ABSTRACT
Zaire ebolavirus (EBOV) VP35 is a double-stranded RNA (dsRNA)-binding protein that inhibits RIG-I signaling and alpha/beta interferon (IFN-α/β) responses by both dsRNA-binding-dependent and -independent mechanisms. VP35 also suppresses dendritic cell (DC) maturation. Here, we define the pathways and mechanisms through which VP35 impairs DC maturation. Wild-type VP35 (VP35-WT) and two well-characterized VP35 mutants (F239A and R322A) that independently ablate dsRNA binding and RIG-I inhibition were delivered to primary human monocyte-derived DCs (MDDCs) using a lentivirus-based expression system. VP35-WT suppressed not only IFN-α/β but also proinflammatory responses following stimulation of MDDCs with activators of RIG-I-like receptor (RLR) signaling, including RIG-I activators such as Sendai virus (SeV) or 5′-triphosphate RNA, or MDA5 activators such as encephalomyocarditis virus (EMCV) or poly(I·C). The F239A and R322A mutants exhibited greatly reduced suppression of IFN-α/β and proinflammatory cytokine production following treatment of DCs with RLR agonists. VP35-WT also blocked the upregulation of DC maturation markers and the stimulation of allogeneic T cell responses upon SeV infection, whereas the mutants did not. In contrast to the RLR activators, VP35-WT and the VP35 mutants impaired IFN-β production induced by Toll-like receptor 3 (TLR3) or TLR4 agonists but failed to inhibit proinflammatory cytokine production induced by TLR2, TLR3, or TLR4 agonists. Furthermore, VP35 did not prevent lipopolysaccharide (LPS)-induced upregulation of surface markers of MDDC maturation and did not prevent LPS-triggered allogeneic T cell stimulation. Therefore, VP35 is a general antagonist of DC responses to RLR activation. However, TLR agonists can circumvent many of the inhibitory effects of VP35. Therefore, it may be possible to counteract EBOV immune evasion by using treatments that bypass the VP35-imposed block to DC maturation.
IMPORTANCE The VP35 protein, which is an inhibitor of RIG-I signaling and alpha/beta interferon (IFN-α/β) responses, has been implicated as an EBOV-encoded factor that contributes to suppression of dendritic cell (DC) function. We used wild-type VP35 and previously characterized VP35 mutants to clarify VP35-DC interactions. Our data demonstrate that VP35 is a general inhibitor of RIG-I-like receptor (RLR) signaling that blocks not only RIG-I- but also MDA5-mediated induction of IFN-α/β responses. Furthermore, in DCs, VP35 also impairs the RLR-mediated induction of proinflammatory cytokine production, upregulation of costimulatory markers, and activation of T cells. These inhibitory activities require VP35 dsRNA-binding activity, an activity previously correlated to VP35 RIG-I inhibitory function. In contrast, while VP35 can inhibit IFN-α/β production induced by TLR3 or TLR4 agonists, this occurs in a dsRNA-independent fashion, and VP35 does not inhibit TLR-mediated expression of proinflammatory cytokines. These data suggest strategies to overcome VP35 inhibition of DC function.
INTRODUCTION
Zaire ebolavirus (EBOV), a member of the filovirus family, is an enveloped, negative-sense RNA virus that causes severe, frequently lethal infections in humans and primates (1). Two notable features of EBOV that likely contribute to virulence are its interference with host innate immune signaling pathways and its suppression of dendritic cell (DC) maturation. In vivo, DCs are target cells of infection (2, 3). In vitro, DCs support productive virus replication (4–6). Experimental infection of human monocyte-derived DCs (MDDCs) results in impaired alpha/beta interferon (IFN-α/β) and proinflammatory cytokine expression, abnormal upregulation of costimulatory markers, and inhibition of MDDC-mediated activation of naive T cells (4, 5, 7). EBOV VP35 protein suppression of innate immune function likely contributes to the suppression of DC function (7).
VP35 is a multifunctional molecule and serves as (i) a nonenzymatic component of the viral RNA synthesis machinery, (ii) a structural protein, and (iii) an inhibitor of innate immune signaling pathways (reviewed in reference 8). Innate immune suppression by VP35 is mediated through inhibition of the retinoic acid-inducible gene I (RIG-I) signaling pathway that triggers IFN-α/β gene expression (9). The importance of such suppression for EBOV is underlined by the fact that activation of RIG-I signaling prior to infection suppressed EBOV yields by approximately 1,000-fold (10). Furthermore, recombinant EBOVs possessing mutated VP35 proteins with impaired IFN-α/β antagonist activity are significantly attenuated in cells capable of mounting an IFN-α/β response (11–13). Such viruses are also attenuated and did not cause disease or death in a guinea pig model of infection (12, 13).
Several mechanisms contribute to VP35 IFN-α/β antagonist function. VP35 can interact with the cellular kinases IKKε and TBK1 and can block their interaction with and phosphorylation of interferon regulatory factor 3 (IRF-3), a transcription factor critical for induction of IFN-β gene expression (14). VP35 also interacts with the transcription factor IRF-7 and the machinery that SUMOylates IRF-7 (Ubc9 and PIAS1), thereby impairing the IRF-7-dependent transcriptional response, which is central to IFN-α gene expression (15, 16). Furthermore, disruption of the VP35 double-stranded RNA (dsRNA)-binding ability substantially impairs its suppression of IFN-α/β responses by RIG-I activators (9, 13, 17).
The VP35 dsRNA-binding domain is referred to as the IFN-inhibitory domain (IID) because of its contribution to suppression of RIG-I-like receptor (RLR)-induced IFN-α/β responses (17–20). The IID exhibits two dsRNA-binding modes (19, 20). The first mode involves direct binding of the VP35 “central basic patch” to dsRNA in a sequence-independent manner. The second mode, the “end-cap” interaction, is mediated by several conserved hydrophobic residues, including phenylalanine 239 (F239), which forms a pocket that may conceal the blunt ends of dsRNA and thereby mask the 5′-triphosphate that is recognized by RIG-I. Importantly, mutation of central basic patch or end-cap residues to alanine disrupts dsRNA binding and impairs VP35 inhibition of RIG-I signaling (17). In addition, the same residues that mediate dsRNA binding are also required for VP35 interaction with PACT (protein activator of the interferon-induced protein kinase), a cellular protein which can promote RIG-I activation. Therefore, the consequence of the VP35-PACT interaction is the disruption of RIG-I activation (21).
Several studies indicate that VP35 can contribute to the suppression of DC maturation by EBOV (7, 22, 23). The present study, which used replication-defective lentiviral vectors to deliver wild-type VP35 (VP35-WT) or mutant VP35 proteins to DCs at high efficiency, was undertaken to address several incompletely resolved issues. Specifically, we sought to determine whether VP35 is sufficient on its own to block MDDC maturation, to define which features of MDDC maturation are targeted by VP35, to evaluate how VP35 affects maturation by a variety of RLR and Toll-like receptor (TLR) activators, and to clarify mechanisms of VP35 inhibition in light of recent structural and mechanistic studies of VP35 IFN antagonist function. The results demonstrate that expression of VP35 on its own is sufficient to suppress RLR-stimulated MDDC maturation, that this function is dependent on the dsRNA-binding domain, and that VP35 has a limited impact on TLR-mediated MDDC maturation. Therefore, it may be possible to circumvent the inhibitory function of VP35 and restore the maturation of EBOV-infected MDDCs.
