Abstract
The notion that there is an association between essential tremor (ET) and higher ethanol consumption has crept into the literature; however, the data are limited and conflicted. 354 ET cases and 370 matched controls were enrolled in a clinical-epidemiological study. Average current daily ethanol consumption was estimated using the Willett Semi-quantitative Food Frequency Questionnaire. The proportion of cases and controls who drank any ethanol was similar: 66.7% vs. 64.1%, p = 0.46, as was the proportion who reported heavy ethanol consumption: 4.0% vs. 3.5%, p = 0.74. The average daily ethanol intake was numerically higher in cases than controls (7.99 ± 12.39 [median = 3.03] vs. 6.55 ± 10.62 [median = 1.80] gm), but this difference did not reach significance (p = 0.15). Among cases, there was no correlation between average daily ethanol intake and tremor severity (r = 0.008, p =0.88). These data, on more than 700 enrollees, do not support any sizable differences between ET cases and controls in terms of average daily ethanol consumption or ethanol overuse. The absence of a correlation in cases between ethanol consumption and tremor severity goes against the hypothesis that ET patients are self-medicating to a significant degree.
Keywords: Essential tremor, Case-control, Epidemiology, Clinical, Ethanol, Alcohol
1. Introduction
Ethanol consumption temporarily lessens the severity of tremor as well as gait abnormalities in patients with essential tremor (ET).1–3 Hence, there is the theoretic potential for patients to self-medicate and/or abuse ethanol. While an early report suggested a higher prevalence of alcoholism among ET cases than controls,4 subsequent studies have failed to confirm this association.5, 6 Furthermore, the notion that there is an association between ET and higher ethanol consumption (although not to the level of alcoholism) has crept into the literature; however, the data are conflicted and not very convincing, and doubts about the tendency towards excessive ethanol use in ET remain.5–7 Available studies are limited by small sample sizes and/or lack of rigor in collecting data on ethanol consumption. There is a need to study this issue more definitively.
Furthermore, there are few data on whether ethanol consumption in ET tracks with severity of symptoms, as one would predict if one were hypothesizing that ET patients were self-medicating.2 Finally, there are some data that suggest that families share a common response to ethanol,8 and therefore, that familial cases might be more prone to use and abuse than sporadic cases, but there are no data to support or refute this.2
Capitalizing on the enrollment of approximately 350 ET cases and a similar number of matched controls in a clinical-epidemiological study in New York, for whom we used the Willett Semi-quantitative Food Frequency Questionnaire9 to estimate daily grams of ethanol intake, we now (1) compare daily ethanol intake in a large sample of ET cases vs. carefully matched controls, (2) determine whether ethanol use segregated more among individuals who were manifesting more symptoms, and (3) stratify the ET sample into familial vs. non-familial cases to determine whether the two groups differ with respect to daily ethanol intake. Our overarching goal was to further refine our understanding of the association between ethanol intake and this disease.
2. Materials and Methods
2.1. Subjects
From 2000 – 2009, ET cases were enrolled in a study of the environmental epidemiology of ET at Columbia University Medical Center (CUMC).10 These cases were adults (≥ 18 years of age) from two primary sources: (1) patients whose neurologist was on staff at the Center for Parkinson’s Disease and Other Movement Disorders at the Neurological Institute of New York, CUMC (see11 for details) or (2) patients who were cared for by their local doctor in the tri-state region (New York, New Jersey, Connecticut) and, as members of the International Essential Tremor Foundation, had read advertisements for the study and volunteered. Prior to enrollment, cases all signed informed consent approved by the CUMC Ethics Committee.
During the same time period, control subjects were recruited for the same study. They were identified within the New York Metropolitan area using random digit telephone dialing within the same set of telephone area codes as the cases (e.g., 212, 201, 203, 516, 718, and 914). Controls were frequency-matched to cases based on age and gender; the intended ratio of controls to cases was ~1:1.
