Introduction
From the experience of high-income countries, the occurrence of all obstetric complications may not be preventable but almost all are treatable before resulting in serious maternal and perinatal morbidity and mortality (1, 2). The interventions may start at preconception; however, providing optimal obstetric care for all pregnant women starting from early pregnancy up to the end of puerperium has paramount significance in the reduction of maternal and perinatal deaths. Specific to low and middle-income countries, improving the intrapartum monitoring and access to a cesarean section and blood transfusion were highly recommended as key interventions to reduce maternal and perinatal deaths (3, 4).
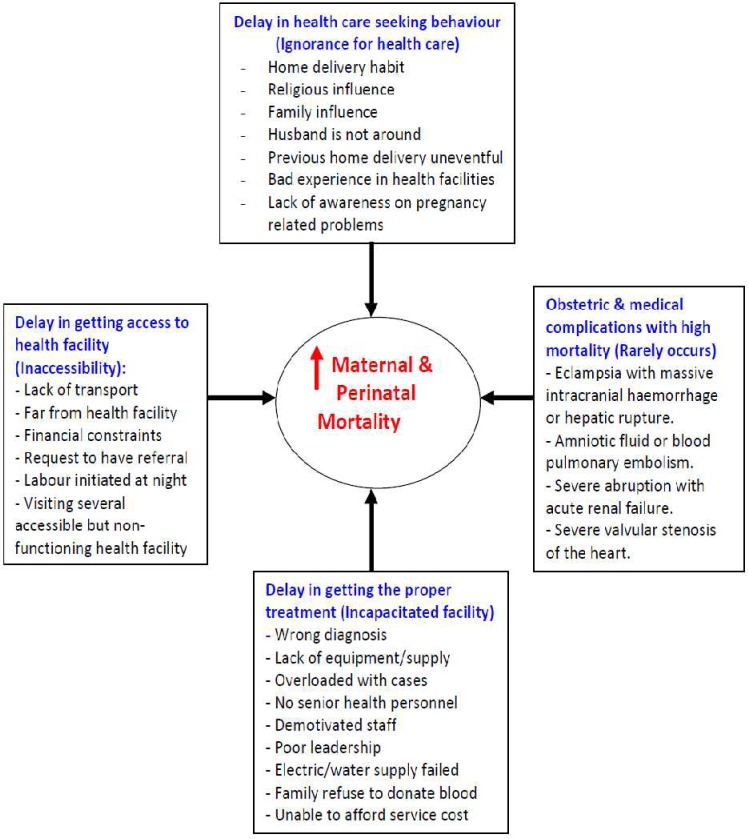
According to the Federal Ministry of Health of Ethiopia 2011/2012 Health and Health Related Indicators report, however, the proportion of at least four visits antenatal care was 19%; total births attended by skilled health personnel were 16.6%; and the proportion of cesarean delivery was about 1% (5), while the WHO cesarean delivery recommendation is 5%–15% for the general population (6). These reports indicate the big gap in utilizing reproductive health services before and after conception. In addressing issues regarding maternal and perinatal death rates, the “three delay” model is frequently used to consider factors that may be obstacles for women receiving appropriate medical care. The three delay model was initially proposed by Thaddeus and Maine in 1990 (7). The components of this model include the delays of the decision to seek health care (8), the ability to get access to a health facility (9) and receiving medical care timely and appropriately once the facility is reached (10). It is generally recognized that diminished access to facilities providing emergency obstetric care contributes to increased maternal and perinatal mortality (11, 12). The purpose of this review was to look into the high maternal and perinatal mortality from the perspective of the three delays models and to show the complexity and interlink of predisposing factors for maternal and perinatal deaths. As discussed in other articles (13, 14), the factors for high maternal and perinatal mortality in the last three decades were multidimensional (the extremely low number of health facilities and health professionals, low adult literacy rate, low utilization of contraceptive methods, high total fertility rate, high early marriage and adolescent pregnancy, low antenatal care service, low skilled person attended deliveries, and rampant harmful traditional practices).
