Abstract
Background:
Childbirth is associated with increased risk of first-time psychiatric episodes, and an unwanted pregnancy has been suggested as a possible etiologic contributor. To what extent childbirth causes psychiatric episodes and whether a planned pregnancy reduces the risk of postpartum psychiatric episodes has not been established.
Methods:
We conducted a cohort study using data derived from Danish population registers, including all women having in vitro fertilization (IVF) treatment and their partners with recorded information in the IVF register covering fertility treatments in Denmark at all public and private treatment sites from January 1994 to December 2005. We compared parents and childless persons to examine whether childbirth is directly associated with onset of first-time psychiatric episodes, with incidence rate ratios (risk of first psychiatric inpatient or outpatient treatment) as the main outcome measures.
Results:
The incidence rate for any type of psychiatric disorder 0-90 days postpartum was 11.3 per 1000 person-years (95% confidence interval = 8.2-15.0), and 3.8 (3.4-4.3) among women not giving birth. IVF-treated mothers had an increased risk of a psychiatric episode postpartum, incidence rate ratio = 2.9 (2.0-4.2) compared with the risk of psychiatric episodes in childless women. Risk of psychiatric episodes from 90 days postpartum and onwards was decreased (incidence rate ratio = 0.9 [0.7-1.0]).
Conclusions:
Using a study design paralleling a natural experiment, our results showed that childbirth is associated with first-time psychiatric disorders in new mothers, indicating that a planned pregnancy does not reduce risks of or prevent postpartum psychiatric episodes.
Childbirth is associated with a marked increase in risk of first-time episodes of psychiatric disorders.1-3 It is estimated that around 15% of new mothers have mild to moderate episodes of postpartum depression, 4 and 0.1% of new mothers experience onset with a psychiatric disorder necessitating inpatient treatment during the first postpartum months.1;3 Established risk factors for postpartum psychiatric disorders include previous history of psychiatric hospitalization, 2;5 and a family history of psychiatric episodes, especially bipolar affective disorder.6 Other proposed risk factors for postpartum depression specifically include low social support, stressful life events, and having an unplanned/unwanted pregnancy.7-9
A large proportion of pregnancies in the US and elsewhere are mistimed or unwanted.10 One US study found that 6% of pregnancies were unwanted and 30% were mistimed.11 When experiencing an unwanted pregnancy, a woman can choose to terminate or continue the pregnancy, and both of these choices have been speculated to influence women’s mental health.11-13 To what extent having an unwanted or unplanned pregnancy influences the risks of severe postpartum psychiatric disorders, and whether there is an effect over and above having an unwanted or unplanned pregnancy, is at present not known.
Couples entering in vitro fertilization (IVF) treatment are actively trying to become parents, and for this reason one can assume that all pregnancies initiated by assisted reproductive technologies are planned and intended. The crude delivery rate 5 years after referral to infertility treatment is around 70%.14 We aimed to study if childbirth is associated with psychiatric episodes and if having a planned pregnancy and subsequently giving birth to a wanted child prevents postpartum psychiatric disorders, using data from a nationwide IVF register. This design parallels a natural experiment,15 where some couples conceive and become parents compared with others who remain childless – which, for a range of apparent reasons, cannot be conducted in real life.
Methods
Study population
We conducted a cohort study based on register data obtained by using a unique personal identification number assigned to all persons living in Denmark. This number, introduced in 1968, is used across all registration systems in the country. The register holds information on a range of variables including dates of birth, deaths, emigration status, and links to family members.
Data sources
Information regarding IVF-treatment was derived from The Danish IVF Register, which was established on 1 January 1994 and is updated through 31 December 2005.16 The register is based on a compulsory reporting system, where all initiated treatment cycles are recorded at all public and private treatment sites in Denmark.