MATERIALS AND METHODS
Isolation of human monocyte-derived DCs and naive T cells.
Human MDDCs were generated from CD14+ cells purified from concentrated leukocytes of healthy human donors (New York Blood Center), as described previously (23). Briefly, peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll density gradient centrifugation (catalog number 95021-205; GE Healthcare), and CD14+ cells were purified by using CD14 microbeads (Miltenyi Biotech). CD14+ cells, at a concentration of 106 cells/ml, were incubated at 37°C for 5 days in DC medium (RPMI containing 4% human AB serum [Fisher Scientific], 2 mM l-glutamine, 1 mM sodium pyruvate, 100 U/ml penicillin–100 μg/ml streptomycin, and 55 μM β-mercaptoethanol) supplemented with 500 U/ml human granulocyte-macrophage colony-stimulating factor (hGM-CSF; PeproTech) and 500 U/ml human interleukin-4 (hIL-4; PeproTech). Typically, we obtained approximately 107 MDDCs per 20 ml of culture. Naive CD4 and naive CD8 T cell isolation was performed with CD4+ (catalog number 130-096-533; Miltenyi Biotech) or CD8+ (catalog number 130-096-495; Miltenyi Biotech) isolation kits according to the manufacturer's recommendations.
Generation of VP35-encoding lentiviruses and Vpx-VLPs.
Replication-defective lentiviruses were generated as previously described (24). Expression plasmids for lentiviral vector-derived virus-like particles (VLPs) were as follows: pHCMV-G, encoding the vesicular stomatitis virus (VSV) glycoprotein (25); packaging plasmid pNL4.3-gag-pol; and VP35-encoding lentiviral vectors derived from pHR-SIN-CSIGW (26, 27). Flag-tagged EBOV VP35-WT or VP35 F239A or R322A mutants were cloned into pHR-SIN-CSIGW to generate lentiviruses encoding each protein. Vpx-containing VLPs (Vpx-VLPs) were generated by cotransfecting expression plasmids for VSV G and pSIV3+, a simian immunodeficiency virus (SIV) SIV251 Gag-Pol-encoding plasmid containing Vpx (a kind gift of Dan Littman, NYU Medical Center) (28).
Transduction of human MDDCs.
MDDCs were transduced by spinoculation at 1,850 rpm with lentiviruses and Vpx-VLPs for 2.5 h and then cultured in fresh medium for 72 h. Transduced MDDCs were harvested to assess expression by flow cytometry and Western blotting or were used in subsequent experiments.
Infection/transfection/stimulation of transduced MDDCs.
A Sendai virus (SeV) strain Cantell stock was generated by inoculating 10-day-old embryonated chicken eggs and incubated for 2 days at 37°C. Encephalomyocarditis virus (EMCV) (a kind gift from Adolfo García-Sastre, Icahn School of Medicine at Mount Sinai) was propagated in baby hamster kidney (BHK) cells. At 72 h posttransduction, transduced MDDCs were infected with SeV or EMCV in serum-free medium for 1 h and then harvested at various time points. 5′-triphosphate RNA (pppRNA), low-molecular-weight poly(I·C), and high-molecular-weight poly(I·C) were purchased from Invivogen; diluted according to the manufacturer's recommendations; and transfected into transduced MDDCs by using Stemfect (Stemgent). Zymosan, poly(I·C), and lipopolysaccharide (LPS) (Sigma-Aldrich) were used at the indicated concentrations.
Allogeneic T cell and transduced DC coculture assays.
Transduced DCs were either mock infected or infected with SeV for 4 h before coculturing them with purified naive CD4 or CD8 T cells for 5 days at the indicated ratios. Culture supernatants were then harvested and assayed by an enzyme-linked immunosorbent assay (ELISA) for IFN-γ (BD bioscience), according to the manufacturer's recommendations.
Quantitative reverse transcription-PCR (qRT-PCR).
Total RNAs were extracted from MDDCs with TRIzol reagent (Sigma). cDNA was prepared by using a SuperScript III first-strand synthesis system (Invitrogen). Relative gene expression was determined by using PerfeCTa SYBR green FastMix (Quanta Biosciences, Inc.) with a Bio-Rad CFX96 instrument. CXF Manager software (Bio-Rad) was used to analyze the relative mRNA expression levels by the change in the threshold cycle (ΔCT), with the RPS11 gene serving as a reference mRNA to which the results were normalized. The copy number for RPS11 was based upon a standard curve generated by using an RPS11-containing plasmid.
IFN bioassay.
IFN bioassays, used to measure levels of secreted, biologically active IFN-α/β, were performed as previously described (23). Supernatants were UV irradiated for 10 min on ice to inactivate virus. Twofold serial dilutions of the supernatants were prepared and then transferred onto Vero 76 cells cultured in 96-well plates (catalog number 3904; Costar, Corning, NY, USA). To determine whether antiviral activity was due to IFN-α/β, anti-IFN-α or anti-IFN-β antibodies (PBL, Piscataway, NJ, USA) were added to supernatants for 30 min at room temperature prior to adding them to cells. Twofold dilutions of IFN-β (PBL, Piscataway, NJ, USA) were also prepared to generate a standard dose-response curve. After incubation in a 5% CO2 incubator at 37°C for 14 to 16 h, the supernatants were removed, and the cells were infected with Newcastle disease virus expressing green fluorescent protein (NDV-GFP) at a multiplicity of infection (MOI) of 4. After 20 to 24 h, the cells were fixed with 4% paraformaldehyde in phosphate-buffered saline (PBS) and then rinsed with PBS. GFP fluorescence was measured by using a Beckman DTX880 microplate reader (Beckman Coulter, Fullerton, CA, USA). Linear regression using the curve-fitting function of Microsoft Excel was used to convert GFP intensity into relative IFN units, since our supernatants contained a mixture of IFN-α/β.
Antibodies for Western blotting.
Goat polyclonal anti-IRF-3 antibody was purchased from Santa Cruz Biotechnology (catalog number sc-15991). Rabbit monoclonal anti-phospho-IRF-3 antibody was purchased from Cell Signaling Technology (catalog number 4947). Mouse monoclonal anti-GFP antibody was purchased from Clontech Laboratories (catalog number 632375). Mouse monoclonal anti-Flag M2 antibody (F3165) and mouse monoclonal anti-β-tubulin antibody (T0198) were purchased from Sigma-Aldrich.
Flow cytometry analysis of DCs.
