Abstract
The evolution of oseltamivir resistance mutations during selection through serial passages in animals is still poorly described. Herein, we assessed the evolution of neuraminidase (NA) and hemagglutinin (HA) genes of influenza A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2) viruses recovered from the lungs of experimentally infected BALB/c mice receiving suboptimal doses (0.05 and 1 mg/kg of body weight/day) of oseltamivir over two generations. The traditional phenotypic and genotypic methods as well as deep-sequencing analysis were used to characterize the potential selection of mutations and population dynamics of oseltamivir-resistant variants. No oseltamivir-resistant NA or HA changes were detected in the recovered A/WSN/33 viruses. However, we observed a positive selection of the I222T NA substitution in the recovered A/Victoria/3/75 viruses, with a frequency increasing over time and with an oseltamivir concentration from 4% in the initial pretherapy inoculum up to 28% after two lung passages. Although the presence of mixed I222T viral populations in mouse lungs only led to a minimal increase in oseltamivir 50% enzyme-inhibitory concentrations (IC50s) (by a mean of 5.7-fold) compared to that of the baseline virus, the expressed recombinant A/Victoria/3/75 I222T NA protein displayed a 16-fold increase in the oseltamivir IC50 level compared to that of the recombinant wild type (WT). In conclusion, the combination of serial in vivo passages under neuraminidase inhibitor (NAI) pressure and temporal deep-sequencing analysis enabled, for the first time, the identification and selection of the oseltamivir-resistant I222T NA mutation in an influenza H3N2 virus. Additional in vivo selection experiments with other antivirals and drug combinations might provide important information on the evolution of antiviral resistance in influenza viruses.
INTRODUCTION
Influenza viruses are major human respiratory pathogens, responsible for seasonal epidemics in temperate countries and occasional but devastating pandemics. Influenza A viruses of the H1N1 and/or H3N2 subtypes have been the viruses most frequently associated with annual epidemics during the past 40 years. Neuraminidase inhibitors (NAIs) such as oseltamivir, the most widely used NAI, and zanamivir target the active site of the influenza neuraminidase (NA) molecule, which is constituted by 8 catalytic (R118, D151, R152, R224, E276, R292, R371, and Y406) (N2 numbering is used here and throughout the text) and 11 framework (E119, R156, W178, S179, D198, I222, E227, H274, E277, N294, and E425) residues that are largely conserved among influenza A and B viruses (1). Accordingly, these antivirals are active against all influenza strains and are thus recommended for the treatment of severe infections and also in high-risk individuals. However, as for other antivirals, extensive use of NAIs might lead to the emergence and transmission of drug-resistant variants that might compromise their clinical usefulness.
The generation and characterization of drug-resistant influenza variants through in vitro passages under NAI pressure can improve our understanding of the mechanisms of resistance to these anti-influenza agents. Indeed, the main NA mutations conferring resistance to oseltamivir in humans, such as the H274Y change in the N1 subtype and the E119V and R292K changes in the N2 subtype, were previously predicted by in vitro studies (2–4). However, in vitro studies do not mimic completely the distribution and configuration of sialic acid receptors in the respiratory tract nor do they account for the role of the immune response. In addition to these oseltamivir resistance NA mutations, clinical influenza A(H1N1) and A(H3N2) variants occasionally contain other substitutions in the NA and/or hemagglutinin (HA) genes (5–7), although the contribution of these secondary mutations to the phenotype of resistance and to viral replicative capacity is not completely understood. Moreover, only a few studies have investigated the in vivo (animal) evolution of NA and HA genes from influenza viruses exposed to NAI pressure (8, 9).
The advent of next-generation deep sequencing has considerably expanded the limits of more traditional detection techniques such as reverse transcriptase (RT) PCR and automated Sanger sequencing in terms of increased sensitivity and multiplexing. This technology enabled the detection and identification of rare low-frequency variants occurring in a given viral population (10). In this study, we selected oseltamivir-resistant variants by performing sequential passages of influenza A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2) strains in mice receiving suboptimal doses of oseltamivir. We used traditional phenotypic and genotypic methods to characterize the recovered viruses, as well as next-generation deep-sequencing analysis to assess the genomic diversity and population dynamics of oseltamivir-resistant variants.
MATERIALS AND METHODS
Ethics statement.
All animal procedures were approved by the institutional animal care committee of Laval University according to the guidelines of the Canadian Council of Animal Care.
Viral stocks.
Two mouse-adapted strains were selected for this study. The recombinant influenza A/WSN/33 (H1N1) wild-type (WT) virus was previously generated using a reverse genetics system that includes eight influenza virus RNA transcription plasmids (pPOLI-PA, -PB1, -PB2, -NP, -HA, -NA, -M, and -NS) and polymerase and nucleoprotein expression plasmids (pCAGGS-PA, -PB1, -PB2, and -NP), kindly provided by Peter Palese (Mount Sinai School of Medicine, New York, NY) (11). A 1-μg aliquot from each of the 12 plasmids was cotransfected into 293T human embryonic kidney cells using the Lipofectamine 2000 reagent (Life Technologies Corporation, Grand Island, NY) as previously described (11). Supernatants were collected 72 h posttransfection and used to inoculate Madin-Darby canine kidney (MDCK) cells for viral amplification. The mouse-adapted influenza A/Victoria/3/75 (H3N2) virus (a gift from Donald Smee, Utah State University, Logan, UT) was passaged twice in MDCK cells in the absence of NAIs before animal infection. Both viruses were sequenced using the automated ABI 3730 DNA analyzer (Applied Biosystems, Carlsbad, CA) and titrated by standard plaque assays in MDCK cells.
Mouse studies. (i) First passage.
In a single experiment, groups of 16 6- to 8-week-old female BALB/c mice (Charles River, ON, Canada) were infected by intranasal (i.n.) instillation of 2 × 103 PFU of A/WSN/33 (H1N1) or A/Victoria/3/75 (H3N2) viruses in 30 μl of saline. Oral treatments (by gavage) with either saline or suboptimal doses of oseltamivir (0.05 and 1 mg/kg of body weight) were started 4 h before viral infection (day 0) and were continued once daily until day 5 postinfection (p.i.) to favor the induction of drug-resistant strains. The low concentration of oseltamivir was chosen to rapidly select for drug resistance based on clinical reports when low-dose prophylaxis or treatment was used (12, 13). Animals were weighed daily for 14 days and monitored for clinical signs and mortality. On days 4 (expected maximum weight loss) and 6 (the first day after the end of the oseltamivir treatment) p.i., four mice per group were sacrificed, and the lungs were removed aseptically. For the determination of the viral titers, harvested lung tissues were homogenized in 1 ml of Dulbecco's modified Eagle medium (Life Technologies Corporation) with antibiotics using the TissueLyser bead mill homogenizer (Qiagen, Toronto, ON, Canada). Cells were pelleted by centrifugation (2,000 × g for 5 min), and the supernatants were collected. A 100-μl aliquot of each lung supernatant was stored at −80°C for phenotypic testing (viral isolation and NA inhibition assay), and the remaining ∼900 μl were pooled by treatment group (4 lungs per pool) and stored at −80°C for subsequent RNA extraction and viral titration by plaque assays in MDCK cells.