2.2. Evaluation
A Telephone Interview for Cognitive Status (TICS, range = 0 – 41 [no deficits]) was administered,12 and all cases and controls who scored < 30 were excluded. An in-person structured evaluation was performed during which a trained research assistant administered demographic, medical, and family history questionnaires. The questionnaires also included several items that were socioeconomic indicators (e.g., number of rooms in home/number of people living in home, number of live births [women], and years since last hospitalization), which we have used in our own studies or which have been used by others.13–17 The Cumulative Illness Rating Scale (CIRS) was used to quantify comorbid illness. The CIRS score can range from 0 (no illness) – 42 (severe comorbidity in all 14 systems).18
The Willett Semi-Quantitative Food-Frequency Questionnaire was also administered.9 This is a 20-minute food-frequency questionnaire that includes questions on frequency of current consumption of numerous foods and on the use of vitamins and mineral supplements. During the questionnaire, average current daily ethanol use was reported in detail (wine, beer, spirits), and based on the mean ethanol content of a standard drink, then converted to daily intake of ethanol (gms). Food frequency data were also used to compute mean daily caloric intake (in Kcal). The questionnaire has shown good reliability and validity related to recent nutrient intake.9
A videotaped neurological examination was performed on all cases and controls. This included one test for postural tremor and five tests for kinetic tremor (pouring, using spoon, drinking, finger-nose-finger, drawing spirals) performed with each arm (12 tests total). A neurologist specializing in movement disorders (E.D.L.) used a reliable19 and validated20 clinical rating scale, the Washington Heights-Inwood Genetic Study of ET (WHIGET) tremor rating scale, to rate tremor during each test: 0 (none), 1 (mild), 2 (moderate), 3 (severe). Head, voice and jaw tremors were noted to be present vs. absent. These ratings were combined to form the total tremor score (range = 0 – 36), which is an assessment of postural and kinetic tremor.21 The videotaped examination, as well as the history, were used to confirm the ET diagnosis using published diagnostic criteria (kinetic arm tremor rated ≥2 during at least 3 tests or head tremor) in the absence of Parkinson’s disease or dystonia.21
Weight and height were assessed in cases and controls using a standard protocol. Measurements were taken of body weight to the nearest 0.1 pound using a balance scale designed for field surveys (Scale-Tronix 5600, White Plains, NY). Height was measured to the nearest 0.5 cm using a movable anthropometer (GPM Martin Type, Pfister Inc, Carlstadt, NJ). BMI was then calculated as weight in kg divided by the square of height in meters.
2.3. Statistical Analyses
Analyses were performed using SPSS (version 21.0). Clinical characteristics of ET cases and controls were compared using Student’s t-tests and chi-square (X2) tests. When variables were not normally distributed (as determined using the Kolmogorov-Smirnov test), a non-parametric test (Mann-Whitney test) was used.
We report raw data (average current daily use of wine, beer, spirits), and data on average daily ethanol consumption in grams. Average daily ethanol consumption was not normally distributed (Kolmogorov-Smirnov test = 7.12, p < 0.001); therefore, medians as well as means and standard deviations were reported and case-control differences were assessed using the Mann-Whitney test. Heavy ethanol consumption has been defined as consumption of an average of four or more standard drinks (10 grams ethanol) per day for a man, or three or more per day for a woman.22 In one analysis, we stratified the sample by decade of current age (≤40, 40 – 49, 50 – 59, 60 – 69, ≥70 years) to assess case-control differences in average daily ethanol intake. Among the 473 subjects who drank any ethanol, we also created ethanol consumption quartiles (≤2 gms/day, 3–7 gms/day, 8–14 gms/day, ≥15 gms/day). In a logistic regression model (outcome = diagnosis) restricted to these 473 subjects, we assessed the likelihood of being in the highest vs. lowest quartile.
3. Results
The 354 ET cases and 370 controls were similar in age, gender, race, education, socioeconomic indicators (number of rooms in home/number of people living in home, number of live births [women], and years since last hospitalization) and CIRS score (Table 1). BMI was lower in ET cases than controls, despite a marginally higher caloric intake in cases (Table 1).
Table 1.
