Abstract
The radiographs of patients on long term bisphosphonates with atypical femur fractures demonstrate markedly thick cortices at the site of the fracture. We conducted a prospective clinical study to determine if cortical thickening is increased in long term bisphosphonate users. We recruited 43 patients who had taken bisphosphonates for more than 5 years. A group of 45 healthy volunteers and 12 patients recently diagnosed with osteoporosis served as controls. We measured the cortical thickening as the ratio of femoral cortical thickness to diameter of the femur, and looked for cortical beaking.
No difference in the cortical thickness ratio was observed between long term bisphosphonate users and osteoporotic controls (0.53 vs. 0.54, p= 0.659). No cases of cortical beaking were seen and no increase in thigh pain was observed. The power of the study was 95% to detect a 10% difference in cortical thickness ratio. We conclude that long term bisphosphonate use does not produce a generalized increase in subtrochanteric femoral cortical thickening in the majority of patients.
Keywords: Atypical femur fracture, Osteoporosis
Introduction
Atypical femur fractures are a distinct clinical entity with a specific radiographic pattern. The fractures occur in the subtrochanteric or diaphyseal region of the femur, have a transverse component, and manifest cortical thickening at the fracture site. The focal cortical thickening has been referred to as “beaking” or “flaring.” This radiographic fracture pattern is strongly associated with long term bisphosphonate use [1,2].
There have been few studies where patients at high risk for atypical femur fractures are screened using imaging for pre-fracture lesions. One study found that two bisphosphonate users out of 100 studied prospectively had radiographic evidence of impending fracture such as beaking of the femoral cortex [3].
As highlighted by the 2013 ASBMR task force report, numerous questions remain regarding the risk factors, etiology, and pathophysiology of atypical femur fractures [4]. One important clinical question is, do patients on long term bisphosphonate medications develop cortical thickening in the subtrochanteric region that is a pre-cursor to developing atypical femur fractures? If radiographic abnormalities are present in asymptomatic patients, a corollary question is, were the radiographic abnormalities present before the bisphosphonates were started? While atypical femur fractures are rare, it is not known whether long-term bisphosphonate users demonstrate radiographic abnormalities in femur well before the fracture occurs.
We performed a prospective observational radiographic and clinical study of healthy volunteers, short term bisphosphonate users, and long term (greater than 5 years) bisphosphonate users to determine the relative rate of radiographic cortical thickening. We hypothesized that the long term users, who were at the highest risk of atypical femur fracture, would display more cortical thickening than short term users or healthy controls.
Methods
Patient cohorts
After Institutional Review Board approval, we recruited from the community 45 patients older than 50 years who had been taking bisphosphonates for at least five years (long term users). We recruited two control cohorts: 12 patients who had recently been diagnosed with osteoporosis and had been taking bisphosphonates for less than 1 year, and an age- and sex-matched group of 43 healthy controls (Table 1). The long term users had taken bisphosphonates for a mean of 8.4 years (standard deviation 3.7 years).
Table 1.
Demographics of Patient Cohorts. No differences between groups were observed other than as noted. FRAX score represents 10 year probability of hip fracture.
| Bisphosphonate use cohort |
|||
|---|---|---|---|
| Naïve | Greater than 5 years |
Less than 1 year |
|
| N | 43 | 45 | 12 |
| Age (SD) | 64 (9) | 66 (10) | 66 (11) |
| Female sex n (%) | 33 (76%) | 39 (86%) | 8 (66%) |
| BMI | 28 (6.0)* | 24 (3.8) | 23 (4.9) |
| Mean femoral neck T score (SD) | −0.74 (1.1)*** | −2.07 (0.76) | −2.07 (0.5) |
| FRAX score (SD) | 1.0 (1.41)*** | 3 (2) | 2.7 (2.2) |
| Thigh pain reported n (%) | 4 (9%) | 5 (11%) | 1 (8%) |
| Median years of bisphosphonate use (range) | 0*** | 7.8 (4.8) | 0.46 (0.65) |
| Cortical thickness index (SD) | 0.58 (0.54)** | 0.53 (0.061) | 0.54 (0.063) |
p < 0.01 compared to bisphosphonate cohorts.
p < 0.001 compared to bisphosphonate cohorts.
p < 0.0001 compared to bisphosphonate cohorts.