(ii) Second passage.
Groups of 16 6- to 8-week-old female BALB/c mice were infected intranasally with 1 × 103 PFU of viruses originating from the pooled supernatants of the lung homogenates recovered on day 6 p.i. of the first passage (P1). Treatments were carried out in the same way as for P1, with the exception that the two groups treated with oseltamivir in P1 (0.05 and 1 mg/kg) were both treated with 1 mg/kg oseltamivir during the second passage (P2). The group treated with saline during P1 (“P1-untreated”) also received saline during P2. Mortality, weight loss, and clinical signs were monitored for 14 days. Lungs were also removed from 4 mice per group on days 4 and 6 p.i. for NA inhibition assays and then pooled for subsequent RNA extraction and viral titration.
RT-PCR amplification and automated sequencing.
RNA was isolated from the pooled supernatants of the lung homogenates using the QIAamp viral RNA minikit (Qiagen) and then was resuspended in a volume of 50 μl. cDNA was synthesized using specific A/WSN/33 and A/Victoria/3/75 NA and HA primers and the SuperScript II reverse transcriptase enzyme (Life Technologies Corporation). Full-length viral NA and HA cDNAs were amplified by PCR using the Phusion high-fidelity DNA polymerase (New England BioLabs, Whitby, ON, Canada) and specific primers (available upon request) in standard conditions. The nucleotide sequences of the PCR products were determined using the ABI 3730 DNA analyzer, and the heights of the chromatogram peaks were analyzed using BioEdit, version 7.0.5.
Cloning of PCR products.
Complete PCR-amplified NA genes from the pooled lung homogenates collected on day 6 p.i. during P2 were purified and then cloned by blunt-end ligation into the pJET 1.2 vector using the CloneJET PCR cloning kit (Fisher Scientific, Ottawa, ON, Canada), according to the manufacturer's instructions. At least 18 NA-positive recombinant plasmids per group were randomly selected and subjected to sequence analysis with the ABI 3730 DNA analyzer.
Deep sequencing.
DNA libraries were prepared with 0.5 ng of each of the full-length viral NA and HA PCR products obtained from the viral inocula and from the pooled lung homogenates recovered on days 4 and 6 p.i. of both P1 and P2, using the Nextera XT sample preparation kit (Illumina, San Diego, CA), according to the manufacturer's instructions. Previously cloned A/Quebec/144147/09 (H1N1)pdm09 NA and HA genes (14) were amplified in the same conditions as the samples and included in the preparation of DNA libraries as controls. A purification step with AMPure XP beads (Beckman Coulter, Mississauga, ON, Canada) to remove very short library fragments was performed prior to library normalization. The libraries were then multiplexed, clustered, and finally sequenced using the Nextera XT kit (Illumina) as described by the manufacturer, except that 10% phiX Control (Illumina) was added to the library pool. The paired-end sequencing (2 × 250 nucleotides [nt]) was performed on a MiSeq system (Illumina), and reads were demultiplexed using CASAVA 1.8.2 (Illumina), allowing no mismatch in the bar codes. After sequencing, reads were filtered for quality using the FASTX-Toolkit 0.0.13 quality trimmer, and only reads passing the filter (quality score of >30 and read length of >150 nt) were kept for the following analysis.
Bioinformatics analysis.
The reads obtained from the A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2) inocula (viral stocks) were assembled de novo using Ray 2.2.0 (15, 16), and the consensus sequences of the two NA and HA genes were extracted from the contig files based on their similarity to reference sequences (GenBank accession numbers J02177, HE802059, HM641200, and V01098). The extremities of each gene were verified and completed manually, based on the reference sequences, to facilitate downstream analyses. Reads were aligned to the full-length assembled gene sequences to ascertain the absence of assembly errors. Single nucleotide polymorphisms (SNPs) were searched with GATK 2.7.4 (17), and no mismatches between the reads and the assembled contigs were detected. These curated and validated sequences were considered at this point the reference sequences for assessing the emergence of mutations. The reads from each sample were aligned to each corresponding reference sequence using BWA 0.6.1 (18), and the nucleotide depth for each position was assessed with GATK. To correct for potential erroneous calling of SNPs due to the intrinsic error rate of the RT-PCR amplification and sequencing reactions, we used the A(H1N1)pdm09 NA and HA control amplicons to calculate the proportion of nucleotides not matching the known reference sequences and obtained a mismatch frequency of 0.13% ± 0.10%. Therefore, we established a 1% cutoff value, over which all positions with a nucleotide different from the reference sequence were considered significant. These sequences were selected using a simple Python script (available at https://github.com/plpla/SNP_finder).
Evolution of the A/Victoria/3/75 (H3N2) I222T NA genotype during in vitro passages.
The A/Victoria/3/75 (H3N2) inoculum (stock) virus and the virus recovered on day 6 p.i. from the P2-oseltamivir/P1-oseltamivir 1 mg/kg group were subjected to 4 serial passages in MDCK cells infected at a multiplicity of infection (MOI) of 0.001 in the absence of drug pressure. Passages in the presence of increasing concentrations of oseltamivir (from 10 nM at passage 1 to 80 nM at passage 4) were concomitantly performed. At each passage, viral RNA was isolated from supernatants of infected cell cultures, and complete NA genes were amplified by RT-PCR. PCR products were purified and sequenced with the ABI 3730 DNA analyzer, and the heights of the chromatogram peaks were analyzed using BioEdit, version 7.0.5.
Expression of recombinant NA proteins.
The pPOLI transcription plasmids containing the WT NA gene of either A/WSN/33 (H1N1) or A/Victoria/3/75 (H3N2) viruses were used for the introduction of single mutations (F149S and D434V in A/WSN/33 and I222T in A/Victoria/3/75) using the appropriate primers and the QuikChange site-directed mutagenesis kit (Stratagene, La Jolla, CA). The resulting plasmids were sequenced to ensure the absence of undesired mutations. The expression and analysis of recombinant NA proteins were performed as previously described (19). Briefly, 293T cells were cotransfected with 1 μg of each of the 4 expression plasmids (pCAGGS-PA, -PB1, -PB2, and -NP) of A/WSN/33 and one of the respective pPOLI-NA transcription plasmids of A/WSN/33 or A/Victoria/3/75. At 48 h posttransfection, cells were treated with 0.02% EDTA in phosphate-buffered saline (PBS) and harvested. After one wash with PBS, the cells were resuspended in PBS containing 3.5 mM CaCl2 and used in NA inhibition assays to determine the susceptibility of expressed proteins to oseltamivir.
Drug susceptibility assays.