Demographic and Clinical Characteristics of ET Cases and Control Subjects
| Controls | ET Cases | Difference | |
|---|---|---|---|
| Number | 370 | 354 | NA |
| Age in years | 68.0 (11.5) | 67.3 (15.2) | t = 0.73, p = 0.46 |
| Female gender | 208 (56.2) | 186 (52.5) | X2 = 0.98, p = 0.32 |
| White race | 345 (93.2) | 334 (94.4) | X2 = 0.38, p = 0.54 |
| Years of education | 15.3 (3.4) Median = 16.0 |
15.1 (3.8) Median = 16.0 |
MW = 0.08, p = 0.93 |
| Number of rooms in Home/number of people living in home | 3.3 (1.7) Median = 3.0 |
3.4 (1.6) Median = 3.0 |
MW = 1.19, p = 0.23 |
| Number of live births (women) | 2.1 (1.7) Median = 2.0 |
2.1 (1.5) Median = 2.0 |
MW = 0.06, p = 0.95 |
| Years since last hospitalization | 14.5 (19.2) Median = 6.0 |
15.0 (20.7) Median = 6.0 |
MW = 0.26, p = 0.80 |
| Total tremor score | 3.8 (2.9) | 18.9 (7.2) | t = 36.14, p < 0.001 |
| First- or second-degree relative with ET or tremor | 41 (11.1) | 218 (61.6) | X2 = 200.8, p <0.001 |
| Tremor duration in years | NA | 23.5 (18.8) | NA |
| Taking a medication to treat tremor | NA | 189 (53.4) | NA |
| Surgery (thalamotomy, DBS, other) for tremor | NA | 11 (3.0) | NA |
| CIRS score | 5.5 (3.7) Median = 5.0 |
5.4 (3.6) Median = 5.0 |
MW = 0.07, p = 0.94 |
| BMI (kg/m2) | 27.7 (5.6) Median = 26.7 |
26.7 (5.0) Median = 26.3 |
MW = 2.03, p = 0.04 |
| Mean daily caloric intake (Kcal) | 1397.8 (458.8) Median = 1341.6 |
1440.3 (427.6) Median = 1420.9 |
MW = 1.69, p = 0.09 |
Mean (standard deviation) or number (percent).
BMI = body mass index, CIRS = Cumulative Illness Rating Scale, DBS = deep brain stimulation, ET = essential tremor, MW = Mann-Whitney test, NA = Not applicable.
The proportion of cases and controls who drank any ethanol was similar: 236 (66.7%) vs. 237 (64.1%), X2 = 0.55, p = 0.46. The proportion of cases and controls who reported heavy ethanol consumption was similar: 14 (4.0%) vs. 13 (3.5%), X2 = 0.098, p = 0.74. Raw data on number of drinks per day are shown, and did not differ in cases vs. controls (Table 2).
Table 2.
Beer, Wine and Spirit Consumption in 354 ET Cases vs. 370 Controls
| Controls | ET | |
|---|---|---|
| Beer | ||
| < once per month | 277 (74.9) | 243 (68.6) |
| 1–3 per month | 44 (11.9) | 48 (13.6) |
| 1 per week | 18 (4.9) | 23 (6.5) |
| 2–4 per week | 22 (5.9) | 25 (7.1) |
| 5–6 per week | 5 (1.4) | 3 (0.8) |
| 1 per day | 4 (1.1) | 3 (0.8) |
| 2–3 per day | 0 (0.0 | 7 (2.0) |
| 4–5 per day | 0 (0.0) | 1 (0.3) |
| 6+ per day | 0 (0.0) | 1 (0.3) |
| Wine | ||
| < once per month | 232 (62.7) | 253 (71.5) |
| 1–3 per month | 49 (13.2) | 30 (8.5) |
| 1 per week | 15 (4.1) | 20 (5.6) |
| 2–4 per week | 43 (11.6) | 28 (7.9) |
| 5–6 per week | 3 (0.8) | 2 (0.6) |
| 1 per day | 19 (5.1) | 14 (4.0) |
| 2–3 per day | 6 (1.6) | 6 (1.7) |
| 4–5 per day | 2 (0.5) | 0 (0.0) |
| 6+ per day | 1 (0.3) | 1 (0.3) |
| Spirits | ||
| < once per month | 244 (65.9) | 220 (62.1) |
| 1–3 per month | 44 (11.9) | 47 (13.3) |
| 1 per week | 33 (8.9) | 28 (7.9) |
| 2–4 per week | 24 (6.5) | 29 (8.2) |
| 5–6 per week | 5 (1.4) | 5 (1.4) |
| 1 per day | 15 (4.1) | 19 (5.4) |
| 2–3 per day | 5 (1.4) | 4 (1.1) |
| 4–5 per day | 0 (0.0) | 2 (0.6) |
| 6+ per day | 0 (0.0) | 0 (0.0) |
All values represent numbers (percentages).