The subjects were recruited via newspaper advertisement, flyers, and website postings. The inclusion criteria were: age 50 or older, ambulatory, and living independently. The exclusion criteria were: cognitive impairment, current diagnosis of cancer, previous bilateral hip fractures, pregnancy, small bowel resections, malabsorption, and Paget's disease of bone. There were 54 patients who expressed interest but did not enroll. Two patients had a history of small bowel resection, 42 patients did not meet the medication duration use criteria, and 10 patients declined to enroll for personal reasons.
Patients were enrolled between 2011 and 2012. Patients underwent a standard history and physical examination, completed a detailed medication history, took questionnaires regarding thigh pain and osteoporosis, and underwent standardized radiographs of the femur. Patients underwent DEXA tests and current FRAX scores for 10 year probability of hip fracture were calculated.
Radiographic measurements
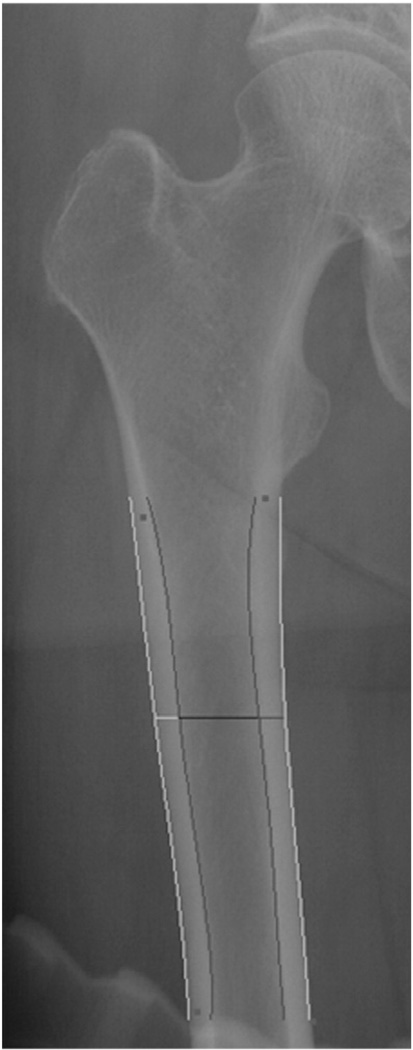
All patients underwent low anterior–posterior pelvic radiographs to include the femurs. A 25 mm radiographic ball was placed on the field as well. The radiographs were read in a blinded fashion by one orthopedic surgeon and one radiologist. Evidence of periosteal reaction, beaking, or flaring was noted. The digital radiographs were imported into a custom program based on Image J. The lower border of the lesser trochanter and most distal portion of femur were identified by the user. The image processing program then identified the medial and lateral cortical borders. The program calculated the thickness of femoral cortex at 5 cm distal to the lesser trochanter, and then identified the position of maximal femoral thickening in the femur. In each femur, we measured the maximal lateral thickness, the maximal medial thickness, the lateral thickness at 5 cm below the lesser trochanter, the medial thickness at 5 cm below the lesser trochanter, and femoral diameter at 5 cm below the lesser trochanter (Fig. 1). Pixel measurements were converted to millimeters using the radiographic marker to eliminate magnification. We found that the maximal thickness was highly correlated with the thickness at 5 cm below the lesser trochanter, and that the magnification variability was very low(data not shown). Thus we found the cortical thickness ratio, as described by Koeppen et al. [5], to be the best measurement for cortical thickening. The cortical thickness ratio is the sum of the medial and lateral cortical thickness of the femur on an anterior posterior radiograph, measured at 5 cm below the lesser trochanter, divided by the diameter of the femur at the same point.
Fig. 1.
