Abstract
Most persons infected with enterically transmitted viruses shed large amounts of virus in feces for days or weeks, both before and after onset of symptoms. Therefore, viruses causing gastroenteritis may be detected in wastewater, even if only a few persons are infected. In this study, the presence of eight pathogenic viruses (norovirus, astrovirus, rotavirus, adenovirus, Aichi virus, parechovirus, hepatitis A virus [HAV], and hepatitis E virus) was investigated in sewage to explore whether their identification could be used as an early warning of outbreaks. Samples of the untreated sewage were collected in proportion to flow at Ryaverket, Gothenburg, Sweden. Daily samples collected during every second week between January and May 2013 were pooled and analyzed for detection of viruses by concentration through adsorption to milk proteins and PCR. The largest amount of noroviruses was detected in sewage 2 to 3 weeks before most patients were diagnosed with this infection in Gothenburg. The other viruses were detected at lower levels. HAV was detected between weeks 5 and 13, and partial sequencing of the structural VP1protein identified three different strains. Two strains were involved in an ongoing outbreak in Scandinavia and were also identified in samples from patients with acute hepatitis A in Gothenburg during spring of 2013. The third strain was unique and was not detected in any patient sample. The method used may thus be a tool to detect incipient outbreaks of these viruses and provide early warning before the causative pathogens have been recognized in health care.
INTRODUCTION
Enterically transmitted infections are common and can be caused by a large number of different pathogens, including viruses. Many of these viruses cause subclinical infections, which is why their prevalence is difficult to estimate. Increased urbanization and high frequency of global travel favor the emergence and reemergence of enteric pathogens and outbreaks of gastrointestinal infections.
Most of the fecal-oral-transmitted viruses are highly resistant in the water environment, where they may persist at high levels despite the decontamination processes commonly used for drinking water and sewage treatment (1, 2). Most of them are nonenveloped viruses, such as norovirus, enterovirus, Aichi virus, parechovirus, hepatitis A and E viruses (HAV and HEV, respectively), astrovirus, rotavirus, and adenovirus (Ad). These viruses cause outbreaks or sporadic cases with a wide range of symptoms from mild to severe gastroenteritis to meningitis, respiratory disease, conjunctivitis, paralysis, or hepatitis.
Human norovirus (HuNoV), a positive-sense RNA virus, is one of the leading gastroenteritis agents and has become an increasing public concern worldwide. It belongs to the Caliciviridae family and is classified into 5 genogroups (GI to GV), of which GI, GII, and GIV infect humans. While GII causes the majority of reported outbreaks, GI is frequently found in environmental water settings (3, 71).
Aichi virus, parechovirus, and hepatitis A virus all belong to the Picornaviridae family and are spread globally. They possess a single-stranded positive-sense RNA genome of 7 to 8 kb. Aichi virus causes gastroenteritis and infects both children and adults. Human parechoviruses infect mainly infants, causing mild or severe gastroenteritis, meningitis, encephalitis, and paralysis (4–6). Hepatitis A and E viruses may cause sporadic hepatitis as well as large outbreaks. Hepatitis A virus (HAV) is classified into 6 genotypes (I to VI), with somewhat different geographical distributions, with types IA and IB being common in Europe (7).
Hepatitis E virus (HEV) belongs to the Hepeviridae family and is a positive-sense RNA virus. HEV infecting humans is classified into four genotypes (1, 2, 4). Types 1 and 2 infect only humans, and the infection has a high mortality rate among pregnant females and young children (8). These two types may cause large waterborne outbreaks (8). Types 3 and 4 have zoonotic spread, and have been identified in samples from many different mammals apart from humans, such as pigs, wild boar, deer, moose, and mongooses (8, 9).
Astroviruses belong to the Astroviridae family and are also positive-sense RNA viruses. They cause predominately gastroenteritis in children under the age of 2 years. Elderly persons and immunocompromised individuals are involved in up to 20% of the clinical cases and 0.5 to 15% of the outbreaks (10).
Rotavirus belongs to the Reoviridae family. Its genome consists of 11 segments of double-stranded RNA (11). Globally nearly every child has been infected by rotavirus by the age of 5 years (12), and it is the most common cause of severe diarrhea among infants. However, it also causes diarrhea among elderly persons. Although rotavirus infection is prevalent worldwide, most deaths from this infection occur in developing countries, mostly due to dehydration (13).
There are seven species of human adenoviruses (Ads), classified A through G in the Adenoviridae family. Each species is further classified into different serotypes (14–16). The genome is a nonsegmented DNA 26 to 45 kbp in length. Gastroenteritis is caused mainly by Ad-F types 40 and 41 and Ad-G type 52. Most of the Ads belonging to the other species are also spread fecally and orally. They may cause respiratory diseases, conjunctivitis, and, more rarely hepatitis, pancreatitis, or encephalitis.
It is possible to detect these viruses in sewage, since each individual sheds around 100 g fecal matter per day (17, 18), and 105 to 109 enteric virus particles per gram of stool are released daily from an infected individual (19).
During the study period, there was an ongoing hepatitis A outbreak caused by two different IB strains in Scandinavia (20). By 17 March 2013, there were 52 hepatitis A cases infected with IB strains in Scandinavia, and at least 28 of these persons were infected by the outbreak strains (20). This outbreak is thought to have been caused by contaminated frozen strawberries.
Several techniques have been developed to detect viruses in sewage (21–24). Many of these have been developed for poliovirus surveillance as part of the WHO polio eradication program (25). The techniques have also been used to detect noroviruses and other viruses in water (26–28). In this study, human viruses in sewage were concentrated and detected by PCR to investigate if this technique could be used as an early warning system for incipient outbreaks of enterically transmitted viruses.
MATERIALS AND METHODS
Sewage treatment plant and sampling.
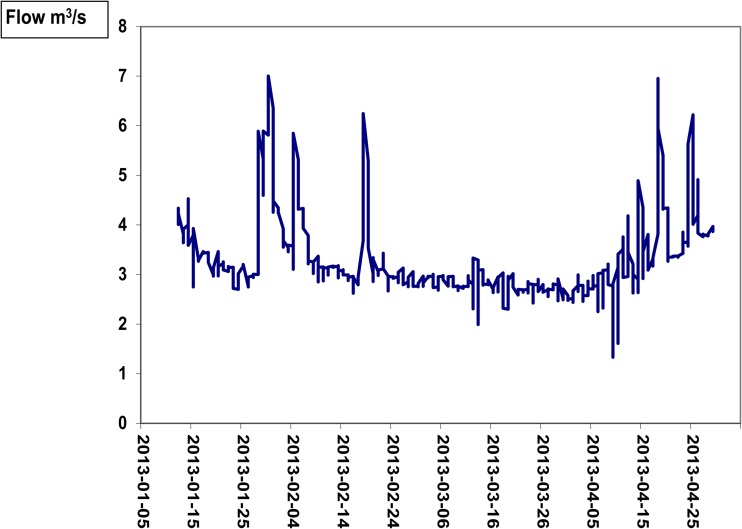
Sewage samples were collected at the wastewater treatment plant Ryaverket (owned and run by Gryaab AB), Gothenburg, Sweden. The plant receives and treats wastewater from a population of 690,000 in the Gothenburg region and industrial wastewater and storm water. While the inflow of wastewater from households is fairly constant during the year, the total flow increases during periods of heavy rain due the inflow of storm water. Such daily variations in the flow during the sampling period are shown in Fig. 1.
FIG 1.
Variations in real time of the inflow of sewage to the treatment plant Ryaverket, Gothenburg, Sweden, for the study period between 12 January 2013 and 20 April 2013. Dates are given in the format year-month-day.
The sampling in the present study encompassed every second week, between 14 January and 15 April 2013 (weeks 3, 5, 7, 9, 11, 13, and 15). Wastewater was sampled over 24 h by a fixed-site sampler (model Maxx SP II; Mess-u. Probenahmetechnik GmbH, Rangendingen, Germany) routinely used at Ryaverket for monitoring and control of the sewage. The volume collected was proportional to the flow of the influent wastewater. The sampler was adjusted to withdraw 30 ml wastewater per cycle from the inlet pipe of the sewage plant. Combined weekly samples were prepared by pooling daily collected samples. All daily samples were stored in a refrigerator at +4°C before weekly pooling, and the pooled samples were kept frozen at −20C before analysis.
Virus concentration.
