The use of contact isolation precautions for patients colonized or infected with drug-resistant or easily transmissible organisms is a widely accepted strategy for reducing transmission of hospital-associated infections. Although hospitals throughout the country have implemented these practices at great logistical and financial expense, there is little high quality data to support their use.
Isolation precautions have unintended consequences, including a reduction in time spent with health care providers, lower patient satisfaction and more preventable adverse events (1–3). Only a few small studies have measured the impact of contact isolation on time spent by health care providers with patients. Given recent advances in spatial tracking technology, we set out to measure differences in time spent by internal medicine interns in contact isolation compared to non-isolation rooms.
Methods
Using tracking devices attached to hospital identification badges, we collected real-time data on the location of 15 internal medicine interns working in our hospital between October 1, 2012 and December 31, 2012. The devices work by emitting RFID signals to a network of receivers located throughout our hospital. Based on the strength of the signal relative to the receivers, the location of the asset can be mapped to within a 5-foot radius.
For each intern, the tracking system recorded exact start and end times for each specific location they entered in the hospital. By combining this data with data on the isolation status of each room on a ward where all patients have individual rooms, we were able to compare time spent in isolation versus non-isolation rooms. New patient admissions typically occur in the Emergency Department and therefore the encounters on the selected ward were primarily patient follow up visits. SAS version 9.3 was used to create a mixed model, and individual interns were used as random effects in the model.
Results
There were 1,156 encounters with isolated patients and 2,467 encounters with non-isolated patients over three months of continuous observation. Interns visited isolated patients less often (2.3 compared to 2.5 visits per day, P<0.0001) and spent less time per visit with isolated patients (2.2 compared to 2.8 minutes per visit, P<0001). Thus, on average, interns spent 5.2 minutes per day with each of their isolated patients compared to 6.9 minutes per day with each of their non-isolated patients (P<0.0001).
Discussion
We were surprised to discover that interns spend little time in direct contact with their patients, and even less time with those patients on contact isolation precautions. Interestingly, in the most recent time-motion study of intern work flow, Block et al. found that interns spent an average of 7.7 minutes per follow up visit per day, which is comparable to our average of 7 minutes per patient per day for non-isolation patients (4). Nevertheless, the fact that trainees spend less time with isolated patients might explain why these patients experience more adverse events and have lower overall satisfaction (3,5), particularly if senior residents and attending physicians exhibit the same behavior.
Our results support a growing body of literature suggesting that contact precautions may impede patient care. Infection prevention strategies that minimize the barrier between physicians and patients, including hand hygiene, antimicrobial stewardship, and, as has recently been suggested, universal decolonization (6) should continue to be investigated, as these methods may be more effective at reducing the spread of resistant organisms and less disruptive to patients. Further research is needed, both to better define the patient population for whom the benefits of contact isolation outweigh the risks and to develop strategies to ameliorate those risks for those who must be placed into isolation.
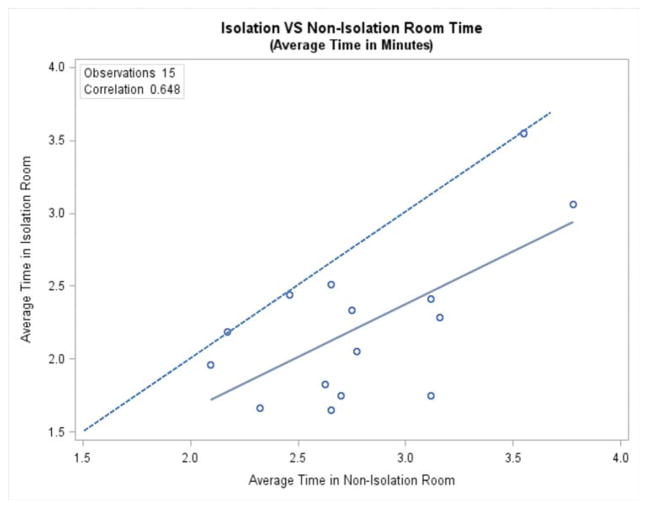
Figure 1. Average time per visit to isolation versus non-isolation rooms.
Each data point represents one intern. Dashed line shows where values would be if time in isolation and non-isolation rooms were equal. Solid line shows the least-squares regression for the relationship between isolation room and non-isolation room time among interns (r=0.65).
