Abstract
Fluconazole is a first-line antifungal agent for the treatment and prophylaxis of invasive candidiasis in pediatric patients. Pediatric patients are at risk of suboptimal drug exposure, due to developmental changes in gastrointestinal and renal function, metabolic capacity, and volume of distribution. Therapeutic drug monitoring (TDM) can therefore be useful to prevent underexposure of fluconazole in children and infants. Children, however, often fear needles and can have difficult vascular access. The purpose of this study was to develop and clinically validate a method of analysis to determine fluconazole in oral fluid in pediatric patients. Twenty-one paired serum and oral fluid samples were obtained from 19 patients and were analyzed using a validated liquid chromatography-tandem mass spectrometry (LC–MS-MS) method after cross-validation between serum and oral fluid. The results were within accepted ranges for accuracy and precision, and samples were stable at room temperature for at least 17 days. A Pearson correlation test for the fluconazole concentrations in serum and oral fluid showed a correlation coefficient of 0.960 (P < 0.01). The mean oral fluid-to-serum concentration ratio was 0.99 (95% confidence interval [CI], 0.88 to 1.10) with Bland-Altman analysis. In conclusion, an oral fluid method of analysis was successfully developed and clinically validated for fluconazole in pediatric patients and can be a noninvasive, painless alternative to perform TDM of fluconazole when blood sampling is not possible or desirable. When patients receive prolonged courses of antifungal treatment and use fluconazole at home, this method of analysis can extend the possibilities of TDM for patients at home.
INTRODUCTION
Fluconazole was introduced in 1990 and is still a first-line antifungal agent for the treatment and prophylaxis of invasive candidiasis in children and infants (1, 2). The bioavailability of orally administered fluconazole is over 90%, and fluconazole has excellent penetration in tissue and body fluids (3, 4). The pharmacokinetic/pharmacodynamic parameter that best predicts the outcome of the fluconazole treatment is the area under the concentration-time curve over 24 h in steady state divided by the MIC (AUC/MIC) (5, 6). To ensure an AUC/MIC of ≥50, which corresponds to a favorable outcome, an AUC of ≥400 mg · h/liter is required for Candida species with a MIC breakpoint of ≤8 mg/liter (7–10). Routine therapeutic drug monitoring (TDM) of fluconazole is currently not advised due to its high bioavailability, linear dose-concentration relationship, and good safety profile (1, 11, 12). However, children and infants are at risk of suboptimal drug exposure, due to developmental changes in the gastrointestinal and renal function, metabolic capacity, and volume of distribution (13). A previous study showed that the serum fluconazole concentration was correlated with the age, weight, and renal function of critically ill pediatric patients and that the fluconazole exposure was not sufficient in pediatric cancer patients (14). TDM of fluconazole can therefore be useful to prevent possible underexposure in critically ill pediatric patients (14, 15). Since obtaining a blood sample from children is often more complicated than for adults and children often fear needles, oral fluid sampling can be a noninvasive, painless alternative to plasma or serum (16). Previous studies showed a mean ratio of the saliva drug concentration to the plasma drug concentration of approximately 1 for fluconazole in healthy volunteers (3, 17, 18). However, in another study, a saliva-to-plasma concentration ratio of 0.4 was found (19). A median saliva-to-plasma ratio of 1.1 to 1.3 was seen in adult patients with HIV or AIDS (20, 21) and a mean ratio of 1.4 in adult cancer patients who underwent radiotherapy (22). The correlation between fluconazole in oral fluid and in plasma or serum has not yet been studied in children. The purpose of this study was to develop and clinically validate a method of analysis of fluconazole in oral fluid in hospitalized children with an (invasive) Candida infection and to evaluate the fluconazole exposure in these children.
MATERIALS AND METHODS
Study design.
This prospective observational study was conducted in the 150-bed pediatric department of the University Medical Center Groningen, Groningen, The Netherlands, from July 2007 to March 2014. Patients were eligible for inclusion if the following criteria were met: (i) age, 0 to 18 years; (ii) admission to a pediatric ward or pediatric/neonatal intensive care unit (ICU); (iii) oral or intravenous treatment with fluconazole; and (iv) scheduled routine TDM of fluconazole in serum. Children from whom it was impossible to get oral fluid or who had serious mucositis of their oral cavity or oral thrush were excluded from the study. The study protocol was approved by the local medical ethics committee (institutional review board protocol no. 2007.198). For patients less than 12 years of age, written informed consent was given by the parents, and for patients over 12 years of age, the patient and parents were both asked to give informed consent. The study population was also included in a retrospective study of fluconazole exposure by van der Elst et al. (14).