For beer, X2 = 12.49, p = 0.13. For wine, X2 = 11.97, p = 0.15. For spirits, X2 = 4.45, p = 0.73.
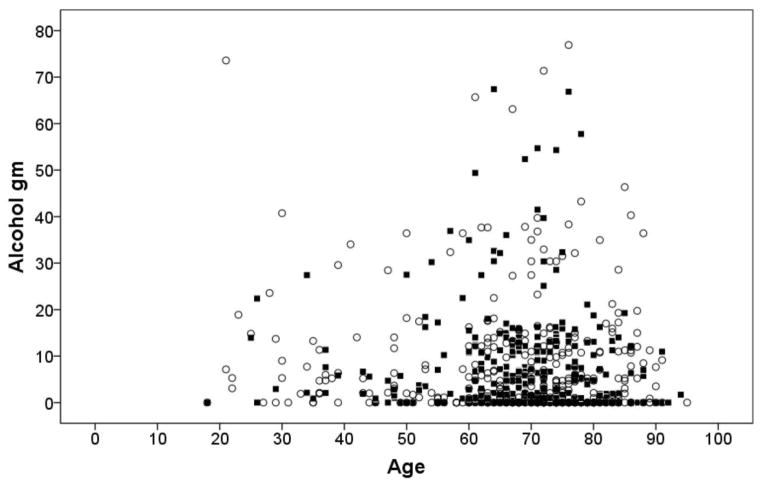
The average daily ethanol intake was numerically higher in ET cases than controls (7.99 ± 12.39 [median = 3.03] vs. 6.55 ± 10.62 [median = 1.80] gm), but this difference did not reach significance (Mann-Whitney = 1.44, p = 0.15) (Figure 1). Stratifying the sample by decade of current age (≤40, 40 – 49, 50 – 59, 60 – 69, ≥70 years) did not reveal any significant case-control differences in average daily ethanol intake (data not shown). Among the 473 subjects who drank any ethanol, we created ethanol consumption quartiles (≤2 gms/day, 3–7 gms/day, 8–14 gms/day, ≥15 gms/day), and results were marginally significant (X2 = 6.62, p = 0.085, Table 3), with greater consumption among ET cases. In a logistic regression model (outcome = diagnosis) restricted to 473 subjects who drank any ethanol, ET cases were 74% more likely than controls to be in the highest than lowest quartile (odds ratio [OR] = 1.74, 95% confidence interval [CI] = 1.02 – 2.95, p = 0.04).
Figure 1.
Average current daily ethanol consumption plotted against age in ET cases (open circles) and controls (black squares).
Table 3.
Ethanol Consumption Quartiles Among ET Cases and Controls who Drank Any Ethanol
| Controls | ET | |
|---|---|---|
| Lowest quartile | 63 (26.6) | 43 (18.2) |
| Second quartile | 59 (24.9) | 74 (31.4) |
| Third quartile | 61 (25.7) | 55 (23.3) |
| Highest quartile | 54 (22.8) | 64 (27.1) |
Number (percent).
ET = essential tremor
The correlates between average daily ethanol intake and demographic/clinicaI variables were assessed in controls. Average daily ethanol intake was higher in men than women (11.85 ± 14.97 [median = 7.00] in men vs. 4.50 ± 8.04 [median = 0.93] in women, Mann-Whitney = 6.65, p < 0.001) and was associated with higher education (Spearman’s r = 0.10, p = 0.055), white race (6.76 ± 10.83 [median = 1.90] in whites vs. 3.72 ± 6.64 [median = 0.00] in non-whites, Mann-Whitney = 2.07, p = 0.039), lower BMI (Spearman’s r = −0.14, p = 0.007) and higher calorie counts (Spearman’s r = 0.15, p = 0.005). There was no correlation between average daily ethanol intake and age (Spearman’s r = −0.05, p = 0.38), number of rooms in home/number of people living in home (Spearman’s r = 0.03, p = 0.51), number of live births [women] (Spearman’s r = −0.009, p = 0.090), or years since last hospitalization (Spearman’s r = 0.05, p = 0.039).
