Luke C, Callahan K, Thumar B, Dilorenzo S, McAuliffe J, Schappell E, Suguitan A, Mills K, Chen G, Lamirande E, Coelingh K, Jin H, Murphy BR, Kemble G, Subbarao K. 2009. Evaluation of two live attenuated cold-adapted H5N1 influenza virus vaccines in healthy adults. Vaccine 27:4953–4960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Talaat KR, Karron RA, Callahan KA, Luke CJ, DiLorenzo SC, Chen GL, Lamirande EW, Jin H, Coelingh KL, Murphy BR, Kemble G, Subbarao K. 2009. A live attenuated H7N3 influenza virus vaccine is well tolerated and immunogenic in a phase I trial in healthy adults. Vaccine 27:3744–3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karron RA, Callahan K, Luke C, Thumar B, McAuliffe J, Schappell E, Joseph T, Coelingh K, Jin H, Kemble G, Murphy BR, Subbarao K. 2009. A live attenuated H9N2 influenza vaccine is well tolerated and immunogenic in healthy adults. J. Infect. Dis. 199:711–716. 10.1086/596558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Z, Santos C, Aspelund A, Gillim-Ross L, Jin H, Kemble G, Subbarao K. 2009. Evaluation of live attenuated influenza a virus h6 vaccines in mice and ferrets. J. Virol. 83:65–72. 10.1128/JVI.01775-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suguitan AL, Jr, McAuliffe J, Mills KL, Jin H, Duke G, Lu B, Luke CJ, Murphy B, Swayne DE, Kemble G, Subbarao K. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3:e360. 10.1371/journal.pmed.0030360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen H, Matsuoka Y, Swayne D, Chen Q, Cox NJ, Murphy BR, Subbarao K. 2003. Generation and characterization of a cold-adapted influenza A H9N2 reassortant as a live pandemic influenza virus vaccine candidate. Vaccine 21:4430–4436. [DOI] [PubMed] [Google Scholar]
- 26.Joseph T, McAuliffe J, Lu B, Vogel L, Swayne D, Jin H, Kemble G, Subbarao K. 2008. A live attenuated cold-adapted influenza A H7N3 virus vaccine provides protection against homologous and heterologous H7 viruses in mice and ferrets. Virology 378:123–132. 10.1016/j.virol.2008.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen GL, Lamirande EW, Yang CF, Jin H, Kemble G, Subbarao K. 2010. Evaluation of replication and cross-reactive antibody responses of H2 subtype influenza viruses in mice and ferrets. J. Virol. 84:7695–7702. 10.1128/JVI.00511-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Min JY, Vogel L, Matsuoka Y, Lu B, Swayne D, Jin H, Kemble G, Subbarao K. 2010. A live attenuated H7N7 candidate vaccine virus induces neutralizing antibody that confers protection from challenge in mice, ferrets, and monkeys. J. Virol. 84:11950–11960. 10.1128/JVI.01305-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Z, Wang W, Zhou H, Suguitan AL, Jr, Shambaugh C, Kim L, Zhao J, Kemble G, Jin H. 2010. Generation of live attenuated novel influenza virus A/California/7/09 (H1N1) vaccines with high yield in embryonated chicken eggs. J. Virol. 84:44–51. 10.1128/JVI.02106-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galloway SE, Reed ML, Russell CJ, Steinhauer DA. 2013. Influenza HA subtypes demonstrate divergent phenotypes for cleavage activation and pH of fusion: implications for host range and adaptation. PLoS Pathog. 9:e1003151. 10.1371/journal.ppat.1003151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zaraket H, Bridges OA, Russell CJ. 2013. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus replication and pathogenesis in mice. J. Virol. 87:4826–4834. 10.1128/JVI.03110-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zaraket H, Bridges OA, Duan S, Baranovich T, Yoon SW, Reed ML, Salomon R, Webby RJ, Webster RG, Russell CJ. 2013. Increased acid stability of the hemagglutinin protein enhances H5N1 influenza virus growth in the upper respiratory tract but is insufficient for transmission in ferrets. J. Virol. 87:9911–9922. 10.1128/JVI.01175-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ilyushina NA, Govorkova EA, Russell CJ, Hoffmann E, Webster RG. 2007. Contribution of H7 haemagglutinin to amantadine resistance and infectivity of influenza virus. J. Gen. Virol. 88:1266–1274. 10.1099/vir.0.82256-0. [DOI] [PubMed] [Google Scholar]