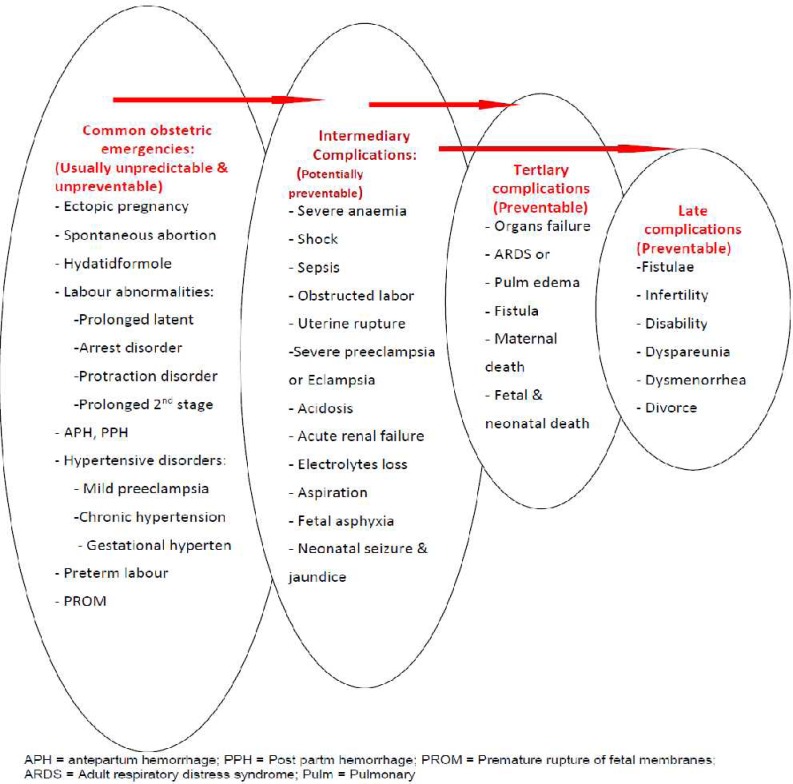
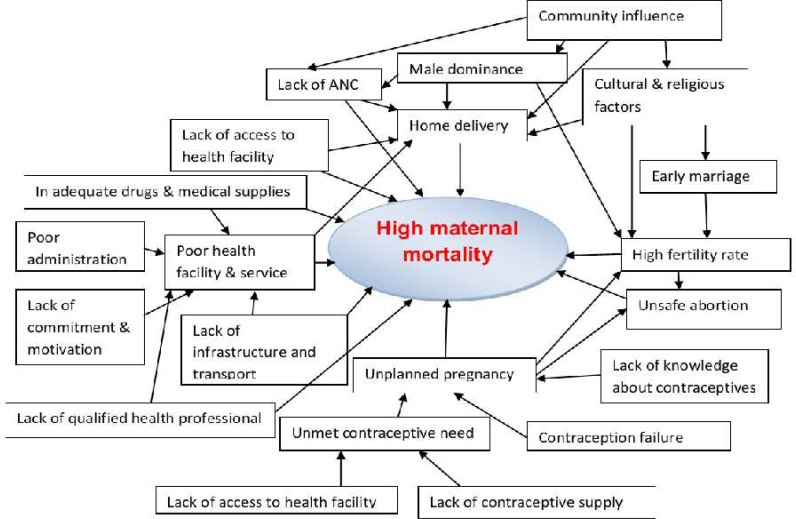
The main focus of this review is the “Delay Model”. To summarize these complex and interlinked factors for the increased risk of maternal and perinatal deaths in Ethiopia, a simplified schematic presentation from the perspective of the “three delays” model (Figure 1). As a complimentary, two more schematic presentations were developed from the perspective of “etiologic” factors (Figure 2), and to show the multidimensional nature of maternal mortality (Figure 3).
Figure 1.
Contextual factors that contribute to high maternal and perinatal mortality in Ethiopia, using the “Delay model”
Figure 2.
Potential contributors to high maternal and perinatal mortality and morbidity in Ethiopia: Perspective on “etiology” and complications
Figure 3.
Contributing factors to high maternal mortality in Ethiopia, the “multifactorial” nature
Delay I: Delay in the decision to seek health care
The first delay, failure to seek treatment by the pregnant women or her partner/family/relatives, is largely affected by local health beliefs (cultural, religious, bad experience in health facilities, good outcome in previous pregnancies without health care, gender inequality, unaffordable medical service cost and low education) (2, 7, 15). All these are significant limitations particularly among people with limited education and limited exposure to a modern medical care system.
In Ethiopia, where the cultural barriers, religious influence, male dominance in household decision making and bad experiences in available health facilities are quite common-pregnant women usually come to health facilities with obstetric complications. This is well observed in preliminary results from an ongoing cohort study in Hawassa University Hospital, where the author is working. Other studies have also shown a big delay in the health care seeking among Ethiopian pregnant women (16–18). Although the magnitude is variable, this is not a problem specific to Ethiopia or even to Sub Saharan Africa. Studies in the United States and in Thailand, among many others, have also identified “delay I” as a major obstacle to care (19, 20).
As a result of the big delay at home, pregnant women encountered the common life threatening obstetric complications: hemorrhagic, shock, severe anemia, sepsis, generalized peritonitis, obstructed labor, uterine rupture, eclampsia, aspiration pneumonia, coma, severe fetal asphyxia or fetal death. Once a woman develops any of these clinical conditions, the chance of deteriorating to tertiary level complications (multiple organs failure and death) is very high partly because of the 2nd and 3rd delay. Previous author also pointed out that many pregnant women with life threatening obstetric complications could not be saved; women who survive death from obstetric complications, either by chance or treatment as “near miss”, are very likely to share similar experiences with those who died (7).