In an unadjusted logistic regression model (outcome = ET vs. control diagnosis), average daily ethanol intake was only marginally associated with diagnosis (OR = 1.011, 95% CI = 0.998 – 1.024, p = 0.097), but inclusion of items that had covaried with average daily ethanol intake in bivariate analyses (gender, education, race, calorie count, and BMI) completely attenuated this effect (OR = 1.008, 95% CI = 0.995 – 1.022, p = 0.22).
Among cases, there was no correlation between average daily ethanol intake in gms and tremor severity (total tremor score)(Spearman’s r = 0.008, p = 0.88). Average daily ethanol intake was similar in ET cases with vs. without voice tremor (p = 0.59), with vs. without jaw tremor (p = 0.22). Average daily ethanol intake did not differ by presence vs. absence of head tremor in men or women. in ET cases with voiceAverage daily ethanol intake was similar in ET cases with vs. without a first- or second-degree relative with ET or tremor (7.51 ± 11.36 [median = 3.07] vs. 8.16 ± 12.63 [median = 2.09] gm/day, Mann-Whitney = 0.089, p = 0.93).
4. Discussion
These data, on more than 700 enrollees evaluated over a nine-year period in a clinical-epidemiological study, do not support any sizable differences between ET cases and controls in terms of average daily ethanol consumption or ethanol overuse. The absence of a correlation in cases between ethanol consumption and tremor severity goes against the hypothesis that ET patients are self-medicating to a significant degree.
A notion has crept into the medical literature that ET cases drink more ethanol than controls, and that they are more likely to abuse ethanol. However, a close examination of the literature indicates that there are few data to support this belief; indeed, with the exception of a single, early case-control study, none of the subsequent 8 case-control studies noted a significant association between ET and ethanol use or misuse.3 In the initial study, of 36 hospitalized ET patients in the US and 36 patients who had been hospitalized for herniorrhaphy, there was a higher prevalence of alcohol dependence in the ET cases.4 Yet these patients were enrolled at a Veterans Administration Hospital and concerns have been raised about the applicability of these data to other settings.2 As noted above, the remaining data do not support such an association. For example, a study in Finland that assessed self-reported ethanol intake among 194 ET cases and 125 controls from the population found that the frequency and amount of alcohol intake was largely similar.7 A study in the US of 30 ET cases, 30 patients with other tremor disorders, and 60 patients with chronic neurological diseases without tremor indicated no differences in ethanol consumption; only 3.3% of ET cases were considered chronic alcoholics compared to 18.3% of patients with chronic neurological diseases without tremor.23 Our prior publication, which reported the results on the first 130 ET cases and 175 controls enrolled in this study, similarly did not detect a case-control difference in ethanol consumption.5 Finally, a study of blood and urinary biomarkers of ethanol intake in 95 ET cases and 35 controls in the Czech Republic did not reflect case-control differences.6 A study in Spain noted an association between baseline consumption of ethanol and risk of incident ET;24 unlike the other studies discussed above, this was a prospective study assessing the role of ethanol as a risk factor for ET.
We also report that ET cases with affected relatives did not differ from those with sporadic ET in terms of ethanol consumption. We are unaware of other data on this topic. BMI was lower in ET cases than controls. This has been reported previously.25, 26
This study was not without limitations. First, we used the Willett Semi-Quantitative Food-Frequency Questionnaire9 to assess current ethanol intake but we did not collect data on pre-disease or past ethanol intake. Second, ethanol consumption was by self- report and could have been under-reported; however, this was equally true in both cases and controls and is not likely to have influenced the results of our case-control comparisons. It is possible that our study under-enrolled alcoholics, as these individuals might have been less likely to visit their doctor, volunteer for studies or cooperate with study protocols; nonetheless, this under-enrollment would have affected alcoholic cases and controls equally, and would not have affected our case-control comparisons. The study also had considerable strengths, including its unprecedented sample size, the uniform collection of data using a reliable and valid food frequency questionnaire, the careful matching of cases to controls who were similar with respect to demographic and socioeconomic indicators, the analysis that assessed the correlation between ethanol intake and a clinical measure of tremor severity, and the adjustment for potential confounding factors in our analyses.