Information from The Danish Psychiatric Central Register was used to identify all admissions (recorded since 1969) and outpatient contacts (recorded since 1995).17 The diagnostic system used in the register since 1995 is the Danish version of ICD-10.18 For the present study we were interested in all diagnoses as a measure of any type of disorder that requires treatment at a psychiatric facility. Additionally, psychiatric diagnoses were grouped as follows: psychotic disorders (F2), affective disorders (F3), neurotic disorders (F4), and other psychiatric disorders (remaining diagnoses). Postpartum psychiatric episodes were divided into two groups based on timing of the recorded disease episode: 0-90 days postpartum and 90+ days postpartum. The rationale for this grouping was based on evidence that, especially for bipolar affective disorders, episodes immediately following childbirth are subtypes of psychiatric disorders, most likely constituting a specific sub-phenotype of patients – indicating etiological, diagnostic and prognostic significance.19-21
The Danish National Hospital Register holds data on inpatient treatments since 1978 and outpatient treatments since 1995.22 This register contains information on all treatments at medical hospitals in the country; we used information through 2007. We calculated the Charlson Comorbidity Index by using information derived from this register.23
The Integrated Database for Longitudinal Labor Market Research holds information from 1980 and onwards on data such as income and education, derived from administrative registers on persons living in Denmark on December 31 every year.24;25 It was also possible to identify spouses and cohabitees on a yearly basis. Note that a cohabitee is defined as a non-first degree relative of the opposite sex with an age difference <15 years who is sharing a residence with only one other adult.
Study cohort, design and statistical analyses
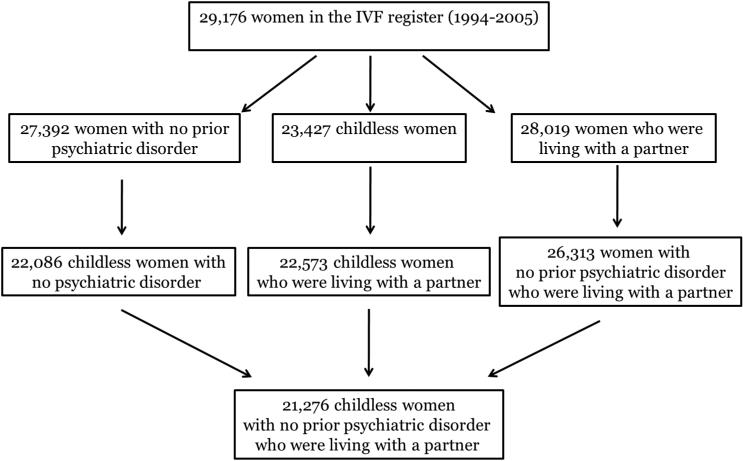
By using information from the above mentioned registries, we formed a study cohort existing of all women and their partners (spouse or cohabiting person) who were registered in the IVF register, similar to a previous study by our group.26 Only couples living in Denmark in the year prior to the first IVF treatment were included in the cohort. We excluded women who were not childless and those who had records of psychiatric diagnoses prior to the infertility treatment; women whose partners met either of these criteria were also excluded. A flowchart presenting the data and exclusion criteria is shown in Figure 1.
Figure 1.
Flow diagram of study participants
We followed all cohort members from entry into the IVF register (date of first treatment) until the outcome of interest: date of first psychiatric inpatient or outpatient treatment, or until date of death, emigration or 31 December 2008, whichever came first. In its present version the IVF register covers treatments until 31 December 2005. Because information on psychiatric treatments was available until December 2008, each cohort member was followed for least a three years.
Data were analyzed with Cox regression using the PhReg procedure in SAS (version 9.1). Incidence rate ratios (IRRs), Wald statistics, and 95% confidence intervals (CIs) were computed.27 Dates when a child was born were modeled as time-dependent covariates. At baseline the following possible confounders were considered: male partner’s gross annual income (wages, pensions, unemployment and social security benefits, and interest rates), grouped into highest age-year quartile (quartiles based on the entire Danish population) versus the lower quartiles; female’s educational attainment (primary school only versus additional educational achievement); Charlson comorbidity index (0,1,2,3+)23;28, age (≥25,25-30,30-35,35-40,≤40 years) and calendar year as a continuous variable. The following time-dependent mediating factors were analyzed: marital breakup (i.e. not sharing address with partner); partner diagnosed with a psychiatric illness; adoption and abortion status; and number of IVF treatment sessions.
