Abstract
Introducton:
Kidney stone recurrence is common. Preventive measures can lead to improved quality of life and costs savings to the individual and healthcare system. Guidelines to prevent recurrent kidney stones are published by various urological societies. Adherence to guidelines amongst healthcare professionals in general is poor, while adherence to preventive management guidelines regarding stone disease is unknown. To understand this issue, we conducted an online study to assess the knowledge, attitudes, and practice patterns of healthcare practitioners in Northern Ontario.
Methods:
We used the database of healthcare providers affiliated with the Northern Ontario School of Medicine, in Sudbury (East Campus) and Thunder Bay (West Campus), Ontario. We designed the survey based on current best practice guidelines for the management of recurrent kidney stones. Questions covered 3 domains: knowledge, attitudes, and practice patterns. Demographic data were also collected. The survey was distributed electronically to all participants.
Results:
A total of 68 healthcare providers completed the survey. Of these, most were primary care physicians (72%). To keep uniformity, we analyzed the data of this homogenous group. A total of 70% of the respondents were aware of the current guidelines; however, only 43% applied their knowledge in clinical practice. Most participants lacked confidence while answering most items in the attitude domain.
Conclusions:
Most primary care physician respondents were aware of the appropriate preventive measures for recurrent kidney stones; however, they do not appear to apply this knowledge effectively in clinical practice. A low response rate is a limitation of our study. Further studies involving a larger sample size may lead to information sharing and collaborative care among healthcare providers.
Introduction
Kidney stones affect up to 5% of the population, with a lifetime risk of passing a kidney stone of about 8% to 10%.1 Once a kidney stone forms, the probability that a second stone will form within 5 to 7 years is about 50%.1 After a stone recurrence, the subsequent relapse risk is higher and the interval between recurrences is shortened.2 Thus, the recurrent nature of kidney stones underscores the importance of prevention. Effectively utilized preventive measures at “stone clinics” have shown to reduce the 5-year recurrence rate by 60%.3 However, this notable degree of reduction is not always observed in the general population.
The rates of healthcare preventive service delivery among primary care providers is low.4 This gap in the utilization of preventive strategies may be related to a variety of factors, including physician disagreement with clinical guidelines, lack of awareness, provider inertia, lack of outcome expectancy, or the absence of incentives that reinforce delivery of preventive services.5–6 Efforts to improve preventive service delivery in primary care practice are numerous, but yield small to modest results.7–10
Practice pattern compliance of healthcare professionals to guidelines has been reviewed in numerous medical conditions. However, adherence to preventive stone disease management guidelines among healthcare providers is unknown. To understand this issue, we conducted an online survey to assess the knowledge, attitudes, and practice patterns of healthcare providers regarding recurrent stone prevention.
Methods
The study population included a random sample of health-care providers practicing in Northern Ontario. The survey was distributed electronically using the clinical faculty e-mail database of the Northern Ontario School of Medicine (NOSM) and included primary care physicians, specialists and allied healthcare professionals (nurse practitioners).
The questions were designed based on current best practice guidelines for the prevention of recurrent kidney stones. The survey comprised of 3 domains: knowledge, attitudes, and practice patterns. Demographic data were also collected. Only those participants who manage patients with kidney stones completed the practice patterns section. The practice patterns section was completed prior to the knowledge and attitude sections to avoid leading answers. Answer formats consisted of multiple-choice questions for the knowledge and practice pattern domains and the Likert scale for the attitude domain. The senior authors reviewed all questions. The ethics committee of the Timmins and District Hospital approved the study protocol and consent was obtained from all subjects.
In August 2012, an email link to the online survey was sent to the survey population. Qualtrics survey software was used to build the survey tool.11 Two reminder emails were sent. Compensation was not offered for survey completion. The survey remained open for 2 months. Descriptive statistics were performed using Microsoft Excel (Microsoft Canada Co., Mississauga, ON).
Results
We sent out 468 survey invitations. In total, 68 were completed by Northern Ontario physicians and allied healthcare professionals, for a response rate of 14.5%. Of these 68, 20 had to be excluded due to profession-specific low response rates (13 were specialists and 7 were allied healthcare professionals). In total, 48 respondents were part of our data analysis.