The concentration of viruses from the weekly sample of wastewater was performed by virus adsorption to milk powder, mainly as previously described (29). Briefly, viruses in 1,000 ml sewage were adsorbed to 10 g acidified skim milk powder (pH 3.5 [Difco]) by stirring at room temperature for 8 h. The skim milk powder was precipitated by centrifugation at 4,500 × g. The pellet was dissolved by addition of 3 ml phosphate buffer (pH 7.5) and further treated with 6 ml 0.25 M glycine buffer (pH 9.5) for 45 min. An additional 10 ml phosphate buffer was added, and centrifugation was performed at 180,000 × g for 2 h. The pellets obtained were dissolved in 200 μl phosphate buffer (pH 7.5) and stored at −20°C.
To estimate the efficiency of the technique for virus concentration from sewage, ∼0.5 cm3 of three norovirus genogroup II (GII)-positive fecal samples was dissolved in 2.5 ml physiologic NaCl and added to 1,000 ml of the first sewage sample that was collected during week 3 prior to the addition of skimmed milk powder and concentration of viruses. The added fecal extract had a threshold cycle (CT) value of 14.7 in the PCR assay for norovirus GII, which corresponded to 3.5 ×109 genomes/ml cDNA, based on CT values obtained from dilutions of a known concentration of a pUC57plasmid with all targeted regions cloned into the EcoRV site (pUC57cl; GenScript HK, Ltd., Hong Kong). The fecal extract was negative for the other investigated fecal-oral-transmitted viruses. The values obtained after concentration were compared with those obtained from concentration of virus in sewage without addition of fecal suspensions.
Extraction of nucleic acid.
The DNeasy blood and tissue kit (Qiagen) was used for extraction of nucleic acids from 100 μl of concentrated virus solution from sewage or patient samples according to the manufacturer's instructions. Extraction was also performed directly from 100 μl raw sewage without prior concentration of virus by adsorption to milk powder. The nucleic acids were eluted with 100 μl RNase-free H2O (Sigma) and stored at −70°C.
Synthesis of cDNA.
For cDNA synthesis, 5 μl of extracted nucleic acids was added to 6.6 μl of RNase-free H2O (Sigma), 1 μl (4 μg/μl) random primer (Roche), 0.4 μl (25 mM) deoxynucleoside triphosphate (dNTP) (Roche), 4 μl 5× First Strand buffer (Invitrogen, Carlsbad, CA), 1 μl dithiothreitol (DTT) (Invitrogen), 1 μl RNase OUT (Invitrogen), and 1 μl Superscript III (Invitrogen), which gave a total reaction mixture volume of 20 μl. For detection of hepatitis A virus (HAV), the antisense primer used in PCR, HA3381AS (Table 1), was used in the cDNA reaction instead of random primers. The cDNA synthesis was performed at 50°C for 60 min followed by inactivation of the reverse transcriptase at 70°C for 15 min. The cDNA was stored at −20°C until use.
TABLE 1.
Primers and probes targeting the investigated viruses in sewage and patient samples
| Virus | Sequence of: |
Reference or source | ||
|---|---|---|---|---|
| Forward primer | Reverse primer | Probe | ||
| Norovirus GI | YTGGATGCGNTTYCATGA | CTTAGACGCCATCATCATT | AGATYGCGATCYCCTGTCCAAGATCGCGGTCTCCTGTCCA | Modified from reference 73 |
| Norovirus GII | TGGAYTTTTAYGTGCCCAG | CGACGCCATCTTCATTCAC | AGCCAGATTGCGATCGCCC | 74 |
| Astrovirus | TCTTCTCAACGTGTCCGTATCTAATCAACGTGTCCGTA | TTTTGGTCCTGTGACACC | ATTGTCAATAARCAACTCAGGAACA | This study |
| Adenovirus | CTCGACATGACTTTTGAGGT | GTAGACGGCCTCGATGAC | AGCCCACACTTCT | Modified from reference 75 |
| Aichi virus | TGGGCTGCCATGTACAA | GAGCCGTTGACGGTCAC | CACCCACTCCATGTGGAATTGC | This study |
| HAV (qPCR) | AAAGTGGAGTTTASTCAGTGTAAAGTGGAATTYACTCAGTGTAAAGTGGAATTTACTCAATGT | ACWGCAGGAAAATTAATCATG | TGAATGTGGTCTCCAAAACGCTGAATGTAGTCTCCAAAACGC | This study |
| Parechovirus | ATGGCGTGCCATAACTCTAATGGCGTGCCATAATTCTA | AGAGGCACCTGTTACCAGAGGGGCACCTGTTACCACAGAGGCATCTGTTACCAG | CTTATGCTCACACAGCCATCCTCT | This study |
| Rotavirus | ACCATCTACACATGACCCTCACCATCTTCACGTAACCCTC | GGTCACATAACGCCC | ATGAGCACAATAGTTAAAAGCTAACACTGTC | Modified from reference 76 |
| HEV | GGTGGTTTCTGGGGTGACACGCGGCACACGATCAG | AGGGGTTGGTTGGATGAAGGGGTTGGTTGGGTGAA | TGATTCTCAGCCCTTTGATTCCCAGCCCTT | This study |
| HAV (PCR for sequencing first PCR) | AAYGTTGCTTCYCATGTYAGRGT | ACCADGCCATDCCATCHACATC | 77 | |
| HAV (nested PCR) | ATGYTTTGCWCCHCTHTATCAT | ACCADGCCATDCCATCHACATC | 77 | |
Detection of viruses by real-time qPCR.
Primers for hepatitis A virus (HAV), hepatitis E virus (HEV), rotavirus, adenovirus, Aichi virus, astrovirus, and parechovirus were used at a concentration of 600 nM, and the primers for norovirus detection were used at a concentration of 900 nM. A 200 nM concentration of the probes was used in the quantitative PCR (qPCR) for seven of the viruses. For HEV, 300 nM probe was used in the qPCR. The sequences of the primers and probes used are given in Table 1. A total volume of 50 μl reaction mixture contained 5 μl of cDNA or diluted plasmid pUC57cl, 25 μl universal master mix containing AmpliTaq Gold DNA polymerase, AmpErase UNG, dNTPs, dUTP, passive reference, and optimized buffer components (Applied Biosystems), as well as the primers and probes at the concentrations given above. The qPCRs were optimized with regard to annealing and extension temperatures and to primer and probe concentrations by using dilution series of plasmid pUC57cl containing the targeted regions. For HAV, HEV, and astrovirus, the qPCR had also been optimized for detection of these viruses in patient samples, and this qPCR has since long been used routinely for diagnosis of these viruses. Attempts were made to perform multiple qPCRs for detection of several viruses simultaneously in the same assay, but since the sensitivity of the assay then decreased 10- to 100-fold, single qPCRs were performed. The qPCR for HAV, HEV, rotavirus, and adenovirus was performed by an initial incubation at 50°C for 2 min and 95°C for 10 min followed by amplification consisting of 45 cycles of 95°C for 15 s and at 55°C for 1 min. The qPCRs for Aichi virus, astrovirus, and parechovirus were performed as for the hepatitis A and E viruses, but with extension at 60°C for 1 min. The qPCRs were performed in a 7300 real-time PCR system (Applied Biosystems). All samples were tested in triplicate with each qPCR.
Calculation of the number of viral genomes and the approximate number of infected individuals shedding 1011 virus particles per day required for detection of viral genomes in sewage.
The detection limit for the different viruses by qPCR was 6 to 10 viral genomes/50-μl reaction mixture, based on dilution series of a known amount of the pUC57cl plasmid with all targeted regions cloned into the EcoRV site.
The CT values obtained for sewage samples in the qPCR were used to calculate the number of viral genomes (Ci) by performing linear regression of the CT values obtained from serial dilutions of pUC57cl in relation to the dilutions of the plasmid.
An infected individual is assumed to excrete between 107 and 1011 norovirus, HAV, enterovirus, and adenovirus particles per day (19). The number of virus particles excreted daily is, to our knowledge, not known for the other investigated viruses. An infected individual was therefore assumed to excrete similar amounts of all investigated viruses. Calculations of the number of infected persons shedding viruses in this study were based on the maximum amount of virus that is shed per day by a newly infected person, 1011 virus particles/day, thereby estimating the lowest number of individuals shedding virus into the wastewater.
The number of virus particles that was expected to be present in the sewage on the daily basis from one infected person excreting (Cexp) was calculated for each week according to the following equation: Cexp = 1011/{[Σ(respective daily flow)]/7}.
The number of potentially infected individuals (Ninfected) based on the presence of the respective virus in the sewage was estimated as Ninfected = Ci/Cexp.
Patient samples.
