Abstract
Pain is highly prevalent in healthcare settings, however disparities continue to exist in pain care treatment. Few studies have investigated if differences exist based on patient related characteristics associated with aging. The objective of this study was to determine if there are differences in acute pain care for older versus younger patients. This was a multicenter, retrospective, cross-sectional observation study of 5 emergency departments across the US evaluating the 2 most commonly presenting pain conditions for older adults - abdominal and fracture pain. Multivariable adjusted hierarchical modeling was completed. A total of 6,948 visits were reviewed. Older (≥65 years) and oldest (≥85 years) were less likely to receive analgesics when compared to younger patients (<65 years), yet older patients had greater reductions in final pain scores. When evaluating pain treatment and final pain scores, differences appeared to be based on type of pain. Older abdominal pain patients were less likely to receive pain medications, while older fracture patients were more likely to receive analgesics and opioids when compared to younger patients. Differences in pain care for older patients appear to be driven by type of presenting pain.
Keywords: acute pain care, emergency department, geriatrics
1. INTRODUCTION
Disparities in the treatment of pain have been found across a spectrum of settings, conditions, and patient populations with most studies focusing on gender, racial and ethnic differences in care.[1; 4; 6; 7; 13; 17; 20] There has been less attention placed on differences that may exist based on age, in particular for older adults. With our aging population[5] and the greater prevalence of pain in this vulnerable cohort (up to 74% of community dwelling older adults reported pain in last 30 days)[18], there will be increasing demand and a need to address and improve the quality of pain care older adults receive.
Pain is one of the most common complaints clinicians encounter, especially in the emergency department (ED) where it is present in up to 78% of visits.[22] Data on the effect of age on acute pain assessment and management are conflicting and arise from studies of single health care settings or cities or conversely used national databases[11; 16] that did now allow for detailed review of acute pain care processes (e.g., documentation of pain levels, treatment of pain with analgesics, times to these processes, types of analgesics ordered, etc.). To date, no multicenter study has investigated patient related characteristics associated with acute pain care processes and how these differences may impact patient pain outcomes for older patients.
The objective of this study was to compare the quality of acute pain care in older versus younger adults and determine if differences exist based on patient characteristics and presenting condition. Understanding factors associated with acute pain treatment and whether or not these influence pain care processes will allow for the identification and subsequent targeting of factors to reduce pain and improve overall patient care.
2. METHODS
2.1.1 Design and Setting
This was a multi-center, retrospective, cross-sectional observational study of adult patients who presented with fractures or abdominal pain to 5 EDs across the United States. Four of the sites were considered urban, one suburban; 4 were in academic, tertiary care hospitals, while one was at a community hospital. Two sites were located in the Northeast region of the US, one in the Mid-Atlantic, one in the Rocky Mountain region, and one on the West Coast. To account for seasonal variation, included in the review were all adult visits made during the months of January, April, July and October of 2009 (January 1–January 31, 2009, April 1–April 31, 2009, July 1–July 31, 2009, and October 1–October 31, 2009). This study received IRB approval with waiver of informed consent at all 5 sites.
2.1.2. Data collection
All 5 EDs utilize comprehensive electronic health records (EHR)(4 utilized ED Pulsecheck, PICIS, Inc. Wakefield, MA; 1 utilized Epic ASAP, Epic Systems Corporation, Verona, WI) for electronic patient tracking, physician and nursing documentation, and order entry. As such, all data entered into the systems at these 5 EDs are time stamped, and patient charting is organized according to presenting condition. Patient-related and pain care data were collected using both chart review and administrative reports that were created and shared at sites utilizing the same EHR, or standardized to match at the one site that utilized Epic. For chart review, the site-investigator at each site trained research assistants (RAs) to extract all data following 12 recommended criteria for medical record review studies.[24] All RAs had at least a 4-hour training session of the ED EHR process, shadowed the chart review process of the investigator, did test chart abstractions that were compared to those of the investigators, and were deemed qualified to abstract independently when test abstractions were completed with 95% agreement. These methods have been previously utilized and described by investigators for other studies evaluating the quality of ED pain care.[9; 10] RAs were blinded to the study hypothesis.
2.2 Participants
The cohort was comprised of adults aged 18 or older who presented to the ED with a chief complaint of pain and received a final primary diagnosis of the two most commonly presenting ED pain conditions, abdominal pain or fracture pain.[10] As had been done successfully in a previous study,[10] an automated text filter algorithm (Microsoft Excel, Microsoft Corp.) of the chief complaint and ED diagnosis was used and included the following words: “abd,” “-ache,” “appendicitis,” “appendix,” “arthritis,” “biliary,” “burn,” “cancer,” “cholangitis,” “cholecystitis,” “colic,” “colitis,” “contusion,” “Crohn,” “diverticulitis,” “epigastric,” “fall,” “fell,” “flank,” “fracture,” “fx,” “gout,” “hernia,” “injury,” “meniscus,” “kidney,” “lithiasis,” “obstruction,” “pain,” “pancreatitis,” “perforation,” “problem,” “pyelonephritis,” “sprain,” “stone,” “strain,” “tear,” “tendon.” Those with fracture pain had a final ED diagnosis of a confirmed fracture.