MDDCs were harvested and stained for cell surface expression of multiple markers of DC maturation by flow cytometry at 20 h post-SeV infection or post-TLR stimulation. DCs were pelleted and resuspended in staining buffer (PBS, 2% bovine serum albumin [BSA], 10 mM EDTA) and incubated with the antibodies for 20 min on ice in the dark. Antibodies, including anti-CD11C-phycoerythrin (PE)-Cy7, anti-HLA-DR–PE, HLA-ABC-PE, anti-CD40-PE, anti-CD80-PE, anti-CD83-PE, and anti-CD86-PE, were purchased from eBiosciences. Flow cytometry data were collected by using an LSR II flow cytometer equipped with a violet laser (BD Bioscience) and analyzed by using FlowJo software (Tree Star, Ashland, OR, USA).
RESULTS
Efficient transduction of human MDDCs with control and VP35-expressing lentiviruses.
In order to define the effects of wild-type or mutant VP35 proteins on MDDCs, an expression system that would neither activate significant DC maturation nor block DC signaling pathways was desirable. We took advantage of a previously described system where lentiviral vector-derived viruses can efficiently transduce MDDCs when cotransduced with SIV-derived virus-like particles (VLPs) containing the SAMHD1 antagonist SIV Vpx (Vpx-VLPs) (24). In our studies, using a lentiviral vector encoding GFP, substantial GFP expression was detectable beginning at 3 days post-MDDC transduction, and transduction occurred at high efficiency (Fig. 1A). The lentiviral vector used does not express human immunodeficiency virus type 1 (HIV-1) proteins and therefore, based on previous studies, is not expected to trigger MDDC activation (29). To directly address possible MDDC activation, cytokine and cell surface activation marker upregulation was assessed. Transduction resulted in only slightly increased production of IFN-β or tumor necrosis factor alpha (TNF-α) mRNA (Fig. 1B). Furthermore, there was no significant difference in the maturation state between untransduced MDDCs and transduced MDDCs, as assessed by the levels of CD80 and CD86 on the cell surface (Fig. 1C and D).
FIG 1.
Efficient expression of wild-type or mutant EBOV VP35 in human MDDCs. (A) Human MDDCs were either mock transduced, transduced with Vpx-VLPs only, or cotransduced with lentiviral (LV) vectors and Vpx-VLPs. MDDCs were harvested at the indicated days post-lentiviral transduction, and the percentage of GFP-positive cells was measured by flow cytometry. Error bars represent standard deviations. (B) Total RNA was isolated from untransduced MDDCs or transduced MDDCs at the indicated days post-lentiviral transduction and analyzed by qRT-PCR to quantify IFN-β and TNF-α. (C and D) Human MDDCs were either untransduced or transduced for 3 days and harvested to assess the levels of surface expression of the DC maturation markers CD80 and CD86. Representative flow cytometry plots illustrating the changes in CD80 and CD86 expression (C) and the mean fluorescence intensity (MFI) of CD80 or CD86 from three independent experiments (D) are shown. Error bars indicate standard deviations. N.S., not significant. (E) Human MDDCs were transduced with lentiviral vectors that lack VP35 sequences (empty) or that express either Flag-tagged wild-type VP35 (WT) or VP35 F239A or R322A mutants. Each lentivirus also expresses GFP that is under the control of an IRES. Cells from five independent donors were analyzed for transduction efficiency by measuring the percentage of GFP-positive cells by flow cytometry. Error bars represent standard deviations. (F) Cells from one representative donor were analyzed for VP35 expression by Western blotting with anti-Flag antibody. IB, immunoblot.
We inserted VP35-WT or VP35 F239A or R322A mutants upstream of an internal ribosome entry site (IRES)-GFP construct, such that in transduced MDDCs, VP35 and GFP would be translated as separate proteins from the same mRNA. An equivalent lentivirus lacking VP35 but encoding GFP served as an “empty vector” control. As for the empty vector lentivirus, transduction with the VP35 lentiviruses was highly efficient (∼95%) based on GFP expression (Fig. 1E), and VP35-WT and mutants were comparably expressed (Fig. 1F).
VP35 impairs MDDC IFN-α/β and proinflammatory cytokine responses to Sendai virus infection.
VP35-WT blocks the RIG-I signaling pathway, while the F239A and R322A mutants each exhibited an impaired ability to inhibit the RIG-I pathway (17). To determine how VP35-WT and the mutant VP35 proteins impact DC responses to a viral activator of RIG-I signaling, day 5 immature MDDCs were transduced with the empty vector or VP35-WT- or F239A or R322A mutant-expressing lentiviruses for 72 h and subsequently infected with SeV. As assessed by qRT-PCR, VP35-WT substantially suppressed IFN-β, IFN-α, TNF-α, IL-1β, and IL-12p40 expression relative to the empty vector control (Fig. 2A). The suppression of IFN-α/β and cytokine expression by VP35-WT corresponded to enhanced production of SeV nucleoprotein (NP) mRNA, consistent with the prevention of the antiviral IFN-α/β response (Fig. 2A). The F239A and R322A mutants each exhibited substantially reduced suppression of IFN-α/β and cytokine responses, although each mutant consistently displayed modest suppression relative to the empty vector control (Fig. 2A). Suppression of IFN-α/β production was confirmed by an IFN bioassay in the absence and presence of IFN-β or IFN-α neutralizing antibodies. VP35-WT again suppressed IFN-α/β production, whereas the two dsRNA-binding mutants were impaired for this function (Fig. 2B). To determine whether suppression of the IFN-α/β response correlates with inhibition of the RIG-I signaling pathway, the phosphorylation of interferon regulatory factor 3 (IRF-3) was assessed by Western blotting. VP35-WT potently suppressed IRF-3 phosphorylation at 4 and 6 h post-SeV infection, whereas little to no effect was detected in F239A or R322A mutant-transduced MDDCs (Fig. 2C). Therefore, VP35 appears to inhibit RLR-mediated IFN-α/β and cytokine gene expression, and full inhibition requires intact VP35 dsRNA-binding activity.
FIG 2.
Effect of wild-type and mutant EBOV VP35 proteins on IFN-α/β and proinflammatory cytokine production in SeV-infected MDDCs. MDDCs were transduced with the indicated empty vector or wild-type or mutant VP35-expressing lentiviruses. (A) Total RNA was isolated from transduced MDDCs infected with SeV and analyzed by qRT-PCR to quantify IFN-β, IFN-α, SeV NP, TNF-α, IL-1β, and IL-12 levels. Each value was normalized to RPS11 mRNA levels to determine the relative copy number. Error bars indicate standard deviations (*, P < 0.05 relative to empty vector-transduced MDDCs at the same time point). Samples were collected from three independent donors. (B) Transduced MDDCs were infected with SeV for 20 h, and supernatants were harvested and analyzed for IFN by a bioassay. For samples treated with anti-IFN-β or anti-IFN-α antibody, supernatants were cultured with the indicated antibodies for 30 min at room temperature prior to analysis by the IFN bioassay. Data were obtained in triplicates from cells from three independent donors. (C) Levels of phosphorylated IRF-3 (P-IRF3) and total IRF-3 were analyzed by Western blotting at the indicated times post-SeV-infection. Error bars indicate standard deviations (*, P < 0.05 relative to empty vector-transduced MDDCs at the same time point). ø, mock-infected transduced MDDCs; hpi, hours postinfection; GAPDH, glyceraldehyde-3-phosphate dehydrogenase.