Between the end of December 2012 and mid-May 2013, there were nine patients notified for hepatitis A infection in the county of Västra Götaland. Five of these patients lived in the Gothenburg area, and wastewater from their households passed through Ryaverket. Serum samples from these patients were sent for hepatitis A diagnosis to the Clinical Microbiology Laboratory (CML) at Sahlgrenska University Hospital. During the study period, there was also an outbreak of norovirus in Gothenburg. Throughout the sewage sampling period, a total of 970 fecal samples from patients with gastroenteritis were sent to the CML for diagnosis of norovirus, sapovirus, rotavirus, astrovirus, and adenovirus. No patient was identified with HEV IgM or had detectable HEV RNA during the study period.
PCR amplification of HAV RNA.
For the first PCR, 5 μl of cDNA with HAV-specific primers was added to 34.4 μl RNase-free water (Sigma), 5 μl 10× TaqMan buffer (Applied Biosystems, Foster City, CA), 3 μl 25 mM MgCl2 (Applied Biosystems), 0.4 μl (25 mM) dNTP (Roche Diagnostics, Bromma, Sweden), 200 nM sense primer, 200 nM antisense primer, and 1 U (5 U/μl) Taq polymerase in a total 50-μl reaction volume for each PCR. The sequences of the primers covering the N-terminal region of VP1 are given in Table 1. The PCR was performed by using an initial step at 94°C for 3 min and then 40 cycles at 94°C for 20 s, 54°C for 30 s, and 72°C for 1 min. From the product of this initial PCR, 5 μl was used in a nested PCR, which was performed as described above but with other antisense primers (Table 1). The amplified fragments were visualized on a 1.5% agarose gel with DNA GelRed (Biotium, Hayward, CA).
Sequencing.
Amplified PCR fragments were purified using the QIAquick PCR purification kit (Qiagen) according to the manufacturer's instructions. The eluted DNA was sequenced with the BigDye terminator cycle sequencing ready reaction kit (Applied Biosystems) using the same primers as in the second PCR. After the cycle sequence reaction, the amplified DNA fragments were precipitated by adding 25 μl 95% ethanol and 1 μl 3 M NaAc to each tube and incubated at room temperature for 10 min prior to centrifugation for 45 min. The supernatant was removed, and the pellet was washed with 70% ethanol. Each pellet was dissolved in 15 μl formamide before loading for separation and detection on an Avanti3130XL genetic analyzer (Applied Biosystems).
Sequence analysis.
The sequences obtained were checked manually against the chromatograms with the program SeqMan in the DNASTAR program package (DNASTAR, Inc., Madison, WI). The corrected sequences were aligned with the corresponding region of 500 sequences obtained from GenBank by use of the ClustalX2 program (30). After manual correction of the alignment, phylogenetic analysis was performed with the PHYLIP program package, version 3.65 (31). The F84 algorithm with a gamma correction and a transition/transversion ratio of 3.76 was used for genomic distance determination by the DNADIST program. Phylogenetic trees were constructed using the unweighted pair-group method using arithmetic averages (UPGMA) in the NEIGHBOR program. The trees were visualized by the TreeView program (32).
Nucleotide sequence accession numbers.
The HAV sequences obtained in this study have been deposited in GenBank under accession no. KM486802 to KM486807.
RESULTS
qPCR optimization and estimation of virus recovery.
All qPCRs were optimized with regard to primer and probe concentrations and annealing and extension temperatures by analyzing dilution series of plasmid pUC54cl containing all targeted regions. The sensitivity varied from 6 to 10 genomes/assay, which corresponds to 120 to 200 viral genomes/ml. No virus could be detected by qPCR when nucleic acids were extracted directly from wastewater without prior concentration.
To estimate the sensitivity of the technique for virus detection in sewage, 2.5 ml of a pool of four dissolved fecal samples positive for norovirus GII (CT of 14.7, corresponding to approximately 4 × 1010 viral genomes/2.5 ml fecal samples) was added to 1,000 ml sewage from week 3 before virus concentration. The same amount of sewage without addition of fecal extracts was also concentrated and was shown to be negative for norovirus GII. After concentration to100 μl and nucleic acid extraction, qPCR was performed for detection of norovirus GII. The CT value obtained was 13.6, which corresponded to approximately 7.6 × 109 norovirus GII genomes/ml cDNA or 3.8 ×1010 genomes/ml extracted RNA, which in turn corresponded to 3.8 × 109 genomes in 1 liter raw sewage. About 10% of the amount of virus added could thus be detected in the sewage.
Virus detected in sewage and number of patients diagnosed.
Norovirus, sapovirus, rotavirus, astrovirus, and adenovirus could be detected in all sewage samples and also during weeks when there were no positive patient samples. The CT values obtained and the estimated amounts of virus genomes are given in Table 2. Aichi virus was also detected in all sewage samples, while parechovirus could not be detected in any of the samples (Table 2).
TABLE 2.
Expected viral particles shed per day by persons secreting 1011 virus particles/day and compiled results for the viruses detected in sewagea
| Parameter and virus | Result for sampling wk: |
||||||
|---|---|---|---|---|---|---|---|
| 3 | 5 | 7 | 9 | 11 | 13 | 15 | |
| Cexpb | 343 | 250 | 383 | 401 | 412 | 435 | 385 |
| Norovirus GI | |||||||
| Sewage CT | 36.6 | 36.7 | 32.7 | 31.2 | 34.9 | >40 | >40 |
| Avg virus concn/liter | 70 | 65 | 1,200 | 3,500 | 250 | <10 | <10 |
| Estimated virus concn based on recovery of 10% | 700 | 650 | 12,000 | 35,000 | 2,500 | ||
| Avg load of virus/day | 100 | 100 | 1,700 | 5,000 | 350 | ||
| Nexpc | 0.3 | 0.4 | 4 | 12 | 0.8 | 0 | 0 |
| No. of persons diagnosed/tested (%) | 0 | 0 | 0 | 0 | 6/159 (3.8) | 4/166 (2.4) | 2/142 (1.4) |
| Norovirus GII | |||||||
| Sewage CT | 16d | 29.4 | 24.7 | 25 | 25.2 | 26.4 | 28 |
| Avg virus concn/liter | 12,400 | 320,000 | 270,000 | 230,000 | 100,000 | 33,000 | |
| Estimated virus concn based on recovery of 10% | 124,000 | 3.2 × 106 | 2.7 × 106 | 2.3 × 106 | 1 × 106 | 330,000 | |
| Avg load of virus/day | 17,700 | 460,000 | 380,000 | 330,000 | 140,000 | 47,000 | |
| Nexp | 70 | 1,200 | 950 | 800 | 320 | 120 | |
| No. of persons diagnosed/tested (%) | 20/90 (22) | 39/122 (32) | 44/135 (33) | 64/156 (41) | 62/159 (39) | 45/166 (27) | 42/142 (30) |
| Astrovirus | |||||||
| Sewage CT | 27.7 | 25.6 | 24.2 | 29.6 | 26.3 | 27.2 | 24.3 |
| Avg virus concn/liter | 40,300 | 180,000 | 460,000 | 10,700 | 107,000 | 57,000 | 430,000 |
| Estimated virus concn based on recovery of 10% | 403,000 | 1.8 × 106 | 4.6 × 106 | 107,000 | 1.1 × 106 | 570,000 | 4.3 × 106 |
| Load avg virus/day | 57,500 | 250,000 | 660,000 | 15,300 | 160,000 | 81,500 | 610,000 |