Additional analyses were performed for singleton births, twin births, fathers, outpatient and inpatient psychiatric treatment, and for women who had had a psychiatric episode before start of IVF treatment.
Results
Among the 21,276 women who received IVF treatment during the period January 1994 to December 2005, 42 had psychiatric episodes requiring treatment at an outpatient or inpatient treatment facility during the first 90 days postpartum (21 inpatient treatments and 21 treatments at outpatient clinics). The postpartum ICD-10 diagnoses included psychotic disorders (F2, 3 cases), affective disorders (F3, 12 cases), neurotic disorders (F4, 21 cases) and remaining diagnoses (6 cases). In comparison, a total of 374 new mothers had a psychiatric episode from 90 days postpartum until the end of the follow-up period (31 December 2008). Among women who remained childless, 294 had a psychiatric disorder during the study period. The incidence rate for onset of any type of psychiatric disorder 0 to 90 days postpartum was 11.3 per 1000 person-years (95% CI = 8.2-15.0), compared with 3.6 (3.3-4.0) 90+ days postpartum, and 3.8 (3.4-4.3) among women not giving birth.
The crude and adjusted risks for having a psychiatric episode after delivery are presented in Table 1. Across the different models and after adjustment for selected confounders, women subsequently becoming mothers had higher risks of experiencing a psychiatric episodes 0-90 days after the delivery than 90+ days after the birth compared with the women who remained childless (crude IRR = 2.8 [95% CI = 2.0-4.0], fully adjusted IRR = 2.9 [(2.0-4.2]). Additionally, IRRs for inpatient vs. outpatient treatment 0-90 days postpartum were: 3.5 (2.1-5.8) and 2.2 (1.3-3.6), respectively. In comparison, among the 689 women who had experienced a psychiatric episode prior to the initial IVF-treatment and who were not included in the main analyses, 150 women had a subsequent episode of which 11 were in the postpartum period, resulting in an IRR of 3.1 (1.6-6.0). The IRR associated with psychiatric episodes within 0-30, 0-60, 0-182 and 0-365 days after delivery were 3.3 (2.0-5.5), 3.3 (2.2-4.8), 1.8 (1.3-2.5) and 1.2 (0.9-1.5), respectively. Figure 2 shows the IRR as a function of days since birth. The risk appeared to be particularly increased immediately after birth and tended to level off within a year.
Table 1.
Risks of postpartum psychiatric episodes in new mothers after delivery of child conceived through IVF treatment.
| Inpatient or outpatient psychiatric treatment |
No. cases |
No. person- years |
Crude HR (95% CI) |
Adjusted HRa (95% CI) |
Adjusted HRb (95% CI) |
Adjusted HRc (95% CI) |
|---|---|---|---|---|---|---|
| 0-90 days postpartum |
42 | 3,725 | 2.8 (2.0-4.0) |
2.7 (1.9-3.8) |
2.8 (2.0-4.0) |
2.9 (2.0-4.2) |
| 90 + days postpartum |
374 | 103,323 | 0.8 (0.7-1.0) |
0.7 (0.6-0.9) |
0.8 (0.7-1.0) |
0.9 (0.7-1.0) |
| Noned | 294 | 77,378 | 1.00 | 1.00 | 1.00 | 1.00 |
Adjusted for adoption, age and calendar year.
Adjusted for variables in footnote a, plus income, education and Charlson comorbidity Index.
Adjustment for variables in footnote b, plus psychiatric disorder in spouse, death of spouse, abortion history, and number of IVF treatments.
Reference category. Non-exposed group: childless women
Figure 2.