2.3 Measures
2.3.1 Variables Studied
The primary patient-related predictor studied was age, which was categorized into younger (18 to 64 years), older (65–84 years), and oldest (85 and older years). Covariates were selected based on construct validity or using evidence-based review of the literature for factors known to be associated with the quality of pain care received.[1; 4; 6; 7; 10; 13; 17; 20] The following covariates were included in adjusted analyses: initial reported pain score (0 to 10 with 0 = none to 10 = worst pain or severe)(i.e., if a patient reported no initial ED pain, it would be reasonable to account for this in whether they did not receive any analgesics), gender, race/ethnicity (white, black, Hispanic, Asian, other), number of prior medications, triage score (Emergency Severity Index (ESI), 1 = urgent, 5 = nonurgent),[25] and Charlson comorbidity score.[3] Additional pain covariates included in adjusted analyses were categorization of final ED diagnosis for type of fracture (long, short, facial bone) or abdominal pain (non-specific abdominal pain, appendicitis, biliary, bowel obstruction, cancer, colitis, constipation, flank pain, hernia, musculoskeletal, non-abdomen related (e.g., chest pain), ob/gyn, pancreatic, urology related,) based on final ED diagnoses, and admission status as a surrogate for longer times patient may have remained in the ED and acuity of their diagnosis. All variables that were continuous in nature (i.e., pain score 0–10, number of prior medications, ESI, Charlson score) were treated as continuous variables in adjusted analyses.
2.3.2 ED analgesic administration
Pain treatment outcomes were evaluated. These included whether analgesics were given, and if so initial type of analgesic received (opioids vs. non-steroidal anti-inflammatory drugs (NSAIDs) vs. others vs. none). Opioids included codeine, fentanyl, hydromorphone, morphine, oxycodone, propoxyphene, as well as a combination opioid and nonopioid medications such as acetaminophen/oxycodone. NSAIDs included aspirin, cyclooxygenase-2 inhibitors, ibuprofen, indomethacin, naproxen, and ketorolac. "Other" medications included acetaminophen; specifically for abdominal pain patients, this included antacids, H1-receptor antagonists, and proton pump inhibitors. For subjects that received any opioid, equianalgesic doses were calculated using standard conversions.[23]
2.3.3 Final and reduction in pain scores
All sites utilized a 0-to-10 verbal numeric rating scale to assess patients’ pain severity. The initial pain score was considered to be the first pain score recorded in the EHR while the final pain score was the last score recorded before discharge from the ED or admission. Overall reduction in pain scores was calculated by subtracting the final pain score from the initial pain score. Both final pain score and overall reduction in pain score were used as a patient pain care outcome.
2.4 Data analyses
Descriptive analyses were completed of the cohort by age category and stratified by pain condition (fracture versus abdominal pain). Univariate comparisons of the primary predictor (age category) and covariates were run against pain care outcomes. Those found significant (p≤0.05) or with construct validity (gender, race/ethnicity, Charlson score, number of medications) [1; 4; 6; 7; 10; 13; 17; 20] were included in adjusted analyses. Multivariable adjusted hierarchical modeling clustered by clinician and site level were performed for pain care outcomes using both mixed linear and General Estimating Equation regression models in which the age category "young" was used as the referent comparison group. All analyses were completed in SAS version 9.3 (SAS Institute, Inc. Cary, NC).
3. RESULTS
3.1 Cohort characteristics
A total of 94,264 adult patients (>18 years age) were seen at the 5 EDs during the study period. Of these, a total of 23,205 (24.6%) visit were for painful conditions (using both chief complaint AND final ED diagnosis of painful conditions) of any type. Thirty percent of these, 6,948 visits, were of abdominal or fracture pain. The characteristics of the study cohort can be found in Table 1. There were significant differences by age category based on gender, race/ethnicity, ESI, number of current medications, Charlson comorbidity scores, admission status, and final ED diagnoses of the abdominal or fracture pain. [An overview of the study cohort characteristics arranged by site is available upon request from the corresponding author.]
Table 1.