VP35 inhibits MDDC responses to both RIG-I and MDA5 agonists.
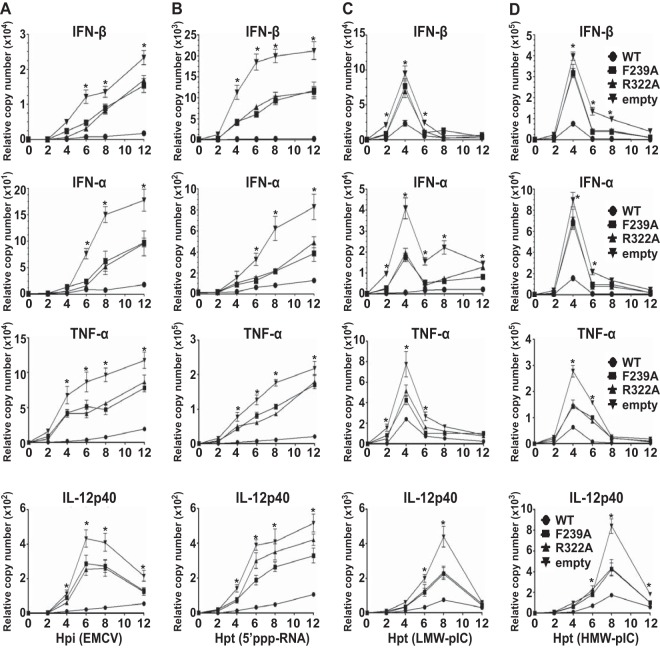
SeV likely activates MDDCs primarily through RIG-I. We sought to clarify the capacity of VP35 to inhibit MDDC activation via each of the RLR pattern recognition receptors RIG-I and MDA5. Therefore, transduced MDDCs were infected with encephalomyocarditis virus (EMCV), an MDA5 activator (30), or the MDDCs were transfected with RNAs of differing lengths and structures that are expected to have specificity for either RIG-I or MDA5. Specifically, the RIG-I agonist 5′-triphosphate RNA (5′-pppRNA) or low-molecular-weight poly(I·C) or the MDA5 ligand high-molecular-weight poly(I·C) was used (Fig. 3B to D). Under each condition tested, VP35-WT very effectively suppressed IFN-β and IFN-α expression (Fig. 3). Furthermore, VP35-WT also effectively suppressed proinflammatory cytokine TNF-α and IL-12p40 mRNA expression (Fig. 3). The F239A and R322A mutants again were significantly impaired and displayed intermediate to low levels of inhibitory effects on IFN-α/β and cytokine production (Fig. 3). These data suggest that VP35 effectively inhibits both RIG-I and MDA5 responses in MDDCs, and this requires intact VP35 dsRNA-binding activity.
FIG 3.
Effect of wild-type and mutant EBOV VP35 proteins on IFN-α/β and cytokine production following stimulation of MDDCs with different RLR agonists. Total RNA was isolated from MDDCs transduced with the empty vector or VP35-WT or mutant VP35 lentiviruses. Transduced MDDCs were either infected with EMCV at an MOI of 1 (A) or transfected with 5′-pppRNA (B), low-molecular-weight poly(I·C) (C), or high-molecular-weight poly(I·C) (D) at 1 μg/ml each and analyzed by qRT-PCR for IFN-β, IFN-α, TNF-α, and IL-12p40 levels. Each value was normalized to the RPS11 mRNA level to obtain the relative copy number. Error bars indicate standard deviations (*, P < 0.05 relative to empty vector-transduced MDDCs at the same time point). Hpi, hours postinfection; Hpt, hours posttransfection.
VP35 impairs DC maturation and T cell stimulation in response to RIG-I activation.
Upon activation, for example, by RNA virus infection, DCs undergo phenotypic maturation by upregulating maturation markers and enhancing their ability to stimulate T cells. To determine whether VP35 expression is sufficient to inhibit upregulation of maturation markers, the surface expression of major histocompatibility complex class II (MHC-II), MHC-I, CD40, CD80, and CD83 was examined in transduced MDDCs following SeV infection. VP35-WT expression largely prevented SeV-dependent upregulation of CD80, while the empty vector and mutant VP35 proteins did not (Fig. 4A and B). Upregulation of the other DC maturation markers MHC-II, MHC-I, CD40, and CD83 was also abrogated in VP35-WT-expressing MDDCs upon SeV infection, but once again, the inhibitory activity was largely absent from the F239A and R322A mutant-transduced MDDCs (Fig. 4B). These observations indicate that VP35-WT is sufficient to antagonize phenotypic maturation upon RIG-I activation, while VP35 dsRNA-binding mutants are not.
FIG 4.
Effect of wild-type and mutant EBOV VP35 proteins on cell surface markers of DC maturation. Transduced MDDCs were infected with SeV for 18 h, harvested, and stained for the expression of MHC-II, MHC-I, CD40, CD80, CD83, and CD86. (A) Representative flow cytometry plots illustrating the changes in HLA-DR and CD80 expression levels of EBOV VP35-transduced MDDCs and empty vector-transduced MDDCs at 20 h post-SeV infection. Filled histograms represent uninfected MDDCs, and white histograms represent infected MDDCs. (B) Fold change in mean fluorescence intensity (MFI) for the indicated proteins in transduced MDDCs. Fold increase indicates comparisons of SeV-infected to uninfected MDDCs. Error bars indicate standard deviations from three independent experiments (*, P < 0.05 relative to empty vector-transduced MDDCs at the same time point).
To determine whether VP35 expression is also sufficient to inhibit the ability of MDDCs to activate naive T cells, transduced MDDCs were infected with SeV and cocultured with allogeneic CD4+ and CD8+ T cells for 5 days at various DC-to-T cell ratios. The supernatants from the cocultures were analyzed for accumulation of IFN-γ, an indication of T cell activation. Compared to T cells cocultured with control MDDCs, T cells cultured with MDDCs expressing VP35-WT produced less IFN-γ (Fig. 5A and B). However, T cells cultured with DCs expressing the F239A or R322A mutant produced levels of IFN-γ comparable to that produced by T cells cultured with control MDDCs (Fig. 5A and B). Hence, VP35-WT inhibits DC stimulation and an allogeneic T cell response upon RIG-I activation in a manner that depends on the dsRNA-binding ability of EBOV VP35.
FIG 5.

Effect of wild-type and mutant VP35 proteins on allogeneic T cell activation by SeV-infected MDDCs. Transduced MDDCs were mock infected or infected with SeV and then cultured with either purified naive CD4 T cells (A) or purified naive CD8 T cells (B) at the indicated ratios for 5 days. Cultured supernatants were harvested, and the levels of IFN-γ were determined by ELISA. The data were collected from three independent experiments. Error bars indicate standard deviations (*, P < 0.05 relative to empty vector-transduced MDDCs at the same time point).