Demographics
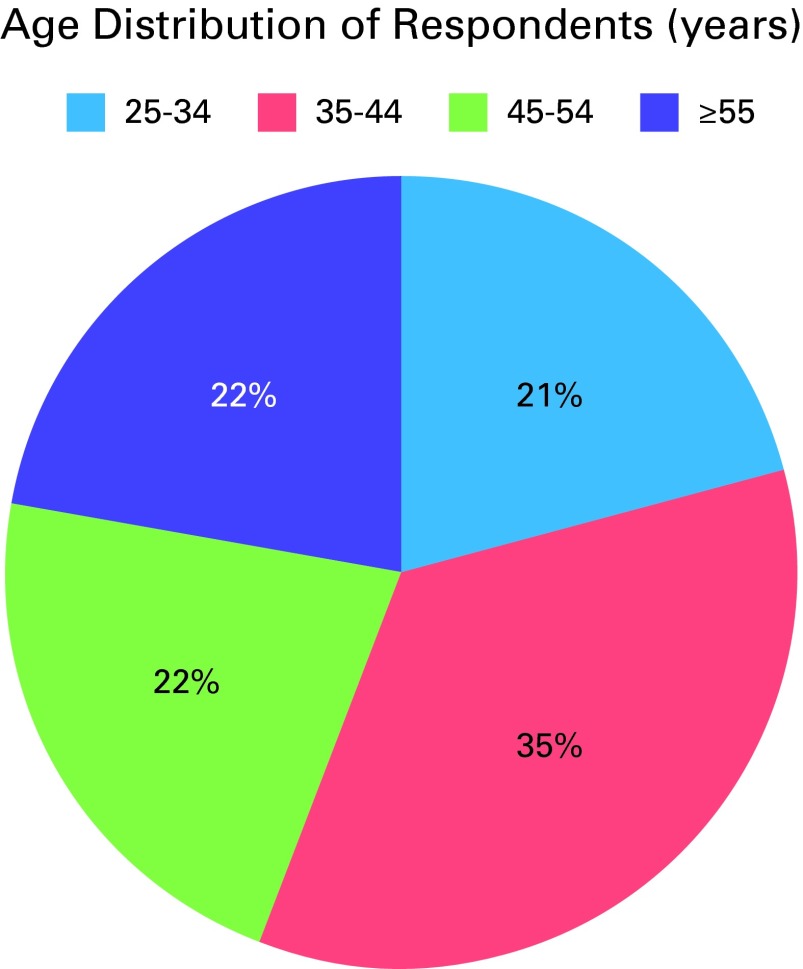
Of the 468 invitations, 420 were primary care physicians (206 were male and 214 were female). Among the total included respondents, 22 (46%) were male, 26 (54%) were female. The age of respondents was equally distributed (Fig. 1). Respondents’ geographic location varied vastly, representing the true demographics of Northern Ontario.
Fig. 1.
Age distribution of respondents.
Knowledge
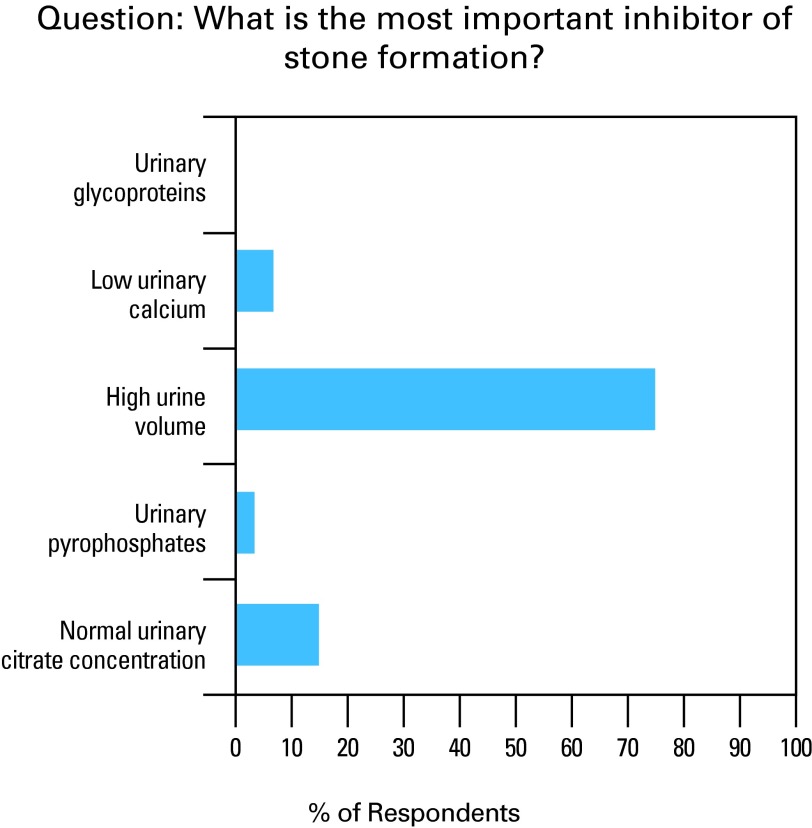
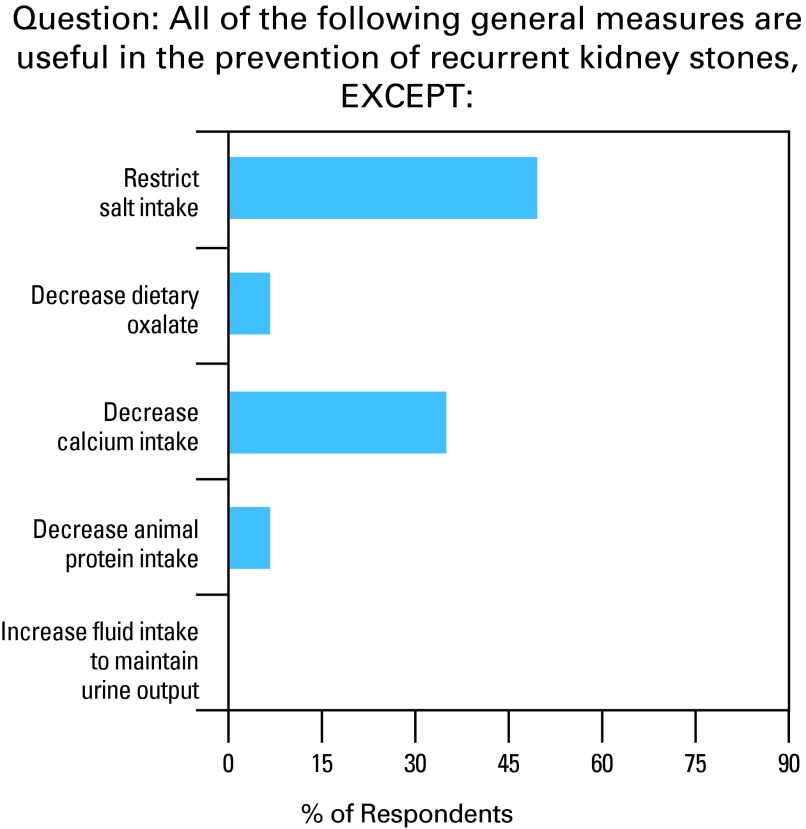
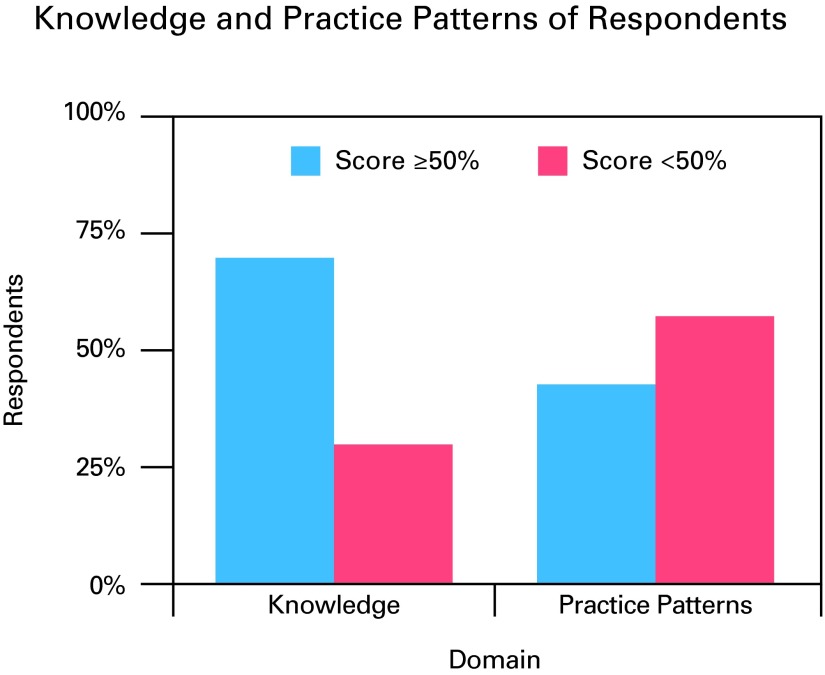
We found that 75% of respondents correctly identified high urine volume as a critical factor in preventing stone recurrence (Fig. 2). The choice of diuretic was identified correctly by 49% of respondents. Seventy percent of respondents were aware of associated comorbidities that increase the likelihood of stone formation. Only 7% of respondents correctly identified the stone type that recurs most frequently. The importance of salt restriction was correctly identified by only half of respondents (Fig. 3). We found that 63% of respondents recognized that the timing of the detailed workup of the kidney stone formation is important in prevention. Overall, 70% of respondents answered in concordance with best practice guidelines in at least half of the questions (Fig. 4).