Patient characteristics by age category (n = 6948).
| Characteristics | Young* (<65 years) n = 5896 (85) |
Older* (65–84 years) n = 828 (12) |
Oldest* (≥85 years) n = 224 (3) |
p value |
|---|---|---|---|---|
| Female | 3416 (58) | 529 (64) | 164 (73) | <0.0001 |
| Race/ethnicity White Black Hispanic Other/Unknown |
2523 (43) 1286 (22) 1368 (23) 719 (12) |
393 (47) 155 (19) 183 (22) 97 (12) |
144 (64) 27 (12) 38 (17) 15 (7) |
<0.0001 |
| ESI, mean (SD) [1=acute, 5=non-acute] | 3.07 (0.53) | 2.93 (0.54) | 2.73 (0.48) | <0.0001 |
| Number of current medications, mean (SD) | 1.95 (3.28) | 4.02 (4.08) | 4.90 (4.22) | <0.0001 |
| Charlson comorbidity score, mean(SD) | 0.56 (1.40) | 1.31 (1.66) | 1.38 (1.54) | <0.0001 |
| Admission status | 2964 (50) | 515 (62) | 178 (79) | <0.0001 |
| Abdominal pain, n = 5224 (75) | 4557 (77) | 550 (67) | 117 (52) | |
| Abdominal pain final diagnoses,order of most to least commonn=5224 |
|
|
|
<0.0001 |
| Fracture pain, n = 1722 (25) | 1338 (23) | 277 (33) | 107 (48) | |
| Fracture final diagnoses, order of most to least common, |
|
|
|
<0.0001 |
ESI = Emergency Severity Index
All values are reported as n(%) except for ESI, Charlson comorbidity score, and Number of current medications.
3.2 Analgesic use
Analgesic administration varied by age and condition. When comparing analgesic used by age, older and oldest adults were the less likely to have received any analgesic medication [64% for oldest (p=0.0040) and 69% for older adults (p=0.0021) versus 74% of younger adults in adjusted analyses] and the oldest were least likely to received any opioid [50% of oldest adults (p=0.0132) when compared to 57% of younger adults]. Older and oldest patients received lower total morphine equivalent doses of analgesics when compared to younger patients. [3.42mg ± 5.42 for older (p<0.0001) and 2.61 ±mg 3.90 for oldest (p<0.0001) when compared to 3.99mg ± 5.72 for younger adults] (Table 2) Abdominal pain patients were more likely to receive analgesic medications (74%) when compared to fracture patients (69%)(p<0.0001). Secondary to this notable difference in analgesic administration based on condition, the cohort was stratified by type of painful condition (abdominal pain versus fracture pain).
Table 2.
Pain care outcomes for all patients by age (n = 6948).
| Outcome | Young* (<65 years) n = 5896 (85) (REF) |
Older* (65–84 years) n = 828 (12) |
p value Older compared to Young |
Oldest* (≥85 years) n = 224 (3) |
p value Oldest compared to Young |
|---|---|---|---|---|---|
| Received any analgesic medication | 4384 (74) | 573 (69) | 0.0040† | 144 (64) | 0.0021† |
| Received any opioid medication | 333 (57) | 459 (54) | 0.2779 | 113 (50) | 0.0132† |
| Total morphine equivalent dose in mg, mean (SD) | 3.99 (5.72) | 3.42 (5.42) | <0.0001† | 2.61 (3.90) | <0.0001† |
| Initial recorded pain score, mean (SD) | 7.45 (2.49) | 6.67 (3.00) | <0.0001‡ | 6.34 (2.85) | <0.0001‡ |
| Final recorded pain score, mean (SD) | 4.27 (3.30) | 3.17 (3.33) | <0.0001† | 2.27 (3.07) | <0.0001† |
| Reduction in pain score (final – initial), mean (SD) | −3.12 (3.56) | −3.42 (3.82) | 0.2680 | −3.84 (3.64) | 0.0353† |
All values are reported as n(%) except for the initial, final, and reduction in pain scores.
Statistically significant associations in multivariable hierarchical modeling when clustering by site and treating clinician and adjusting for gender, race/ethnicity, ESI, Charlson comorbidity, number of current medications, admission, and degree of initial presenting pain, when using YOUNG as referent group for comparison.
Statistically significant associations in multivariable hierarchical modeling when clustering by site and treating clinician and adjusting for gender, race/ethnicity, ESI, Charlson comorbidity, number of current medications, and admission when using YOUNG as referent group for comparison.