| Nexp | 170 | 1,000 | 1,720 | 40 | 390 | 190 | 1,600 |
| No. of persons diagnosed/tested (%) | 6/90 (6.7) | 0/122 | 0/135 | 4/156 (2.4) | 9/159 (5.7) | 3/166 (1.8) | 4/142 (2.8) |
| Adenovirus | |||||||
| Sewage CT | 25.5 | 26.5 | 25.2 | 25.9 | 24.7 | 27.2 | 26.9 |
| Avg virus concn/liter | 190,000 | 93,000 | 230,000 | 140,000 | 330,000 | 57,000 | 70,500 |
| Estimated virus concn based on recovery of 10% | 1.9 × 106 | 930,000 | 2.3 × 106 | 1.4 × 106 | 3.3 × 106 | 570,000 | 705,000 |
| Avg load of virus/day | 270,000 | 133,000 | 330,000 | 200,000 | 470,000 | 81,000 | 100,700 |
| Nexp | 1,100 | 530 | 860 | 500 | 1,100 | 190 | 260 |
| No. of persons diagnosed/tested (%) | 4/90 (4.4) | 4/122 (3.3) | 5/135 (3.7) | 7/156 (4.5) | 8/159 (5) | 0/166 | 0/142 |
| Rotavirus | |||||||
| Sewage CT | 31.7 | 31.9 | 31.3 | 34 | 31.1 | 32.8 | 33.2 |
| Avg virus concn/liter | 2,500 | 2,100 | 3,300 | 500 | 3,800 | 1,100 | 870 |
| Estimated virus concn based on recovery of 10% | 25,000 | 21,000 | 33,000 | 5,000 | 38,000 | 11,000 | 8,700 |
| Avg virus load/day | 3,600 | 3,000 | 4,700 | 710 | 5,400 | 1,600 | 1,200 |
| Nexp | 10 | 12 | 12 | 2 | 13 | 4 | 3 |
| No. of persons diagnosed/tested (%) | 0/90 | 1/122 (0.8) | 1/135 (0.7) | 0/156 | 6/159 (3.8) | 17/166 (10.2) | 9/142 (6.3) |
| Aichi virus | |||||||
| Sewage CT | 31.2 | 33.2 | 33.6 | 36.5 | 35.4 | 37 | 33.4 |
| Avg virus concn/liter | 3,500 | 870 | 650 | 87 | 180 | 60 | 760 |
| Estimated virus concn based on recovery of 10% | 35,000 | 8,700 | 6,500 | 870 | 1,800 | 600 | 7,600 |
| Avg load of virus/day | 5,000 | 1,200 | 930 | 120 | 260 | 86 | 1,100 |
| Nexp | 14 | 5 | 2 | 0.3 | 0.6 | 0.2 | 3 |
| No. of persons diagnosed | NDe | ND | ND | ND | ND | ND | ND |
| HAV | |||||||
| Sewage CT | >45 | 37.7 | 34.1 | 37.3 | 41.2 | 40.7 | >45 |
| Avg virus concn/liter | <10 | 120 | 1,400 | 150 | 12 | 20 | <10 |
| Estimated virus concn based on recovery of 10% | 1,200 | 14,000 | 1,500 | 120 | 200 | ||
| Avg load of virus/day | 170 | 6,700 | 210 | 17 | 29 | ||
| Nexp | 0 | 0.7 | 17 | 0.5 | 0.1 | 0.1 | |
| No. of persons diagnosed | 1 + 3f | 0 | 1g | 1h | 1 | 0 | 2i |
| HEV | |||||||
| Sewage CT | 39.7 | 41 | 39.3 | >45 | 40.2 | 39 | 38.5 |
| Avg virus concn/liter | 95 | 40 | 120 | <10 | 70 | 155 | 215 |
| Estimated virus concn based on recovery of 10% | 950 | 400 | 1,200 | 700 | 1,550 | 2,150 | |
| Avg load of virus/day | 140 | 60 | 170 | 100 | 220 | 307 | |
| Nexp | 0.4 | 0.2 | 0.4 | 0 | 0.2 | 0.5 | 1 |
| No. of persons diagnosed | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Shown are the number of expected viral particles shed per day by persons secreting 1011 virus particles/day and compiled results for the viruses detected in sewage, presented as CT values (estimated number of viral genomes/liter sewage during the week of collection and per day). In addition, values are given for the number of expected persons shedding 1011 viral particles per day based on the inflow volume of wastewater, as detailed in Materials and Methods. The number of patients diagnosed with the respective gastroenteritis virus is given together with the number of patients investigated routinely for gastroenteritis at the CML for the weeks when sewage was collected.
Cexp, number of expected virus particles/day in the collected sewage from one infected person shedding 1011 particles/day.
Nexp, number of expected persons that excrete 1011 virus particles per day.
Fecal samples positive for norovirus GII were added to the sewage sample before concentration.
ND, not determined.
Three patients were diagnosed in week 52 in 2012.
This patient was diagnosed in week 8.
This patient was diagnosed in week 10.
One of these patients was diagnosed in week 14 and the other in week 19.
The number of infected patients diagnosed with the investigated viruses and the estimated number of patients shedding the virus daily, based on the number of virus genomes detected in sewage, are given in Table 2. Norovirus had the highest concentration of detectable viral genomes, followed by astrovirus, adenovirus, Aichi virus, hepatitis E virus, and hepatitis A virus in declining order of concentration.
Hepatitis E virus was detected at low levels (about 400 to 2,000 viral genomes) in the sewage samples for all weeks, except week 9 (Table 2). The amount of excreted hepatitis E virus particles from an infected individual is not known. If it equals that from a person infected with norovirus and hepatitis A virus, the number of persons shedding the virus varied from one person excreting virus 1 day only during weeks 5 and 11 to one with daily shedding during week 15.
Norovirus GII outbreak.
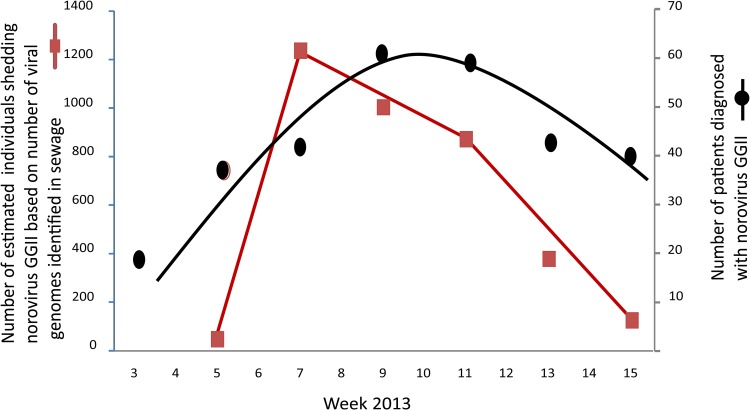
An outbreak of norovirus GII occurred in Gothenburg during the sampling period and was reflected by the detection of 12.4 × 103 to 320 × 103 viral genomes per liter sewage (Table 2). When taking into account a 90% loss of viruses in the method, this amount of viral genomes corresponds to 71 to 1,200 infected persons who shed 1011 virus particles per day. There was a peak in the number of detected norovirus genomes in week 7, followed by a slow decline until week 15. This peak was 2 to 4 weeks before a peak occurred of diagnosed patients with norovirus GII infection, primarily in hospital wards and elder care centers in Gothenburg (Fig. 2).
FIG 2.
Estimation of the number of infected persons that secrete norovirus GII daily during weeks 5, 7, 9, 11, and 13 in 2013 based on the number of viruses identified in the weekly wastewater samples (assuming an infected person shed 1011 particles per day) and the number of patients diagnosed as infected with norovirus GII in the corresponding weeks.
Hepatitis A virus outbreak.
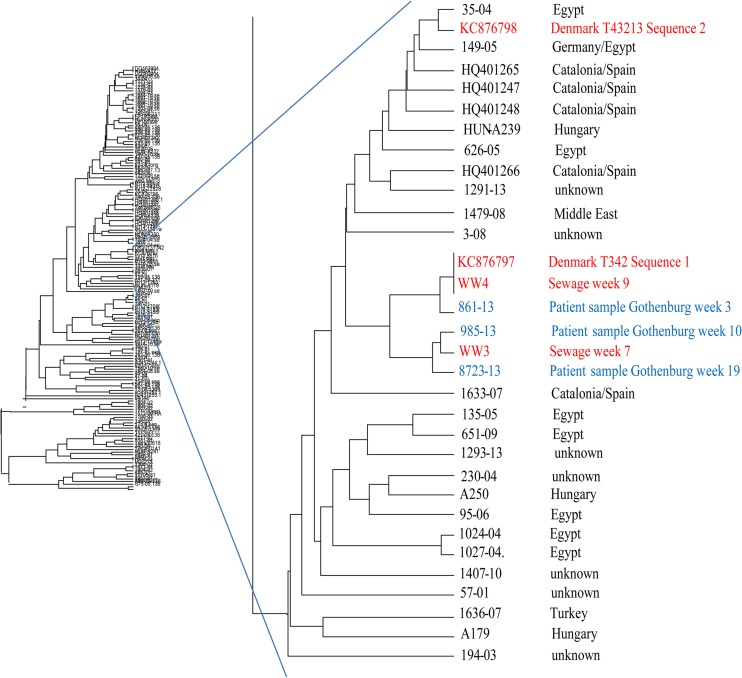
Hepatitis A virus RNA was detected in sewage between weeks 5 and 13. Most viral genomes were detected in week 7, with 14 × 103 viral genomes per liter sewage, followed by a decline until week 15, when HAV RNA could no longer be detected (Table 2). The amount of HAV RNA in wastewater showed that at least one infected individual excreted 1011 particles per day in week 5, followed by 17 daily shedders during week 7. The rapid decline in the amount of HAV RNA in wastewater during weeks 9, 11, and 13 indicated a decrease in the outbreak, with only one person shedding virus for 3 days during week 9 and for only 1 day during the other 2 weeks. Three of the HAV strains found in the effluent samples could be amplified and sequenced in the N-terminal region of VP1. All three strains were of genotype IB. The strain in the sewage collected on week 5 was similar to strains that are common in the Middle East. The other two strains collected during weeks 7 and 9 differed genetically by about 1% from the strains that caused the Scandinavian outbreak (19) (Fig. 3).