Routine serum and oral fluid trough samples were obtained pairwise before administration of fluconazole. Fluconazole samples were eligible for evaluation when obtained at steady state, which is after 2 days when a loading dose has been given or after 5 days without a loading dose (10, 23). Serum was obtained by centrifuging the blood samples, and the serum was directly analyzed or stored at −20°C until analysis. Only the unbound fraction of fluconazole is present in oral fluid. Since the protein binding of fluconazole is only 11 to 12% (18, 20), the total fluconazole concentration was determined in serum. Oral fluid samples were obtained by chewing/sucking for 1 min on a small cotton roll (Salivette, without preparation; Sarstedt, Leicester, United Kingdom). If the patient was unable to chew, the oral fluid samples were obtained through suction of the oral fluid with a routine suction device. Oral fluid samples were directly centrifuged and stored at −20°C until analysis. Demographic and clinical data were collected through review of the medical records and included age, sex, weight, renal function (serum urea and serum creatinine concentration), underlying condition, stay in an ICU, and the Candida species. Medical data were collected on the fluconazole dose (mg/kg of body weight/day) and route of administration, fluconazole trough concentration, and duration of treatment.
Oral fluid method validation.
Fluconazole serum and oral fluid samples were analyzed using a previously validated liquid chromatography-tandem mass spectrometry (LC–MS-MS) method (24). The analytical method was validated in accordance with the Guidance for Industry, Bioanalytical Method Validation of the Food and Drug Administration (25). Cross-validation between serum and oral fluid was performed by comparing calibration samples of pooled serum and pooled oral fluid. The lower limit of quantification (LOQ) was 0.5 μg/ml for both the serum and oral fluid assays. The linearity of the standard curve was assessed with 1/x2 weighting over a concentration range of 0.5 to 50.0 μg/ml. Accuracy and precision were evaluated for quality control samples at concentrations of 0.5, 1.0, 2.5, 5.0, 10.0, 20.0, 40.0, and 50.0 μg/ml in triplicate. Stability was assessed by storing oral fluid samples with fluconazole concentrations of 1.0 μg/ml (low), 20.0 μg/ml (medium), and 40.0 μg/ml (high) at room temperature (20°C) for 1, 3, 5, and 17 days. For the determination of the recovery of fluconazole from the cotton rolls, 1.5 ml spiked oral fluid at low, medium, and high concentrations was applied to the Salivette. Afterwards, the Salivettes were centrifuged, and the extracts were compared to blank oral fluid subsequently spiked at low, medium, and high concentrations. The recovery was determined immediately after preparation of the Salivettes and after storing the Salivettes for 2 and 6 days at room temperature (20°C). The analysis was clinically validated by comparing the fluconazole concentrations in paired serum and oral fluid samples from patients. Furthermore, the percentage of patients with a fluconazole trough concentration of <11 μg/ml (10, 14, 23) was determined.
Statistical analysis.
In the analytical method validation, bias was defined as the difference between the analytical result and the nominal concentration, expressed as a percentage. The oral fluid analysis was validated by comparing the serum fluconazole concentration with the concentration of fluconazole in oral fluid using Passing-Bablok regression and Bland-Altman analysis (with Analyze-it 2.20 software). Furthermore, a Pearson correlation coefficient was calculated to determine the correlation between the concentrations in serum and oral fluid. Additionally, a leave-one-out cross-validation was performed to validate the predictive performance of a linear regression model used to predict serum concentrations based on oral fluid concentrations. In this model, the serum fluconazole concentration was set as the dependent variable and the oral fluid fluconazole concentration as the independent variable. The model was refitted n times (with n the total number of observations) while leaving out a single observation t, so that a prediction could be derived for the left-out observation based on all other observations. The error for observation t was then defined as the difference between the observed and predicted serum fluconazole concentrations, as follows: . In order to determine the performance of the linear regression model, the root mean square error (RMSE) was calculated using the following equation: .