The drug susceptibility phenotype was determined by a fluorometric NA inhibition assay as described elsewhere (20). Stock viruses, viruses isolated from mouse lungs before pooling on days 4 and 6 p.i. and passaged once in MDCK cells, or recombinant proteins were standardized to an NA activity level 10-fold higher than that of the background as measured by the production of a fluorescent product from the 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA) (Sigma, St. Louis, MO, USA) substrate. Drug susceptibility profiles were determined by the extent of NA inhibition after incubation with serial 3-fold dilutions of oseltamivir carboxylate (Hoffmann-La Roche, Basel, Switzerland) at final concentrations ranging between 0 and 1,800 nM. The 50% enzyme-inhibitory concentration (IC50) values were determined from the dose-response curves.
Statistical analysis.
Weight loss, lung viral titers (LVT), and mutation frequencies from in vitro passages were compared by one-way analysis of variance (ANOVA) with Tukey's multiple comparison posttest using GraphPad, version 5.
RESULTS
Effect of oseltamivir treatment on A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2) virus infections in mice.
As shown in Table 1, i.n. inoculation of mice with 2 × 103 PFU of A/WSN/33 or A/Victoria/3/75 viruses (P1) resulted in mortality rates of 87.5% and 25% and mean maximum weight losses on day 4 of 19.9% ± 1.5% and 15.3% ± 1.8%, respectively, in both untreated groups. No mortality or significant weight loss was observed in any of the groups infected and treated with oseltamivir during P1. In line with these observations, the mean LVT on day 6 p.i. were higher for the untreated groups than for those treated with 0.05 mg/kg and 1 mg/kg oseltamivir, although these differences were significant only in the case of A/WSN/33 [(8.6 ± 0.3) × 106 versus (3.5 ± 0.1) × 106 and (0.59 ± 0.03) × 106 PFU/lung, respectively, P < 0.05], but not in the case of A/Victoria/3/75 [(2.1 ± 0.2) × 106 versus (1.7 ± 0.1) × 106 and (1.3 ± 0.3) × 106 PFU/lung, respectively]. Notably, the mean LVT in untreated groups were significantly higher in mice infected with A/WSN/33 than in those infected with A/Victoria/3/75 on day 6 of P1 [(8.6 ± 0.3) × 106 versus (2.1 ± 0.2) × 106 PFU/lung, respectively, P < 0.05] but not P2.
TABLE 1.
Effect of oseltamivir therapy in mice infected with the A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2) viruses
| Virus/regimena | % wt loss on day 4 p.i.b (mean ± SD) (n = 8) | % mortality on day 14 p.i. (n = 8) | LVTc on day 6 p.i. (mean ± SD) (n = 4) |
|---|---|---|---|
| A/WSN/33 (H1N1) | |||
| P1-unt | 19.9 ± 1.5 | 87.5 | 8.6 ± 0.3 × 106 |
| P1-ose 0.05 mg/kg | <1 | 0 | 3.5 ± 0.1 × 106d |
| P1-ose 1 mg/kg | <1 | 0 | 0.59 ± 0.03 × 106d |
| P2-unt/P1-unt | 5.3 ± 1.2 | 0 | 3.2 ± 0.4 × 106 |
| P2-ose/P1-ose 0.05 mg/kg | <1 | 0 | 5.9 ± 0.4 × 103e |
| P2-ose/P1-ose 1 mg/kg | <1 | 0 | 5.4 ± 0.3 × 103e |
| A/Victoria/3/75 (H3N2) | |||
| P1-unt | 15.3 ± 1.8 | 25 | 2.1 ± 0.2 × 106 |
| P1-ose 0.05 mg/kg | <1 | 0 | 1.7 ± 0.1 × 106 |
| P1-ose 1 mg/kg | <1 | 0 | 1.3 ± 0.3 × 106 |
| P2-unt/P1-unt | 4.8 ± 0.9 | 0 | 3.1 ± 0.3 × 106 |
| P2-ose/P1-ose 0.05 mg/kg | <1 | 0 | 2.4 ± 0.3 × 106 |
| P2-ose/P1-ose 1 mg/kg | <1 | 0 | 3.0 ± 0.4 × 106 |
The viral inoculum was 2 × 103 PFU in passage 1 (P1) and 1 × 103 PFU in passage 2 (P2). unt, untreated; ose, oseltamivir.
p.i., postinfection.
LVT, lung viral titers in PFU/lung. Means ± SD from a single experiment performed in triplicate are presented.
P < 0.05 compared to the corresponding untreated group of each passage.
P < 0.001 compared to the corresponding untreated group of each passage.
For the second passage (P2), mice were infected with 1 × 103 PFU of viruses originating from the pooled supernatants from the lung homogenates recovered on day 6 p.i. of P1, and the oseltamivir pressure was maintained at the highest concentration used in P1 (1 mg/kg). No mortality was observed in any of the groups, and only small mean weight losses on day 4 p.i. were observed in both P2-untreated/P1-untreated groups (5.3% ± 1.2% in A/WSN/33 and 4.8% ± 0.9% in A/Victoria/3/75) (Table 1). Significantly higher LVT on day 6 p.i. were observed in the A/WSN/33 P2-untreated/P1-untreated [(3.2 ± 0.4) × 106 PFU/lung] group than in the P2-oseltamivir/P1-oseltamivir 0.05 mg/kg [(5.9 ± 0.4) × 103 PFU/lung] and P2-oseltamivir/P1-oseltamivir 1 mg/kg [(5.4 ± 0.3) × 103 PFU/lung] groups (P < 0.001). Conversely, for A/Victoria/3/75, the mean LVT on day 6 p.i. were comparable between the P2-untreated/P1-untreated [(3.1 ± 0.3) × 106 PFU/lung], P2-oseltamivir/P1-oseltamivir 0.05 mg/kg [(2.4 ± 0.3) × 106 PFU/lung], and P2-oseltamivir/P1-oseltamivir 1 mg/kg [(3.0 ± 0.4) × 106 PFU/lung] groups.
Characterization of viruses recovered from mouse lungs.
Both pretherapy inoculum viruses were susceptible to oseltamivir, with IC50s of 0.75 ± 0.04 nM for A/WSN/33 and 0.26 ± 0.04 nM for A/Victoria/3/75. Since it is difficult to perform NAI assays directly from lung homogenates, 100-μl aliquots from each individual lung (4 per group) recovered at the four time points of the study were taken prior to pooling and then propagated once in MDCK cells for phenotypic analysis (Table 2). The WHO guidelines on the determination of NAI resistance for influenza A virus isolates define “reduced inhibition” by a 10- to 100-fold increase in IC50s and “highly reduced inhibition” by a >100-fold increase in IC50s (21). According to this criterion, none of the viruses recovered from mouse lungs had reduced or highly reduced inhibitions to oseltamivir compared to the respective pretherapy inoculum viruses. For A/WSN/33 (H1N1) viruses, the maximum increase in oseltamivir IC50 (mean of 2.7-fold; range, 1.9- to 3.5-fold) was observed in isolates obtained from the P1-oseltamivir 0.05 mg/kg group on day 4 p.i. Of note, the low NA activity displayed by the P1-oseltamivir 1 mg/kg and P2-oseltamivir/P1-oseltamivir 0.05 mg/kg A/WSN/33 viruses precluded NA inhibition testing. On the other hand, IC50s seemed to slightly increase with oseltamivir pressure in A/Victoria/3/75 (H3N2) viruses, with the maximum increase (mean of 5.7-fold; range, 5.5- to 5.8-fold) observed for the P2-oseltamivir/P1-oseltamivir 1 mg/kg group on day 6 p.i.