FIG 3.
Phylogenetic tree based on 465 nucleotides of the N-terminal part of VP1 in the HAV genome. Shown is the branch with HAV IB strains identified in patients and sewage from Gothenburg. Patient samples are marked in blue and sewage samples and outbreak strains in red.
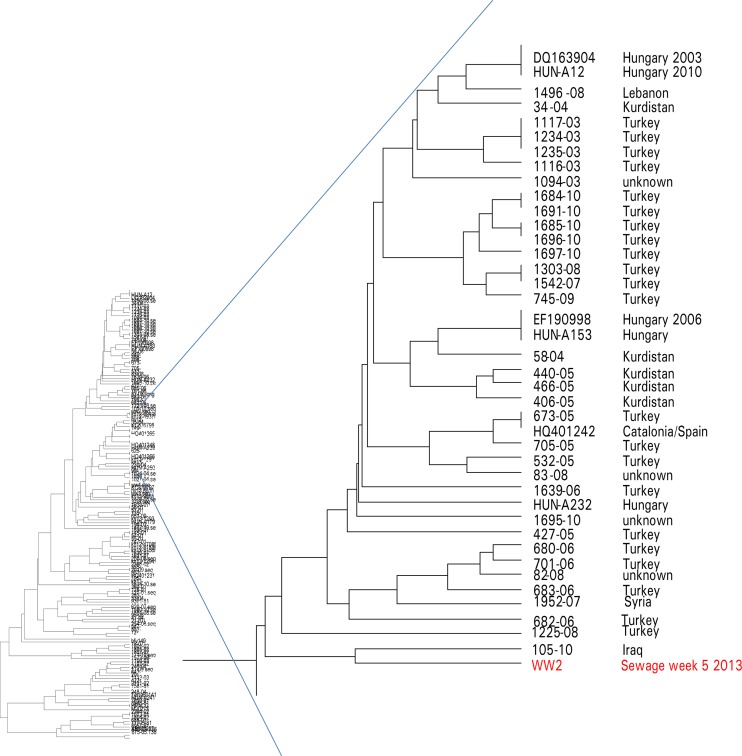
It was possible to amplify HAV RNA in sera from all five notified hepatitis A patients. The amount of HAV in the patient samples was between 3,000 and 1,000,000 genomes/ml (Table 3). The N-terminal part of VP1 could be sequenced for strains from four of the patients and was compared phylogenetically with the HAV strains identified in sewage (Fig. 4). One patient was found to be infected with a genotype IA strain identical to a strain that caused outbreaks in Hungary and The Netherlands in 2012. The other three patients were infected with IB strains similar to the Scandinavian outbreak strains, which were also identified in sewage in weeks 7 and 9. One of these patients had clinical hepatitis in week 3. This strain was most similar to the outbreak strain identified in sewage in week 9. The other two patients were infected with strains similar to the outbreak strain identified in sewage in week 7. One of these patients had clinical hepatitis in week 10 and the other in week 19 (Fig. 4).
TABLE 3.
Strain designation, amount of viral genomes, and HAV genotype in samples from patients with the indicated week of HAV diagnosis in Gothenburga
| Patient strain designation | wk of diagnosis in 2013 | No. of viral genomes/ml in patient sample | Genotype | Similar strain | wk detected in sewage |
|---|---|---|---|---|---|
| 861-13 | 3 | 5.9 × 104 | IB | Outbreak strain | 9 |
| Sewage strain w5 | IB | Strain from Iraq | 5 | ||
| 985-13 | 10, 11c | 0.7 × 104 | IB | Outbreak strain | 7 |
| 2926-13 | 12 | 0.3 × 104 | NDb | Could not be sequenced | |
| 6033-13 | 13 | 123 × 104 | IA | Outbreak strain in Hungary/The Netherlands, 2012 | Not found in sewage |
| 8723-13 | 19 | 1 × 104 | IB | Outbreak strain | 7 |
The designation, amount of viral genomes/ml sample, and genotypes of HAV in samples from patients with the indicated week for HAV diagnosis in Gothenburg are given, together with the genotype of one strain found only in sewage in week 5. In addition, the nucleotide similarity of the strains to other HAV strains is listed, along with the week when the strain was also found in sewage.
ND, not determined.
Last week of sampling.
FIG 4.
Phylogenetic tree based on 465 nucleotides of the N-terminal part of VP1 in the HAV genome. The tree shows part of the HAV IB branch. The identified strain from sewage collected during week 5 in 2013 at Ryaverket, Gothenburg, Sweden, is shown in red.
DISCUSSION
Analysis of seven weekly pooled untreated sewage samples from Ryaverket (a large wastewater treatment plant in Gothenburg) performed in the present study clearly demonstrated the presence of seven different enteric viruses: norovirus, astrovirus, rotavirus, adenovirus, Aichi virus, hepatitis A virus, and hepatitis E virus. The amount of virus genomes per liter sewage of each virus was quantified, and even if there was a high loss of viral particles, with only about 10% of the original amount of viruses detected, all viruses except parechovirus could be identified in the samples. The low level of recovery of virus was determined in one experiment only and needs to be confirmed. The magnitude of viral loss in this study is, however, in accordance with those of other studies on virus detection in wastewater (21, 22, 33). In addition, the concentration seemed to have removed inhibitors of qPCR present in raw sewage, as has been shown also by others (21, 22, 33, 34). Since an infected person excretes 107 to 1013 virus particles per day (19), analysis of incoming sewage may be a useful tool to reveal the presence of and quantify excreted fecal human pathogens and thereby give an estimation of the number of infected persons. Most studies on enteric viruses in sewage only detect the viruses and do not relate the virus sequences identified in sewage to those from patients from the same sampling time and region (27, 35–42). Several of the techniques for virus detection in sewage have also been developed for detection of poliovirus in line with the WHO polio eradication program (36, 43–49).
There was a peak in number of detected viral genomes during week 7 for most of the investigated viruses in this study. This was the week for winter school holidays in this region of Sweden. The assays to detect the different virus types were not performed on the same day or even during the same week, which means that the identified elevated amount of virus particles in the wastewater probably did not reflect a systematic technical error but may indicate that there was an influx of persons from other regions who shed virus during these holidays.
Analysis of wastewater for enterically transmitted viruses has a number of advantages as it makes it possible to monitor a large population by analyzing samples collected in one place, since wastewater from hundreds of thousands of households gathers at the same wastewater treatment plant. Wastewater contains enteric viruses excreted from persons who are ill as well as from cases of subclinical infection, which reflects the real magnitude of circulating virus in the community. In addition, virus can be detected before an outbreak occurs, as shown in this study for norovirus, since the virus may be excreted in feces before onset of symptoms (50), which is 1 to 2 days for norovirus GII and 4 to 5 days for astrovirus, (51), while for hepatitis A and E viruses, the excretion period is longer and occurs for up to 7 weeks (8, 52).
Detection of norovirus in sewage has been extensively studied, since it is known to cause large waterborne and seasonal outbreaks, sometimes with severe consequences for vulnerable persons (3, 26, 53–57). In this study, the amount of norovirus GII in wastewater peaked 2 to 3 weeks before the infection spread in hospital wards and nursing homes, indicating that the outbreak was ongoing at least 2 weeks before most persons severely affected by the norovirus infection came to medical attention.
Genetic comparison of viruses in sewage with virus from clinical sporadic cases and from outbreaks may provide a model for understanding the epidemiology of enteric viral pathogens in the population. This was highlighted by the Scandinavian hepatitis A outbreak, which began in Denmark during autumn 2012 and spread during winter 2012 and spring 2013 throughout Scandinavia, with at least 28 persons infected in 2012 (20). One of the two strains causing this outbreak was detected in sewage in weeks 7 and 9, together with samples from three patients infected with these strains. Two of the patients were diagnosed with acute hepatitis A in weeks 10 and 19 and were both infected with the strain found in the wastewater from week 7. This sewage sample had a large amount of HAV RNA, indicating that there were probably more infected persons than those identified. The third patient, who was infected with the second outbreak strain, had onset of hepatitis in week 3 and was infected by the strain that was found in the wastewater in week 9. None of the reported hepatitis A patients during the study period was infected with the strain that was identified in the wastewater in week 5 and which resembled a strain originating from Iraq. This suggests that there may have been several patients with subclinical cases of hepatitis A who did not seek health care.