In regard to patients, values are expressed as medians with interquartile range (IQR) for continuous variables and as percentages of the group from which they were derived for categorical variables. A Spearman correlation coefficient was calculated to determine correlations between two continuous variables. To compare two groups, the Mann-Whitney U test was used. Statistical analyses were performed using SPSS for Windows, version 20.0 (IBM SPSS, Chicago, IL). A P value of <0.05 was considered statistically significant.
RESULTS
A total of 19 patients were included in the study, and their medical records were reviewed. The mean age of the patients was 4.6 years (range, 22 days to 16 years), and 9 patients (47.4%) were male. The patients' characteristics are summarized in Table 1. The causative pathogen was Candida albicans in 16 patients (84.2%), C. parapsilosis in 1 patient (5.3%), C. krusei in 1 patient (5.3%), and not specified in 1 patient (5.3%). The median fluconazole dose was 9.4 mg/kg/day (IQR, 6.4 to 10.4 mg/kg/day), and the median duration of the fluconazole treatment was 31 days (IQR, 18 to 61 days). Thirteen patients (68.4%) received fluconazole intravenously, and 6 patients (31.6%) received oral treatment. The fluconazole serum trough concentrations ranged from 2.8 to 37.5 μg/ml.
TABLE 1.
Characteristics of 19 children and infants receiving fluconazole
| Characteristic | No. (%) of patients |
|---|---|
| Gender (male) | 9 (47.4) |
| Age | |
| 0–1 mo | 2 (10.5) |
| 1–24 mo | 8 (42.1) |
| 2–12 yr | 6 (31.6) |
| 12–18 yr | 3 (15.8) |
| Underlying condition | |
| Solid organ transplantation | 2 (10.5) |
| Cancer | 5 (26.3) |
| Surgery | 7 (36.8) |
| Prematurity | 2 (10.5) |
| Othera | 3 (15.8) |
| Stay in intensive care unit | 11 (57.9) |
Other: 1 patient was diagnosed with cardiac and respiratory insufficiency, 1 patient with liver failure, and 1 patient with spina bifida.
Analytical method validation.
The serum and oral fluid analytical method showed good linearity over the fluconazole concentration range. The regression equations and correlation coefficients were as follows: 0.00195 + 0.0274 × response and r2 = 0.998 for serum and −0.000461 + 0.0265 × response and r2 = 0.997 for oral fluid. The mean measured concentrations were between 93.8% and 102.7% of the nominal concentration for serum and between 96.6% and 107.4% for oral fluid. The calibration curves were analyzed in triplicate, with the coefficients of variation between 1.2% and 5.9% for serum and between 1.4% and 5.4% for oral fluid, well within the required limit of <15% for the whole concentration range. Serum samples were stable at room temperature (20°C) for 7 days, with a bias of 2.3% for the low, 7.6% for the medium, and 5.6% for the high concentrations (24). Oral fluid samples were stable at room temperature (20°C) for 1, 3, 5, and 17 days, with a bias of 3.5% to 12.9% for the low, 2.8% to 6.1% for the medium, and −0.6% to 5.7% for the high concentrations. The recovery of the fluconazole extraction from the cotton rolls was between 93.5% and 97.8% for the freshly prepared Salivettes and between 97.3% and 104.8% after storing the Salivettes at room temperature (20°C) for 2 and 6 days and was well within the required limit of <15%.
Clinical validation.