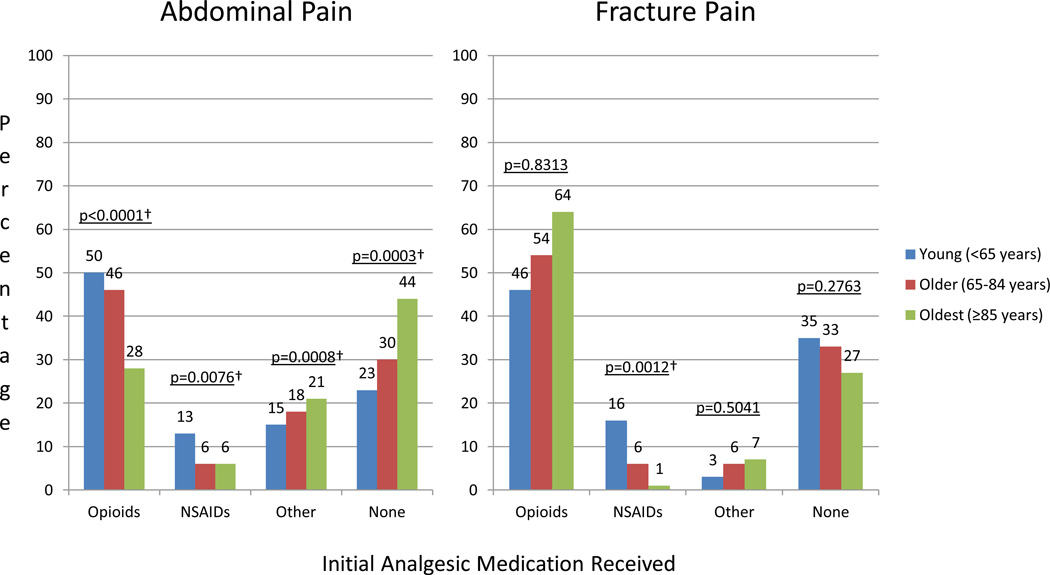
For the abdominal pain patients, pain treatment differences continued to exist when compared by age. The older and oldest abdominal pain adults were less likely to receive any analgesic medication [56% for oldest (p=0.0003) and 70% for older adults (p=0.0116) versus 77% of younger adults in adjusted analyses] or opioids [33% for oldest (p<0.0001) and 52% for older adults (p=0.0036) versus 58% of younger adults in adjusted analyses]. Older and oldest adults also received lower total morphine equivalent doses for their abdominal pain when compared to younger patients [3.19mg ± 4.42 for older (p<0.0001) and 1.90mg ± 3.34 for oldest (p<0.0001) when compared to 4.25mg ± 5.61 for younger adults]. (Table 3). For a comparison of types of initial analgesics used by age groups, see Figure 1. In adjusted analyses for abdominal pain, NSAIDs were less likely to be initially used in older and oldest adults while "other" analgesics were more used more often in older adults.
Table 3.
Pain care outcomes for abdominal pain patients by age (n = 5224)
| Outcome | Young* (<65 years) n = 4557 (87) (REF) |
Older* (65–84 years) n = 550 (11) |
p value Older compared to Young |
Oldest* (≥85 years) n = 117 (2) |
p value Oldest compared to Young |
|---|---|---|---|---|---|
| Received any analgesic medication | 3513 (77) | 386 (70) | 0.0116† | 65 (56) | 0.0003† |
| Received any opioid | 2641 (58) | 287 (52) | 0.0036† | 39 (33) | <0.0001† |
| Total morphine equivalent does in mg, mean (SD) | 4.25 (5.61) | 3.19 (4.42) | <0.0001† | 1.90 (3.34) | <0.0001† |
| Initial recorded pain score, mean (SD) | 7.61 (2.43) | 6.91 (2.89) | <0.0001‡ | 5.74 (2.82) | <0.0001‡ |
| Final recorded pain score, mean (SD) | 3.93 (3.31) | 2.60 (3.22) | <0.0001† | 1.59 (2.65) | <0.0001† |
| Reduction in pain score (final- initial), mean (SD) | −3.62 (3.63) | −4.26 (3.79) | 0.0042† | −4.03 (3.70) | 0.1323 |
All values reported as n(%) except for the initial, final, and reduction in pain scores.
Statistically significant associations in multivariable hierarchical modeling when clustering by site and treating clinician and adjusting for gender, race/ethnicity, ESI, Charlson comorbidity, number of current medications, abdominal pain type, admission, and degree of initial presenting pain when using YOUNG as referent group for comparison.
Statistically significant associations in multivariable hierarchical modeling when clustering by site and treating clinician and adjusting for gender, race/ethnicity, ESI, Charlson comorbidity, number of current medications, abdominal pain type, and admission when using YOUNG as referent group for comparison.
Figure 1.
Comparison of initial analgesic medication given to each type of presenting pain according to age category (n=6,948) NSAIDs = nonsteroidal anti-inflammatory drugs.
†Statistically significant associations in multivariable hierarchical modeling when clustering by site and treating clinician and adjusting for gender, race/ethnicity, ESI, presenting pain, Charlson comorbidity score, number of current medications, abdominal pain or fracture type, admission, and degree of initial pain when using YOUNG as referent group for comparison.
In contrast, fracture pain in older and oldest adults appeared to receive more analgesics and more opioids when compared to younger patients. These associations, however, were not statistically significant in adjusted analyses. (Table 4 and Figure 1) The only statistically significant associations were that NSAIDs were less likely to be used in older and oldest fracture patients and the oldest patients received higher total morphine equivalent doses for their fracture pain than to younger patients (3.38 ± 4.32 vs. 3.10 ±5.99). (Table 4)
Table 4.