One of the reasons why such complications occur is that pregnant women and their caretakers at home may not recognize that there is a serious pregnancy related problem until late in its course. They are fearful of hospitals because they may be aware of friends or relatives who died there. Pregnant women and their relatives may not trust the health professional care and may be justifiably afraid that needed medicines and equipment will not be available at the health facility (21). One of the major reasons for delay at home is waiting for the response to traditional therapy. In other words, it is a commonly observed phenomenon to attempt a traditional therapy in the community (traditional medicine, massaging the abdomen, holy water, pray), albeit unsuccessful, before bringing the sick pregnant women to a health facility. Due to lack of empowerment, Ethiopian women may not be the decision-makers determining whether they should seek medical care, which is not only the case in Ethiopia (22).
Equally important, the mother or mother-to-be and her family have witnessed many pregnancies and deliveries ending up in a traditional way with no maternal and fetal/neonatal complications. Even when there are maternal or fetal casualties in the community, the majority of our people associate pregnancy-related complications with God's punishment for sins couples committed (23). However, if the death occurred in a hospital, there is a tendency to exaggerate it and attribute it solely to health professionals' failure. This unfortunate ending may be taken as an excuse for not coming again and it can be a moral boost for the local healers.
There is a strong cultural network that ties up most of the society pertaining pregnancy and delivery. Having about 50% urban institutional delivery (24) is not only because of lack of delivery setup across all urban areas in the country, it is probably because of binding cultural factors which usually encourage mothers to give birth at home accompanied by their parents and relatives.
In the authors' opinion, in this regard, the major barriers to poor utilization of available modern health service are the majority of our population being illiterate for modern education, low economic status, women's dependence on husbands and cultural influence (24). As a result, since the majority of pregnant women were not demanding medical care during pregnancy, during delivery and after birth, the survival of the women after afterwards was a little bit far from the natural course. This is because, among others, nationally only about 19% of the pregnant women attended antenatal care; 10% of the deliveries were attended by skilled person and only 7% of women attended postnatal care (24).
In general, in the Ethiopian context, the contribution of “delay I” to the high maternal and perinatal mortality may be more than that of “delay II and III”. Therefore, to bring a significant change in the maternal and perinatal mortality, much has to be done in: 1) increasing the public awareness on dangers of pregnancy related complications, 2) improving education for females and 3) empowering women to make decision on their own health.
Delay II: Delay in getting access to a health facility
Once decision is made at home to seek medical care in one of the accessible health facilities, several other barriers may impede access to health facilities: lack of transport, inaccessibility of transport, long distance from functioning health facility, nonfunctioning health facilities in between home and the functioning health facility. It is known that the time between onset of an obstetric emergency and definitive care is critical for the survival of the mother and her baby. All of the top 4 causes of maternal mortality in Ethiopia in the last decade (obstructed labor with or without uterine rupture, hemorrhage, hypertensive disorders and sepsis) need urgent treatment.
Guidelines have been developed to estimate the amount of time between the onset of an obstetric emergency and maternal death. For postpartum hemorrhage, there are only two hours in which to intervene to prevent maternal death. Death from a ruptured uterus may take one day, and from eclampsia two days (25). In prolonged or obstructed labor, the fetus may die of asphyxia within 24 hours; and in 24–48 hours, the mother's pelvic organs sloughed off and create fistula; she will develop metabolic acidosis, acute renal failure (post and pre-renal), paralytic ileus and physical disability due to peroneal nerves compression (26,27). These limited time intervals make the problem of obtaining accessible transportation of more significance than in other medical emergencies.
Thereafter, the delay to reach a health facility where they can get the definitive treatment depends on the distance they travel and the number of health facilities they visited on the way. In several circumstances, the physically accessible health facilities may become “physical obstacles” for pregnant women in accessing a functioning health facility in time.
Pregnant women with complication (usually from the rural area and probably in the interest of the family) have the tendency to visit rather than bypass the easily accessible health center, district hospital and occasionally private clinics before coming to a hospital that can give them appropriate therapy. Some of the pregnant women with complications may visit three to five or more health facilities before arriving at a health facility where they can be managed somehow optimally.
Among the survivors of obstructed labor and uterine rupture, maternal morbidity as well may be significantly increased due to delayed care: among others, fistulae, infertility, physical disability, psychological trauma, secondary dysmenorrhea and dyspareunia are the commonly encountered problems, and all these may result in marriage divorce (28, 29). Ethiopian women who received treatment for fistulae had traveled an average of 11 hours to reach emergency obstetric services. One of the founders of the fistula hospitals in Ethiopia described the high incidence of fistulae in Ethiopia as due to ‘obstructed labor and obstructed transport’(30).
Studies have demonstrated that causes of maternal mortality as well as health status on arrival at a hospital differ between local women compared to those who have had to travel long distances. The most common causes of death for local women (women with easy access to health facilities) were eclampsia and hemorrhage while for distant travelers were ruptured uterus and abortion complications. It is possible to deduce that women who hemorrhaged or became eclamptic and had no easy access to functioning health facilities died en route. Importantly, according to one report, most of the women coming from outside the city were in shock while none of the women from the immediate area of the hospital were in shock upon arrival at the hospital (31).