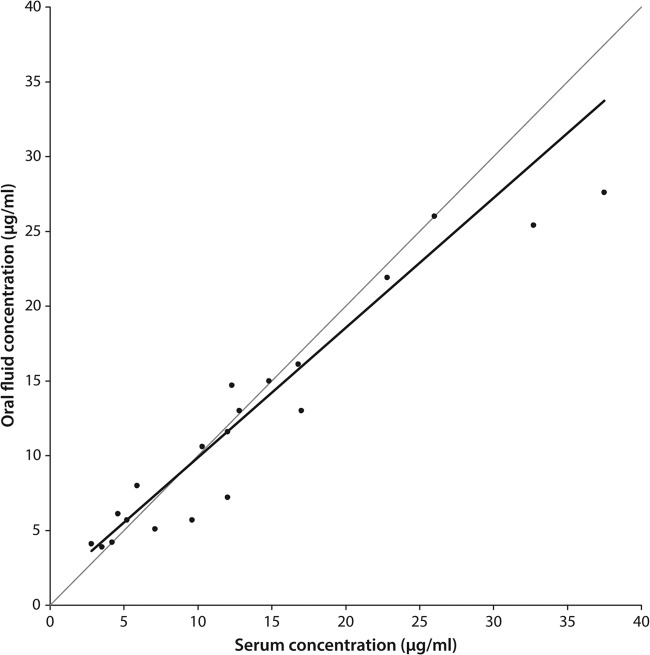
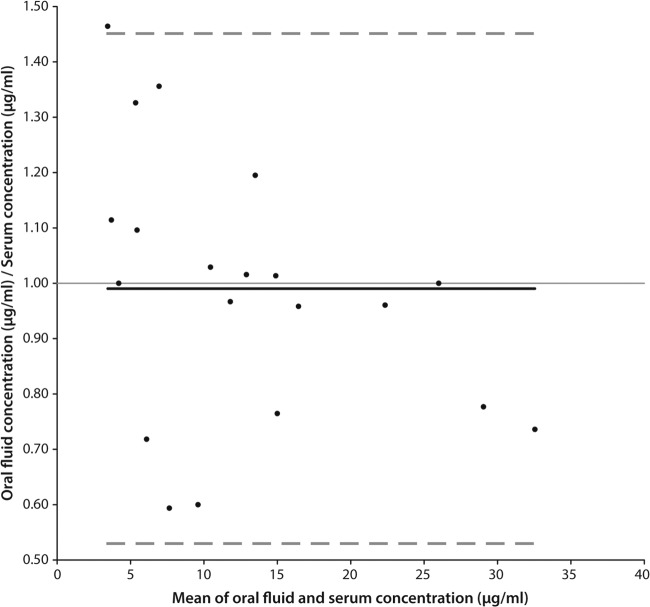
Twenty-one paired serum and oral fluid samples from 19 patients were included in the clinical validation of the oral fluid analysis. A Pearson correlation test showed a correlation coefficient of 0.960 (P < 0.01) for the fluconazole concentrations in serum and oral fluid. The unadjusted median of the oral fluid-to-serum ratio was 1.00 (range, 0.59 to 1.46). Passing-Bablok regression between the serum and oral fluid drug concentrations showed a proportional bias of 0.87 (95% confidence interval [CI], 0.69 to 0.98) and a constant bias of 1.19 (95% CI, 0.44 to 2.92) (Fig. 1). With Bland-Altman analysis, the mean oral fluid-to-serum drug concentration ratio versus the mean concentration in oral fluid and serum was 0.99 (95% CI, 0.88 to 1.10). Twenty out of 21 values were within the limits of agreement of 95% (Fig. 2). Using a leave-one-out cross-validation analysis, the standard deviation of the error in the predictive linear regression model was found to be 3.1 μg/ml. The oral fluid-to-serum drug concentration ratio did not significantly differ in patients receiving oral treatment versus intravenous treatment (P = 0.791). No significant correlation was found between the oral fluid-to-serum drug concentration ratio and the age (P = 0.316) or weight (P = 0.266) of the patient, the renal function (P = 0.743 for urea and P = 0.186 for the creatinine concentration), or the fluconazole dose (P = 0.636). Ten patients (52.6%) had a serum fluconazole concentration of <11 μg/ml, which is considered representative of an AUC of <400 mg · h/liter (10, 14, 23).
FIG 1.
Scatter plot (n = 21) with Passing-Bablok regression between serum and oral fluid concentrations. The regression line of fluconazole is presented as a solid line and has a slope of 0.87 (95% CI, 0.69 to 0.98) and an intercept of 1.19 (95% CI, 0.44 to 2.92).
FIG 2.
Bland-Altman plot of the oral fluid-to-serum drug concentration ratio versus the mean concentration in oral fluid and serum. The bias is presented as a solid line, and the 95% limits of agreement are presented as dashed lines. The mean bias is 0.99 (95% CI, 0.88 to 1.10), and the lower and upper 95% limits of agreement are 0.53 (95% CI, 0.34 to 0.72) and 1.45 (95% CI, 1.27 to 1.64), respectively.