Pain care outcomes for fracture pain patients by age (n = 1,722)
| Outcome | Young* (<65 years) n = 1338 (78) (REF) |
Older* (65–84 years) n = 277 (15) |
p value Older compared to Young |
Oldest* (≥85 years) n = 107 (6) |
p value Oldest compared to Young |
|---|---|---|---|---|---|
| Received any analgesic medication | 871 (65) | 187 (67) | 0.2926 | 79 (74) | 0.2763 |
| Received any opioid | 695 (52) | 163 (59) | 0.5401 | 74 (69) | 0.3875 |
| Total morphine equivalent dose in mg, mean (SD) | 3.10 (5.99) | 3.89 (6.97) | 0.4387 | 3.38 (4.32) | 0.0004† |
| Initial recorded pain score, mean (SD) | 6.87 (2.61) | 6.19 (3.13) | <0.0001‡ | 6.96 (2.75) | 0.1465 |
| Final recorded pain score, mean (SD) | 5.44 (2.98) | 4.30 (3.28) | 0.0134† | 3.05 (3.33) | <0.0001† |
| Reduction in pain score (final -initial), mean (SD) | −1.42 (2.73) | −1.79 (3.32) | 0.9967 | −3.64 (3.59) | 0.0290† |
All values reported as n(%) except for the initial, final, and reduction in pain scores.
Statistically significant associations in multivariable hierarchical modeling when clustering by site and treating clinician and adjusting for gender, race/ethnicity, ESI, Charlson comorbidity, number of current medications, fracture type, admission and degree of initial presenting pain when using YOUNG as referent group for comparison.
Statistically significant associations in multivariable hierarchical modeling when clustering by site and treating clinician and adjusting for gender, race/ethnicity, ESI, Charlson comorbidity, number of current medications, fracture type, and admission when using YOUNG as referent group for comparison.
3.3 Pain scores
When comparing the patients by age group, younger patients reported a higher average initial pain score (7.45 ± 2.49) while oldest adults reported the lowest average initial pain score among the three age categories (6.34 ± 2.85, p <0.0001, Table 2). Younger adults also reported a higher average final pain score (4.27 ± 3.30) when compared to older (3.17 ± 3.33, p<0.0001) and oldest adults (2.27 ± 3.07, p<0.0001) in adjusted analyses. Oldest adults had the greatest reduction from initial to final recorded pain score (younger adults had a mean pain score reduction of −3.12 ± 3.56, vs −3.42 ± 3.82 for older adults and - 3.84 ± 3.64 for oldest adults, p<0.01). The differences in reduction of pain score, however only remained statistically significant in adjusted analyses for oldest patients. (Table 2)
When comparing the patients by presenting type of pain, differences in the pain score trends were seen (Tables 3 and 4). For abdominal pain patients, younger adults continued to report a higher average initial pain score [mean 7.61 ± 2.43, compared to 6.91 ± 2.89 for older adults (p<0.0001 in adjusted analyses) and 5.74 ± 2.82 for oldest adults (p<0.0001 in adjusted analyses)]. In contrast to abdominal pain patients, oldest adults with fracture reported a higher average initial pain score (6.96 ± 2.75, vs. 6.87 ± 2.61 for younger adults), but this was not significant in adjusted analyses (p=0.1465), and older adults had lower initial pain scores (6.19 ± 3.13, p<0.0001 in adjusted analyses compared to younger patients). As was seen in the overall cohort, the oldest and older adults in the fracture pain cohort had the greatest reduction from initial to final pain scores (−3.64 ± 3.59, p=0.0290 for oldest and −1.79 ± 3.32, p=0.9967 for older adults in adjusted analyses, vs. −1.42 ± 2.73 for younger adults), while the older adults in the abdominal pain cohort had the greatest reduction (−4.26 ± 3.79, p=0.0042 in adjusted analyses vs. −4.03 ± 3.70 for oldest adults, p=0.1323 in adjusted analyses when compared to −3.62 ± 3.63 for younger adults).
For ease of interpretation, all results presented in tables and the figure are of univariate outcomes comparing older and oldest to young as the referent group. P-values included are of multivariable hierarchical modeling of age as an ordinal predictor variable of pain care outcomes.
3.4 Multivariable adjusted hierarchical modeling
In multivariable hierarchical modeling clustered by site and treating clinician and adjusting for gender, race/ethnicity, ESI, Charlson comorbidity score, number of current medications, admission status, type of abdominal or fracture condition based on ED final diagnosis, and initial presenting pain score (for those outcomes that did not include the initial pain score value), it became apparent that pain care varied not only based on age, but was also influenced by the type of presenting pain.
For example, a examination of the least squares means indicated that when older patients (65–84 years age) were compared to younger patients (<65 years age) for the entire cohort, younger patients were significantly more likely [z=2.88; p<0.01; OR =1.32 (CI 1.09, 1.59)] to receive analgesics. Comparison of the young to oldest (>85 years age) also remained statistically significant [z=3.07; p<0.01; OR=1.73 (CI 1.22, 2.45)]. When older patients were compared to oldest patients, there was no significant different in their receiving analgesics (p=0.13). When comparing reduction of pain scores for the entire cohort, only the oldest patients had the greatest reduction in pain when compared to younger patients [young compared to oldest, t(4700)=2.48, adjusted p=0.01; but not when young was compared to older, t(4700)=1.55, adjusted p=0.12], or older to oldest patients [t(47000)=1.48, adjusted p=0.30].