Fig. 2.
Illustration of knowledge regarding high urine volume.
Fig. 3.
Illustration regarding knowledge of salt intake.
Fig. 4.
Respondent scores on knowledge and practice pattern sections.
Attitudes
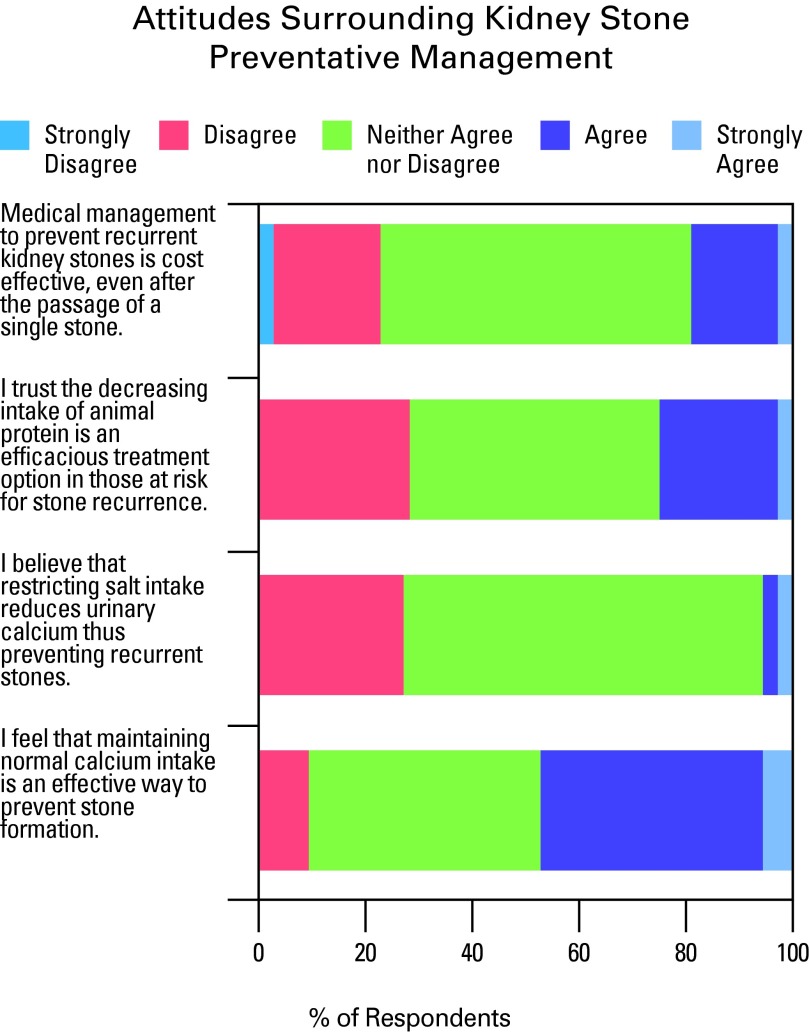
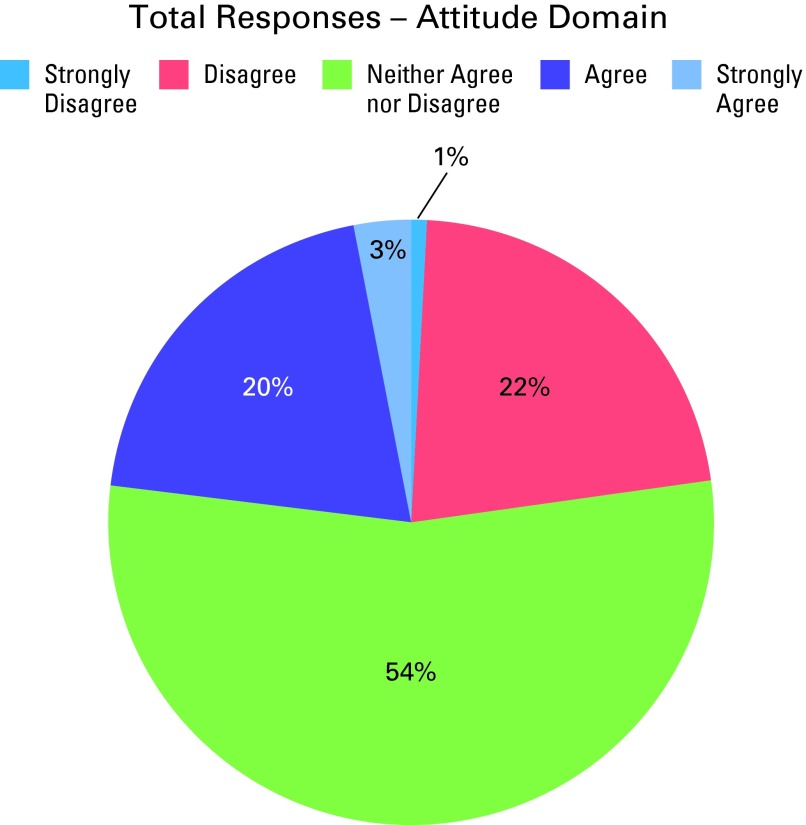
Most respondents lacked confidence regarding commonly recommended cost-effective therapies in the prevention of recurrent kidney stones, including restriction of sodium intake, animal protein and dietary oxalate (Fig. 5, Fig. 6). Respondents displayed confidence in the importance of both fluid intake and stone analysis. We found that 49% of respondents showed uncertainty in at least half of the questions.