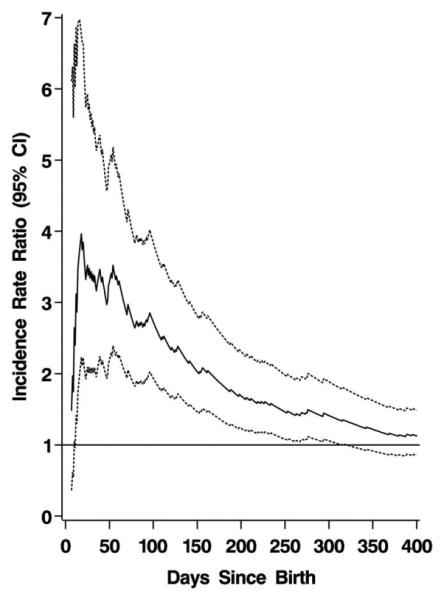
Incidence rate ratios of postpartum psychiatric episodes as a function of days since birth
A twin birth resulted in a higher risk of psychiatric episodes 0-90 days postpartum than singleton birth. For twin birth, IRR = 4.3 (2.4-7.8) compared with singleton birth, IRR = 2.6 (1.7-3.9) (Table 2).
Table 2.
Risks of postpartum psychiatric episodes in new mothers after delivery of single child or twins conceived through IVF treatment
| Singleton birth | Twin birth | |||||
|---|---|---|---|---|---|---|
| Inpatient or outpatient psychiatric treatment |
No. cases |
No. person- years |
Adjusted HRa
(95% CI) |
No. cases |
No. person- years |
Adjusted HRa (95% CI) |
| 0-90 days postpartum |
30 | 2,982 | 2.6 (1.7-3.9) |
12 | 742 | 4.3 (2.4-7.8) |
| 90 + days postpartum |
307 | 81,649 | 0.9 (0.8-1.1) |
62 | 21,658 | 0.7 (0.5-0.9) |
| Noneb | 373 | 99,795 | 1.00 | 636 | 162,026 | 1.00 |
Adjustment for adoption, age, calendar year, income, education, Charlson comorbidity Index, psychiatric disorder in spouse, death of spouse, abortion history, and number of IVF treatments. All variables are mutually adjusted.
Reference category. Singleton births, non-exposed group is childless plus women having twin births. For twin births, non-exposed group is childless women and women having singleton births.
Fatherhood was not associated with increased risks of psychiatric episodes requiring inpatient or outpatient treatment within the first 3 months after the delivery or later, compared with the reference group of men who were not fathers (Table 3).
Table 3.
Risks of postpartum psychiatric episodes in new fathers after delivery of child conceived through IVF treatment.
| All births | Singleton birth | Twin birth | |||||
|---|---|---|---|---|---|---|---|
| Inpatient or outpatient psychiatric treatment |
Adjusted hazard ratios (95% CI) #1 |
No. cases |
No. person- years |
Adjusted HRa (95% CI) |
No. cases |
No. person- years |
Adjusted HRa (95% CI) |
| 0-90 days postpartum |
1.0 (0.5-2.0) |
5 | 2,987 | 0.7 (0.3-1.7) |
4 | 744 | 2.4 (0.9-6.4) |
| 90 + days postpartum |
1.0 (0.9-1.3) |
257 | 81,709 | 1.1 (0.9-1.3) |
60 | 21,685 | 1.0 (0.7-1.3) |
| Noneb | 1.00 | 291 | 99,974 | 1.00 | 489 | 162,240 | 1.00 |
Adjustment for adoption, age, calendar year, income, education, Charlson comorbidity Index, psychiatric disorder in spouse, death of spouse, abortion history, and number of IVF treatments. All variables are mutually adjusted.
Reference category. For singleton births, non-exposed group is all childless men plus fathers having twins. For twin births, non-exposed group is all childless men plus fathers of singletons.
Discussion
Based on a study design paralleling a natural experiment, the present study indicated that childbirth is associated with onset with postpartum psychiatric episodes following delivery in women, but not in men. Results also show that twin births appear to increase risk of psychiatric episodes postpartum more than singleton births.