The implication is that women coming from rural areas with obstetric complications may represent the tip of the iceberg as far as the magnitude of obstetric problem is concerned. It is assumed that the majority are dying at home probably because of: 1) the delay to get health service and fast-killing nature of obstetric complications (uterine rupture, antepartum hemorrhage, postpartum hemorrhage, eclampsia and sepsis), 2) lack of transport or lack of money for transport, 3) false reassurance given by local healers or traditional birth attendants or some other influential people in the community (religious leaders, community leaders and elderly people).
A frequent problem cited for delays in reaching appropriate medical facilities in obstetric emergencies is distance. According to the 2011 Ethiopian Demographic and Health Survey study participants, the major barriers for pregnant women to access health services were lack of transport to a facility (71%), lack of money (68%) and distance to a health facility (66%) (24). The most important reason why delay in getting access to health facilities had been a challenge in Ethiopia was because of the very limited number of health facilities and medical personnel availability in the rural areas; the few hospitals nationally available were constructed around the big towns while more than 85% of the population was living in the rural area.
Data from the Federal Ministry of Health revealed that coverage of basic health services and infrastructures in Ethiopia have been low and unevenly distributed. Health care coverage is measured by access, i.e. a health facility within a 10 kilometer radius. In 1997/8, it was estimated that only about 45% of the population had access to any type of health facility, with regional variations between 11% and 86%. By the end of 2005, the potential health service coverage had reached to about three-fourths of the population (32). Even this improvement does not address the issue of facilities being adequately equipped and staffed to handle emergency obstetric care.
It is estimated that 40–60% of people living in developing countries live at a distance of > 8 km from a health care facility (33). A study on women coming to the Jimma University Hospital found out that 19% of the women traveled between 100–400 kms to reach a hospital (34). The significance of distance has been studied for a variety of medical conditions. One study demonstrated that a 10% increase in distance from a hospital increased maternal and neonatal death by 2% (35).
While the findings are not consistent, studies in Nigeria, Southern Tanzania and Uganda all demonstrate that distance from medical care increases the risk of perinatal deaths in children (36). In a report on the implementation of the 18 Prevention of Mother to Child (HIV) Transmission (PMTCT) services in South Africa, lack of affordable transport and long distances between pregnant women's homes and health outlets were a major obstacle to treatment (37). Within Ethiopia, distance from a health facility (defined as greater or less than one hour walk) significantly affected the use of antenatal care. One would expect it to have much greater impact on the laboring or the bleeding woman (38).
Distance alone is only one factor in accessing prompt obstetric care. Other factors which contribute to inadequate transportation include few motorized vehicles, poor roads and high costs. All of these function as deterrents to women obtaining appropriate health care at medical facilities (39).
While motorized transportation is thought to be the most effective and efficient mode (40), individual ownership of cars is unusual in rural areas where public transportation is also limited. More frequently, carts drawn by donkeys or horses are what are available to transport laboring or postpartum women and their babies. Roads may be poorly developed or in need of repair and climactic conditions may affect their passability (41). In Nepal, road construction led to an overall increase in the use of regional facilities, although results varied among different communities (42).
Cost of transportation is another critical factor which delays access to effective obstetric care. Once a decision is made by the patient and her family that a medical service is needed, they must first raise money, often borrowing from friends and family in order to hire a vehicle. Since the transportation is required immediately, transporters may charge excessive amounts. The authors encountered several women with obstetric problems who paid more than 200 USD for less than 100 km travel, which was extremely high and unacceptable by any standard in the country. Both of these decrease the likelihood someone will go to a medical facility in an emergency condition and increase the likelihood that going for treatment will impoverish the family whether or not the mother and baby survive (43).
Cost in obtaining transportation is a known deterrent to receiving appropriate care (44). Transport costs may approach 25% of the total health care cost, and in some circumstances, far exceeds the direct costs (45). A study in Nepal found that over half of the families of women who delivered in hospitals had to borrow money (46). Asking for and collecting the money in itself contributes to the delay in definitive treatment.
There are many low resource countries in which initiatives to provide low cost transportation have been successful in reducing maternal deaths (12). In Mali, the introduction of a maternal referral system which included transportation reduced maternal deaths with the greatest decrease in deaths due to hemorrhage (where time to care is the most critical) (47). In New Guinea, improving transfer management resulted in a decreased incidence of uterine rupture from 20% to 12% (48). In Sierra Leone, development of an ambulance service for obstetric emergencies increased the need for the service (49). The importance of transportation cannot be overemphasized. According to World Bank Strategy, “an estimated 75% of maternal deaths could be prevented through timely access to childbirthrelated care, facilitated by transport” (50).