Fig. 5.
Illustration of attitudes toward preventative kidney stone measures.
Fig. 6.
Illustration of uncertainty among respondents.
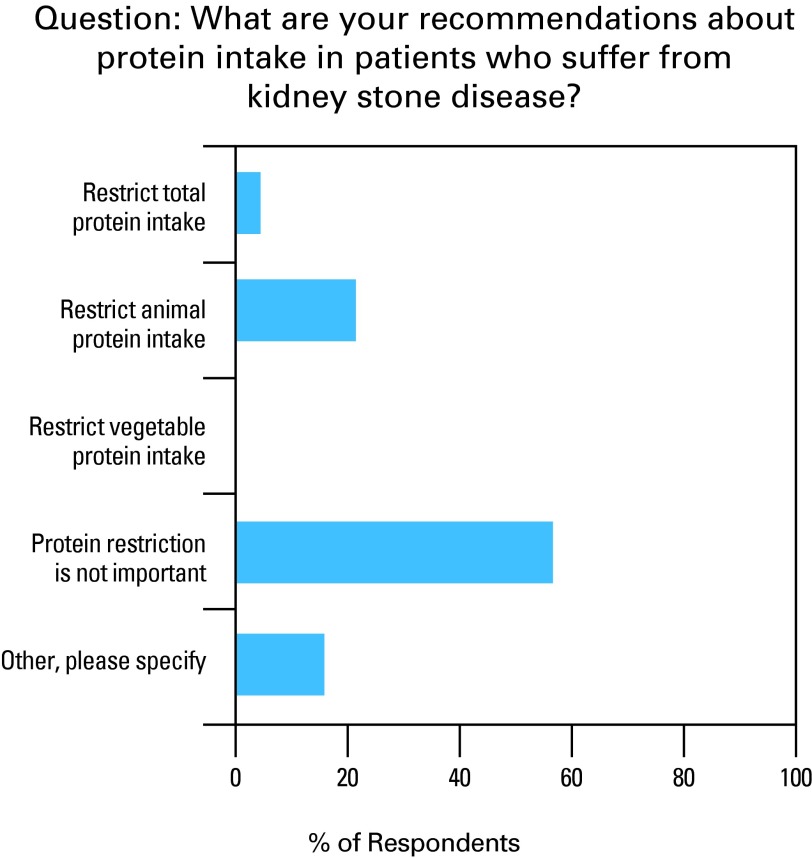
Practice patterns
Most respondents agree with lifestyle modification, before considering drug therapy in the prevention of stones. Sixty-nine percent of respondents agree that normal calcium intake should be maintained in stone disease patients. A little over half of respondents (56%) negated the importance of animal protein restriction (Fig. 7). Twenty-seven percent of respondents recommended stone analysis with each stone retrieved, while 57% reported to complete stone analysis on patients who suffer from multiple stones. Only 20% of respondents agreed with fluid intake guidelines. A total of 43% of respondents’ answers agreed with best practice guidelines in over half of the questions in the practice patterns domain.
Fig. 7.
Illustration of recommendations regarding protein intake.
Discussion
Knowledge, attitudes, and adherence to guidelines have been reviewed in numerous medical conditions. Despite evidence-based recommendations from professional organizations, preventive services have shown to be delivered at low rates. Unfortunately, measures to improve preventive service delivery have not demonstrated optimal results.7–10 The results of our study mirror this recurrent literature finding.
Respondents demonstrated a reasonable level of knowledge regarding kidney stone prevention, but did not appear to effectively apply this knowledge in clinical practice. Although 70% of respondents were aware of preventive measures, only 43% applied their knowledge effectively in clinical practice (Fig. 7). Reasons for the lack of application are unknown, but the treatment gap is clearly demonstrated in this study.