VP35 inhibits IFN-β responses induced by TLR agonists but fails to effectively block TLR-mediated MDDC maturation.
To determine if VP35 inhibitory activity in MDDCs can extend beyond RLR signaling pathways, transduced MDDCs were treated with agonists of TLR2, TLR3, or TLR4. As expected, the TLR2 agonist zymosan A did not induce IFN-β, even in empty vector-transduced MDDCs, but it did induce TNF-α (Fig. 6A). Neither VP35-WT nor mutant VP35s inhibited zymosan A-induced TNF-α production (Fig. 6A). The TLR3 agonist poly(I·C) or the TLR4 agonist lipopolysaccharide (LPS) was added to MDDCs. Each agonist induced an IFN-β response and a TNF-α response in empty vector-transduced MDDCs (Fig. 6B and C), although it should be noted that the magnitude of gene expression was less than that seen with the RLR activators (Fig. 2 and 3). The presence of VP35-WT or mutant VP35s decreased induction of IFN-β mRNA to similar degrees (Fig. A), suggesting that this inhibition did not depend on the dsRNA-binding ability of VP35. Interestingly, neither VP35-WT nor mutant VP35 inhibited TNF-α production upon stimulation with TLR agonists (Fig. 6B). These data suggest that while VP35 retains the ability to inhibit IFN-β responses to non-RLR activators, its capacity to block other DC activators is limited. We also determined whether VP35-WT or mutant VP35s can affect other measures of DC activation and function. Neither VP35-WT nor mutant VP35 proteins inhibited the upregulation of the DC markers CD40 and CD80 upon stimulation by the TLR4 agonist LPS (Fig. 6B). We also tested LPS-treated VP35-WT and mutant VP35 proteins expressing MDDCs for allogeneic stimulation of a CD4+ T cell response. While there was a slight trend toward decreased T cell responses in the presence of either VP35-WT or mutant VP35 proteins, this inhibition was not statistically significant (Fig. 6C). These data indicate that VP35 has a limited capacity to block TLR-induced MDDC responses.
FIG 6.
Impact of wild-type and mutant EBOV VP35 proteins on MDDC responses to TLR agonists. (A) Total RNA was isolated at the indicated times from transduced MDDCs stimulated with zymosan A (1 μg/ml), poly(I·C) (100 μg/ml), or LPS (100 ng/ml) and analyzed by qRT-PCR for IFN-β and TNF-α mRNA levels. Each value was normalized to the RPS11 mRNA level to obtain the relative copy number. Error bars indicate standard deviations (*, P < 0.05 relative to empty vector-transduced MDDCs at the same time point). Hpt, hours posttreatment. (B) Transduced MDDCs were treated with LPS for 18 h, harvested, and stained for the expression of CD40 and CD80. The fold change in mean fluorescence intensity (MFI) of MDDCs was determined by comparing LPS-treated to mock-treated cells. Error bars indicate standard deviations from three independent experiments. (C) Transduced MDDCs were mock treated or treated with LPS and then cultured with purified naive CD4 T cells at the indicated ratios for 5 days. The cultured supernatants were harvested, and the levels of IFN-γ were determined by ELISA. The data were collected from three independent experiments. Error bars indicate standard deviations (N.S., not significant relative to empty vector-transduced MDDCs at the same time point).
DISCUSSION
Although EBOV infects DCs in vivo and productively replicates in MDDCs in vitro, DCs infected with EBOV fail to undergo maturation and do not activate naive T cells (4, 5, 7, 31). Because activation of DC pattern recognition receptors and the subsequent phenotypic maturation of DCs serve as an important bridge between innate and adaptive immune responses, the suppression of DC maturation may contribute to the uncontrolled viral growth seen during EBOV infection in vivo (32). Defining specific EBOV-encoded inhibitors of DC maturation and their mechanisms of action should suggest strategies to overcome or mitigate EBOV immune evasion. Previous studies indicated that VP35 contributes to the impairment of DC maturation and function by EBOV (4, 7, 22). However, those previous studies left several issues unresolved regarding the impact of VP35 on DC maturation and function. Specifically, it was unclear whether VP35 is sufficient on its own to fully suppress MDDC maturation and function; which pathways in MDDCs are or are not suppressed by VP35 and how effectively VP35 blocks MDDC maturation induced through different pattern recognition receptors. Finally, it was unclear to what extent the well-characterized VP35 IID contributes to the various DC-suppressive functions of VP35.
To address these issues, we used HIV-1-based, replication-incompetent lentiviruses delivered to MDDCs in the presence of SIV VLPs containing the Vpx protein. Vpx eliminates the HIV-1 restriction factor SAMHD1 and facilitates efficient infection of human MDDCs (24). With this approach, human MDDCs were reproducibly transduced at >90% efficiency, and VP35 was expressed in the absence of other viral proteins. Consistent with what has been reported in the literature regarding lentiviral vectors that do not express HIV proteins, this transduction approach did not promote MDDC maturation and induced a very transient, barely detectable IFN-α/β response (Fig. 1A to D) (29).
As noted above, previous work implicated VP35 as a suppressor of DC maturation but did not fully resolve whether VP35 alone was sufficient to suppress such responses. One study showed that VP35 expressed from an alphavirus vector impaired MDDC IFN-α/β and cytokine production, but VP35 suppression of other aspects of MDDC function was not directly assessed (4). In a separate study, VP35 expressed from a herpes simplex virus 1 (HSV-1) mutant influenced IFN-α/β, cytokine, and T cell stimulation function (22). However, the use of a complex virus such as HSV-1, which encodes many immune modulators, left open the possibility that other HSV-1-encoded factors may have cooperated with VP35 to suppress aspects of MDDC maturation. Characterization of recombinant EBOVs that possess mutant VP35s also pointed to a role for VP35 in suppression of MDDC maturation, but the latter study also suggested a role for other filoviral proteins in suppression (7). Our data demonstrate conclusively that, when expressed in the absence of other viral proteins, VP35 can effectively impair RLR-mediated MDDC IFN-α/β and cytokine production, upregulation of surface markers characteristic of activation, and activation of T cell responses.
Previous studies did not systematically define which signaling pathways are effectively targeted by VP35 and which are not. Here, we demonstrated that VP35 effectively blocks IFN-α/β production by either RIG-I or MDA5. We further extended our analyses to demonstrate that inhibition of RLR responses extends to multiple aspects of MDDC maturation, including MDDC stimulation of T cell responses. SeV infection was used as an initial stimulus because it induces IFN-α/β by activating RIG-I, although some reports suggest that it may also activate MDA5 (33). SeV also provides a strong RIG-I-dependent DC maturation stimulus (34). As expected, SeV infection stimulated phosphorylation of IRF-3 and a strong IFN-α/β response from the empty vector-transduced MDDC control. VP35-WT suppressed IRF-3 phosphorylation and IFN-α/β production. Therefore, the effect of VP35 on MDDCs is similar to what has been seen in previous studies that used a variety of primary cells and cell lines (9, 13, 17). This suppression resulted in an apparent enhancement of SeV replication, as evidenced by the substantially increased accumulation of SeV NP mRNA. The increased RNA synthesis by SeV may account for the increased IFN-β mRNA levels seen in VP35-expressing cells at the 12-h time point; where accumulation of SeV NP mRNA may begin to exceed the VP35 inhibitory capacity. Such a phenomenon, though, may be less likely to occur in actual EBOV-infected DCs, since in a natural infection, VP35 expression would be coupled to levels of virus replication.