For abdominal pain, a examination of the least squares means indicated younger patients were significantly more likely [z=2.52; p=0.01; OR =1.36 (CI 1.07 1.73)] to receive analgesics than older patients. Comparison of young to oldest (>85 years age) also remained statistically significant [z=3.59; p<0.001; OR=2.51 (CI 1.52, 4.15)]. Older abdominal patients were more likely to receive analgesics than the oldest (z=2.36; p=0.02; OR=1.85 (CI 1.11, 3.07). Despite these differences in analgesics for older and oldest patients with abdominal pain, older patients were the only ones found to have a statistically significant greater reduction in pain scores in adjusted analyses when compared to younger patients for abdominal pain [young compared to older t(3135)=3.18, adjusted p<0.01.]. There were no statistically significant differences between younger and oldest (adjusted p=0.13) and older and oldest patients in abdominal pain reduction (adjusted p=0.99).
Consistent with reported univariate analyses, an examination of whether or not fracture patients received analgesics found no statistically significant differences in least square means when comparing across all age categories (young compared to older p=0.29, young compared to oldest p=0.28, older compared to oldest p=0.67). Despite no differences in adjusted analyses of receiving analgesics opioids, oldest fracture patients received a statistically significant higher total morphine equivalent dosage when compared to young patients [t(1239)=3.82, adjusted p<0.001] and had a significant difference in reduction in pain scores for fracture pain [oldest compared to young t(1157)=2.55, adjusted p=0.03; oldest compared to older t(1157)=2.42, adjusted p=0.04]. There were no significant differences in pain score reductions for young compared to older (adjusted p=0.99).
4. DISCUSSION
The results of this multicenter observational study demonstrate differences in pain and acute pain care for older ED patients when compared to younger patients, but also indicate that phenomenon is quite complex. At first glance, older adults (65–84) and oldest adults (≥85) who presented to the ED with a painful condition were less likely than younger adults (18–64) to have received any analgesic medication. Of those who did receive analgesics, older and oldest adults were less likely than younger adults to receive opioids and lower total morphine equivalent doses of these. As such, it would appear that older adult patients, in general, receive less pain care in the ED. They receive fewer analgesics overall and fewer opioids than younger patients. (Table 2)
These results are consistent with those from recent studies demonstrating differences in pain care for older adults who present to the ED with a painful condition. Platts-Mills et al.[16] found that patients aged ≥75 years who visited the ED for a painful condition were less likely to receive analgesics than younger patients aged 35 to 54 years and less likely to receive opioids or NSAIDs. Mills et al.[14] studied older ED adults with either abdominal or back pain and found these patients also less likely to receive analgesic medication than younger patients. Finally, Hwang et al.[10] found that when compared to younger patients, older patients presenting with all types of pain in the ED were less likely to receive any opioids and had lower overall reductions of pain scores.
Distinctions in pain and pain treatment patterns began to rise in this study, however, when evaluating by type of presenting pain and using multivariable adjusted hierarchical modeling. Older and oldest adults presenting with abdominal pain were less likely to receive any analgesics, any opioids, and lower total doses of opioids for their pain and these associations persisted in adjusted analyses (Table 3). In contrast, older and oldest adults with fracture pain appeared to receive better pain care than younger patients. More older and oldest adults received pain medications or opioids than younger patients. (Table 4) In adjusted analyses, however, these differences were no longer statistically significant. Not surprisingly, when comparing patients on the basis of presenting pain condition without separating them into age categories, differences in analgesic administration appeared to be driven by the type of pain. Patients (≥18yrs) who presented to an ED with abdominal pain were more likely to receive analgesics (74%) than patients who presented with fracture pain (69%). Almost one-third of fracture pain patients did not receive any analgesics compared to a quarter of abdominal pain patients. These are somewhat unexpected findings given the generally overt presentation of fracture pain, and the longstanding controversial belief that treating abdominal pain might mask diagnoses.[21] It is assumed pain treatment for acute musculoskeletal conditions such as fracture would receive better pain care and be treated immediately versus abdominal pain, which can present in many forms and have multiple etiologies. Yet these findings are consistent with previous reports indicating patients with fracture pain are often poorly managed within the ED with respect to receiving analgesics.[2; 15; 19]
This study is novel in that it compares and contrasts the acute treatment of different types of commonly presenting ED pain conditions. These data shed findings that different pain types are treated differentially in an age-dependent manner. To further investigate these associations, the study accounted for multiple patient-related confounders including final ED abdominal pain or fracture diagnoses and whether or not a patient may have been admitted to the hospital. As can be found in Table 1, the definitive etiology for the cause of the abdominal or fracture pain varied by age group. Unfortunately for more than half of abdominal patients in all age groups, no causative diagnoses were made. Fifty-four percent of younger patients, 55% older patients, 61% oldest patients left the ED with an nonspecific "abdominal pain" diagnosis. Other notable points include the increasing prevalence of certain diagnoses such as bowel obstruction and pancreatic related abdominal pain for older adults, while younger adults had more urology-related problems. For fracture pain, older adults were more likely to have long bone fractures (68% and 88% of older and oldest patients when compared to only 46% of younger patients).