- 34.Keleta L, Ibricevic A, Bovin NV, Brody SL, Brown EG. 2008. Experimental evolution of human influenza virus H3 hemagglutinin in the mouse lung identifies adaptive regions in HA1 and HA2. J. Virol. 82:11599–11608. 10.1128/JVI.01393-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reed ML, Yen HL, DuBois RM, Bridges OA, Salomon R, Webster RG, Russell CJ. 2009. Amino acid residues in the fusion peptide pocket regulate the pH of activation of the H5N1 influenza virus hemagglutinin protein. J. Virol. 83:3568–3580. 10.1128/JVI.02238-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reed ML, Bridges OA, Seiler P, Kim JK, Yen HL, Salomon R, Govorkova EA, Webster RG, Russell CJ. 2010. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity and transmissibility in ducks. J. Virol. 84:1527–1535. 10.1128/JVI.02069-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DuBois RM, Zaraket H, Reddivari M, Heath RJ, White SW, Russell CJ. 2011. Acid stability of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity. PLoS Pathog. 7:e1002398. 10.1371/journal.ppat.1002398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koerner I, Matrosovich MN, Haller O, Staeheli P, Kochs G. 2012. Altered receptor specificity and fusion activity of the haemagglutinin contribute to high virulence of a mouse-adapted influenza A virus. J. Gen. Virol. 93:970–979. 10.1099/vir.0.035782-0. [DOI] [PubMed] [Google Scholar]
- 39.Cotter CR, Jin H, Chen Z. 2014. A single amino acid in the stalk region of the H1N1pdm influenza virus HA protein affects viral fusion, stability and infectivity. PLoS Pathog. 10:e1003831. 10.1371/journal.ppat.1003831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krenn BM, Egorov A, Romanovskaya-Romanko E, Wolschek M, Nakowitsch S, Ruthsatz T, Kiefmann B, Morokutti A, Humer J, Geiler J, Cinatl J, Michaelis M, Wressnigg N, Sturlan S, Ferko B, Batishchev OV, Indenbom AV, Zhu R, Kastner M, Hinterdorfer P, Kiselev O, Muster T, Romanova J. 2011. Single HA2 mutation increases the infectivity and immunogenicity of a live attenuated H5N1 intranasal influenza vaccine candidate lacking NS1. PLoS One 6:e18577. 10.1371/journal.pone.0018577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. (Lond.) 1938:493–497. [Google Scholar]
- 42.Hoffmann E, Krauss S, Perez D, Webby R, Webster RG. 2002. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine 20:3165–3170. [DOI] [PubMed] [Google Scholar]
- 43.Daniels RS, Downie JC, Hay AJ, Knossow M, Skehel JJ, Wang ML, Wiley DC. 1985. Fusion mutants of the influenza virus hemagglutinin glycoprotein. Cell 40:431–439. 10.1016/0092-8674(85)90157-6. [DOI] [PubMed] [Google Scholar]
- 44.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428. 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cross KJ, Burleigh LM, Steinhauer DA. 2001. Mechanisms of cell entry by influenza virus. Expert Rev. Mol. Med. 3:1–18. 10.1017/S1462399401002575. [DOI] [PubMed] [Google Scholar]
- 46.Yoshimura A, Kuroda K, Kawasaki K, Yamashina S, Maeda T, Ohnishi S. 1982. Infectious cell entry mechanism of influenza virus. J. Virol. 43:284–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scholtissek C. 1985. Stability of infectious influenza A viruses at low pH and at elevated temperature. Vaccine 3:215–218. [DOI] [PubMed] [Google Scholar]
- 48.Carr CM, Chaudhry C, Kim PS. 1997. Influenza hemagglutinin is spring-loaded by a metastable native conformation. Proc. Natl. Acad. Sci. U. S. A. 94:14306–14313. 10.1073/pnas.94.26.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Haywood AM, Boyer BP. 1986. Time and temperature dependence of influenza virus membrane fusion at neutral pH. J. Gen. Virol. 67:2813–2817. 10.1099/0022-1317-67-12-2813. [DOI] [PubMed] [Google Scholar]