Ransom and Yinger (51) are not alone in proposing that ‘making motherhood safe” includes the four components of teaching women to recognize critical complications, reducing reasons for seeking transport (such as fear of costs), creating efficient emergency systems for referrals and transfer of patients and, lastly, improving the quality and comprehensiveness of care at medical facilities.
In general, the authors assume that the limited number of functioning health facilities and senior health professionals were inaccessible for the majority of the population to get an emergency obstetric care. As a result, the delay in getting access to health facilities had probably played its role for the high maternal and perinatal mortality in Ethiopia. In this regard, identifying obstacles limiting the use of efficient transportation may be more quickly addressed and be more responsive to treat the time-sensitive and life-threatening causes of maternal and neonatal deaths in the years to come.
Delay III: Delay in receiving medical care
On top of community based barriers and lack of access to health facilities, failure to detect obstetric problems timely and take action (including delay in referral and delay in consultation) are also among the major problems in the health care system (52). Some women who have access to health facilities may not get the service in time either because of a poor management of the available resources or due to incapacitated health manpower or due to lack of basic medical equipment and supplies.
Of these factors, shortage of well-trained health manpower takes the lion's share for the delay in providing the medical care for those who have access to a health facility. In the majority of the hospitals outside each regional state's capital, there may not be a single specialist of any clinical field; probably more than 95% of the public hospitals outside the regional states capital are run by junior general practitioners, health officers and nurses (13).
However, it is well noted that obstetric emergencies which cause maternal death, obstetric fistula, severe infections (including septic abortions), stillbirths and early neonatal deaths require early intervention, which many women in low resource settings are unable to get (7). The recent focus of many publications is on creating a system of care that involves timely screening of women (often in labor) for high risk conditions with timely intervention including rapid transport of the mother to a facility that can provide the comprehensive obstetric care and newborn care (CEmONC) (53).
However, the health facilities with CEmONC service may not be free from limitations and poor quality of service. The major reason for the poor quality of service is usually the delay in providing treatment. Since health service is a team work involving staff with different background (administrative and support, clinical, laboratory, imaging and pharmacy staff), the delay in giving treatment as early as possible may be multifactorial, which again may be due to one or more of the following reasons:
1. Unavailability of health professionals (absent, scarce, demotivated, and burnt out)
In one of the previous reviews (13), we saw how scarce health professionals were in Ethiopia in the last three decades. It was not unusual to find one or two midwives, one to three general practitioners and rarely one gynecologist in hospitals outside the big towns. By their nature, the majority of obstetric problems are night-time emergencies and bloody encounters. Due to overwhelming day and night work for years by few health professionals are likely to result in burn out and loss of interest to work with full energy. On top of that, if there are demotivating factors probably due to poor administration, the chance of on-time availability in the working place will be low. As a result, it is not unusual to find critically ill pregnant or laboring women unseen and unmanaged for several hours.
2. Health professionals' poor knowledge and skill
Emergency obstetric problems usually need at spot diagnosis and treatment. However, probably because of wrong diagnosis, it is not unusual to find a laboring or critically ill pregnant woman unnecessarily delayed in health facilities where appropriate treatment cannot be provided (delay in referral). Similarly, because of poor evaluation and lack of diagnostic skill or lack of better qualified health professionals in the rural areas and occasionally in big towns, wrong diagnosis can be made and delay providing appropriate treatment. A multi method assessment of 19 hospitals in Ethiopia revealed that only about 40% of the health service providers knew how to prevent, identify, and manage common maternal and perinatal complications like obstructed labor, preeclampsia/eclampsia, postpartum hemorrhage, maternal sepsis, neonatal sepsis and newborn resuscitation. The investigators concluded that there was poor quality of obstetric care at all levels of hospitals and among all provider types (54).
3. Incapacitated health facility ( lack of medical equipment, drugs, supplies, reagents, blood bank and oxygen)
The lack of essential medical equipment in the diagnostic setting (laboratory, imaging, delivery suite, operation theatre), lack of essential drugs for obstetric problems (misoprostol, dinoprostol, magnesium sulphate, broad spectrum intravenous antibiotics), and lack of oxygen, blood for transfusion or its substitute like iron infusion are very serious problems that are delaying the timely provision of treatment for critical ill laboring or pregnant women.
4. Uncooperative patient or relatives (refuse medication, procedure, blood donation, blood transfusion)
This may be because of cultural or religious reasons. It is a commonly observed phenomenon in the hospital setting where either the patients themselves or their relatives refusing medication, surgical procedures, blood donation or blood transfusion. Particularly for eclamptic women, relatives prefer to take the patient home claiming that this is not a disease to be treated medically; rather, they prefer to pray to God or to take her to a holy water or traditional healer. They call it “devil disease”. Similarly, the big challenge is with blood donation and transfusion. As partly discussed in the previous review (13), some people do not like to donate blood; some others may refuse blood transfusion due to religious or some other reasons. In short, patients and relatives may not only have a role in delaying sick pregnant women at home but also in the hospital for delaying treatment.