To assess VP35 inhibitory activity toward MDA5, transduced DCs were infected with EMCV or transfected with high-molecular-weight poly(I·C), either of which induces IFN-α/β production through MDA5 (30). For comparison, DCs were transfected with 5′-triphosphate RNA and low-molecular-weight poly(I·C) to activate RIG-I. VP35-WT suppressed IFN-α/β production under all conditions tested, indicating that VP35 is an effective inhibitor of both RIG-I and MDA5 signaling. As was seen with SeV infection, the mutant VP35 proteins exhibited substantially reduced suppression of IFN-α/β production in response to the other RLR agonists. Furthermore, VP35-WT also suppressed inflammatory cytokine production, as evidenced by reduced TNF-α and IL-12p40 mRNA levels, following stimulation of MDDCs with different RLR agonists. Therefore, the dsRNA-binding activity of VP35 plays a critical role not only for RIG-I inhibition but also for MDA5 inhibition.
We also addressed the effect of VP35 on TLR agonists and obtained previously undescribed outcomes. A previous study tested the effect of a VP35 R312A mutant and a separate VP35 mutant lacking the IID on LPS-treated murine bone marrow-derived DCs (22). Those data suggested an ability of VP35 to inhibit not only IFN-α/β production but also cytokine production and upregulation of CD80 and CD86. In contrast, our data obtained with primary human MDDCs indicate that while VP35 can inhibit TLR4-mediated expression of IFN-α/β, it fails to effectively block other aspects of MDDC maturation. The difference in experimental outcomes between the present and previous studies could reflect the source of DCs (mouse bone marrow versus human blood monocytes) or expression systems (HSV-1 versus lentiviruses). Importantly, this observation allowed us to demonstrate that the MDDC-suppressive function of VP35 can be overcome by activating the MDDCs with LPS, a TLR4 agonist. These data suggest that it will be possible to identify therapeutic strategies that overcome the immune-suppressive functions exerted by VP35 on EBOV-infected DCs.
A previous study tested the effects of a single VP35 dsRNA-binding mutant, R312A, in assays where LPS was used to stimulate DCs (22). However, that study did not directly assess how this mutant affected MDDC maturation when maturation was induced by either RLR agonists or other TLR agonists. Given that VP35 has both dsRNA-dependent and dsRNA-independent mechanisms of innate immune inhibition, it was important to define which inhibitory effects in DCs are due to the dsRNA-dependent and dsRNA-independent mechanisms. We addressed this issue by expressing, in MDDCs, VP35-WT and well-characterized mutants that disrupt VP35's dsRNA-binding ability and severely impair the inhibition of the RIG-I signaling pathway. The two VP35 mutants tested exhibited an impaired ability to counter IFN-α/β production (9, 13, 17). The design of these mutants was based on data from a previous study that characterized the structure of VP35 in complex with dsRNA (17). The dsRNA-binding C-terminal interferon-inhibitory domain (IID) of VP35 makes contacts through residues comprising the IID central basic patch with the dsRNA phosphodiester backbone (17). In this complex, VP35 also “end caps” the dsRNA, potentially masking 5′-triphosphates that could be recognized by RIG-I (17). Mutation of central basic patch residue R322 or end-cap residue F239 to alanine abrogates the dsRNA-binding activity of VP35 and the ability of VP35 to interact with PACT (21). As a consequence of these mutations, VP35 is unable to inhibit RIG-I signaling and SeV-induced IFN-α/β production in cell lines (9, 13, 21, 35). For the present studies, the use of two distinct mutants reduces the concern that we may have inadvertently disrupted an interface that may impact DC maturation by an undefined mechanism. In MDDCs, these mutants exhibited reduced suppression of SeV-induced IFN-α/β production, consistent with a model where SeV is activating RIG-I in DCs. Interestingly, these mutants retain modest inhibitory activity relative to the empty vector control. This finding is consistent with a dsRNA-binding-independent inhibitory mechanism, such as the capacity of VP35 to serve as a decoy substrate of IKKε and TBK1 (14).
VP35 has been reported to inhibit IFN-α/β production by multiple mechanisms. It can inhibit signaling via the RIG-I pathway; it can inhibit the kinases IKKε and TBK1, which activate the transcription factors IRF-3 and IRF-7; and it can promote SUMOylation of IRF-7, thereby impairing IRF-7 activation of transcription (9, 13–15). VP35 can also inhibit activation of the dsRNA-activated kinase PKR (36). Therefore, it is possible that VP35 inhibits DC responses to agonists of non-RLR pattern recognition receptors. Consistent with this possibility, in mouse DCs, delivery of VP35 via retrovirus modestly suppressed costimulatory marker and cytokine expression in response to LPS (22). It was therefore of interest to determine how VP35 would influence DC responses to different TLR agonists. This was examined by comparing the responses of transduced MDDCs to the TLR2 agonist zymosan A, the TLR3 agonist poly(I·C), and the TLR4 agonist LPS. While all three stimuli induce inflammatory cytokine production, only poly(I·C) and LPS also induced IFN-α/β production. When IFN-β gene expression was assessed following TLR3 or TLR4 agonist stimulation, VP35-WT was inhibitory. Interestingly, in the context of TLR3/4 agonists, VP35-WT and mutant VP35 proteins exhibited equal levels of inhibition of IFN-β induction. Therefore, inhibition of TLR-induced IFN-β gene expression is dsRNA binding independent. Likely, the dsRNA-dependent activity targets RLR signaling, for example, through the RIG-I activator PACT or cytoplasmic immunostimulatory RNAs. In contrast, the inhibition of TLR-mediated IFN-β expression should reflect VP35's effects on signaling molecules shared by the RLR and TLR3/4 pathways. It is likely that VP35 inhibits TLR-mediated induction through its ability to act as a decoy substrate for the kinases IKKε and TBK1. Interestingly, when a different dsRNA-binding mutant of VP35, R312A, was introduced into mouse DCs, it also suppressed IFN-β expression, corroborating our conclusion (22). In contrast to the previous study, in our work, neither wild-type nor mutant VP35 proteins inhibited inflammatory cytokine production in response to any of the TLR agonists. This may reflect the fact that VP35 can inhibit near the “top” of the RLR pathways, leading to efficient inhibition of RLR agonist-mediated activation of interferon regulatory factors and NF-κB. In contrast, inhibition of TLR3 and TLR4 signaling by VP35 may act further downstream, for example, at the levels of IKKε and TBK1, below the point where signals bifurcate to activate IRFs and NF-κB. In this model, EBOV-infected DCs may retain sensitivity to activation by non-IFN-inducing stimuli.