The differences in pain etiology of abdominal and fracture pain accounted for differences in ED pain care by age group in adjusted analyses. This was apparent in fracture pain treatment, where older patients appeared to receive "better" pain care in terms of more analgesics and more opioids when compared to younger patients. This association, however, disappeared when type of fracture was accounted for in adjusted analyses. This latter finding is in contrast to those reported by Jones et al.[12] and Brown et al.[2] In these studies, older patients who presented to the ED with fracture pain were significantly less likely than younger adults to receive any analgesic medication or to receive a narcotic. It is possible that "better" or equivalent pain care for older adults in this study may be due to the emerging awareness over the past decade that fracture pain had been inadequately managed in the ED. Similarly, our data on analgesic use for abdominal pain are consistent with those from previous studies whereby older adults were less likely to receive any analgesics.[10; 14] As evident in the wide ranging abdominal pain diagnoses for this cohort, the (in)ability to identify the cause of pain may impact the quality of pain care received.
In considering differences in pain treatment for both conditions, there were equivocal findings in pain score reductions for older and younger patients. In general, older and oldest patients appeared to have lower initial and final pain scores when compared to younger patients, despite receiving fewer analgesics. While this finding would appear counterintuitive given the etiology of the presenting pain (e.g.., more bowel obstruction, or long-bone fractures in older and oldest adults than younger) there are some important considerations to take into account when interpreting this. First, older adults may believe that pain is a normal part of aging and therefore should be accepted with minimal to no complaints.[8] It has been shown that adults ≥60 years exhibit an age-related increase in reticence to report pain as well as increased uncertainty and conservatism in evaluating painful sensations.[26] This may account for why older adults presented with lower initial pain scores than did younger adults for all types of pain. (Table 2)
Our finding of lower final pain scores in most older patients despite receiving fewer analgesics raises several implications and questions about acute pain care. The first is that pain should be appropriately managed while determining pain etiology. Clinicians should work aggressively using the history, physical exam, and diagnostic procedures to identify and treat the etiology of the pain, but not forget to treat pain. While it could be hypothesized that for many of the abdominal pain patients, treatment of the cause (e.g., IV hydration and gastric decompression for obstruction) may have facilitated the reduction of pain scores, for the majority of the study patients (i.e., abdominal pain) a final diagnosis was never determined. A second consideration is if improvement in pain scores is to be used as a process measure of pain care quality, it would be reasonable to conclude that better quality pain care (i.e., more analgesics) may be associated with achieving lower pain scores. Oldest adults fracture patients received higher total morphine equivalent doses than younger patients; older patients had statistically significant greater final pain score reductions, even when accounting for type of fracture pain.(Table 4) Finally (as a corollary), if self-reported pain is the gold standard outcome for pain care and older patients had lower final pain scores, were younger adults in this study undertreated for pain? Further investigation should evaluate the complex nature of age-related pain, the conditions associated with pain, and how these are associated.
Limitations of this study include its retrospective design. Patient factors not easily ascertained with chart review, such as cognitive impairment or if a patient declined pain treatment could not be evaluated. Prospective data collection assessing patient and clinician perceptions of pain and pain care would enable better interpretation of pain scores and pain care outcomes. A more detailed evaluation comparing pain care for the range of pain diagnoses (i.e., urologic pain versus obstruction pain, long-bone versus short-bone fracture) is also further warranted. This, however, is beyond the scope of this study.
In conclusion, differences in acute pain and pain care exist based on age. The direction of age-related differences in pain treatment appear to vary on type of presenting pain and etiology of pain. Not all pain is treated equally and pain outcomes vary by condition and age. Future studies assessing the quality of acute pain care and differences that may occur should also take into account the type of pain and pain conditions that are evaluated. Understanding why older abdominal patients are medicated differently, yet in an age-dependent manner have improved pain scores remains elusive and warrants continued investigation.
Acknowledgements
Ula Hwang was supported by a K23 award from the National Institute on Aging (K23 AG031218); R. Sean Morrison by a K24 from the National Institute on Aging (K24 AG022345).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest.