An increase in fluid intake remains the strongest recommendation in stone prevention.12 A randomized clinical trial showed that stones recurred in only 12 (12%) of the 99 patients who maintained a urine volume of about 2.6 L/day over 5 years, whereas stones recurred in 27 (27%) of the 100 patients in the control group, whose urine volume was about 1.2 L/day (p = 0.008). The experimental group showed a greater duration between recurrences than in the control group (38.7 vs. 25.1 months; p = 0.016).13 Current literature suggests that patients should increase their fluid intake with a goal of maintaining a urine volume of 2 to 3 L per day (Table 1).12 Only 20% of respondents advocate a urine output of 2 to 3 L per day for their kidney stone patients.
Table 1.
General measures to prevent recurrence of stones
|
Uric acid stones, although not common, recur frequently.14 Most respondents (93%) failed to identify the high rate of recurrence with such stones. Detailed medical evaluation and prophylaxis were not considered cost-effective in patients who form stones less than once every 3 years. We found that 63% of respondents showed consistency with this practice.15
The attitudes of most respondents concerning the role of dietary oxalate, salt intake, and cranberry juice in stone prevention did not parallel current evidence-based literature. Oxalate plays an integral role in calcium stone formation. Foods rich in oxalate include spinach, cranberries, chocolate, and tea. The concentration of oxalate is considerably lower than the concentration of calcium in urine. Thus, changes in oxalate concentration have a greater impact than changes in calcium concentration on the relative supersaturation of calcium oxalate crystals. The rate of change in supersaturation is 23 times greater for increases in oxalate than for comparable increases in calcium.16 Current guidelines suggest a moderate consumption of oxalate-rich foods.17
Restricting sodium intake is important in stone prevention, as a resulting reduction in renal excretion of sodium reduces renal excretion of calcium thereby rendering urine less lithogenic.13 Further, urinary sodium excretion increases the saturation of monosodium urate, acting as a nidus for calcium crystallization.18 Canadian guidelines advocate for a reduced sodium diet of less than 2300 mg daily.17
Cranberry juice significantly alters key urinary risk factors by decreasing urinary excretion of oxalate and phosphate and increasing citrate excretion, an inhibitor of calcium stone formation. There is a decrease in the relative super-saturation of calcium oxalate, which tends to be substantially lower than that induced by water alone.19
Animal protein intake influences the likelihood of calcium stone formation. Ingested animal protein generates an acid load increasing urinary calcium excretion and reducing the excretion of citrate, an inhibitor of calcium stones.20–23 The Canadian Urological Association (CUA) guidelines recommend reduced animal protein intake to stone formers (Table 1).17 In contrast to current recommendations, over half of respondents (57%) did not advocate protein restriction to patients.
The CUA advocates that all kidney stone patients undergo a limited metabolic evaluation to rule out systemic disease. A metabolic evaluation for all stone patients should include blood studies (sodium, potassium, chloride, bicarbonate, creatinine, calcium, albumin, uric acid and phosphate), a urinalysis and a stone analysis.17 Over half of respondents (57%) complete stone analysis for patients who have experienced multiple stones.
A moderate dietary calcium intake (1 g/day) is reasonable for patients.17 A low-calcium diet is strongly discouraged as it permits greater oxalate absorption, leading to hyperoxaluria.13 While intake of dietary calcium appears to decrease the risk of symptomatic kidney stones, consumption of supplemental calcium may increase risk.24 Most respondents (69%) advocated normal calcium intake to stone patients.
As outlined, many medical associations and international researchers have described the role of preventive medicine in stone disease. Our study showed an adequate level of knowledge of primary care provider respondents. However, despite sufficient knowledge, their attitudes lack confidence and practice patterns are generally not consistent with current best practice guidelines.
Our study has its limitations, including a low response rate, introducing the possibility of biases. Nevertheless, to our knowledge this is the first study to assess the practices of Northern Ontario primary care providers regarding kidney stone prevention.
Conclusion
We found that most primary care physicians knew about appropriate preventive measures; however, they did not always apply this knowledge effectively in clinical practice. Low rates of preventive service delivery have been demonstrated in many areas of medicine; our results concur with this conclusion. Efforts to improve guideline adherence to date have been unsuccessful. Methods to improve confidence around stone prevention in the primary care setting should be further explored. Future studies involving a larger sample size may lead to information sharing and collaborative care among healthcare providers, translating into better quality of care and cost-savings to the patient and the healthcare system.