Our data demonstrate that expression of VP35-WT is sufficient to impair several aspects of human MDDC maturation beyond IFN-α/β and proinflammatory cytokine production. VP35, in the absence of other viral factors, can also inhibit chemokine gene expression following SeV infection (data not shown). Furthermore, upregulation of cell surface markers of DC maturation, CD40 and CD80, was impaired, as was T cell activation. These data are consistent with previous studies where expression of VP35 was demonstrated to suppress IFN-α production in human MDDCs (4) and where delivery of VP35 in the context of an HSV-1 mutant lacking γ134.5 and thymidine kinase genes had pleiotropic suppressive effects on mouse DCs (22). In the latter study, relative to a control HSV-1 vector, HSV-1 VP35 inhibited upregulation of costimulatory molecules on the surface of the DCs, induction of proinflammatory cytokines and IFN-α/β, and stimulation of allogeneic CD4+ T cells (22). Our study clarified that VP35 can exert such suppressive effects, even when expressed in the absence of other viral proteins, but its suppressive activities do not extend to TLR signaling pathways. Therefore, in the context of DCs, VP35 suppresses multiple aspects of DC maturation when maturation is induced through RLRs. However, the effects of VP35 upon TLR-induced maturation are more limited.
Based on the observations in this study, therapeutic strategies that disrupt or circumvent VP35 function would be expected to increase both innate and adaptive immune responses to EBOV infection, thereby facilitating control and clearance of the virus. Because VP35 mutants lacking dsRNA-binding activity are impaired in the suppression of RLR-mediated activation of MDDCs, therapeutic approaches designed to block this function deserve attention. Because VP35 only partly impaired DC responses to TLRs, the stimulation of non-RLR pathways of DC activation should also be explored as strategies to enhance immunity to EBOV infection in vivo.
ACKNOWLEDGMENTS
This work was supported by NIH-NIAID grants R01AI059536 and U19AI109945 to C.F.B. and NIH-NIAID grant R21 AI096943 to L.C.F.M.
We thank Ana Fernandez-Sesma, Thomas Moran, Reed Shabman, Irene Ramos-Lopez, and Viviana Simon (Icahn School of Medicine at Mount Sinai) for insightful discussions and reagents. We thank Dan Littman (New York University and Howard Hughes Medical Institute) for the gift of the pSIV3+ plasmid and Adolfo García-Sastre (Icahn School of Medicine at Mount Sinai) for EMCV.
Footnotes
Published ahead of print 20 August 2014
REFERENCES
- 1.Feldmann H, Geisbert TW. 2011. Ebola haemorrhagic fever. Lancet 377:849–862. 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bavari S, Bosio CM, Wiegand E, Ruthel G, Will AB, Geisbert TW, Hevey M, Schmaljohn C, Schmaljohn A, Aman MJ. 2002. Lipid raft microdomains: a gateway for compartmentalized trafficking of Ebola and Marburg viruses. J. Exp. Med. 195:593–602. 10.1084/jem.20011500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geisbert TW, Hensley LE, Larsen T, Young HA, Reed DS, Geisbert JB, Scott DP, Kagan E, Jahrling PB, Davis KJ. 2003. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am. J. Pathol. 163:2347–2370. 10.1016/S0002-9440(10)63591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bosio CM, Aman MJ, Grogan C, Hogan R, Ruthel G, Negley D, Mohamadzadeh M, Bavari S, Schmaljohn A. 2003. Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J. Infect. Dis. 188:1630–1638. 10.1086/379199. [DOI] [PubMed] [Google Scholar]
- 5.Mahanty S, Hutchinson K, Agarwal S, McRae M, Rollin PE, Pulendran B. 2003. Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J. Immunol. 170:2797–2801. 10.4049/jimmunol.170.6.2797. [DOI] [PubMed] [Google Scholar]
- 6.Martinez O, Johnson JC, Honko A, Yen B, Shabman RS, Hensley LE, Olinger GG, Basler CF. 2013. Ebola virus exploits a monocyte differentiation program to promote its entry. J. Virol. 87:3801–3814. 10.1128/JVI.02695-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lubaki NM, Ilinykh P, Pietzsch C, Tigabu B, Freiberg AN, Koup RA, Bukreyev A. 2013. The lack of maturation of Ebola virus-infected dendritic cells results from the cooperative effect of at least two viral domains. J. Virol. 87:7471–7485. 10.1128/JVI.03316-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basler CF, Amarasinghe GK. 2009. Evasion of interferon responses by Ebola and Marburg viruses. J. Interferon Cytokine Res. 29:511–520. 10.1089/jir.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cardenas WB, Loo YM, Gale M, Jr, Hartman AL, Kimberlin CR, Martinez-Sobrido L, Saphire EO, Basler CF. 2006. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J. Virol. 80:5168–5178. 10.1128/JVI.02199-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spiropoulou CF, Ranjan P, Pearce MB, Sealy TK, Albarino CG, Gangappa S, Fujita T, Rollin PE, Nichol ST, Ksiazek TG, Sambhara S. 2009. RIG-I activation inhibits ebolavirus replication. Virology 392:11–15. 10.1016/j.virol.2009.06.032. [DOI] [PubMed] [Google Scholar]
- 11.Hartman AL, Dover JE, Towner JS, Nichol ST. 2006. Reverse genetic generation of recombinant Zaire Ebola viruses containing disrupted IRF-3 inhibitory domains results in attenuated virus growth in vitro and higher levels of IRF-3 activation without inhibiting viral transcription or replication. J. Virol. 80:6430–6440. 10.1128/JVI.00044-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hartman AL, Ling L, Nichol ST, Hibberd ML. 2008. Whole-genome expression profiling reveals that inhibition of host innate immune response pathways by Ebola virus can be reversed by a single amino acid change in the VP35 protein. J. Virol. 82:5348–5358. 10.1128/JVI.00215-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prins KC, Delpeut S, Leung DW, Reynard O, Volchkova VA, Reid SP, Ramanan P, Cardenas WB, Amarasinghe GK, Volchkov VE, Basler CF. 2010. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J. Virol. 84:3004–3015. 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prins KC, Cardenas WB, Basler CF. 2009. Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKKepsilon and TBK-1. J. Virol. 83:3069–3077. 10.1128/JVI.01875-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang TH, Kubota T, Matsuoka M, Jones S, Bradfute SB, Bray M, Ozato K. 2009. Ebola Zaire virus blocks type I interferon production by exploiting the host SUMO modification machinery. PLoS Pathog. 5:e1000493. 