Computerized measurement of femoral cortices. An anteroposterior image of the proximal femur is shown. The imaging program measures the cortical thickness of the femur at a point 5 cm below the lesser trochanter.
Statistical analysis
Data were imported in to SPSS 10.0. We calculated the difference in categorical variables with the chi square test. Continuous variables were compared using ANOVA with two sided significance level set at 0.05. A post hoc power analysis was conducted.
Results
We enrolled 100 patients in the study (Table 1). We did not identify a difference in age or sex, between cohorts. As expected, patients in the osteoporotic cohorts had significantly lower T-scores than healthy controls (−2.07 vs.−0.74, p < 0.0001). Naïve patients had a slightly higher BMI (28 vs 24, p < 0.01). We did identify two patients in the healthy cohort with T-scores less than −2.5. These patients were referred to their primary care providers. We did not exclude them from the study. Thigh pain was reported by patients in 11% of long term users and 9% of healthy controls (p = 0.33). As has been previously described, we noted that a number of patients taking bisphosphonates had FRAX hip fracture scores (i.e. 10 year probability of hip fracture) of less than 3% and DEXA scores in the non-osteoporotic range [6].
We did not identify any cases of beaking, periosteal thickening, or endosteal thickening on the radiographs in any of the three cohorts. No lateral cortical stress fractures were identified.
The cortical thickness ratio was not significantly different between long term and short term bisphosphonate users (0.53 vs. 0.54, p = 0.659). Compared to healthy controls, long term users had significantly thinner cortices (6.8 mm vs. 8.0 mm, p < 0.0001) and a lower cortical thickness ratio (0.53 vs. 0.58, p < 0.001).
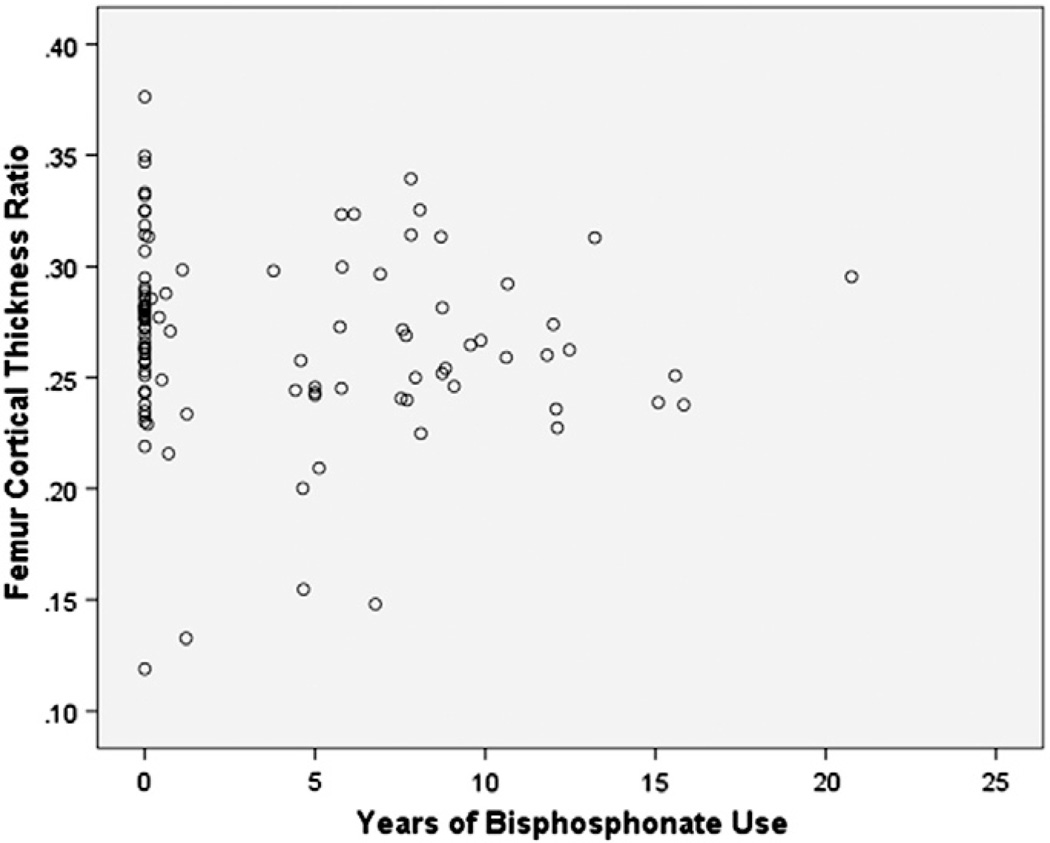
As shown in Fig. 2, we saw no significant correlation between the length of bisphosphonate use and the cortical thickness ratio in bisphosphonate users (r= 0.053, p = 0.68).