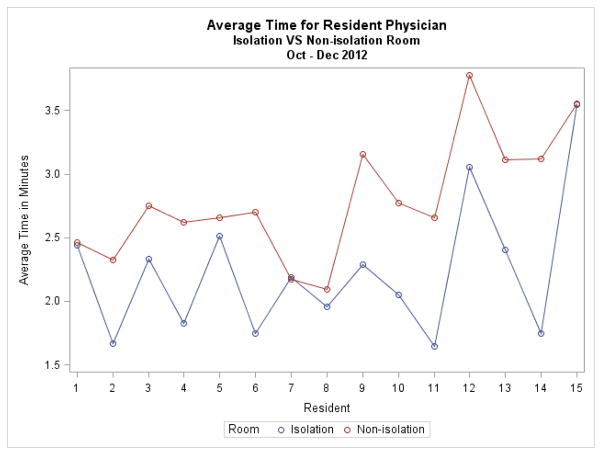
Figure 2. Average time spent by each intern per visit to isolation compared to non-isolation rooms.
Red line shows time per visit to non-isolation rooms. Blue line shows time per visit to isolation rooms.
Table 1.
Mean time spent per visit by each intern to isolation versus non-isolation rooms
| Contact Isolation Rooms | Non-Contact Isolation Rooms | |||
|---|---|---|---|---|
|
| ||||
| Intern ID | Number of encounters | Mean minutes per encounter (+/− SD) | Number of encounters | Mean minutes per encounter (+/− SD) |
| 1 | 70 | 2.44 (1.93) | 50 | 2.46 (1.97) |
| 2 | 90 | 1.67 (0.94) | 230 | 2.32 (1.98) |
| 3 | 150 | 2.33 (1.98) | 187 | 2.75 (3.23) |
| 4 | 116 | 1.83 (2.16) | 240 | 2.63 (2.52) |
| 5 | 51 | 2.51 (2.65) | 188 | 2.65 (3.17) |
| 6 | 52 | 1.75 (1.05) | 77 | 2.7 (1.95) |
| 7 | 81 | 2.19 (1.78) | 180 | 2.17 (1.88) |
| 8 | 92 | 1.96 (1.5) | 180 | 2.09 (1.69) |
| 9 | 146 | 2.29 (2.2) | 132 | 3.16 (3.45) |
| 10 | 59 | 2.05 (1.71) | 220 | 2.77 (2.64) |
| 11 | 17 | 1.65 (0.86) | 87 | 2.66 (2.14) |
| 12 | 35 | 3.06 (2.86) | 104 | 3.78 (5.02) |
| 13 | 49 | 2.41 (2.98) | 181 | 3.12 (3.34) |
| 14 | 68 | 1.75 (1.38) | 282 | 3.12 (2.86) |
| 15 | 80 | 3.55 (3.7) | 129 | 3.55 (3.97) |
Acknowledgments
We would like to thank Carlene Anteau and Bianca Christenson of Awarepoint Corporation for donating the RFID tags and for their technical support.
References
- 1.Aboelela SW, Saiman L, Stone P, Lowy FD, Quiros D, Larson E. Effectiveness of barrier precautions and surveillance cultures to control transmission of multidrug-resistant organisms: a systematic review of the literature. Am J Infect Control. 2006 Oct;34(8):484–94. doi: 10.1016/j.ajic.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al. Isolation measures in the hospital management of methicillin resistant Staphylococcus aureus (MRSA): systematic review of the literature. BMJ. 2004 Sep 4;329(7465):533. doi: 10.1136/bmj.329.7465.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA J Am Med Assoc. 2003 Oct 8;290(14):1899–905. doi: 10.1001/jama.290.14.1899. [DOI] [PubMed] [Google Scholar]
- 4.Block L, Habicht R, Wu AW, Desai SV, Wang K, Silva KN, et al. In the wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med. 2013 Aug;28(8):1042–7. doi: 10.1007/s11606-013-2376-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehrotra P, Croft L, Day HR, Perencevich EN, Pineles L, Harris AD, et al. Effects of contact precautions on patient perception of care and satisfaction: a prospective cohort study. Infect Control Hosp Epidemiol Off J Soc Hosp Epidemiol Am. 2013 Oct;34(10):1087–93. doi: 10.1086/673143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang SS, Septimus E, Kleinman K, Moody J, Hickok J, Avery TR, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013 Jun 13;368(24):2255–65. doi: 10.1056/NEJMoa1207290. [DOI] [PMC free article] [PubMed] [Google Scholar]