Unintended vs. intended pregnancies
Unintended pregnancies have been linked with depressive symptoms and symptoms of posttraumatic stress in the mothers,11; 29-32 although this can be difficult to study as unintended pregnancies cover both mistimed and unwanted pregnancies,11 feelings which can change over time of pregnancy and postpartum. We defined the IVF treatment pregnancies as planned and intended, due to these women actively seeking help to become pregnant. Based on this assumption, our results indicate that pregnancy intention does not reduce the risks of having a severe psychiatric episode requiring treatment at a psychiatric facility after a delivery. The cause of postpartum psychiatric disorders is not fully understood. Psychological, social and mainly biological factors are thought to play a role,33-37 and the pathway to psychiatric disorders postpartum is complex and most likely multifactorial.38 Our results could indicate that the etiology behind these psychiatric episodes is biological rather than psychological in nature, although this is challenging to assess. Further support for this biological explanation comes from our finding that new fathers did not experience similarly increased risks of psychiatric episodes, indicating that the cause of the disorders is directly associated with the pregnancy itself.
Incidence rates of psychiatric disorders in IVF-treated women compared with the background population
Among women receiving IVF treatment, the incidence rate of postpartum psychiatric episodes within the first 90 days after a delivery was 11.3 per 1000 person-years (95% CI = 8.2-15.0). In a recent study we found that the incidence rate of psychiatric inpatient or outpatient treatment 0-90 days postpartum based on data covering the entire Danish female population was 10.7 per 1000 person-years (IR = 13.1 for 0 to 30 days after delivery, 11.2 for 31 to 60 days after delivery, and 7.7 for 61 to 90 days after delivery per 1000 person year).13 This suggests that women conceiving after IFT treatments have risks of postpartum psychiatric episodes that are similar to those of the general population. Note that IVF-treated women will represent a group of women with a higher median age than the background population; however the presented results were adjusted for age, as well as other factors, to control for possible confounding.
Singleton vs. twin birth
Among new mothers we found a somewhat higher risk of psychiatric episodes 0 to 90 days postpartum among mothers giving birth to twins compared with singleton births (IRR = 4.3 [2.4-7.8] vs. 2.6 [1.7-3.9]). In comparison, Ross et al recently found an association between multiple birth and self-reported maternal depressive symptoms among women utilizing assisted reproductive technologies.39 Possible explanations for any increased risk associated with multiple births could include high levels of parenting stress and fatigue in mothers with multiple births, as well as increased risks of adverse birth outcome in twins.39; 40
IVF treatment
Based on information from the Danish IVF register, the crude delivery rate is around 70% in the population of IVF-treated women within a 5-year follow-up period.14 Women’s emotional adjustment to unsuccessful IVF treatment was reviewed in 2007 by Verhaak et al.41 In keeping with our results, the authors found that unsuccessful treatments evoked an increase of depressive symptoms when pre- and post-treatment symptom levels are compared. It is plausible that women in our cohort who did not conceive also experienced depressive symptoms due to infertility. However, when studying psychiatric disorders necessitating inpatient or outpatient treatment at psychiatric facilities, risks were higher among postpartum women (0-90 days) compared with women who did not deliver. After the immediate postpartum period, mothers had a decreased risk of psychiatric episodes compared with women who were not mothers, suggesting a more prolonged risk in the women not giving birth. Note that this was also observed after extensive control for possible confounders, such as adoption and abortion history, medical conditions/comorbidity, age, income and number of IVF treatments. In comparison, there were no differences in risk of onset with a first time psychiatric episode in fathers shortly after delivery, fathers more than 90 days postpartum and men who were not fathers.
Strengths vs. limitations
The present study is based on data derived from an IVF register with national coverage. All women entering IVF treatment actively try to conceive, and after one or several treatments a proportion of them become pregnant. Combining data on the IVF treatment outcomes (deliveries vs. childlessness) gave us the possibility of designing a study similar to a natural experiment, which for a range of apparent reasons cannot be conducted in real life. One of the true advantages of this design is that we assume that possible unmeasured factors influencing the outcome of interest (risk of psychiatric episodes) will be equally distributed between the two groups of couples. Furthermore, as our study parallels a natural experiment, our results are less likely to be explained by reverse causation or confounding. Causality could not be established in the present study, as this is an observational study and not a randomized trial. However, due to our particular design, combined with extensive confounder control, we speculate that the current results suggest a direct causality between childbirth and psychiatric disorders.