There was a constant low concentration of HEV in all but one of the sewage samples, indicating that this virus circulated in the population during the study period. Since HEV is common among Swedish pigs and wild boars (58, 59), the strains in sewage need to be sequenced to identify if they derive from infected humans, animals, or contaminated food products. The seroprevalence of anti-HEV is comparably high in Sweden (60, 61), but there are only 10 to 15 notified cases yearly, indicating that most cases are subclinical. However, hepatitis E may also be underdiagnosed, since the awareness of endemic hepatitis E is still low among treating physicians in Sweden.
The surprisingly large amount of Aichi virus found in this study indicates that Sweden could have as high a prevalence of this virus as has been described for other European countries (62). However, no routine investigation for Aichi virus in patients with diarrhea has been performed in Sweden, and to date only three cases of infection with Aichi virus have been described (63). This virus is known to cause diarrhea in adults as well as in children and has been suggested to play an etiological role in gastroenteritis, especially in outbreaks associated with contaminated seafood (64–67). The finding in this study indicates that patients in Sweden with diarrhea should also be investigated for Aichi virus. Investigation of patient samples and sequencing of the strains identified from both patients and sewage will give a better picture of which strains of Aichi virus are circulating in the area and whether only certain strains will cause disease.
This study illustrates the value of typing strains identified in sewage for the communicable disease officer, since regular monitoring of sewage for these viruses may give an early warning of a possible upcoming outbreak. Typing can also be used as a tool for estimating the burden of infection in a specific community. When these viruses are detected in sewage, it is known that there are several persons infected in the community and that these viruses are circulating in the population. Our results indicated that there were more infected persons excreting viruses than those diagnosed with these infections during the study period. However, the number of infected persons is approximate and provides only an estimate of the extent and weekly variation in the number of people who excrete the viruses in the community. According to an experiment performed in Helsinki, Finland, poliovirus could be detected in sewage if 1 only in 10,000 inhabitants excreted the virus (68). The approach used in this study with molecular-based qPCR may increase the level of detection of the investigated viruses. However, it may also detect genomes from noninfectious virus particles (69, 70). Even if only viral fragments are identified, it will still give a good indication as to which viruses circulate in the population and which viruses infect persons that do not seek medical attention. Further testing of the material needs to be done to establish the sensitivity of the method and to find out if the detected viruses are infectious viruses that can escape treatment of the sewage and spread further. Future studies should also include viruses that are excreted in urine and investigate the presence of additional enterically transmitted viruses in order to get a powerful tool that can be used for both epidemiological purposes and early warning of outbreaks.
ACKNOWLEDGMENT
This study was supported under project PREDEMICS (7th Framework Program, grant agreement no. 278433).
Footnotes
Published ahead of print 29 August 2014
REFERENCES
- 1.Kim SJ, Si J, Lee JE, Ko G. 2012. Temperature and humidity influences on inactivation kinetics of enteric viruses on surfaces. Environ. Sci. Technol. 46:13303–13310. 10.1021/es3032105. [DOI] [PubMed] [Google Scholar]
- 2.Kotwal G, Cannon JL. 2014. Environmental persistence and transfer of enteric viruses. Curr. Opin. Virol. 4:37–43. 10.1016/j.coviro.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Nenonen NP, Hannoun C, Horal P, Hernroth B, Bergström T. 2008. Tracing of norovirus outbreak strains in mussels collected near sewage effluents. Appl. Environ. Microbiol. 74:2544–2549. 10.1128/AEM.02477-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boivin G, Abed Y, Boucher FD. 2005. Human parechovirus-3 and neonatal infections. Emerg. Infect. Dis. 11:103–105. 10.3201/eid1101.040606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mizuta K, Kuroda M, Kurimura M, Yahata Y, Sekizuka T, Aoki Y, Ikeda T, Abiko C, Noda M, Kimura H, Mizutani T, Kato T, Kawanami T, Ahiko T. 2012. Epidemic myalgia in adults associated with human parechovirus type 3 infection, Yamagata, Japan, 2008. Emerg. Infect. Dis. 18:1787–1793. 10.3201/eid1811.111570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stanway G, Joki-Korpela P, Hyypia T. 2000. Human parechoviruses-biology and clinical significance. Rev. Med. Virol. 10:57–69. . [DOI] [PubMed] [Google Scholar]
- 7.Vaughan G, Goncalves Rossi LM, Forbi JC, de Paula VS, Purdy MA, Xia G, Khudyakov YE. 2014. Hepatitis A virus: host interactions, molecular epidemiology and evolution. Infect. Genet. Evol. 21:227–243. 10.1016/j.meegid.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 8.Aggarwal R. 2013. Diagnosis of hepatitis E. Nat. Rev. Gastroenterol. Hepatol. 10:24–33. 10.1038/nrgastro.2012.187. [DOI] [PubMed] [Google Scholar]
- 9.Lin J, Norder H, Uhlhorn H, Belák S, Widén F. 2014. Novel hepatitis E like virus found in Swedish moose. J. Gen. Virol. 95:557–570. 10.1099/vir.0.059238-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Benedictis P, Schultz-Cherry S, Burnham A, Cattoli G. 2011. Astrovirus infections in humans and animals—molecular biology, genetic diversity, and interspecies transmissions. Infect. Genet. Evol. 11:1529–1544. 10.1016/j.meegid.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ball LA. 2005. The universal taxonomy of viruses in theory and practice, p 3–8 In Fauquet CM, Mayo MA, Maniloff J, Desselberger U, Ball LA. (ed), Virus taxonomy: Eighth Report of the International Committee on Taxonomy of Viruses. Elsevier Academic Press, Amsterdam, Holland. [Google Scholar]
- 12.Lanata CF, Fischer-Walker CL, Olascoaga AC, Torres CX, Aryee MJ, Black RE. 2013. Child Health Epidemiology Reference Group of the World Health Organization and UNICEF. Global causes of diarrheal disease mortality in children <5 years of age: a systematic review. PLoS One 8:e72788. 10.1371/journal.pone.0072788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parashar UD, Nelson EA, Kang G. 2013. Diagnosis, management, and prevention of rotavirus gastroenteritis in children. BMJ 347:f7204. 10.1136/bmj.f7204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson CM, Seto D, Jones MS, Dyer DW, Chodosh J. 2011. Molecular evolution of human species D adenoviruses. Infect. Genet. Evol. 11:1208–1217. 10.1016/j.meegid.2011.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robinson CM, Singh G, Lee JY, Dehghan S, Rajaiya J, Liu EB, Yousuf MA, Betensky RA, Jones MS, Dyer DW, Seto D, Chodosh J. 2013. Molecular evolution of human adenoviruses. Sci. Rep. 3:1812. 10.1038/srep01812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsushima Y, Shimizu H, Kano A, Nakajima E, Ishimaru Y, Dey SK, Watanabe Y, Adachi F, Mitani K, Fujimoto T, Phan TG, Ushijima H. 2013. Genome sequence of a novel virus of the species human adenovirus D associated with acute gastroenteritis. Genome Announc. 1:e00068-12. 10.1128/genomeA.00068-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Timm DA, Thomas W, Boileau TW, Williamson-Hughes PS, Slavin JL. 2013. Polydextrose and soluble corn fiber increase five-day fecal wet weight in healthy men and women. J. Nutr. 143:473–478. 10.3945/jn.112.170118. [DOI] [PubMed] [Google Scholar]