DISCUSSION
An oral fluid analysis for fluconazole was developed and clinically validated in pediatric patients. The fluconazole concentration in oral fluid was in good agreement with the serum fluconazole concentration. The mean oral fluid-to-serum drug concentration ratio was 1, which corresponds to the ratio of 1 reported in the summary of product characteristics of fluconazole (18) and in studies in healthy volunteers (3, 17). Fluconazole has a low protein binding of 11% to 12% and is largely nonionized under physiological conditions, which makes fluconazole easily penetrate in oral fluid (18, 20). In the high-concentration area (>30 μg/ml), the concentration in oral fluid was lower than the concentration in serum, which possibly indicates saturation of the amount of fluconazole in the oral fluid. It is possible that fluconazole is excreted in oral fluid, not only by passive diffusion, but also by an active transport mechanism (20). However, there were only 2 patients with a serum trough concentration of >30 μg/ml, and previous reports studied fluconazole trough concentrations only up to 10 μg/ml (17, 19, 20, 22, 26).
The overall bias between the fluconazole concentrations in oral fluid and serum found with Bland-Altman analysis was low. However, in the low-concentration area, a larger bias was seen in the oral fluid-to-serum ratio with Bland-Altman analysis. Furthermore, the standard deviation of the error in the predictive linear regression model was 3.1 μg/ml. When increasing the fluconazole dose in case of underexposure based on the oral fluid drug concentration, this standard deviation must be taken into account, especially when the measured concentration is ranged around the target concentration. A slightly higher fluconazole trough concentration can be pursued to ensure the exposure is adequate. This higher fluconazole concentration is not likely to cause adverse drug reactions, since fluconazole has a good safety profile and is well tolerated in pediatric patients at higher doses (12). In case the MIC for the Candida species is known, the fluconazole dose can be adjusted to achieve the required exposure and to prevent unnecessary dose increase. TDM of fluconazole revealed a fluconazole trough concentration of <11 μg/ml in 52.6% of the pediatric patients. Hence, TDM of fluconazole can be useful to detect possible underexposure in children and infants.
In our hospital, only trough concentrations of fluconazole were measured and included in the clinical validation. The oral fluid-to-serum concentration ratio of 1 that was found in this study can therefore be applied only to fluconazole trough concentrations. A trough concentration is probably most convenient to obtain and will give no drug contamination when fluconazole is administered orally. Furthermore, oral fluid was collected by chewing/sucking on a small cotton roll (Salivette) or by a routine suction device when the patient was not able to chew. Collection devices other than the Salivette have not been clinically validated in our study. Research has shown that Salivette collection devices achieve good recovery for most drugs, and they were found to be very practical and convenient for the user (27). In contrast with full-term infants, the collection of oral fluid from premature neonates was difficult, since these patients produce very little oral fluid. Oral fluid sampling is therefore not suitable for premature neonates. In some other cases, blood sampling may also be preferred over oral fluid sampling, for example, when other laboratory tests are ordered along with the fluconazole measurement. Furthermore, in patients with severe mucositis or other damage to or inflammation of the oral mucosa/salivary glands and in patients where oral fluid production is reduced (e.g., when treated with anticholinergic comedication), blood sampling is preferred (16).
Based on the results of our study, TDM of fluconazole in oral fluid can be a noninvasive, painless alternative to serum in children who fear needles or who have difficult vascular access. Oral fluid sampling is preferred over blood sampling by the majority of patients and their parents (16). Besides, oral fluid sampling can reduce costs due to the lower level of training of personnel, less time needed for oral fluid sampling, and lower costs of materials used for oral fluid sampling (16). When patients receive prolonged courses of antifungal treatment and use fluconazole at home, oral fluid sampling by the parents or the patient can extend the possibilities of TDM for patients at home. Samples do not have to be obtained solely during office hours and can be shipped by mail, thereby avoiding trips to the hospital, and the biohazard risk when shipping oral fluid samples is low. Furthermore, the physician already has the results of the analysis before the consultation or can give advice to adjust the dose over the telephone.