References
- 1.Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111(1):52–58. doi: 10.1093/bja/aet127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown J, Klein E, Lewis C, Johnston B, Cummings P. Emergency department analgesia for fracture pain. Ann Emerg Med. 2003;42:197–205. doi: 10.1067/mem.2003.275. [DOI] [PubMed] [Google Scholar]
- 3.Charlson M, Pompei P, Ales K, MacKenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 4.Cintron A, Morrison RS. Pain and ethnicity in the United States: A systematic review. J Palliate Med. 2006;9(6):1454–1473. doi: 10.1089/jpm.2006.9.1454. [DOI] [PubMed] [Google Scholar]
- 5.Federal Interagency Forum on Aging-Related Statistics, editor. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key Indicators of Well-Being. Washington, DC: U.S. Government Printing Office; 2012. Jun, pp. 1–200. [Google Scholar]
- 6.Green C, Anderson K, Baker T, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4:277–294. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 7.Heins J, Heins A, Grammas M, Costello M, Huang K, Mishra S. Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs. 2006;32:219–224. doi: 10.1016/j.jen.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Hofland SL. Elder beliefs: Blocks to pain management. J Gerontol Nurs. 1992;18(2):19–24. doi: 10.3928/0098-9134-19920601-05. [DOI] [PubMed] [Google Scholar]
- 9.Hwang U, Morrison RS, Livote E, Harris B, Spencer N, Richardson LD. Emergency department crowding and decreased quality of pain care. Acad Emerg Med. 2008;15:1248–1255. doi: 10.1111/j.1553-2712.2008.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang U, Richardson LD, Harris B, Morrison RS. The quality of emergency department pain care for older adult patients. J Am Geriatr Soc. 2010;58:2122–2128. doi: 10.1111/j.1532-5415.2010.03152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iyer RG. Pain documentation and predictors of analgesic prescribing for elderly patients during emergency department visits. J Pain Symptom Manage. 2010;41:367–373. doi: 10.1016/j.jpainsymman.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 12.Jones J, Johnson K, McNinch M. Age as a risk factor for inadequate emergency department analgesia. Am J Emerg Med. 1996;14:157–160. doi: 10.1016/S0735-6757(96)90123-0. [DOI] [PubMed] [Google Scholar]
- 13.Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med. 2012;13(2):150–174. doi: 10.1111/j.1526-4637.2011.01310.x. [DOI] [PubMed] [Google Scholar]
- 14.Mills AM, Edwards JM, Shofer FS, Holena DN, Abbuhl SB. Analgesia for older adults with abdominal or back pain in emergency department. West J Emerg Med. 2011;12:43–50. [PMC free article] [PubMed] [Google Scholar]
- 15.Ngai B, Ducharme J. Documented use of analgesics in the emergency department and upon release of patietns with extremity fractures. Acad Emerg Med. 1997;1997(4):12. doi: 10.1111/j.1553-2712.1997.tb03708.x. [DOI] [PubMed] [Google Scholar]
- 16.Platts-Mills TF, Esserman DA, Brown L, Bortsov AV, Sloane PD, McLean SA. Older US emergency department patients are less likely to receive pain medication than younger patients: results from a national survey. Ann Emerg Med. 2012;60:199–206. doi: 10.1016/j.annemergmed.2011.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rupp T, Delaney K. Inadequate analgesia in emergency medicine. Ann Emerg Med. 2004;43:494–503. doi: 10.1016/j.annemergmed.2003.11.019. [DOI] [PubMed] [Google Scholar]
- 18.Sawyer P, Bodner EV, Ritchie CS, Allman RM. Pain and pain medication use in community-dwelling older adults. Am J Geriatr Pharmacother. 2006;4(4):316–324. doi: 10.1016/j.amjopharm.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Selbst SM, Clark M. Analgesic use in the emergency department. Ann Emerg Med. 1990;19(9):1010–1013. doi: 10.1016/s0196-0644(05)82565-x. [DOI] [PubMed] [Google Scholar]
- 20.Shavers VL, Bakos A, Sheppard VB. Race, ethnicity, and pain among the US adult population. J Health Care Poor Underserved. 2010;21:177–220. doi: 10.1353/hpu.0.0255. [DOI] [PubMed] [Google Scholar]
- 21.Silen W, editor. Title|, Vol. Volume|. City|: Publisher|, Year|. [Google Scholar]
- 22.Tanabe P, Buschmann M. A prospective study of ED pain management practices and the patient's perspective. J Emerg Nurs. 1999;25:171–177. doi: 10.1016/s0099-1767(99)70200-x. [DOI] [PubMed] [Google Scholar]
- 23.Webster LR, Fine PG. Review and critique of opioid rotation practices and associated risks of toxicity. Pain Medicine. 2012;13(4):562–570. doi: 10.1111/j.1526-4637.2012.01357.x. [DOI] [PubMed] [Google Scholar]
- 24.Worster A, Bledsoe R, Cleve P, Fernandes C, Upadhye S, Eva K. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45:448–451. doi: 10.1016/j.annemergmed.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 25.Wuerz R, Milne L, Eitel D, Gilboy N. Reliability and validity of a new five-level triage instrument. Acad Emerg Med. 2000;7:236–242. doi: 10.1111/j.1553-2712.2000.tb01066.x. [DOI] [PubMed] [Google Scholar]
- 26.Yong HH, Gibson SJ, de L, Horne DJ, Helme RD. Development of a pain attitudes questionnaire to assess stoicism and cautiousness for possible age differences. J Gerontol Psych Sci. 2001;56B(5):279–284. doi: 10.1093/geronb/56.5.p279. [DOI] [PubMed] [Google Scholar]