Appendix:
Kidney Stone Recurrence Management
| KNOWLEDGE: Below are a series of questions aimed at assessing your knowledge surrounding management of kidney stone recurrence. |
|
|
What is the most important inhibitor of stone formation?
|
|
|
Of the following, which type of stone recurs most frequently?
|
|
|
After occurrence of kidney stones, when would you consider detailed work-up to prevent stone recurrence?
|
|
|
All of the following general measures are useful in the prevention of recurrent kidney stones, EXCEPT:
|
|
|
All of the following factors increase the risk of stone formation, EXCEPT:
|
|
|
Which of the following diuretics is the least helpful in controlling urinary calcium excretion in patients with hypercalciuria?
|
|
|
| Thank you for completing the questionnaire. Please provide any comments/suggestions regarding the survey. |
| PRACTICE PATTERNS: The following questions are to assess the practice patterns and the answers to these questions should reflect what you do in your daily practice, to prevent recurrence of kidney stones. |
|
|
What do you recommend about fluid intake in patients who suffer from kidney stone disease?
|
|
|
What are your recommendations about protein intake in patients who suffer from kidney stone disease?
|
|
|
What are your recommendations about calcium intake in patients who suffer from kidney stone disease?
|
|
|
What are your practices with regards to stone analysis in prevention of kidney stones?
|
|
|
After the initial presentation of a calcium oxalate stone, I would prescribe _________________ to help with prevention of stone recurrence:
|
| ATTITUDES: Below is a list of statements that are to assess your attitudes surrounding the management of recurrent kidney stones. | |||||
|
| |||||
| Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | |
| I feel that it is important to maintain normal calcium intake is an effective way to prevent stone formation. | ❍ | ❍ | ❍ | ❍ | ❍ |
| I have confidence that decreasing dietary oxalate (i.e. spinach, chocolate) is an efficient method in reducing risk of stone recurrence. | ❍ | ❍ | ❍ | ❍ | ❍ |
| Increasing fluid intake is a measure I promote to all patients at risk of kidney stone recurrence. | ❍ | ❍ | ❍ | ❍ | ❍ |
| I believe that restricting salt intake reduces urinary calcium thus preventing recurrent stones. | ❍ | ❍ | ❍ | ❍ | ❍ |
| I believe that cranberry juice intake is a worthwhile treatment option for patients who are at risk of stone recurrence. | ❍ | ❍ | ❍ | ❍ | ❍ |
| I trust that decreasing intake of animal protein is an efficacious treatment option in those at risk for stone recurrence. | ❍ | ❍ | ❍ | ❍ | ❍ |
| I believe stone analysis is important in prevention of recurrent kidney stones. | ❍ | ❍ | ❍ | ❍ | ❍ |
| Medical management to prevent recurrent kidney stones is cost effective, even after the passage of a single stone. | ❍ | ❍ | ❍ | ❍ | ❍ |
| KNOWLEDGE: Below are a series of questions aimed at assessing your knowledge surrounding management of kidney stone recurrence. |
|
|
What is the most important inhibitor of stone formation?
|
|
|
Of the following, which type of stone recurs most frequently?
|
|
|
After occurrence of kidney stones, when would you consider detailed work-up to prevent stone recurrence?
|
|
|
All of the following general measures are useful in the prevention of recurrent kidney stones, EXCEPT:
|
|
|
All of the following factors increase the risk of stone formation, EXCEPT:
|
|
|
Which of the following diuretics is the least helpful in controlling urinary calcium excretion in patients with hypercalciuria?