- 50.Suguitan AL, Jr, Marino MP, Desai PD, Chen LM, Matsuoka Y, Donis RO, Jin H, Swayne DE, Kemble G, Subbarao K. 2009. The influence of the multi-basic cleavage site of the H5 hemagglutinin on the attenuation, immunogenicity and efficacy of a live attenuated influenza A H5N1 cold-adapted vaccine virus. Virology 395:280–288. 10.1016/j.virol.2009.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jin H, Lu B, Zhou H, Ma C, Zhao J, Yang CF, Kemble G, Greenberg H. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18–24. 10.1016/S0042-6822(02)00035-1. [DOI] [PubMed] [Google Scholar]
- 52.Jin H, Zhou H, Lu B, Kemble G. 2004. Imparting temperature sensitivity and attenuation in ferrets to A/Puerto Rico/8/34 influenza virus by transferring the genetic signature for temperature sensitivity from cold-adapted A/Ann Arbor/6/60. J. Virol. 78:995–998. 10.1128/JVI.78.2.995-998.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maassab HF. 1968. Plaque formation of influenza virus at 25°C. Nature 219:645–646. 10.1038/219645a0. [DOI] [PubMed] [Google Scholar]
- 54.Gruber WC. 2002. The role of live influenza vaccines in children. Vaccine 20:S66–S73. 10.1016/S0264-410X(02)00141-X. [DOI] [PubMed] [Google Scholar]
- 55.Skehel JJ, Wiley DC. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69:531–569. 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- 56.Giannecchini S, Campitelli L, Calzoletti L, De Marco MA, Azzi A, Donatelli I. 2006. Comparison of in vitro replication features of H7N3 influenza viruses from wild ducks and turkeys: potential implications for interspecies transmission. J. Gen. Virol. 87:171–175. 10.1099/vir.0.81187-0. [DOI] [PubMed] [Google Scholar]
- 57.Lin YP, Wharton SA, Martin J, Skehel JJ, Wiley DC, Steinhauer DA. 1997. Adaptation of egg-grown and transfectant influenza viruses for growth in mammalian cells: selection of hemagglutinin mutants with elevated pH of membrane fusion. Virology 233:402–410. 10.1006/viro.1997.8626. [DOI] [PubMed] [Google Scholar]
- 58.Doms RW, Gething MJ, Henneberry J, White J, Helenius A. 1986. Variant influenza virus hemagglutinin that induces fusion at elevated pH. J. Virol. 57:603–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Steinhauer DA, Martin J, Lin YP, Wharton SA, Oldstone MB, Skehel JJ, Wiley DC. 1996. Studies using double mutants of the conformational transitions in influenza hemagglutinin required for its membrane fusion activity. Proc. Natl. Acad. Sci. U. S. A. 93:12873–12878. 10.1073/pnas.93.23.12873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Steinhauer DA, Wharton SA, Skehel JJ, Wiley DC. 1995. Studies of the membrane fusion activities of fusion peptide mutants of influenza virus hemagglutinin. J. Virol. 69:6643–6651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Steinhauer DA, Wharton SA, Skehel JJ, Wiley DC, Hay AJ. 1991. Amantadine selection of a mutant influenza virus containing an acid-stable hemagglutinin glycoprotein: evidence for virus-specific regulation of the pH of glycoprotein transport vesicles. Proc. Natl. Acad. Sci. U. S. A. 88:11525–11529. 10.1073/pnas.88.24.11525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ciampor F, Bayley PM, Nermut MV, Hirst EM, Sugrue RJ, Hay AJ. 1992. Evidence that the amantadine-induced, M2-mediated conversion of influenza A virus hemagglutinin to the low pH conformation occurs in an acidic trans-Golgi compartment. Virology 188:14–24. 10.1016/0042-6822(92)90730-D. [DOI] [PubMed] [Google Scholar]
- 63.Grambas S, Bennett MS, Hay AJ. 1992. Influence of amantadine resistance mutations on the pH regulatory function of the M2 protein of influenza A viruses. Virology 191:541–549. 10.1016/0042-6822(92)90229-I. [DOI] [PubMed] [Google Scholar]