Limitations in the present study should also be noted. First, despite using a register with national coverage, there are few cases with postpartum psychiatric episodes, due to the rarity of severe disorders postpartum. This limits the possibility of studying risks of specific diagnostic groups. Second, we cannot rule out the possibility that unmeasured residual confounding related to physical or mental health of the women could have influenced our results. Third, our study sample is highly selected as all women underwent fertility treatment, were childless and had no record of any psychiatric diagnoses at time of inclusion into the study. For these reasons our results may not be generalizable to involuntary childless women and men in the background population. However, in the present study, among the 21,276 women who entered IVF treatments, 42 experienced a postpartum psychiatric episode – which is similar to the rate in the entire Danish population (1-3 per 1000 new mothers).1 Lastly, we relied on information from population registers, which captures only psychiatric treatment at psychiatric inpatient or outpatient facilities, thus restricting the analyses only to women and men who actively sought care. It is therefore possible that we have underestimated the proportion of women and men with psychiatric disorders in our cohort. Note that a Swedish study looked at prevalence of psychiatric disorders in couples undergoing IVF treatment and found that 31% of women and 10% of men had any type of psychiatric diagnoses, with only 21% of the subjects who had a DSM-IV defined psychiatric disorder receiving some form of treatment.42
In conclusion, using a study design paralleling a natural experiment, our results indicated that childbirth is associated with risk of psychiatric disorders in new mothers, but we cannot conclude that childbirth causes psychiatric episodes, as our data are observational and we cannot rule out unmeasured confounding in this unique study population. Our results suggest that an intended pregnancy does not reduce risks of postpartum psychiatric episodes, since IVF-treated women have risks of postpartum psychiatric episodes similar to those of the background population. In contrast, becoming a father was not associated with psychiatric disorders.
Sources of funding
This study is funded by the iPSYCH, The Lundbeck Foundation Initiative for Integrative Psychiatric Research. The Stanley Medical Research Institute funds an unrestricted research grant to The National Center for Register-Based Research. TMO is funded by NIMH (National Institute of Mental Health), grant number R01MH104468 (co-I).
Footnotes
Both author T. Munk-Olsen and E. Agerbo report no competing interests.
Reference List
- (1).Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New Parents and Mental Disorders. A Population-Based Register Study. JAMA. 2006;296(21):2582–9. doi: 10.1001/jama.296.21.2582. [DOI] [PubMed] [Google Scholar]
- (2).Harlow BL, Vitonis AF, Sparen P, Cnattingius S, Joffe H, Hultman CM. Incidence of hospitalization for postpartum psychotic and bipolar episodes in women with and without prior prepregnancy or prenatal psychiatric hospitalizations. Arch Gen Psychiatry. 2007 Jan;64(1):42–8. doi: 10.1001/archpsyc.64.1.42. [DOI] [PubMed] [Google Scholar]
- (3).Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987 May;150:662–73. doi: 10.1192/bjp.150.5.662. [DOI] [PubMed] [Google Scholar]
- (4).Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset Timing, Thoughts of Self-harm, and Diagnoses in Postpartum Women With Screen-Positive Depression Findings. JAMA Psychiatry. 2013 Mar;13:1–9. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Munk-Olsen T, Laursen TM, Mendelson T, Pedersen CB, Mors O, Mortensen PB. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009 Feb;66(2):189–95. doi: 10.1001/archgenpsychiatry.2008.528. [DOI] [PubMed] [Google Scholar]