|
|
|
| Thank you for completing the questionnaire. Please provide any comments/suggestions regarding the survey. |
Footnotes
Competing interests: Dr. Bos, Dr. Abara and Dr. Parmar declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Asplin JR, Favus MJ, Coe FL. Nephrolithiasis. In: Brennder BM, editor. Brenner and Rector’s the kidney. 5th ed. Philadelphia: PA. Saunders; 1996. pp. 1893–935. [Google Scholar]
- 2.Strauss AL, Coe FL, Deutsch L, et al. Factors that predict relapse of calcium nephrolithiasis during treatment: A prospective study. Am J Med. 1982;72:17–24. doi: 10.1016/0002-9343(82)90566-6. [DOI] [PubMed] [Google Scholar]
- 3.Heilberg IP. Update on dietary recommendations and medical treatment of renal stone disease. Nephrol Dial Transplant. 2000;15:117–23. doi: 10.1093/ndt/15.1.117. [DOI] [PubMed] [Google Scholar]
- 4.Stange KC, Goodwin MA, Zyzanski SJ, et al. Sustainability of a practice-individualized preventive service delivery intervention. Am J Prev Med. 2003;25:296–300. doi: 10.1016/S0749-3797(03)00219-8. [DOI] [PubMed] [Google Scholar]
- 5.Flocke SA, Litaker D. Physician practice patterns and variation in the delivery of preventative services. J Gen Intern Med. 2007;22:191–6. doi: 10.1007/s11606-006-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayward R. Clinical practice guidelines on trial. Can Med Assoc J. 1997;156:1725–7. [PMC free article] [PubMed] [Google Scholar]
- 7.Solberg LI, Kottke TE, Brekke ML. Will primary care clinics organize themselves to improve the delivery of preventive services? A randomized controlled trial. Prev Med. 1998;27:623–31. doi: 10.1006/pmed.1998.0337. [DOI] [PubMed] [Google Scholar]
- 8.Solberg LI, Kottke TE, Brekke ML, et al. Failure of a continuous quality improvement intervention to increase the delivery of preventive services. A randomized trial. Eff Clin Pract. 2000;3:105–15. [PubMed] [Google Scholar]
- 9.McBride P, Underbakke G, Plane MB, et al. Improving prevention systems in primary care practices: The Health Education and Research Trial (HEART) J Fam Pract. 2000;49:126–9. [PubMed] [Google Scholar]
- 10.Goodwin MA, Zyzanski SJ, Zronek S, et al. A clinical trial of tailored office systems for preventive service delivery: The Study To Enhance Prevention by Understanding Practice (STEP-UP) Am J Prev Med. 2001;21:20–8. doi: 10.1016/S0749-3797(01)00310-5. [DOI] [PubMed] [Google Scholar]
- 11.Qualtics. https://www.qualtrics.com. Accessed November 5, 2014.
- 12.Borghi L, Meschi T, Amato F, et al. Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: A 5-year randomized prospective study. J Urol. 1996;155:839–43. doi: 10.1016/S0022-5347(01)66321-3. [DOI] [PubMed] [Google Scholar]
- 13.Morton RA, Iliescu EA, Wilson J. Nephrology: 1. Investigation and treatment of recurrent kidney stones. CMAJ. 2002;166:213–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Munoz-Velez D, Garcia-Montes F, Costa-Bauza A, et al. Analysis of spontaneously passed urinary tract stones. Springer-Verlag. 2010;38:35–6. doi: 10.1007/s00240-009-0230-4. [DOI] [PubMed] [Google Scholar]
- 15.Chandhoke PS. When is medical prophylaxis cost effective for recurrent calcium stones? J Urol. 2002;168:937–40. doi: 10.1016/S0022-5347(05)64546-6. [DOI] [PubMed] [Google Scholar]
- 16.Rodgers A. Aspects of calcium oxalate crystallization: Theory, in vitro studies, and in vivo implementation. J Am Soc Nephrol. 1999;10:S351–4. [PubMed] [Google Scholar]
- 17.Paterson R, Fernandez A, Razvi H, et al. Evaluation and medical management of the kidney stone patient. Can Urol Assoc J. 2010;4:375–9. doi: 10.5489/cuaj.10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parmar MS. Clinical review: Kidney stones. BMJ. 2004;328:1420–4. doi: 10.1136/bmj.328.7453.1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McHarg T, Rodgers A, Charlton K. Influence of cranberry juice on the urinary risk factors for calcium oxalate kidney stone formation. BJU Int. 2003;92:765–8. doi: 10.1046/j.1464-410X.2003.04472.x. [DOI] [PubMed] [Google Scholar]
- 20.Kok DJ, Iestra JA, Doorenbos CJ, et al. The effects of dietary excesses in animal protein and in sodium on the composition and the crystallization kinetics of calcium oxalate mono- hydrate in urines of healthy men. J Clin Endocrinol Metab. 1990;71:861–7. doi: 10.1210/jcem-71-4-861. [DOI] [PubMed] [Google Scholar]
- 21.Breslau NA, Brinkley L, Hill KD, et al. Relationship of animal protein-rich diet to kidney stone formation and calcium metabolism. J Clin Endocrinol Metab. 1988;66:140–6. doi: 10.1210/jcem-66-1-140. [DOI] [PubMed] [Google Scholar]
- 22.Lemann J, Jr, Gray RW, Maierhofer WJ, et al. The importance of renal net acid excretion as a determinant of fasting urinary calcium excretion. Kidney Int. 1986;29:743–6. doi: 10.1038/ki.1986.60. [DOI] [PubMed] [Google Scholar]
- 23.Hamm LL. Renal handling of citrate. Kidney Int. 1990;38:728–35. doi: 10.1038/ki.1990.265. [DOI] [PubMed] [Google Scholar]
- 24.Curhan GC, Walter WC, Speizer FE, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497–504. doi: 10.7326/0003-4819-126-7-199704010-00001. [DOI] [PubMed] [Google Scholar]