TABLE 2.
Oseltamivir susceptibility of viruses recovered from individual lungs of mice infected with the A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2) viruses
| Virus/regimena | Oseltamivir IC50b (mean [range]) (nM) |
|||
|---|---|---|---|---|
| Day 4 p.i.c (n = 4) | Foldd | Day 6 p.i. (n = 4) | Fold | |
| A/WSN/33 (H1N1) | ||||
| P1-unt | 1.36 (1.09–1.87) | 1.8 | 1.07 (0.94–1.20) | 1.4 |
| P1-ose 0.05 mg/kg | 2.06 (1.46–2.65) | 2.7 | 1.27 (1.04–1.47) | 1.7 |
| P1-ose 1 mg/kg | Low activitye | Low activity | ||
| P2-unt/P1-unt | 0.61 (0.46–0.81) | 0.8 | 0.36 (0.34–0.37) | 0.5 |
| P2-ose/P1-ose 0.05 mg/kg | Low activity | Low activity | ||
| P2-ose/P1-ose 1 mg/kg | 0.75 (0.70–0.80) | 1.0 | 0.68 (0.65–0.72) | 0.9 |
| A/Victoria/3/75 (H3N2) | ||||
| P1-unt | 0.37 (0.26–0.49) | 1.4 | 0.45 (0.39–0.55) | 1.7 |
| P1-oseltamivir 0.05 mg/kg | 0.78 (0.48–1.14) | 3.0 | 0.57 (0.56–0.58) | 2.2 |
| P1-ose 1 mg/kg | 1.24 (0.88–1.85) | 4.8 | 1.02 (0.98–1.07) | 3.9 |
| P2-unt/P1-unt | 0.73 (0.50–1.06) | 2.8 | 0.21 (0.19–0.22) | 0.8 |
| P2-ose/P1-ose 0.05 mg/kg | 0.63 (0.42–0.94) | 2.4 | 0.72 (0.68–0.74) | 2.8 |
| P2-ose/P1-ose 1 mg/kg | 1.30 (1.17–1.48) | 5.0 | 1.47 (1.42–1.52) | 5.7 |
P1, passage 1; P2, passage 2; unt, untreated; ose, oseltamivir.
IC50, 50% enzyme-inhibitory concentration. Mean values from a single experiment performed in duplicate are presented.
p.i., postinfection.
Fold increase versus oseltamivir IC50s of the pretherapy inoculum viruses (A/WSN/33 = 0.75 ± 0.04 nM; A/Victoria/3/75 = 0.26 ± 0.04 nM).
Low activity, NA activity was detected but was not high enough to determine the IC50.
To detect the possible emergence and/or selection of NA variants due to oseltamivir pressure, RNA from the pooled lung homogenates recovered on days 4 and 6 p.i. of P2 was amplified by specific RT-PCR and subjected to automated conventional sequencing (Table 3). Interestingly, the chromatogram analysis of the NA gene from A/Victoria/3/75 revealed the presence of mixed I222T viral populations with an approximate 80:20 (WT/mutant) ratio in the P2-oseltamivir/P1-oseltamivir 1 mg/kg group, on both days 4 (not shown) and 6 p.i. In addition, no other mutations or mixed viral populations were identified in the remaining A/Victoria/3/75 groups or in any of the A/WSN/33 groups.
TABLE 3.
Detection of single nucleotide polymorphisms in the NA of viruses recovered from lungs of mice (day 6 p.i. of passage 2) infected with the A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2) viruses by automated (Sanger) sequencing, colony screening (cloning), and deep sequencinga
| Virus/regimenb | NA positionc | Referenced | SNP detected by: |
Depthe | ||
|---|---|---|---|---|---|---|
| Sanger sequencing (%) | Cloning (%) | Deep sequencing (%) | ||||
| A/WSN/33 (H1N1) | ||||||
| P2-ose/P1-ose 0.05 mg/kg | 389 | M | M | M/T (95/5) | M/T (99/1) | 124,898 |
| 434 | D | D | D/E (95/5) | D/Ef (98/2) | 77,999 | |
| A/Victoria/3/75 (H3N2) | ||||||
| P2-unt/P1-unt | 46 | A | A | A/P (94/6) | A/P (94/6) | 57,911 |
| 73 | I | I | I/T (94/6) | I/T (96/4) | 72,738 | |
| 131 | Q | Q | Q/H (88/12) | Q/H (96/4) | 78,897 | |
| 398 | V | V | V/I (94/6) | V/I (93/7) | 66,338 | |
| P2-ose/P1-ose 0.05 mg/kg | 200 | N | N | N/D (89/11) | N/D (88/12) | 81,069 |
| 222 | I | I | I/T (84/16) | I/T (85/15) | 78,541 | |
| 398 | V | V | V/I (95/5) | V/I (87/13) | 56,232 | |
| P2-ose/P1-ose 1 mg/kg | 131 | Q | Q | Q/H (94/6) | Q/H (98/2) | 128,656 |
| 222 | I | I/T (80/20) | I/T (78/22) | I/T (72/28) | 167,234 | |
| 398 | V | V | V/I (94/6) | V/I (95/5) | 104,690 | |
Data correspond to viruses recovered from pooled lung homogenates on day 6 p.i. of the second passage (P2). Only treatment groups in which single nucleotide polymorphisms (SNPs) were detected are shown (deletions are not shown). The residues in bold type confer reduced susceptibility to oseltamivir.
P1, passage 1; P2, passage 2; unt, untreated; ose, oseltamivir.
N2 numbering.
Reference; the predominant residues found in these positions in the reference sequences.
Mean number of reads that cover that position in the deep-sequencing analysis.
A D/V (93/7) substitution was also found at this position by deep sequencing but not by cloning in the P2-ose/P1-ose 1 mg/kg group.