5. Inability of patient or relatives to afford for health service cost
As described in ‘delay II’, the majority of obstetric problems are ‘unbooked emergencies’ and the worst happens in the rural areas because of three reasons. 1) Since they are too far from hospitals, the transportation cost is very high. 2) Since the majority of the rural populations are farmers with subsistence life, they might not have enough money for emergency purpose. 3) Before arriving at the last hospital, they may visit several health facilities (particularly private or profit based health facilities). As a result, when they arrive at to the last hospital, it is not unusual for them to come with empty pockets. The worst happens when the hospital is short of emergency drugs and supplies, especially if the time of arrival is at night.
6. Poor leadership
Poor leadership in the hospital setting can be seen if the emergency facilities for obstetric emergencies are not well equipped; if there is mismanagement of hospital resources; if there is poor coordination and lack of understanding; if no action is taken for wrong doing and if the leaders (top-bottom) in the hospital are not role models for the majority, patients may not be managed timely and appropriately.
In short, delay in providing treatment can be manifested in two ways: failure to provide any treatment in time and failure to provide appropriate treatment. The reason for the delay in providing treatment is multifactorial. The contribution of delay in getting treatment to the high maternal and perinatal mortality in Ethiopia in the last three decades was probably as significant as delay I and II.
It should also be noted that although the major contributing factors for high maternal and perinatal mortality are the three Ds, there are several obstetric and medical complications which may not be treated even in the best hospitals of Ethiopia still due to limited capacity to provide maximum care. Among others, eclampsia with massive intracranial haemorrhage or hepatic rupture, amniotic fluid or blood pulmonary embolism, severe abruption with acute renal failure, and severe valvular stenosis of the heart with pregnancy are usually observed to have high maternal mortality.
In Ethiopia, where the government is investing a lot in health facilities, all-time accessible road construction, ambulance procurement and availing universal primary education, the contribution of delay I and II to maternal and perinatal mortality is expected to be low in the coming ten to fifteen years. Similarly, maternity care is now becoming free in several public health facilities with the exception of university and federal hospitals. And, training a huge number of health professionals is going on with the exception of specialty training. The cumulative effect is that the establishment of several infrastructure and facilities, human resource for health close to eliminating health service cost including transport is a collective virtue to make the high maternal and perinatal mortality a history. The detail is available in the next article (55).
Acknowledgement
We would like to thank PANE and KMG Ethiopia for the modest financial support granted for this review. We are also grateful to UNFPA Ethiopia for their generous financial support to cover the publication fee.
References
- 1.Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PFA. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–1074. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 2.Hunt P, De Mesquita JB. Reducing maternal mortality: the contribution of the right to the highest attainable standard of health. London: Human Rights Centre; 2010. University of Essex and UNFPA, New York. 2010. Available at: http://www.unfpa.org/webdav/site/global/shared/documents/publications/reducing_mm.pdf. [Google Scholar]
- 3.Neonatal & perinatal mortality: country, regional & global estimates. WHO; 2004. [Google Scholar]
- 4.Bhutta ZA, Darmstadt GL, Haws RA, Yakoob MY, Lawn JE. Delivering interventions to reduce the global burden of stillbirths: improving service supply and community demand. BMC Pregnancy Childbirth. 2009;7:9. doi: 10.1186/1471-2393-9-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Federal Democratic Republic of Ethiopia, author. Ministry of Health Health and Health Related Indicators. Policy planning directorate. 2010/2011. www.moh.gov.et.
- 6.World Health Organization, author. Appropriate technology for birth. Lancet. 1985;2:436–437. [PubMed] [Google Scholar]
- 7.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38:1091–1110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 8.Hill K, Thomas K, AbouZahr C, et al. Estimates of maternal mortality worldwide between 1990 and 2005: an assessment of available data. Lancet. 2007;370(9595):1311–1319. doi: 10.1016/S0140-6736(07)61572-4. [DOI] [PubMed] [Google Scholar]
- 9.WHO, UNICEF, UNFPA and The World Bank estimates, author. Trends in Maternal Mortality: 1990 to 2010. Retrieved from: http://whqlibdoc.who.int/publications/2012/97 89241503631_eng.pdf.