Fig. 2.
Relationship between duration of bisphosphonate use and femoral cortical thickness ratio. The femoral cortical thickness ratio is the thickness of the lateral and medial cortices divided by the diameter of the femur.
A post hoc power analysis revealed that the study was 95% powered to detect a 10% difference in cortical thickness ratio between long term and short term users. The long term users had a 1% thicker cortex with the 95% confidence intervals from 4.7% thinner to +4.6% thicker.
Discussion
We conducted a prospective study of a group of patients at highest risk for atypical femur fracture. We identified a low incidence of thigh pain, an absence of radiographic beaking, and no significant increase in cortical thickening in these long term bisphosphonate users. We did observe, as have others [6], that there are a group of patients taking bisphosphonates whose FRAX score (10 year probability of hip fracture) is below the recommended threshold for treatment of osteoporosis.
There is now abundant evidence demonstrating that users of bisphosphonate medications are at increased risk of atypical femur fractures [4, 7]. The pathophysiology of the phenomenon remains a mystery. A consistent hallmark of the atypical femur fracture is the thickening of the femoral cortex seen at the fracture site. One hypothesis is that long term bisphosphonate exposure leads to abnormal thickening in the femur that is brittle and prone to fracture. While the complete fracture maybe rare, the radiographic precursor may be common.
Our study argues against both of these theories. After careful comparison, we did not observe an increase in the femoral cortical thickness in long term bisphosphonate users compared to osteoporotic or healthy controls. We did not observe a beaking or flaring either in the long term users or in controls. Nor did we observe any significant thigh pain or tenderness in either cohort. Our data support the notion that atypical femur fractures begin with a small transverse crack, and that periosteal reaction leads to beaking or flaring in an attempt to heal the fracture.
These data are in line with the other studies of cortical thickening in long term bisphosphonate users. Lenart et al. in a retrospective study found that duration of bisphosphonate use correlated with cortical thickness ratio measured from radiographs [1]. However, Lenart studied radiographs of patients who had already sustained a fracture. In a follow up study, Unnanuntana et al. measured DEXA scans of long and short term bisphosphonate users and found no increase in cortical thickness [8]. The ability of DEXA scans to measure cortical thickness down in the diaphysis of the femur where atypical femur fractures occur is not known. Allison et al. prospectively obtained full femur radiographs on patients who had been on bisphosphonate therapy for 3 years or more. Two of 110 patients were found to have cortical thickening and a stress fracture confirmed by MRI [9]. The absence of any control group prevented statistical analysis. Koeppen et al. measured femoral cortical thickness in 58 atypical femur fracture patients compared to 218 controls [5]. Controls were patients who sustained subtrochanteric or femoral shaft fractures. After correcting for age, no difference in cortical thickness ratio was seen between atypical femur fracture patients and controls.
The absence of global femoral cortical thickening in long term bisphosphonate users, yet the presence of cortical thickening at the fracture site of atypical femur fracture patients, seems to support the prospect that the atypical femur fracture represents a rare, idiosyncratic response that occurs in certain individuals. It may be that there is a yet undefined risk factor that leads patients who are exposed to bisphosphonates toward atypical femur fractures. The risk factor may be genetic variant, an environmental exposure, or an anatomic factor such as femoral geometry.