In summary, despite an entrenched notion in the medical literature that there is an association between greater daily ethanol consumption and ET as well as an association between ethanol overuse and ET, the published data, from a variety of sources, do not support this notion.
Highlights.
Published data on ethanol consumption in essential tremor are limited/conflicted.
We assessed ethanol consumption in a large sample of 354 cases and 370 controls.
We did not detect any sizable case-control differences in daily consumption.
There was no correlation in cases between ethanol consumption and tremor severity.
These data go against the notion that patients are extensively self-medicating.
Acknowledgments
Dr. Louis has received research support from the National Institutes of Health: NINDS #R01 NS042859 (principal investigator), NINDS #R01 NS39422 (principal investigator), NINDS #R01 NS086736 (principal investigator), NINDS #R01 NS073872 (principal investigator), NINDS #R01 NS085136 (principal investigator), NINDS #T32 NS07153-24 (principal investigator), NINDS #R21 NS077094 (co-Investigator), and NINDS #R01 NS36630 (co-Investigator). He has also received support from Parkinson’s Disease Foundation, the Arlene Bronstein Essential Tremor Research Fund (Columbia University), and the Claire O’Neil Essential Tremor Research Fund (Columbia University). He also acknowledges the support of NIEHS P30 ES09089 and the Irving Institute for Clinical and Translational Research: UL1 TR000040.
Footnotes
Conflicts of Interest:
The authors declare that there are no conflicts of interest and no competing financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Growdon JH, Shahani BT, Young RR. The effect of alcohol on essential tremor. Neurology. 1975;25(3):259–262. doi: 10.1212/wnl.25.3.259. [DOI] [PubMed] [Google Scholar]
- 2.Hess CW, Saunders-Pullman R. Movement disorders and alcohol misuse. Addict Biol. 2006;11(2):117–125. doi: 10.1111/j.1369-1600.2006.00017.x. [DOI] [PubMed] [Google Scholar]
- 3.Mostile G, Jankovic J. Alcohol in essential tremor and other movement disorders. Mov Disord. 2010;25(14):2274–2284. doi: 10.1002/mds.23240. [DOI] [PubMed] [Google Scholar]
- 4.Schroeder D, Nasrallah HA. High alcoholism rate in patients with essential tremor. Am J Psychiatry. 1982;139(11):1471–1473. doi: 10.1176/ajp.139.11.1471. [DOI] [PubMed] [Google Scholar]
- 5.Louis ED, Jurewicz EC, Applegate L, Luchsinger JA, Factor-Litvak P, Parides M. Semiquantitative study of current coffee, caffeine, and ethanol intake in essential tremor cases and controls. Mov Disord. 2004;19(5):499–504. doi: 10.1002/mds.20035. [DOI] [PubMed] [Google Scholar]
- 6.Ulmanová O, Vinopalová M, Zima T, Růžička E. Biomarkers demonstrate increased consumption, but not abuse, of ethanol in essential tremor. J Neurol. 2012;259(6):1177–1180. doi: 10.1007/s00415-011-6323-3. [DOI] [PubMed] [Google Scholar]
- 7.Rautakorpi I, Marttila RJ, Rinne UK. Alcohol consumption of patients with essential tremor. Acta Neurol Scand. 1983;68(3):177–179. doi: 10.1111/j.1600-0404.1983.tb05345.x. [DOI] [PubMed] [Google Scholar]
- 8.Bain PG, Findley LJ, Thompson PD, et al. A study of hereditary essential tremor. Brain. 1994;117 (Pt 4):805–824. doi: 10.1093/brain/117.4.805. [DOI] [PubMed] [Google Scholar]