- 18.Fechner A, Fenske K, Jahreis G. 2013. Effects of legume kernel fibres and citrus fibre on putative risk factors for colorectal cancer: a randomised, double-blind, crossover human intervention trial. Nutr. J. 12:101. 10.1186/1475-2891-12-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bosch A. 1998. Human enteric viruses in the water environment: a minireview. Int. Microbiol. 1:191–196. [PubMed] [Google Scholar]
- 20.Gillesberg Lassen S, Soborg B, Midgley SE, Steens A, Vold L, Stene-Johansen K, Rimhanen-Finne R, Kontio M, Löfdahl M, Sundqvist L, Edelstein M, Jensen T, Vestergaard HT, Fischer TK, Molbak K, Ethelberg S. 2013. Ongoing multi-strain food-borne hepatitis A outbreak with frozen berries as suspected vehicle: four Nordic countries affected, October 2012 to April 2013. Euro Surveill. 18:20467. 10.1017/S0950268813001398. [DOI] [PubMed] [Google Scholar]
- 21.Calgua B, Rodriguez-Manzano J, Hundesa A, Suñen E, Calvo M, Bofill-Mas S, Girones R. 2013. New methods for the concentration of viruses from urban sewage using quantitative PCR. J. Virol. Methods 187:215–221. 10.1016/j.jviromet.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 22.Prado T, Guilayn Wde C, Gaspar AM, Miagostovich MP. 2013. The efficiency of concentration methods used to detect enteric viruses in anaerobically digested sludge. Mem. Inst. Oswaldo Cruz 108:77–83. 10.1590/S0074-02762013000100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koo ES, Yoo CH, Na Y, Park SY, Lyoo HR, Jeong YS. 2012. Reliability of non-culturable virus monitoring by PCR-based detection methods in environmental waters containing various concentrations of target RNA. J. Microbiol. 50:726–734. 10.1007/s12275-012-2279-y. [DOI] [PubMed] [Google Scholar]
- 24.Rodríguez RA, Polston PM, Wu MJ, Wu J, Sobsey MD. 2013. An improved infectivity assay combining cell culture with real-time PCR for rapid quantification of human adenoviruses 41 and semi-quantification of human adenovirus in sewage. Water Res. 47:3183–3191. 10.1016/j.watres.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 25.Levitt A, Diop OM, Tangermann RH, Paladin F, Kamgang JB, Burns CC, Chenoweth PJ, Goel A, Wassilak SG. 2014. Office of Infectious Diseases, CDC. Surveillance systems to track progress toward global polio eradication—worldwide, 2012–2013. MMWR Morb. Mortal. Wkly. Rep. 63:356–361. [PMC free article] [PubMed] [Google Scholar]
- 26.Nenonen NP, Hannoun C, Larsson CU, Bergström T. 2012. Marked genomic diversity of norovirus genogroup I strains in a waterborne outbreak. Appl. Environ. Microbiol. 78:1846–1852. 10.1128/AEM.07350-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rusiñol M, Fernandez-Cassi X, Hundesa A, Vieira C, Kern A, Eriksson I, Ziros P, Kay D, Miagostovich M, Vargha M, Allard A, Vantarakis A, Wyn-Jones P, Bofill-Mas S, Girones R. 2014. Application of human and animal viral microbial source tracking tools in fresh and marine waters from five different geographical areas. Water Res. 59:119–129. 10.1016/j.watres.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 28.Rezaeinejad S, Vergara GG, Woo CH, Lim TT, Sobsey MD, Gin KY. 2014. Surveillance of enteric viruses and coliphages in a tropical urban catchment. Water Res. 58:122–131. 10.1016/j.watres.2014.03.051. [DOI] [PubMed] [Google Scholar]
- 29.Calgua B, Mengewein A, Grunert A, Bofill-Mas S, Clemente-Casares P, Hundesa A, Wyn-Jones AP, López-Pila JM, Girones R. 2008. Development and application of a one-step low cost procedure to concentrate viruses from seawater samples. J. Virol. Methods 153:79–83. 10.1016/j.jviromet.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Larkin MA, Blackshields G, Brown NP, Chenna R, McGettigan PA, McWilliam H, Valentin F, Wallace IM, Wilm A, Lopez R, Thompson JD, Gibson TJ, Higgins DG. 2007. Clustal W and Clustal X version 2.0. Bioinformatics 23:2947–2948. 10.1093/bioinformatics/btm404. [DOI] [PubMed] [Google Scholar]
- 31.Felsenstein J. 1993. PHYLIP: Phylogeny Inference Package, version 3.52c. University of Washington, Seattle, WA. [Google Scholar]
- 32.Page RDM. 1996. TREEVIEW: an application to display phylogenetic trees on personal computers. Comp. Appl. Biosci. 12:357–358. [DOI] [PubMed] [Google Scholar]
- 33.Prado T, Gaspar AM, Miagostovich MP. 2014. Detection of enteric viruses in activated sludge by feasible concentration methods. Braz. J. Microbiol. 45:343–349. 10.1590/S1517-83822014000100049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang S, Dezfulian H, Chu W. 2005. Real-time quantitative PCR for enteric adenovirus serotype 40 in environmental waters. Can. J. Microbiol. 51:393–398. 10.1139/w05-016. [DOI] [PubMed] [Google Scholar]
- 35.Wong MV, Hashsham SA, Gulari E, Rouillard JM, Aw TG, Rose JB. 2013. Detection and characterization of human pathogenic viruses circulating in community wastewater using multi target microarrays and polymerase chain reaction. J. Water Health 11:659–670. 10.2166/wh.2013.322. [DOI] [PubMed] [Google Scholar]
- 36.Battistone A, Buttinelli G, Bonomo P, Fiore S, Amato C, Mercurio P, Cicala A, Simeoni J, Foppa A, Triassi M, Pennino F, Fiore L. 2013. Detection of enteroviruses in influent and effluent flow samples from wastewater treatment plants in Italy. Food Environ. Virol. 6:13–22. 10.1007/s12560-013-9132-2. [DOI] [PubMed] [Google Scholar]
- 37.Miura T, Parnaudeau S, Grodzki M, Okabe S, Atmar RL, Le Guyader FS. 2013. Environmental detection of genogroup I, II, and IV noroviruses by using a generic real-time reverse transcription-PCR assay. Appl. Environ. Microbiol. 79:6585–6592. 10.1128/AEM.02112-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hartmann NM, Dartscht M, Szewzyk R, Selinka HC. 2013. Monitoring of adenovirus serotypes in environmental samples by combined PCR and melting point analyses. Virol. J. 10:190. 10.1186/1743-422X-10-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Di Martino B, Di Profio F, Ceci C, Di Felice E, Marsilio F. 2013. Molecular detection of Aichi virus in raw sewage in Italy. Arch. Virol. 158:2001–2005. 10.1007/s00705-013-1694-7. [DOI] [PubMed] [Google Scholar]
- 40.Vecchia AD, Fleck JD, Kluge M, Comerlato J, Bergamaschi B, Luz RB, Arantes TS, Silva JV, Thewes MR, Spilki FR. 2012. Assessment of enteric viruses in a sewage treatment plant located in Porto Alegre, southern Brazil. Braz. J. Biol. 72:839–846. 10.1590/S1519-69842012000500009. [DOI] [PubMed] [Google Scholar]
- 41.Staley C, Gordon KV, Schoen ME, Harwood VJ. 2012. Performance of two quantitative PCR methods for microbial source tracking of human sewage and implications for microbial risk assessment in recreational waters. Appl. Environ. Microbiol. 78:7317–7326. 10.1128/AEM.01430-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bofill-Mas S, Albinana-Gimenez N, Clemente-Casares P, Hundesa A, Rodriguez-Manzano J, Allard A, Calvo M, Girones R. 2006. Quantification and stability of human adenoviruses and polyomavirus JCPyV in wastewater matrices. Appl. Environ. Microbiol. 72:7894–7896. 10.1128/AEM.00965-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tulchinsky TH, Ramlawi A, Abdeen Z, Grotto I, Flahault A. 2013. Polio lessons 2013: Israel, the West Bank, and Gaza. Lancet 382:1611–1612. 10.1016/S0140-6736(13)62331-4. [DOI] [PubMed] [Google Scholar]
- 44.Kuryk L, Wieczorek M, Diedrich S, Böttcher S, Witek A, Litwińska B. 2014. Genetic analysis of poliovirus strains isolated from sewage in Poland. J. Med. Virol. 86:1243–1248. 10.1002/jmv.23803. [DOI] [PubMed] [Google Scholar]
- 45.Al-Hello H, Jorba J, Blomqvist S, Raud R, Kew O, Roivainen M. 2013. Highly divergent type 2 and 3 vaccine-derived polioviruses isolated from sewage in Tallinn, Estonia. J. Virol. 87:13076–13080. 10.1128/JVI.01174-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pellegrinelli L, Binda S, Chiaramonte I, Primache V, Fiore L, Battistone A, Fiore S, Gambino M, Bubba L, Barbi M. 2013. Detection and distribution of culturable human enteroviruses through environmental surveillance in Milan, Italy. J. Appl. Microbiol. 115:1231–1239. 10.1111/jam.12321. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. 2013. Evaluating surveillance indicators supporting the Global Polio Eradication Initiative, 2011–2012. MMWR Morb. Mortal. Wkly. Rep. 62:270–274. [PMC free article] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. 2012. Tracking progress toward global polio eradication, 2010–2011. MMWR Morb. Mortal. Wkly. Rep. 61:265–269. [PubMed] [Google Scholar]