- 64.Barman S, Ali A, Hui EK, Adhikary L, Nayak DP. 2001. Transport of viral proteins to the apical membranes and interaction of matrix protein with glycoproteins in the assembly of influenza viruses. Virus Res. 77:61–69. 10.1016/S0168-1702(01)00266-0. [DOI] [PubMed] [Google Scholar]
- 65.Scholtissek C, Stech J, Krauss S, Webster RG. 2002. Cooperation between the hemagglutinin of avian viruses and the matrix protein of human influenza A viruses. J. Virol. 76:1781–1786. 10.1128/JVI.76.4.1781-1786.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Enami M, Enami K. 1996. Influenza virus hemagglutinin and neuraminidase glycoproteins stimulate the membrane association of the matrix protein. J. Virol. 70:6653–6657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Radyukhin V, Fedorova N, Ksenofontov A, Serebryakova M, Baratova L. 2008. Cold co-extraction of hemagglutinin and matrix M1 protein from influenza virus A by a combination of non-ionic detergents allows for visualization of the raft-like nature of the virus envelope. Arch. Virol. 153:1977–1980. 10.1007/s00705-008-0214-7. [DOI] [PubMed] [Google Scholar]
- 68.Betakova T, Ciampor F, Hay AJ. 2005. Influence of residue 44 on the activity of the M2 proton channel of influenza A virus. J. Gen. Virol. 86:181–184. 10.1099/vir.0.80358-0. [DOI] [PubMed] [Google Scholar]
- 69.Murakami S, Horimoto T, Ito M, Takano R, Katsura H, Shimojima M, Kawaoka Y. 2012. Enhanced growth of influenza vaccine seed viruses in Vero cells mediated by broadening the optimal pH range for virus membrane fusion. J. Virol. 86:1405–1410. 10.1128/JVI.06009-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cox NJ, Kitame F, Kendal AP, Maassab HF, Naeve C. 1988. Identification of sequence changes in the cold-adapted, live attenuated influenza vaccine strain, A/Ann Arbor/6/60 (H2N2). Virology 167:554–567. [PubMed] [Google Scholar]
- 71.Washington N, Steele RJ, Jackson SJ, Bush D, Mason J, Gill DA, Pitt K, Rawlins DA. 2000. Determination of baseline human nasal pH and the effect of intranasally administered buffers. Int. J. Pharm. 198:139–146. [DOI] [PubMed] [Google Scholar]
- 72.Vareille M, Kieninger E, Edwards MR, Regamey N. 2011. The airway epithelium: soldier in the fight against respiratory viruses. Clin. Microbiol. Rev. 24:210–229. 10.1128/CMR.00014-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fischer H, Widdicombe JH. 2006. Mechanisms of acid and base secretion by the airway epithelium. J. Membr. Biol. 211:139–150. 10.1007/s00232-006-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wine JJ, Joo NS. 2004. Submucosal glands and airway defense. Proc. Am. Thorac. Soc. 1:47–53. 10.1513/pats.2306015. [DOI] [PubMed] [Google Scholar]
- 75.Fischer H, Widdicombe JH, Illek B. 2002. Acid secretion and proton conductance in human airway epithelium. Am. J. Physiol. Cell Physiol. 282:C736–C743. 10.1152/ajpcell.00369.2011. [DOI] [PubMed] [Google Scholar]
- 76.Jacoby DB, Tamaoki J, Borson DB, Nadel JA. 1988. Influenza infection causes airway hyperresponsiveness by decreasing enkephalinase. J. Appl. Physiol. 64:2653–2658. [DOI] [PubMed] [Google Scholar]
- 77.Brown JD, Swayne DE, Cooper RJ, Burns RE, Stallknecht DE. 2007. Persistence of H5 and H7 avian influenza viruses in water. Avian Dis. 51:285–289. 10.1637/7636-042806R.1. [DOI] [PubMed] [Google Scholar]
- 78.Yoshimura A, Ohnishi S. 1984. Uncoating of influenza virus in endosomes. J. Virol. 51:497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thoennes S, Li ZN, Lee BJ, Langley WA, Skehel JJ, Russell RJ, Steinhauer DA. 2008. Analysis of residues near the fusion peptide in the influenza hemagglutinin structure for roles in triggering membrane fusion. Virology 370:403–414. 10.1016/j.virol.2007.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]