To further characterize the genotypic profiles of the recovered viruses, amplicons obtained from the pooled lung homogenates recovered on day 6 p.i. of P2 were cloned, and at least 18 NA-positive cDNA clones were sequenced (Table 3). The analysis of A/WSN/33 clones revealed that 20/21 clones were identical to the WT sequence in the P2-untreated/P1-untreated group, while the remaining clone had a deletion of 1 nt at position 351 that resulted in a frameshift. This frameshift generated a stop codon, and the resulting formation of a truncated 118-amino-acid (aa) NA protein. In the P2-oseltamivir/P1-oseltamivir 0.05 mg/kg group, 18/20 clones were identical to the WT sequence. The remaining two clones showed single M389T or D434E mutations. A deletion of 28 nt at position 400 that resulted in a truncated 134-aa NA protein was observed in 1/23 clones of the P2-oseltamivir/P1-oseltamivir 1 mg/kg group. The remaining 22/23 clones were identical to the WT sequence. For the A/Victoria/3/75 virus, 14/18 clones of the P2-untreated/P1-untreated group were identical to the WT sequence, 3 clones presented a single A46P, I73T, or Q131H mutation, and 1 clone presented both Q131H and V398I mutations. In the P2-oseltamivir/P1-oseltamivir 0.05 mg/kg group, 13/19 clones were identical to the WT sequence, whereas the remaining clones presented single N200D (2 clones), I222T (3 clones), or V398I (1 clone) substitutions. In the P2-oseltamivir/P1-oseltamivir 1 mg/kg group, 4/18 clones presented the I222T mutation, and 2 other clones had either a single Q131H or V398I substitution. The remaining 12/18 clones were identical to the WT sequence.
Characterization of genomic diversity and population dynamics of oseltamivir-resistant variants by deep sequencing.
The frequencies of the SNPs found in the viruses recovered from the lung homogenates on day 6 p.i. of P2 by the conventional sequencing and clone analysis were compared with those found by deep sequencing in Table 3. In general, SNPs found by molecular cloning correlated well with the frequencies found at these positions by deep sequencing. We also analyzed the changes in the frequencies of the individual SNPs as a function of the oseltamivir concentration, day of specimen collection, and passage number. None of the hallmark NA mutations associated with resistance to oseltamivir in N1 (I222V, H274Y, and N294S) or N2 (E119V and R292K) viruses were observed. Furthermore, no NA or HA mutations found in any of the groups infected with the A/WSN/33 virus showed frequency variations that might be considered indicators of a positive selection due to passage or oseltamivir pressure compared to the initial inoculum. The only exceptions were the F149S and D434V NA substitutions that, despite being undetectable by molecular cloning, emerged by deep sequencing in the P2-oseltamivir/P1-oseltamivir 1 mg/kg group at the last time point of the study (day 6 p.i. of P2) with frequencies of 22.9% and 7.1%, respectively (not shown).
Conversely, in the A/Victoria/3/75 virus, the temporary evolution of the I222T NA substitution revealed a pattern of positive selection by oseltamivir pressure, with an increase in frequencies that correlated with both the drug concentration and days of treatment, reaching a peak of 28.2% for the P2-oseltamivir/P1-oseltamivir 1 mg/kg group on day 6 p.i. (Fig. 1). This oseltamivir-dependent selection was further confirmed by in vitro passages of the inoculum (stock) virus as well as the virus recovered on day 6 p.i. from the P2-oseltamivir/P1-oseltamivir 1 mg/kg group. The chromatogram analysis showed no changes in the frequencies of the T222 NA viral populations after 4 passages in the absence of oseltamivir, remaining undetectable in the inoculum virus and at a mean of 19.9% ± 0.9% in the P2-oseltamivir/P1-oseltamivir 1 mg/kg virus. On the other hand, after the fourth passage under increasing concentrations of oseltamivir (final concentration of 80 nM), the frequencies of the T222 NA viral populations shifted from undetectable levels to a mean of 9.6% ± 0.8% in the inoculum virus and from 19.9% ± 0.9% to 29.1% ± 0.9% (P < 0.001) in the P2-oseltamivir/P1-oseltamivir 1 mg/kg virus. Interestingly, the deep-sequencing analysis revealed that the I222T substitution was already present in the initial inoculum (stock) virus, albeit at a low frequency (4.1%) that had no impact on the susceptibility to oseltamivir of the whole viral population, precluding its detection by the conventional sequencing methods. Finally, a positive selection of the N500D HA substitution was observed in the A/Victoria/3/75 virus (not shown), resulting in the loss of a potential N-linked glycosylation site. This mutation evolved in a passage-dependent yet drug-independent manner, increasing its frequency from 8.4% in the initial inoculum to 30.9%, 26.1%, and 35.5% on day 6 p.i. for the P2-untreated/P1-untreated, P2-oseltamivir/P1-oseltamivir 0.05 mg/kg, and P2-oseltamivir/P1-oseltamivir 1 mg/kg groups, respectively. The complete results with all minor NA and HA variants found by deep sequencing are presented in File S1 in the supplemental material.
FIG 1.
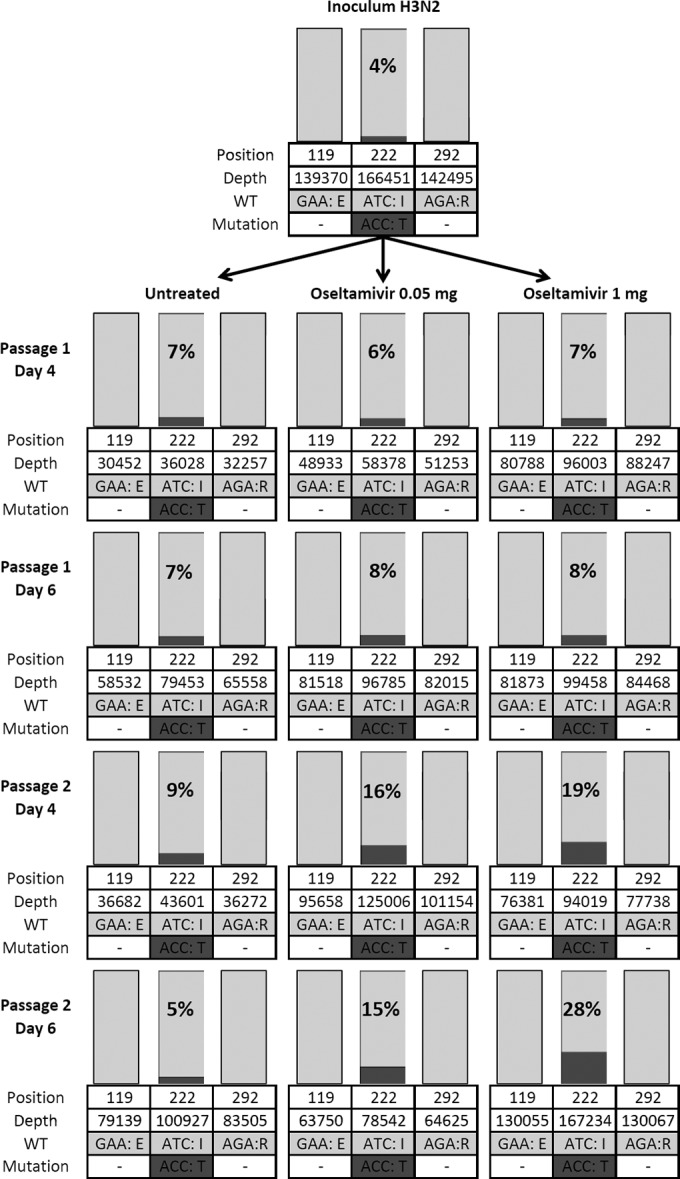
Longitudinal analysis of viral population diversity by deep sequencing. The ratios of major and minor codons are presented for the hallmark NA positions associated with resistance to oseltamivir in N2 viruses (E119 and R292) and for the residues with sustained significant (>1%) frequency of variation over time (I222). Codons and single-letter amino acid codes are indicated below the position numbers.