- 10.Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S, Stat DM. 3.6 Million Neonatal Deaths—What Is Progressing and What Is Not? Semin Perinatol. 2010;34:371–386. doi: 10.1053/j.semperi.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Babinard J, Roberts P. Maternal and child mortality development goals: what can the transport sector do? World Bank; 2006. Retrieved from http://www.eldis.org/go/topics/resource- guids/health&id=24669&type=Document. [Google Scholar]
- 12.Fournier P, Dumont A, Tourigny C, Dunkley G, Dramé S. Improved access to comprehensive emergency obstetric care and its effect on institutional maternal mortality in rural Mali. Bull World Health Organ. 2009;87(1):30–38. doi: 10.2471/BLT.07.047076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berhan Y, Berhan A. Reasons for persistently high maternal and perinatal mortalities in Ethiopia: Part I - Health system factors. Ethiop J Health Sci. 2014;(Special issue 1) doi: 10.4314/ejhs.v24i0.11s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berhan Y, Berhan A. Reasons for persistently high maternal and perinatal mortalities in Ethiopia: Part II - Socio-economic and cultural factors. Ethiop J Health Sci. 2014;(Special issue 1) doi: 10.4314/ejhs.v24i0.11s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nieburg P. Improving maternal mortality and other aspects of Women's health. The United States' global role. Center for strategic and international studies (CSIS) 2012 www.csis.org. [Google Scholar]
- 16.Kelly J, Kohls E, Poovan P, et al. The role of a maternity waiting area (MWA) in reducing maternal mortality and stillbirths in high-risk women in rural Ethiopia. BJOG. 2010;117:1377–1383. doi: 10.1111/j.1471-0528.2010.02669.x. [DOI] [PubMed] [Google Scholar]
- 17.Getachew B, Yifru B. Perinatal mortality and associated risk factors: a case control study. Ethiopian J Health Sci. 2012;22(3):153–162. [PMC free article] [PubMed] [Google Scholar]
- 18.Worku AG, Yalew AW, Afework MF. Maternal Complications and Women's Behavior in Seeking Care from Skilled Providers in North Gondar, Ethiopia. PLoS ONE. 2013;8(3):e60171. doi: 10.1371/journal.pone.0060171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Insaf TZ, Jurkowski JM, Alomar L. Sociocultural factors influencing delay in seeking routine health care among Latinas: A community-based participatory research study. Ethn Dis. 2010;20:148–154. [PubMed] [Google Scholar]
- 20.Bhosai SJ, Sinthusake T, Miwa S, Bradley E. Factors affecting patient access in Thailand: Understanding delay in care seeking for patients with cancer. Glob Public Health. 2010;20:1–13. doi: 10.1080/17441692.2010.508750. [DOI] [PubMed] [Google Scholar]
- 21.Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85(10):812–819. doi: 10.2471/BLT.06.035659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oxaal Z, Baden S. Challenges to women's reproductive health: maternal mortality. BRIDGE. 1996. Retrieved from: http://www.eldis.org/go/topics/
- 23.Hinz C. Maternal health. 2008. Retrieved from: http://www.dandc.eu/en/article/fistulas- serious-health-problem-ethiopia.
- 24.Central Statistical Agency [Ethiopia] and ICF International, author. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Agency and ICF International; 2012. [Google Scholar]
- 25.Monitoring Emergency Obstetric care: A handbook. World Health Organization; 2009. Retrieved from: http://www.unfpa.org/webdav/site/global/mon itoring.pdf. [Google Scholar]
- 26.van Beekhuizen HJ, Unkels R, Mmuni NS, Kaiser M. Complications of obstructed labour: pressure necrosis of neonatal scalp and vesicovaginal fistula. Lancet. 2006;368(9542):1210. doi: 10.1016/S0140-6736(06)69477-4. [DOI] [PubMed] [Google Scholar]
- 27.Fantu S, Segni H, Alemseged F. Incidence, causes and outcome of obstructed labor in Jimma University specialized hospital. Ethiop J Health Sci. 2010;20(3):145–151. doi: 10.4314/ejhs.v20i3.69443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bieler RW, Schnabel T. Pituitary and ovarian function in women with vesicovaginal ?stula after obstructed and prolonged labour. S Afr Med J. 1976;50:257–266. [PubMed] [Google Scholar]
- 29.Ijaiya MA, Rahman AG, Aboyeji AP, et al. Vesicovaginal fistula: a review of nigerian experience. West Afr J Med. 2010;29(5):293–298. doi: 10.4314/wajm.v29i5.68247. [DOI] [PubMed] [Google Scholar]
- 30.Hamlin C. Back to Office Report. Addis Ababa Fistula Hospital; 2004. Preventing Fistula: Transport's Role in Empowering Communities for Health in Ethiopia, (August 30–September 13, 2004) Retrieved from: http://www.transaid.org/images/ [Google Scholar]
- 31.Abdella A. Maternal Mortality Trend in Ethiopia. Ethiop J Health Dev. 2010;(Special Issue 1):115–122. [Google Scholar]
- 32.El-Sahrty S, Kebede S, Olango P, Siadat B. Ethiopia - Improving health service delivery. 2009. http://www.scribd.com/doc/23145128/Ethiopia-Health-Service-Delivery-2009.
- 33.Babinard J. Transport for health in developing countries: Overview of issues and measures to improve access —MDG 4 & 5 context. 2006. http://siteresources.worldbank.org/INTTSR/Resources/06-01-30-Transport.