- (6).Jones I, Craddock N. Familiality of the puerperal trigger in bipolar disorder: results of a family study. Am J Psychiatry. 2001 Jun;158(6):913–7. doi: 10.1176/appi.ajp.158.6.913. [DOI] [PubMed] [Google Scholar]
- (7).Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001 Sep;50(5):275–85. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- (8).O′Hara MW, Swain AM. Rates and Risk of Postpartum Depression - a Meta-analysis. International Review of Psychiatry. 1996;8(1):37–54. [Google Scholar]
- (9).Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004 Jul;26(4):289–95. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- (10).Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006 Jun;38(2):90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- (11).Mercier RJ, Garrett J, Thorp J, Siega-Riz AM. Pregnancy intention and postpartum depression: secondary data analysis from a prospective cohort. BJOG. 2013 Aug;120(9):1116–22. doi: 10.1111/1471-0528.12255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Major B, Appelbaum M, Beckman L, Dutton MA, Russo NF, West C. APA Task Force on Mental Health and Abortion. 2008 doi: 10.1037/a0017497. [DOI] [PubMed] [Google Scholar]
- (13).Munk-Olsen T, Laursen TM, Pedersen CB, Lidegaard O, Mortensen PB. Induced first-trimester abortion and risk of mental disorder. N Engl J Med. 2011 Jan 27;364(4):332–9. doi: 10.1056/NEJMoa0905882. [DOI] [PubMed] [Google Scholar]
- (14).Pinborg A, Hougaard CO, Nyboe AA, Molbo D, Schmidt L. Prospective longitudinal cohort study on cumulative 5-year delivery and adoption rates among 1338 couples initiating infertility treatment. Hum Reprod. 2009 Apr;24(4):991–9. doi: 10.1093/humrep/den463. [DOI] [PubMed] [Google Scholar]
- (15).Petticrew M, Cummins S, Ferrel C, Findlay A, Higgens C, Hoy C, et al. Natural Experiments: an underused tool for public health? Public Health. 2005;119:751–757. doi: 10.1016/j.puhe.2004.11.008. [DOI] [PubMed] [Google Scholar]
- (16).Andersen AN, Westergaard HB, Olsen J. The Danish in vitro fertilisation (IVF) register. Dan Med Bull. 1999 Sep;46(4):357–60. [PubMed] [Google Scholar]
- (17).Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011 Jul;39(7 Suppl):54–7. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- (18).World Health Organization . WHO ICD-10: Psykiske lidelser og adfærdsmæssige forstyrrelser. Klassifikation og diagnostiske kriterier [WHO ICD-10: Mental and Behavioural Disorders. Classification and Diagnostic Criteria] Munksgaard; Copenhagen: 1994. [Google Scholar]
- (19).Munk-Olsen T, Laursen TM, Meltzer-Brody S, Mortensen PB, Jones I. Psychiatric Disorders With Postpartum Onset: Possible Early Manifestations of Bipolar Affective Disorders. Arch Gen Psychiatry. 2011 Dec 5; doi: 10.1001/archgenpsychiatry.2011.157. [DOI] [PubMed] [Google Scholar]
- (20).Sharma V, Mazmanian D. The DSM-5 peripartum specifier: prospects and pitfalls. Arch Womens Ment Health. 2014 Apr;17(2):171–3. doi: 10.1007/s00737-013-0406-3. [DOI] [PubMed] [Google Scholar]
- (21).Munk-Olsen T, Jones I, Laursen TM. Birth order and postpartum psychiatric disorders. Bipolar Disord. 2014 May;16(3):300–7. doi: 10.1111/bdi.12145. [DOI] [PubMed] [Google Scholar]
- (22).Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999 Jun;46(3):263–8. [PubMed] [Google Scholar]
- (23).Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- (24).Danmarks Statistik. IDA - en integreret database for arbejdsmarkedsforskning (The Integrated Database for Longitudinal Labour Market Research) Copenhagen; Statistics Denmark Press: 1991. [Google Scholar]
- (25).Sorensen HT, Christensen T, Schlosser HK, Pedersen L. Use of Medical Databases in Clinical Epidemiology, second edition. Aarhus University; Aarhus, Denmark: 2009. [Google Scholar]