Our study is consistent with the existing literature but enhanced by recruitment of long term users from the community and comparison to unfractured controls. While the numbers are smaller, the cohorts have comparable ages and demographics, the radiographs were performed in a consistent manner with magnification markers.
The major limitation of this study is the risk of type II error. It is entirely possible that with larger numbers, a difference in the cortical thickness ratio could be observed between controls and long term bisphosphonate users. However our study was powered at the 95% level to detect a 10% difference in cortical thickness ratio. The precise measurement of cortical thickness and lack of variance allows the small sample size to achieve the level of power. It remains possible that, while on the whole cortical thickening is not observed, there is a small subset of patients who do exhibit cortical beaking after long term bisphosphonate exposure. This subset may then go on to fracture quite shortly after developing the radiographic cortical thickening and beaking.
The second major limitation of this study is the use of radiographs as the imaging modality. It is possible that bone scan or MRI would be a much more sensitive imaging modality and would identify more lesions. The clinical utility of these advanced imaging modalities as a screening study for an uncommon condition would be limited, however, due to the increased expense and patient time required. Finally, there may be an element of selection bias. Patients who are taking bisphosphonates but developing pain from impending fracture might be reticent to enroll in a research study, but instead seek formal care.
In summary, in a prospective, adequately powered clinical trial, we did not observe an increase in femoral cortical thickening in long-term bisphosphonate users compared to osteoporotic or healthy controls. These findings are consistent with the known rarity of atypical femur fractures.
References
- 1.Lenart BA, Neviaser AS, Lyman S, Chang CC, Edobor-Osula F, Steele B, et al. Association of low-energy femoral fractures with prolonged bisphosphonate use: a case control study. Osteoporos Int. 2009;20(8):1353–1362. doi: 10.1007/s00198-008-0805-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schilcher J, Koeppen V, Ranstam J, Skripitz R, Michaëlsson K, Aspenberg P. Atypical femoral fractures are a separate entity, characterized by highly specific radiographic features. A comparison of 59 cases and 218 controls. Bone. 2013;52(1):389–392. doi: 10.1016/j.bone.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 3.La Rocca Vieira R, Rosenberg ZS, Allison MB, Im SA, Babb J, Peck V. Frequency of incomplete atypical femoral fractures in asymptomatic patients on long-term bisphosphonate therapy. AJR Am J Roentgenol. 2012;198(5):1144–1151. doi: 10.2214/AJR.11.7442. [DOI] [PubMed] [Google Scholar]
- 4.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American society for bone and mineral research. J Bone Miner Res. 2014;29(1):1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 5.Koeppen VA, Schilcher J, Aspenberg P. Atypical fractures do not have a thicker cortex. Osteoporos Int. 2012;23(12):2893–2896. doi: 10.1007/s00198-012-2173-9. [DOI] [PubMed] [Google Scholar]
- 6.Markman LH, Allison MB, Rosenberg ZS, Vieira RL, Babb JS, Tejwani NC, et al. A retrospective review of patients with atypical femoral fractures while on long-term bisphosphonates: including pertinent biochemical and imaging studies. Endocr Pract. 2013;19(3):456–461. doi: 10.4158/EP12179.OR. [DOI] [PubMed] [Google Scholar]
- 7.Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364(18):1728–1737. doi: 10.1056/NEJMoa1010650. [DOI] [PubMed] [Google Scholar]
- 8.Unnanuntana A, Ashfaq K, Ton QV, Kleimeyer JP, Lane JM. The effect of long-term alendronate treatment on cortical thickness of the proximal femur. Clin Orthop Relat Res. 2012;470(1):291–298. doi: 10.1007/s11999-011-1985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allison MB, Markman L, Rosenberg Z, Vieira RL, Babb J, Tejwani N, et al. Atypical incomplete femoral fractures in asymptomatic patients on long term bisphosphonate therapy. Bone. 2013;55(1):113–118. doi: 10.1016/j.bone.2013.03.018. [DOI] [PubMed] [Google Scholar]