Susceptibility profiles of recombinant proteins.
To assess the effects of unknown NA mutations on oseltamivir susceptibility, the WT and mutant recombinant NA proteins were expressed and subjected to NA inhibition assays. While the oseltamivir susceptibility levels of recombinant A/WSN/33 F149S and D434V NA proteins were comparable to that of the WT (IC50s of 0.47 ± 0.05 nM, 0.41 ± 0.04 nM, and 0.48 ± 0.03 nM, respectively), the I222T A/Victoria/3/75 (H3N2) mutant protein showed a reduced inhibition phenotype, with a 16-fold increase in IC50 compared to that of the WT (4.69 ± 0.37 nM versus 0.29 ± 0.01 nM, respectively).
DISCUSSION
Development of resistance to oseltamivir, the most widely used NAI, remains an important concern, not only among immunocompromised patients (22, 23) but also in the general population. This is especially worrisome given the conserved viral fitness observed for the previously disseminated seasonal A/Brisbane/59/2007 (H1N1) H274Y variant (24, 25) as well as recent reports on community outbreaks of A(H1N1)pdm09 H274Y strains (26, 27). Moreover, resistance to oseltamivir conferred by the H274Y and N294S mutations as well as the R292K mutation has already been detected in patients infected with A(H5N1) strains and the novel A(H7N9) virus, respectively (28, 29). Previous studies demonstrated that NA mutations conferring resistance to oseltamivir in the clinical setting might be predicted to some extent by performance of in vitro serial passages of influenza viruses under oseltamivir pressure (3). However, very limited information is available on the selection of oseltamivir-resistant variants in mice and on the temporal evolution of viral quasi-species under selective NAI pressure.
In the present study, we selected two mouse-adapted influenza viruses, A/WSN/33 (H1N1) and A/Victoria/3/75 (H3N2), to perform two serial passages in mice receiving suboptimal doses of oseltamivir and analyzed the phenotypic and genotypic characteristics of the recovered viruses. Although no NA or HA substitutions associated with oseltamivir resistance were detected in the A/WSN/33 background, we observed a positive selection of the I222T NA substitution in the A/Victoria/3/75 virus. Indeed, this mutation was selected in a dose-dependent manner, increasing its frequency with in vivo passages, which also correlated with an increase in the T/I ratio during in vitro passages under oseltamivir pressure. Of interest, the T222 genotype was associated with a 16-fold increase in the oseltamivir IC50 level shown by the expressed recombinant mutant NA protein compared to that for the recombinant WT. This phenotype was not strain specific as the recombinant A/Hong Kong/1/68 (H3N2) NA protein harboring the I222T change also showed reduced susceptibility to oseltamivir (data not shown).
Many factors may account for our inability to select any mutations of resistance to oseltamivir in the A/WSN/33 background under the conditions used in our experimental design. The 2.7-fold maximum increase in oseltamivir IC50, along with the low NA activity of some recovered viruses and the significant reduction in lung viral titers (LVT) observed in both treated groups, suggests that the initial viral inoculum was too low, even if low-dose oseltamivir regimens were used (0.05 and 1 mg/kg/day compared to the more regular treatment of 20 mg/kg/day). As a result, the small amounts of the virus recovered on day 6 p.i. of the first passage led to a reduced viral inoculum for the second passage, thus enhancing the excessive pressure imposed by oseltamivir treatment. In that regard, a higher viral inoculum coupled to lower oseltamivir concentrations and/or increased serial passages would be interesting to test in future experiments. In addition, the late selection of two NA mutations (F149S and D434V) that do not affect susceptibility to oseltamivir is worth mentioning. Since both residues are located relatively far from the active site, they should not affect the enzymatic properties of NA, but recent reports of permissive mutations, at least in influenza viruses of the N1 subtype (24, 25, 30), warrant the need for experiments to assess their potential role in viral fitness.
The selection of the I222T NA substitution in the A/Victoria/3/75 (H3N2) virus is the major finding of our study. Amino acid I222 is a well-conserved framework residue among several influenza A subtypes and influenza B viruses (1). Together with W178, I222 forms a hydrophobic pocket within the NA active site in which lie the methyl groups of both the C4 acetamide of sialic acid and oseltamivir (31). Due to the interaction of I222 with the pentoxyl group of oseltamivir, several substitutions at the I222 residue have been identified in different influenza backgrounds both in vitro and in clinical studies (22, 32–34). Recently, the addition of the I222T mutation to the H274Y mutation in recombinant influenza A/California/04/2009 (H1N1)pdm09 viruses was shown to increase the oseltamivir IC50 from 574-fold in the single H274Y mutant to 1,377-fold in the double I222T/H274Y mutant, compared to that for the recombinant WT (35). In that case, the presence of a threonine at position 222 favored the formation of hydrogen bonds between this residue and its neighboring R152. As a result, R152 translocated to a position closer to T222, causing steric hindrance to the binding of the pentoxyl group of oseltamivir. Moreover, the single I222T mutant remained susceptible to oseltamivir (a 6.4-fold increase in the IC50 compared to that for the WT), and this variant produced viral titers comparable to those of the WT virus in replicative capacity experiments. Also, when introduced in the recombinant influenza B/Yamanashi/166/1998 background, the I222T NA mutation reduced susceptibility to oseltamivir and peramivir (13- and 15-fold increases in the IC50s, respectively, compared to that for the WT) (36) with no alteration of viral fitness in vitro. In line with the available data on the mild effect of the I222T NA mutation on oseltamivir susceptibility, the I222T variant described in the present study derived from an A/Victoria/3/75 (H3N2) NA protein conferred a reduced inhibition phenotype, with a 16-fold increase in the oseltamivir IC50. Furthermore, reports on the isolation of influenza B viruses harboring the I222T mutation from untreated patients indicate that this variant possibly occurs naturally without NAI selective pressure (37). These results are in agreement with previous reports suggesting that framework NA mutations decreasing susceptibility to NAIs generally do not alter the replicative capabilities (38). As a result, it is likely that the A/Victoria/3/75 (H3N2) I222T variant will retain viral fitness, yet this hypothesis and the potential contribution of the loss of an N-linked glycosylation site in the HA due to the N500D mutation on viral replication kinetics and antigenicity remain to be tested.