- 49.Blomqvist S, El Bassioni L, El Maamoon Nasr EM, Paananen A, Kaijalainen S, Asghar H, de Gourville E, Roivainen M. 2012. Detection of imported wild polioviruses and of vaccine-derived polioviruses by environmental surveillance in Egypt. Appl. Environ. Microbiol. 78:5406–5409. 10.1128/AEM.00491-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carter MJ. 2005. Enterically infecting viruses: pathogenicity, transmission and significance for food and waterborne infection. J. Appl. Microbiol. 98:1354–1380. 10.1111/j.1365-2672.2005.02635.x. [DOI] [PubMed] [Google Scholar]
- 51.Lee RM, Lessler J, Lee RA, Rudolph KE, Reich NG, Perl TM, Cummings DA. 2013. Incubation periods of viral gastroenteritis: a systematic review. BMC Infect. Dis. 13:446. 10.1186/1471-2334-13-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Richardson M, Elliman D, Maguire H, Simpson J, Nicoll A. 2001. Evidence base of incubation periods, periods of infectiousness and exclusion policies for the control of communicable diseases in schools and preschools. Pediatr. Infect. Dis. J. 20:380–391. 10.1097/00006454-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 53.Cho HG, Lee SG, Kim WH, Lee JS, Park PH, Cheon DS, Jheong WH, Jho EH, Lee JB, Paik SY. 2014. Acute gastroenteritis outbreaks associated with ground-waterborne norovirus in South Korea during 2008–2012. Epidemiol. Infect. 10.1017/S0950268814000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harris JP, Adak GK, O'Brien SJ. 2014. To close or not to close? Analysis of 4 year's data from national surveillance of norovirus outbreaks in hospitals in England. BMJ Open 4:e003919. 10.1136/bmjopen-2013-003919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Harris JP, Adams NL, Lopman BA, Allen DJ, Adak GK. 2014. The development of web-based surveillance provides new insights into the burden of norovirus outbreaks in hospitals in England. Epidemiol. Infect. 142:1590–1598. 10.1017/S0950268813002896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jack S, Bell D, Hewitt J. 2013. Norovirus contamination of a drinking water supply at a hotel resort. N. Z. Med. J. 126:98–107. [PubMed] [Google Scholar]
- 57.Fiehn C, Miehle N. 2014. How dangerous are norovirus infections in patients with rheumatic diseases treated with biologics and DMARDs? Follow-up on a local outbreak and comparison with a control cohort. Ann. Rheum. Dis. 73:786–787. 10.1136/annrheumdis-2013-204437. [DOI] [PubMed] [Google Scholar]
- 58.Norder H, Sundqvist L, Magnusson L, Ostergaard Breum S, Löfdahl M, Larsen LE, Hjulsager CK, Magnius L, Böttiger BE, Widén F. 2009. Endemic hepatitis E in two Nordic countries. Euro Surveill. 14:19211. [DOI] [PubMed] [Google Scholar]
- 59.Widen F, Sundqvist L, Matyi-Toth A, Meterveli G, Belák S, Hallgren G, Norder H. 2011. Molecular epidemiology of hepatitis E virus in humans, pigs and wild boars in Sweden. Epidemiol. Infect. 139:361–371. 10.1017/S0950268810001342. [DOI] [PubMed] [Google Scholar]
- 60.Sylvan SP, Jacobson SH, Christenson B. 1998. Prevalence of antibodies to hepatitis E virus among hemodialysis patients in Sweden. J. Med. Virol. 54:38–43. . [DOI] [PubMed] [Google Scholar]
- 61.Olsen B, Axelsson-Olsson D, Thelin A, Weiland O. 2006. Unexpected high prevalence of IgG-antibodies to hepatitis E virus in Swedish pig farmers and controls. Scand. J. Infect. Dis. 38:55–58. 10.1080/00365540500321470. [DOI] [PubMed] [Google Scholar]
- 62.Reuter G, Boros Á, Pankovics P. 2011. Kobuviruses—a comprehensive review. Rev. Med. Virol. 21:32–41. 10.1002/rmv.677. [DOI] [PubMed] [Google Scholar]
- 63.Jonsson N, Wahlström K, Svensson L, Serrander L, Lindberg MA. 2012. Aichi virus infection in elderly people in Sweden. Arch. Virol. 157:1365–1369. 10.1007/s00705-012-1296-9. [DOI] [PubMed] [Google Scholar]
- 64.Ambert-Bakay K, Lorrot M, Bon F, Giraudon H, Kaplon J, Wolfer M, Lebon P, Gendrel D, Pothier P. 2008. Prevalence and genetic diversity of Aichi virus strains in stool samples from community and hospitalized patients. J. Clin. Microbiol. 46:1252–1258. 10.1128/JCM.02140-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nielsen AC, Gyhrs ML, Nielsen LP, Pedersen C, Bottiger B. 2013. Gastroenteritis and the novel picornaviruses aichivirus, coasavirus, saffoldvirus, and salivirus in young children. J. Clin. Virol. 57:239–242. 10.1016/j.jcv.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 66.Oh DY, Silva PA, Hauroeder B, Diedrich S, Cardoso DDP, Schreier E. 2006. Molecular characterization of the first Aichi viruses isolated in Europe and in South America. Arch. Virol. 151:1199–1206. 10.1007/s00705-005-0706-7. [DOI] [PubMed] [Google Scholar]
- 67.Yamashita T, Kobayashi S, Sakae K, Nakata S, Chiba S, Ishihara Y, Isomura S. 1991. Isolation of cytopathic small round viruses with BS-C-1 cells from patients with gastroenteritis. J. Infect. Dis. 164:954–957. 10.1093/infdis/164.5.954. [DOI] [PubMed] [Google Scholar]
- 68.Hovi T, Stenvik M, Partanen H, Kangas A. 2001. Poliovirus surveillance by examining sewage specimens. Quantitative recovery of virus after introduction into sewerage at remote upstream location. Epidemiol. Infect. 127:101–106. 10.1017/S0950268801005787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stinski MF, Mocarski ES, Thomsen DR. 1979. DNA of human cytomegalovirus: size heterogeneity and defectiveness resulting from serial undiluted passage. J. Virol. 31:231–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Choi S, Jiang SC. 2005. Real-time PCR quantification of human adenoviruses in urban rivers indicates genome prevalence but low infectivity. Appl. Environ. Microbiol. 71:7426–7433. 10.1128/AEM.71.11.7426-7433.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fuentes C, Guix S, Pérez-Rodriguez FJ, Fuster N, Carol M, Pintó RM, Bosch A. 2014. Standardized multiplex one-step qRT-PCR for hepatitis A virus, norovirus GI and GII quantification in bivalve mollusks and water. Food Microbiol. 40:55–63. 10.1016/j.fm.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 72.Reference deleted.
- 73.Kageyama T, Kojima S, Shinohara M, Uchida K, Fukushi S, Hoshino FB, Takeda N, Katayama K. 2003. Broadly reactive and highly sensitive assay for Norwalk-like viruses based on real-time quantitative reverse transcription-PCR. J. Clin. Microbiol. 41:1548–1557. 10.1128/JCM.41.4.1548-1557.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kabayiza JC, Andersson ME, Welinder-Olsson C, Bergström T, Muhirwa G, Lindh M. 2013. Comparison of rectal swabs and faeces for real-time PCR detection of enteric agents in Rwandan children with gastroenteritis. BMC Infect. Dis. 13:447. 10.1186/1471-2334-13-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.van Maarseveen NM, Wessels E, de Brouwer CS, Vossen AC, Claas EC. 2010. Diagnosis of viral gastroenteritis by simultaneous detection of adenovirus group F, astrovirus, rotavirus group A, norovirus genogroups I and II, and sapovirus in two internally controlled multiplex real-time PCR assays. J. Clin. Virol. 49:205–210. 10.1016/j.jcv.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 76.Pang X, Lee B, Chui L, Preiksaitis JK, Monroe SS. 2004. Evaluation and validation of real-time reverse transcription-PCR assay using the LightCycler system for detection and quantitation of norovirus. J. Clin. Microbiol. 42:4679–4685. 10.1128/JCM.42.10.4679-4685.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tallo T, Norder H, Tefanova V, Ott K, Ustina V, Prukk T, Solomonova O, Schmidt J, Zilmer K, Priimägi L, Krispin T, Magnius LO. 2003. Sequential changes in hepatitis A virus genotype distribution in Estonia during 1994 to 2001. J. Med. Virol. 70:187–193. 10.1002/jmv.10377. [DOI] [PubMed] [Google Scholar]