- 9.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 10.Louis ED, Zheng W, Jurewicz EC, et al. Elevation of blood beta-carboline alkaloids in essential tremor. Neurology. 2002;59(12):1940–1944. doi: 10.1212/01.wnl.0000038385.60538.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scarmeas N, Louis ED. Mediterranean diet and essential tremor. A case-control study. Neuroepidemiology. 2007;29(3–4):170–177. doi: 10.1159/000111579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brandt JSM, Folstein M. The telephone interview for cognitive status. Neuropsychi Neuropsychol Beh Neurol. 1988;1:111–117. [Google Scholar]
- 13.Mannino DM, Caraballo R, Benowitz N, Repace J. Predictors of cotinine levels in US children: data from the Third National Health and Nutrition Examination Survey. Chest. 2001;120(3):718–724. doi: 10.1378/chest.120.3.718. [DOI] [PubMed] [Google Scholar]
- 14.Gerbin M, Viner AS, Louis ED. Sleep in essential tremor: a comparison with normal controls and Parkinson’s disease patients. Parkinsonism Relat Disord. 2012;18(3):279–284. doi: 10.1016/j.parkreldis.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Louis ED, Applegate L, Graziano JH, Parides M, Slavkovich V, Bhat HK. Interaction between blood lead concentration and delta-amino-levulinic acid dehydratase gene polymorphisms increases the odds of essential tremor. Mov Disord. 2005;20(9):1170–1177. doi: 10.1002/mds.20565. [DOI] [PubMed] [Google Scholar]
- 16.Louis ED, Applegate LM, Rios E. Interest in participating in clinical research: A study of essential tremor patients. Mov Disord. 2007;22(1):133–138. doi: 10.1002/mds.21179. [DOI] [PubMed] [Google Scholar]
- 17.DeLia D. Distributional issues in the analysis of preventable hospitalizations. Health Serv Res. 2003;38(6 Pt 2):1761–1779. doi: 10.1111/j.1475-6773.2003.00201.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16(5):622–626. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 19.Louis ED, Ford B, Bismuth B. Reliability between two observers using a protocol for diagnosing essential tremor. Mov Disord. 1998;13(2):287–293. doi: 10.1002/mds.870130215. [DOI] [PubMed] [Google Scholar]
- 20.Louis ED, Wendt KJ, Albert SM, Pullman SL, Yu Q, Andrews H. Validity of a performance-based test of function in essential tremor. Arch Neurol. 1999;56(7):841–846. doi: 10.1001/archneur.56.7.841. [DOI] [PubMed] [Google Scholar]
- 21.Louis ED, Zheng W, Applegate L, Shi L, Factor-Litvak P. Blood harmane concentrations and dietary protein consumption in essential tremor. Neurology. 2005;65(3):391–396. doi: 10.1212/01.wnl.0000172352.88359.2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harasymiw JW, Bean P. Identification of heavy drinkers by using the early detection of alcohol consumption score. Alcohol Clin Exp Res. 2001;25(2):228–235. [PubMed] [Google Scholar]
- 23.Koller WC. Alcoholism in essential tremor. Neurology. 1983;33(8):1074–1076. doi: 10.1212/wnl.33.8.1074. [DOI] [PubMed] [Google Scholar]
- 24.Louis ED, Benito-León J, Bermejo-Pareja F. Population-based study of baseline ethanol consumption and risk of incident essential tremor. J Neurol Neurosurg Psychiatry. 2009;80(5):494–497. doi: 10.1136/jnnp.2008.162701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dogu O, Sevim S, Louis ED, Kaleagasi H, Aral M. Reduced body mass index in patients with essential tremor: a population-based study in the province of Mersin, Turkey. Arch Neurol. 2004;61(3):386–389. doi: 10.1001/archneur.61.3.386. [DOI] [PubMed] [Google Scholar]
- 26.Louis ED, Marder K, Jurewicz EC, Watner D, Levy G, Mejia-Santana H. Body mass index in essential tremor. Arch Neurol. 2002;59(8):1273–1277. doi: 10.1001/archneur.59.8.1273. [DOI] [PubMed] [Google Scholar]