Our study also highlights the power of deep sequencing in terms of versatility and sensitivity for the detection of the expected as well as the unexpected minor variants within the viral population. In that regard, we were able to detect not only differences in the range of 1% in the time course population dynamics but also, importantly, the presence of a 4% oseltamivir-resistant variant in the initial inoculum, both of which would have remained undetected by Sanger sequencing approaches. We were not able to determine at what time the A/Victoria/3/75 (H3N2) virus acquired the I222T mutation, but its presence in the initial inoculum certainly biased its subsequent selection. As recently shown for the A(H1N1)pdm09 and A(H7N9) viruses, early detection of minor viral populations might be of major importance for the rapid and accurate implementation of antiviral therapy in some patients, since the resistance variant may be initially masked in the clinical samples containing mixed populations but rapidly favored and transmitted upon treatment (10, 39). In fact, we reported the rapid emergence of an oseltamivir-resistant variant in the household contact of an index patient infected with an oseltamivir-susceptible A(H1N1)pdm09 virus containing a minor subpopulation of ∼2% of the H274Y mutant, only detectable by deep sequencing (10). In this case, the rapid selection of the H274Y variant virus in the contact patient was favored by the use of a suboptimal (prophylactic) dose of oseltamivir.
In conclusion, the combination of serial in vivo passages under NAI pressure and the temporal deep-sequencing analysis used in this study has allowed the selection and identification of the I222T NA mutation in an influenza H3N2 virus, conferring reduced inhibition to oseltamivir. To our knowledge, this is the first report of this substitution in the N2 background, although the clinical significance of this mutation remains to be assessed. Additional in vivo selection experiments with other antivirals and/or drug combinations might provide important information on the evolution of antiviral resistance in influenza viruses, particularly in the case of new avian viruses infecting humans.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by grants from the Canadian Institutes of Health Research (229733 and 230187).
Guy Boivin is the holder of the Canada Research Chair on emerging viruses and antiviral resistance and is also the Canadian pandemic team leader on antiviral resistance and molecular evolution. Jacques Corbeil is the holder of the Canada Research Chair in medical genomics.
Footnotes
Published ahead of print 11 August 2014
Supplemental material for this article may be found at http://dx.doi.org/10.1128/AAC.02956-14.
REFERENCES
- 1.Colman PM, Hoyne PA, Lawrence MC. 1993. Sequence and structure alignment of paramyxovirus hemagglutinin-neuraminidase with influenza virus neuraminidase. J. Virol. 67:2972–2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tai CY, Escarpe PA, Sidwell RW, Williams MA, Lew W, Wu H, Kim CU, Mendel DB. 1998. Characterization of human influenza virus variants selected in vitro in the presence of the neuraminidase inhibitor GS 4071. Antimicrob. Agents Chemother. 42:3234–3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKimm-Breschkin JL. 2000. Resistance of influenza viruses to neuraminidase inhibitors—a review. Antiviral Res. 47:1–17. 10.1016/S0166-3542(00)00103-0. [DOI] [PubMed] [Google Scholar]
- 4.Gubareva LV. 2004. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 103:199–203. 10.1016/j.virusres.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 5.Kiso M, Mitamura K, Sakai-Tagawa Y, Shiraishi K, Kawakami C, Kimura K, Hayden FG, Sugaya N, Kawaoka Y. 2004. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 364:759–765. 10.1016/S0140-6736(04)16934-1. [DOI] [PubMed] [Google Scholar]
- 6.Sheu TG, Deyde VM, Okomo-Adhiambo M, Garten RJ, Xu X, Bright RA, Butler EN, Wallis TR, Klimov AI, Gubareva LV. 2008. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob. Agents Chemother. 52:3284–3292. 10.1128/AAC.00555-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abed Y, Bourgault AM, Fenton RJ, Morley PJ, Gower D, Owens IJ, Tisdale M, Boivin G. 2002. Characterization of 2 influenza A(H3N2) clinical isolates with reduced susceptibility to neuraminidase inhibitors due to mutations in the hemagglutinin gene. J. Infect. Dis. 186:1074–1080. 10.1086/344237. [DOI] [PubMed] [Google Scholar]
- 8.Mendel DB, Tai CY, Escarpe PA, Li W, Sidwell RW, Huffman JH, Sweet C, Jakeman KJ, Mersosn J, Lacy SA, Lew W, Williams MA, Zhang L, Chen MS, Bischofberger N, Kim CU. 1998. Oral administration of a prodrug of the influenza virus neuraminidase inhibitor GS 4071 protects mice and ferrets against influenza infection. Antimicrob. Agents Chemother. 42:640–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ison MG, Mishin VP, Braciale TJ, Hayden FG, Gubareva LV. 2006. Comparative activities of oseltamivir and A-322278 in immunocompetent and immunocompromised murine models of influenza virus infection. J. Infect. Dis. 193:765–772. 10.1086/500464. [DOI] [PubMed] [Google Scholar]
- 10.Ghedin E, Holmes EC, Depasse JV, Pinilla LT, Fitch A, Hamelin ME, Papenburg J, Boivin G. 2012. Presence of oseltamivir-resistant pandemic A/H1N1 minor variants before drug therapy with subsequent selection and transmission. J. Infect. Dis. 206:1504–1511. 10.1093/infdis/jis571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abed Y, Goyette N, Boivin G. 2004. A reverse genetics study of resistance to neuraminidase inhibitors in an influenza A/H1N1 virus. Antivir. Ther. 9:577–581. [PubMed] [Google Scholar]
- 12.Baz M, Abed Y, Papenburg J, Bouhy X, Hamelin ME, Boivin G. 2009. Emergence of oseltamivir-resistant pandemic H1N1 virus during prophylaxis. N. Engl. J. Med. 361:2296–2297. 10.1056/NEJMc0910060. [DOI] [PubMed] [Google Scholar]