In conclusion, an oral fluid method of analysis was successfully developed and clinically validated for fluconazole in hospitalized children and infants and can be a noninvasive, painless alternative to perform TDM of fluconazole when blood sampling is not possible or desirable.
Footnotes
Published ahead of print 2 September 2014
REFERENCES
- 1.Pappas PG, Kauffman CA, Andes D, Benjamin DK, Jr, Calandra TF, Edwards JE, Jr, Filler SG, Fisher JF, Kullberg BJ, Ostrosky-Zeichner L, Reboli AC, Rex JH, Walsh TJ, Sobel JD, Infectious Diseases Society of America 2009. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 48:503–535. 10.1086/596757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hope WW, Castagnola E, Groll AH, Roilides E, Akova M, Arendrup MC, Arikan-Akdagli S, Bassetti M, Bille J, Cornely OA, Cuenca-Estrella M, Donnelly JP, Garbino J, Herbrecht R, Jensen HE, Kullberg BJ, Lass-Florl C, Lortholary O, Meersseman W, Petrikkos G, Richardson MD, Verweij PE, Viscoli C, Ullmann AJ, Fungal Infection Study Group ESCMID 2012. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: prevention and management of invasive infections in neonates and children caused by Candida spp. Clin. Microbiol. Infect. 18(Suppl 7):38–52. 10.1111/1469-0691.12040. [DOI] [PubMed] [Google Scholar]
- 3.Brammer KW, Farrow PR, Faulkner JK. 1990. Pharmacokinetics and tissue penetration of fluconazole in humans. Rev. Infect. Dis. 12(Suppl 3):S318–S326. 10.1093/clinids/12.Supplement_3.S318. [DOI] [PubMed] [Google Scholar]
- 4.Charlier C, Hart E, Lefort A, Ribaud P, Dromer F, Denning DW, Lortholary O. 2006. Fluconazole for the management of invasive candidiasis: where do we stand after 15 years? J. Antimicrob. Chemother. 57:384–410. 10.1093/jac/dki473. [DOI] [PubMed] [Google Scholar]
- 5.Andes D, van Ogtrop M. 1999. Characterization and quantitation of the pharmacodynamics of fluconazole in a neutropenic murine disseminated candidiasis infection model. Antimicrob. Agents Chemother. 43:2116–2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Louie A, Drusano GL, Banerjee P, Liu QF, Liu W, Kaw P, Shayegani M, Taber H, Miller MH. 1998. Pharmacodynamics of fluconazole in a murine model of systemic candidiasis. Antimicrob. Agents Chemother. 42:1105–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clancy CJ, Yu VL, Morris AJ, Snydman DR, Nguyen MH. 2005. Fluconazole MIC and the fluconazole dose/MIC ratio correlate with therapeutic response among patients with candidemia. Antimicrob. Agents Chemother. 49:3171–3177. 10.1128/AAC.49.8.3171-3177.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pfaller MA, Diekema DJ, Sheehan DJ. 2006. Interpretive breakpoints for fluconazole and Candida revisited: a blueprint for the future of antifungal susceptibility testing. Clin. Microbiol. Rev. 19:435–447. 10.1128/CMR.19.2.435-447.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piper L, Smith PB, Hornik CP, Cheifetz IM, Barrett JS, Moorthy G, Hope WW, Wade KC, Cohen-Wolkowiez M, Jr, Benjamin DK. 2011. Fluconazole loading dose pharmacokinetics and safety in infants. Pediatr. Infect. Dis. J. 30:375–378. 10.1097/INF.0b013e318202cbb3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wade KC, Benjamin DK, Jr, Kaufman DA, Ward RM, Smith PB, Jayaraman B, Adamson PC, Gastonguay MR, Barrett JS. 2009. Fluconazole dosing for the prevention or treatment of invasive candidiasis in young infants. Pediatr. Infect. Dis. J. 28:717–723. 10.1097/INF.0b013e31819f1f50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andes D, Pascual A, Marchetti O. 2009. Antifungal therapeutic drug monitoring: established and emerging indications. Antimicrob. Agents Chemother. 53:24–34. 10.1128/AAC.00705-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Novelli V, Holzel H. 1999. Safety and tolerability of fluconazole in children. Antimicrob. Agents Chemother. 43:1955–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE. 2003. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N. Engl. J. Med. 349:1157–1167. 10.1056/NEJMra035092. [DOI] [PubMed] [Google Scholar]