- (26).Agerbo E, Mortensen PB, Munk-Olsen T. Childlessness, parental mortality and psychiatric illness: a natural experiment based on in vitro fertility treatment and adoption. J Epidemiol Community Health. 2013 Apr;67(4):374–6. doi: 10.1136/jech-2012-201387. [DOI] [PubMed] [Google Scholar]
- (27).Hougaard P. Analysis of Multivariate Survival Data. Springer-Verlag; New York: 2000. [Google Scholar]
- (28).Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004 Dec;57(12):1288–94. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- (29).Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010 Jan;202(1):5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (30).Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009 Mar;79(3):194–8. doi: 10.1016/j.contraception.2008.09.009. [DOI] [PubMed] [Google Scholar]
- (31).Maxson P, Miranda ML. Pregnancy intention, demographic differences, and psychosocial health. J Womens Health (Larchmt ) 2011 Aug;20(8):1215–23. doi: 10.1089/jwh.2010.2379. [DOI] [PubMed] [Google Scholar]
- (32).Beck CT, Gable RK, Sakala C, Declercq ER. Posttraumatic stress disorder in new mothers: results from a two-stage U.S. national survey. Birth. 2011 Sep;38(3):216–27. doi: 10.1111/j.1523-536X.2011.00475.x. [DOI] [PubMed] [Google Scholar]
- (33).Binder EB, Jeffrey ND, Zach EB, Smith AK, Deveau TC, Altshuler LL, et al. A serotonin transporter gene polymorphism predicts peripartum depressive symptoms in an at-risk psychiatric cohort. J Psychiatr Res. 2010 Jul;44(10):640–6. doi: 10.1016/j.jpsychires.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (34).Steiner M, Dunn E, Born L. Hormones and mood: from menarche to menopause and beyond. J Affect Disord. 2003 Mar;74(1):67–83. doi: 10.1016/s0165-0327(02)00432-9. [DOI] [PubMed] [Google Scholar]
- (35).Pearlstein T, Howard M, Salisbury A, Zlotnick C. Postpartum depression. Am J Obstet Gynecol. 2009 Apr;200(4):357–64. doi: 10.1016/j.ajog.2008.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Bloch M, Rotenberg N, Koren D, Klein E. Risk factors associated with the development of postpartum mood disorders. J Affect Disord. 2005 Sep;88(1):9–18. doi: 10.1016/j.jad.2005.04.007. [DOI] [PubMed] [Google Scholar]
- (37).Mahon PB, Payne JL, MacKinnon DF, Mondimore FM, Goes FS, Schweizer B, et al. Genome-wide linkage and follow-up association study of postpartum mood symptoms. Am J Psychiatry. 2009 Nov;166(11):1229–37. doi: 10.1176/appi.ajp.2009.09030417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Misra DP, Guyer B, Allston A. Integrated perinatal health framework. A multiple determinants model with a life span approach. Am J Prev Med. 2003 Jul;25(1):65–75. doi: 10.1016/s0749-3797(03)00090-4. [DOI] [PubMed] [Google Scholar]
- (39).Ross LE, McQueen K, Vigod S, Dennis CL. Risk for postpartum depression associated with assisted reproductive technologies and multiple births: a systematic review. Hum Reprod Update. 2011 Jan;17(1):96–106. doi: 10.1093/humupd/dmq025. [DOI] [PubMed] [Google Scholar]
- (40).Davies MJ, Moore VM, Willson KJ, Van EP, Priest K, Scott H, et al. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012 May 10;366(19):1803–13. doi: 10.1056/NEJMoa1008095. [DOI] [PubMed] [Google Scholar]
- (41).Verhaak CM, Smeenk JM, Evers AW, Kremer JA, Kraaimaat FW, Braat DD. Women's emotional adjustment to IVF: a systematic review of 25 years of research. Hum Reprod Update. 2007 Jan;13(1):27–36. doi: 10.1093/humupd/dml040. [DOI] [PubMed] [Google Scholar]
- (42).Volgsten H, Skoog SA, Ekselius L, Lundkvist O, Sundstrom P. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Hum Reprod. 2008 Sep;23(9):2056–63. doi: 10.1093/humrep/den154. I. [DOI] [PMC free article] [PubMed] [Google Scholar]