- 13.Roussy JF, Abed Y, Bouhy X, Boivin G. 2013. Emergence of an oseltamivir-resistant influenza A/H3N2 virus in an elderly patient receiving a suboptimal dose of antiviral prophylaxis. J. Clin. Microbiol. 51:4234–4236. 10.1128/JCM.02659-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pizzorno A, Bouhy X, Abed Y, Boivin G. 2011. Generation and characterization of recombinant pandemic influenza A(H1N1) viruses resistant to neuraminidase inhibitors. J. Infect. Dis. 203:25–31. 10.1093/infdis/jiq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boisvert S, Laviolette F, Corbeil J. 2010. Ray: simultaneous assembly of reads from a mix of high-throughput sequencing technologies. J. Comput. Biol. 17:1519–1533. 10.1089/cmb.2009.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boisvert S, Raymond F, Godzaridis E, Laviolette F, Corbeil J. 2012. Ray Meta: scalable de novo metagenome assembly and profiling. Genome Biol. 13:R122. 10.1186/gb-2012-13-12-r122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C, Philippakis AA, del Angel G, Rivas MA, Hanna M, McKenna A, Fennell TJ, Kernytsky AM, Sivachenko AY, Cibulskis K, Gabriel SB, Altshuler D, Daly MJ. 2011. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat. Genet. 43:491–498. 10.1038/ng.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li H, Durbin R. 2009. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25:1754–1760. 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abed Y, Baz M, Boivin G. 2006. Impact of neuraminidase mutations conferring influenza resistance to neuraminidase inhibitors in the N1 and N2 genetic backgrounds. Antivir. Ther. 11:971–976. [PubMed] [Google Scholar]
- 20.Pizzorno A, Abed Y, Bouhy X, Beaulieu E, Mallett C, Russell R, Boivin G. 2012. Impact of mutations at residue I223 of the neuraminidase protein on the resistance profile, replication level, and virulence of the 2009 pandemic influenza virus. Antimicrob. Agents Chemother. 56:1208–1214. 10.1128/AAC.05994-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. 2012. Meetings of the WHO working group on surveillance of influenza antiviral susceptibility—Geneva, November 2011 and June 2012. Wkly. Epidemiol. Rec. 87:369–374. [PubMed] [Google Scholar]
- 22.Baz M, Abed Y, McDonald J, Boivin G. 2006. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin. Infect. Dis. 43:1555–1561. 10.1086/508777. [DOI] [PubMed] [Google Scholar]
- 23.Ison MG, Gubareva LV, Atmar RL, Treanor J, Hayden FG. 2006. Recovery of drug-resistant influenza virus from immunocompromised patients: a case series. J. Infect. Dis. 193:760–764. 10.1086/500465. [DOI] [PubMed] [Google Scholar]
- 24.Bloom JD, Gong LI, Baltimore D. 2010. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science 328:1272–1275. 10.1126/science.1187816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abed Y, Pizzorno A, Bouhy X, Boivin G. 2011. Role of permissive neuraminidase mutations in influenza A/Brisbane/59/2007-like (H1N1) viruses. PLoS Pathog. 7:e1002431. 10.1371/journal.ppat.1002431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hurt AC, Hardie K, Wilson NJ, Deng YM, Osbourn M, Gehrig N. 2011. Community transmission of oseltamivir-resistant A(H1N1)pdm09 influenza. N. Engl. J. Med. 365:2541–2542. 10.1056/NEJMc1111078. [DOI] [PubMed] [Google Scholar]
- 27.Meijer A, Jonges M, van Beek P, Swaan CM, Osterhaus AD, Daniels RS, Hurt AC, Koopmans MP. 2012. Oseltamivir-resistant influenza A(H1N1)pdm09 virus in Dutch travellers returning from Spain, August 2012. Euro Surveill. 17(36):pii=20266 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20266. [PubMed] [Google Scholar]
- 28.Le QM, Kiso M, Someya K, Sakai YT, Nguyen TH, Nguyen KH, Pham ND, Ngyen HH, Yamada S, Muramoto Y, Horimoto T, Takada A, Goto H, Suzuki T, Suzuki Y, Kawaoka Y. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. 10.1038/4371108a. [DOI] [PubMed] [Google Scholar]
- 29.Hu Y, Lu S, Song Z, Wang W, Hao P, Li J, Zhang X, Yen HL, Shi B, Li T, Guan W, Xu L, Liu Y, Wang S, Tian D, Zhu Z, He J, Huang K, Chen H, Zheng L, Li X, Ping J, Kang B, Xi X, Zha L, Li Y, Zhang Z, Peiris M, Yuan Z. 2013. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 381:2273–2279. 10.1016/S0140-6736(13)61125-3. [DOI] [PubMed] [Google Scholar]
- 30.Abed Y, Pizzorno A, Bouhy X, Rheaume C, Boivin G. 2014. Impact of potential permissive neuraminidase mutations on viral fitness of the H275Y oseltamivir-resistant influenza A(H1N1)pdm09 virus in vitro, in mice and in ferrets. J. Virol. 88:1652–1658. 10.1128/JVI.02681-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varghese JN, McKimm-Breschkin JL, Caldwell JB, Kortt AA, Colman PM. 1992. The structure of the complex between influenza virus neuraminidase and sialic acid, the viral receptor. Proteins 14:327–332. 10.1002/prot.340140302. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. 2009. Oseltamivir-resistant 2009 pandemic influenza A (H1N1) virus infection in two summer campers receiving prophylaxis–North Carolina, 2009. MMWR Morb. Mortal. Wkly. Rep. 58:969–972. [PubMed] [Google Scholar]
- 33.Nguyen HT, Fry AM, Loveless PA, Klimov AI, Gubareva LV. 2010. Recovery of a multidrug-resistant strain of pandemic influenza A 2009 (H1N1) virus carrying a dual H275Y/I223R mutation from a child after prolonged treatment with oseltamivir. Clin. Infect. Dis. 51:983–984. 10.1086/656439. [DOI] [PubMed] [Google Scholar]
- 34.van der Vries E, Veldhuis Kroeze EJ, Stittelaar KJ, Linster M, Van der Linden A, Schrauwen EJ, Leijten LM, van Amerongen G, Schutten M, Kuiken T, Osterhaus AD, Fouchier RA, Boucher CA, Herfst S. 2011. Multidrug resistant 2009 A/H1N1 influenza clinical isolate with a neuraminidase I223R mutation retains its virulence and transmissibility in ferrets. PLoS Pathog. 7:e1002276. 10.1371/journal.ppat.1002276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang L, Cao Y, Zhou J, Qin K, Zhu W, Zhu Y, Yang L, Wang D, Wei H, Shu Y. 2014. A conformational restriction in the influenza A virus neuraminidase binding site by R152 results in a combinational effect of I222T and H274Y on oseltamivir resistance. Antimicrob. Agents Chemother. 58:1639–1645. 10.1128/AAC.01848-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burnham AJ, Baranovich T, Marathe BM, Armstrong J, Webster RG, Govorkova EA. 2014. Fitness costs for influenza B viruses carrying neuraminidase inhibitor-resistant substitutions: underscoring the importance of E119A and H274Y. Antimicrob. Agents Chemother. 58:2718–2730. 10.1128/AAC.02628-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hatakeyama S, Sugaya N, Ito M, Yamazaki M, Ichikawa M, Kimura K, Kiso M, Shimizu H, Kawakami C, Koike K, Mitamura K, Kawaoka Y. 2007. Emergence of influenza B viruses with reduced sensitivity to neuraminidase inhibitors. JAMA 297:1435–1442. 10.1001/jama.297.13.1435. [DOI] [PubMed] [Google Scholar]
- 38.Samson M, Pizzorno A, Abed Y, Boivin G. 2013. Influenza virus resistance to neuraminidase inhibitors. Antiviral Res. 98:174–185. 10.1016/j.antiviral.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 39.Yen HL, McKimm-Breschkin JL, Choy KT, Wong DD, Cheung PP, Zhou J, Ng IH, Zhu H, Webby RJ, Guan Y, Webster RG, Peiris JS. 2013. Resistance to neuraminidase inhibitors conferred by an R292K mutation in a human influenza virus H7N9 isolate can be masked by a mixed R/K viral population. mBio 4(4):e00396-13. 10.1128/mBio.00396-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