- 14.van der Elst KCM, Pereboom M, van den Heuvel ER, Kosterink JGW, Schölvinck EH, Alffenaar JWC. 22 August 2014. Insufficient fluconazole exposure in pediatric cancer patients and the need for therapeutic drug monitoring in critically ill children. Clin. Infect. Dis. 10.1093/cid/ciu657. [DOI] [PubMed] [Google Scholar]
- 15.Hope WW, Billaud EM, Lestner J, Denning DW. 2008. Therapeutic drug monitoring for triazoles. Curr. Opin. Infect. Dis. 21:580–586. 10.1097/QCO.0b013e3283184611. [DOI] [PubMed] [Google Scholar]
- 16.Gorodischer R, Burtin P, Hwang P, Levine M, Koren G. 1994. Saliva versus blood sampling for therapeutic drug monitoring in children: patient and parental preferences and an economic analysis. Ther. Drug Monit. 16:437–443. 10.1097/00007691-199410000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Koks CH, Meenhorst PL, Hillebrand MJ, Bult A, Beijnen JH. 1996. Pharmacokinetics of fluconazole in saliva and plasma after administration of an oral suspension and capsules. Antimicrob. Agents Chemother. 40:1935–1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pfizer. 2010. Diflucan. Summary of product characteristics. Pfizer, New York, NY. [Google Scholar]
- 19.Force RW, Nahata MC. 1995. Salivary concentrations of ketoconazole and fluconazole: implications for drug efficacy in oropharyngeal and esophageal candidiasis. Ann. Pharmacother. 29:10–15. [DOI] [PubMed] [Google Scholar]
- 20.Koks CH, Crommentuyn KM, Hoetelmans RM, Mathot RA, Beijnen JH. 2001. Can fluconazole concentrations in saliva be used for therapeutic drug monitoring? Ther. Drug Monit. 23:449–453. 10.1097/00007691-200108000-00022. [DOI] [PubMed] [Google Scholar]
- 21.Garcia-Hermoso D, Dromer F, Improvisi L, Provost F, Dupont B. 1995. Fluconazole concentrations in saliva from AIDS patients with oropharyngeal candidosis refractory to treatment with fluconazole. Antimicrob. Agents Chemother. 39:656–660. 10.1128/AAC.39.3.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oliary J, Tod M, Louchahi K, Petitjean O, Frachet B, Le Gros V, Brion N. 1993. Influence of local radiotherapy on penetration of fluconazole into human saliva. Antimicrob. Agents Chemother. 37:2674–2677. 10.1128/AAC.37.12.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JW, Seibel NL, Amantea M, Whitcomb P, Pizzo PA, Walsh TJ. 1992. Safety and pharmacokinetics of fluconazole in children with neoplastic diseases. J. Pediatr. 120:987–993. 10.1016/S0022-3476(05)81975-4. [DOI] [PubMed] [Google Scholar]
- 24.Alffenaar JW, Wessels AM, van Hateren K, Greijdanus B, Kosterink JG, Uges DR. 2010. Method for therapeutic drug monitoring of azole antifungal drugs in human serum using LC/MS/MS. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 878:39–44. 10.1016/j.jchromb.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 25.Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Veterinary Medicine. 2001. Guidance for industry. Bioanalytical method validation. Food and Drug Administration, Washington, DC. [Google Scholar]
- 26.Wildfeuer A, Laufen H, Yeates RA, Zimmermann T. 1996. A new pharmaceutical concept for the treatment of oropharyngeal and oesophageal candidosis with fluconazole. Mycoses 39:357–360. 10.1111/j.1439-0507.1996.tb00153.x. [DOI] [PubMed] [Google Scholar]
- 27.Groschl M, Kohler H, Topf HG, Rupprecht T, Rauh M. 2008. Evaluation of saliva collection devices for the analysis of steroids, peptides and therapeutic drugs. J. Pharm. Biomed. Anal. 47:478–486. 10.1016/j.jpba.2008.01.033. [DOI] [PubMed] [Google Scholar]