- 34.Gaym A. A review of maternal mortality at Jimma Hospital, Southwestern Ethiopia. Ethiop J Health Dev. 2000;14(2):215–223. [Google Scholar]
- 35.De Silva R. Transport - The Missing Link? A catalyst for achieving the MDG, Presentation for the International Federation of Rural Transport Development. Retrieved from: http://www.transaid.org/images/
- 36.Rutherford ME, Mulholland K, Hill PC. How access to health care relates to under-five mortality in sub-Saharan Africa: systematic review. Trop Med Int Health. 2010;15(5):508–519. doi: 10.1111/j.1365-3156.2010.02497.x. [DOI] [PubMed] [Google Scholar]
- 37.McCoy D, Tanya B, Visser M, Doherty R. Interim Findings on the National PMTCT Pilot Sites. Durban: Health Systems Trust & Department of Health, Republic of South Africa; 2002. www.hst.org.za/publications/ [Google Scholar]
- 38.Tewodros B, Mariam AG, Dbaba Y. Factors affecting antenatal care utilization in Yem special woreda, southwestern Ethiopia. Ethiop J Health Sci. 2009;19(1):45–51. [Google Scholar]
- 39.Murray SF, Pearson FC. Maternity referral systems in developing countries: Current knowledge and future research needs. Soc Sci Med. 2006;62:2205–2215. doi: 10.1016/j.socscimed.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 40.Krasovec K. Auxiliary technologies related to transport and communication for obstetric emergencies. Int J Gynaecol Obstet. 2004;85(Suppl. 1):S14–S23. doi: 10.1016/j.ijgo.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 41.Alwar J, Matonga V, Sikatoye b. Report of the summative evaluation of the essential obstetric care project in Mpongwe, Masaiti and Lufwanyama. United Nations Children's Fund. 2000 Retrievable at: http://www.eldis.org/go/topics/ [Google Scholar]
- 42.Molesworth K. The Road to Health? International Forum for Rural Transport and Development. 2002 Retrievable from: http://www.eldis.org/go/topics/resource. [Google Scholar]
- 43.Molesworth K. Mobility and health: the impact of transport provision on direct and proximate determinants of access to health services. 2006 Retrieved from: www.eldis.org/go/topics/resource. [Google Scholar]
- 44.Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19(2):69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- 45.Borghi J, Ensor T, Neupane B D, Tiwari S. Study on the costs of accessing EOC services in Nepal. Kathmandu: Options; 2004. [Google Scholar]
- 46.Luck M. Safe Motherhood intervention studies in Africa: A review. East Afr Med J. 2000;77(11):599–607. doi: 10.4314/eamj.v77i11.46732. [DOI] [PubMed] [Google Scholar]
- 47.Balde MD, Bastert G. Decrease in uterine rupture in Conakry, Guinea by improvements in transfer management. Int J Gynec Obstet. 1990;31:21–24. doi: 10.1016/0020-7292(90)90176-l. [DOI] [PubMed] [Google Scholar]
- 48.Samai O, Sengeh P. Facilitating emergency obstetric care through transportation and communication, Bo, Sierra Leone. The Bo PMM Team. Int J Gynaecol Obstet. 1997;59(supplement 2):S157–S164. doi: 10.1016/s0020-7292(97)00161-6. [DOI] [PubMed] [Google Scholar]
- 49.TRANSAID, author. Access to Health Services: Intermediate modes of transport in resource poor aresa. (For Presentation at the IFRTD Conference on Transport Solutions for Access to Health care in Rural Africa) Retrieved at: http://www.transaiSd.org/images/resources/
- 50.World Bank, author. Safe, clean, and affordable transport for development. worldbank.org/INTTRANSPORT/Resources/
- 51.Ransom EI, Yinger NV. Making motherhood safer: overcoming obstacles on the pathway to care. Population Reference Bureau; 2002. Retrieved at: http://www.eldis.org/go/topics/resource- guides/health&id=16099&type=Document. [Google Scholar]
- 52.Downing A, Sethic D. Health issues in transport and the implications for policy. UK: Department for International Development; 2001. Retrieved on-line from from http://www.eldis.org/go/topics/resource. [Google Scholar]
- 53.Jokhio AH, Winter HR, Cheng KK. An intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N Engl J Med. 2005;352(20):2091–2099. doi: 10.1056/NEJMsa042830. [DOI] [PubMed] [Google Scholar]
- 54.Getachew A, Ricca J, Cantor D, Rawlins B, Rosen H, Tekleberhan A, Bartlett L, Gibson H. Quality of Care for Prevention and Management of Common Maternal and Newborn Complications: A Study of Ethiopia's Hospitals. Jhpiego Brown's Wharf 1615 Thames Street, Baltimore: 2011. www.jhpiego.org. [Google Scholar]
- 55.Berhan Y, Berhan A. Actions in the pipeline and the way forward to reduce maternal and perinatal mortality in Ethiopia. Ethiop J Health Sci. 2014;(Special issue 1) doi: 10.4314/ejhs.v24i0.13s. [DOI] [PMC free article] [PubMed] [Google Scholar]