10.1371/journal.ppat.1000493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kubota T, Matsuoka M, Chang TH, Tailor P, Sasaki T, Tashiro M, Kato A, Ozato K. 2008. Virus infection triggers SUMOylation of IRF3 and IRF7, leading to the negative regulation of type I interferon gene expression. J. Biol. Chem. 283:25660–25670. 10.1074/jbc.M804479200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leung DW, Prins KC, Borek DM, Farahbakhsh M, Tufariello JM, Ramanan P, Nix JC, Helgeson LA, Otwinowski Z, Honzatko RB, Basler CF, Amarasinghe GK. 2010. Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nat. Struct. Mol. Biol. 17:165–172. 10.1038/nsmb.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bale S, Julien JP, Bornholdt ZA, Kimberlin CR, Halfmann P, Zandonatti MA, Kunert J, Kroon GJ, Kawaoka Y, MacRae IJ, Wilson IA, Saphire EO. 2012. Marburg virus VP35 can both fully coat the backbone and cap the ends of dsRNA for interferon antagonism. PLoS Pathog. 8:e1002916. 10.1371/journal.ppat.1002916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kimberlin CR, Bornholdt ZA, Li S, Woods VL, Jr, MacRae IJ, Saphire EO. 2010. Ebolavirus VP35 uses a bimodal strategy to bind dsRNA for innate immune suppression. Proc. Natl. Acad. Sci. U. S. A. 107:314–319. 10.1073/pnas.0910547107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leung DW, Ginder ND, Fulton DB, Nix J, Basler CF, Honzatko RB, Amarasinghe GK. 2009. Structure of the Ebola VP35 interferon inhibitory domain. Proc. Natl. Acad. Sci. U. S. A. 106:411–416. 10.1073/pnas.0807854106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luthra P, Ramanan P, Mire CE, Weisend C, Tsuda Y, Yen B, Liu G, Leung DW, Geisbert TW, Ebihara H, Amarasinghe GK, Basler CF. 2013. Mutual antagonism between the Ebola virus VP35 protein and the RIG-I activator PACT determines infection outcome. Cell Host Microbe 14:74–84. 10.1016/j.chom.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin H, Yan Z, Prabhakar BS, Feng Z, Ma Y, Verpooten D, Ganesh B, He B. 2010. The VP35 protein of Ebola virus impairs dendritic cell maturation induced by virus and lipopolysaccharide. J. Gen. Virol. 91:352–361. 10.1099/vir.0.017343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leung LW, Park MS, Martinez O, Valmas C, Lopez CB, Basler CF. 2011. Ebolavirus VP35 suppresses IFN production from conventional but not plasmacytoid dendritic cells. Immunol. Cell Biol. 89:792–802. 10.1038/icb.2010.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berger G, Durand S, Goujon C, Nguyen XN, Cordeil S, Darlix JL, Cimarelli A. 2011. A simple, versatile and efficient method to genetically modify human monocyte-derived dendritic cells with HIV-1-derived lentiviral vectors. Nat. Protoc. 6:806–816. 10.1038/nprot.2011.327. [DOI] [PubMed] [Google Scholar]
- 25.Yee JK, Friedmann T, Burns JC. 1994. Generation of high-titer pseudotyped retroviral vectors with very broad host range. Methods Cell Biol. 43(Part A):99–112. [DOI] [PubMed] [Google Scholar]
- 26.Demaison C, Parsley K, Brouns G, Scherr M, Battmer K, Kinnon C, Grez M, Thrasher AJ. 2002. High-level transduction and gene expression in hematopoietic repopulating cells using a human imunodeficiency [sic] virus type 1-based lentiviral vector containing an internal spleen focus forming virus promoter. Hum. Gene Ther. 13:803–813. 10.1089/10430340252898984. [DOI] [PubMed] [Google Scholar]
- 27.Aguirre S, Maestre AM, Pagni S, Patel JR, Savage T, Gutman D, Maringer K, Bernal-Rubio D, Shabman RS, Simon V, Rodriguez-Madoz JR, Mulder LC, Barber GN, Fernandez-Sesma A. 2012. DENV inhibits type I IFN production in infected cells by cleaving human STING. PLoS Pathog. 8:e1002934. 10.1371/journal.ppat.1002934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Negre D, Mangeot PE, Duisit G, Blanchard S, Vidalain PO, Leissner P, Winter AJ, Rabourdin-Combe C, Mehtali M, Moullier P, Darlix JL, Cosset FL. 2000. Characterization of novel safe lentiviral vectors derived from simian immunodeficiency virus (SIVmac251) that efficiently transduce mature human dendritic cells. Gene Ther. 7:1613–1623. 10.1038/sj.gt.3301292. [DOI] [PubMed] [Google Scholar]
- 29.Manel N, Hogstad B, Wang Y, Levy DE, Unutmaz D, Littman DR. 2010. A cryptic sensor for HIV-1 activates antiviral innate immunity in dendritic cells. Nature 467:214–217. 10.1038/nature09337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kato H, Takeuchi O, Sato S, Yoneyama M, Yamamoto M, Matsui K, Uematsu S, Jung A, Kawai T, Ishii KJ, Yamaguchi O, Otsu K, Tsujimura T, Koh CS, Reis e Sousa C, Matsuura Y, Fujita T, Akira S. 2006. Differential roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature 441:101–105. 10.1038/nature04734. [DOI] [PubMed] [Google Scholar]
- 31.Geisbert TW, Young HA, Jahrling PB, Davis KJ, Larsen T, Kagan E, Hensley LE. 2003. Pathogenesis of Ebola hemorrhagic fever in primate models: evidence that hemorrhage is not a direct effect of virus-induced cytolysis of endothelial cells. Am. J. Pathol. 163:2371–2382. 10.1016/S0002-9440(10)63592-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bray M, Geisbert TW. 2005. Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. Int. J. Biochem. Cell Biol. 37:1560–1566. 10.1016/j.biocel.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 33.Loo YM, Fornek J, Crochet N, Bajwa G, Perwitasari O, Martinez-Sobrido L, Akira S, Gill MA, Garcia-Sastre A, Katze MG, Gale M., Jr 2008. Distinct RIG-I and MDA5 signaling by RNA viruses in innate immunity. J. Virol. 82:335–345. 10.1128/JVI.01080-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okano S, Yonemitsu Y, Shirabe K, Kakeji Y, Maehara Y, Harada M, Yoshikai Y, Inoue M, Hasegawa M, Sueishi K. 2011. Provision of continuous maturation signaling to dendritic cells by RIG-I-stimulating cytosolic RNA synthesis of Sendai virus. J. Immunol. 186:1828–1839. 10.4049/jimmunol.0901641. [DOI] [PubMed] [Google Scholar]
- 35.Hartman AL, Towner JS, Nichol ST. 2004. A C-terminal basic amino acid motif of Zaire ebolavirus VP35 is essential for type I interferon antagonism and displays high identity with the RNA-binding domain of another interferon antagonist, the NS1 protein of influenza A virus. Virology 328:177–184. 10.1016/j.virol.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 36.Schumann M, Gantke T, Muhlberger E. 2009. Ebola virus VP35 antagonizes PKR activity through its C-terminal interferon inhibitory domain. J. Virol. 83:8993–8997. 10.1128/JVI.00523-09. [DOI] [PMC free article] [PubMed] [Google Scholar]