Abstract
Purpose
To investigate the relationship between central corneal thickness (CCT) and demographics, and determine whether CCT may be a substantial mediator of the relationships between glaucoma and its demographic risk factors.
Methods
This cross-sectional study included patients in the Kaiser Permanente Northern California health plan from January 1, 2007 to December 31, 2011 who were 40 years and older and had a documented CCT measurement (N=81,082). Those with any cornea-related diagnoses or a history of corneal refractive surgery were excluded. Demographic characteristics, including age, sex, and race/ethnicity, as well as clinical information including glaucoma-related diagnosis, diabetic status, CCT, and intraocular pressure were gathered from the electronic medical record.
Results
Multivariate linear regression analysis indicated that female sex, increased age, and Black race were significantly associated with thinner corneas. A subgroup analysis among Asians revealed that Chinese, Japanese, and Koreans had corneas 6-13 μm thicker than South and Southeast Asians, Filipinos, and Pacific Islanders for each diagnosis (P<.001). In our population, 24.5% (N=19878) had some form of open-angle glaucoma; 21.9% (N=17779) did not have any glaucoma-related diagnosis. Variation in CCT accounted for only 6.68% (95% confidence interval [CI] 6.14-7.24%) of the increased risk of open-angle glaucoma seen with increasing age, but explained as much as 29.4% (95% CI 27.0%-32.6%) of the increased risk of glaucoma seen among Blacks, and 29.5% (95% CI 23.5%-37.0%) of the increased risk of glaucoma seen among Hispanics.
Conclusions
CCT appears to explain a substantial portion of the increased risk of glaucoma seen among Blacks and Hispanics.
Introduction
Glaucoma is a progressive optic neuropathy with several risk factors including advancing age, Black race or Hispanic ethnicity, positive family history, and high intraocular pressure (IOP). A thin central corneal thickness (CCT) has recently been identified as a predictor of glaucoma progression1–3. CCT has long been known to affect measurement of intraocular pressure (IOP), with thinner corneas leading to underestimation of IOP4. Controversy continues regarding whether the effect of CCT on glaucoma is due to its effects on IOP measurement error, or whether the link between CCT and glaucoma may also be due to structural and biomechanical differences at the optic nerve head5–8. Furthermore, CCT has also been reported to vary between different glaucoma subtypes9–11 and between different risk groups for glaucoma such as by age,12–15 race, and ethnicity11, but it remains unknown whether differences in CCT explains a portion of the increased risk of glaucoma seen in different risk groups.
We used data from the electronic medical record database of a large multiethnic population in the Kaiser Permanente Northern California health plan system to 1) investigate the relationship between CCT and demographic risk factors for glaucoma, especially age, race, and ethnicity, and 2) quantify the extent to which variation in CCT may explain the impact of race and ethnicity on increasing the risk of glaucoma by acting as a substantial mediator.
Methods
Study design and population
We performed a cross-sectional epidemiologic study among patients enrolled in Kaiser Permanente Northern California (KPNC) from January 1, 2007 to December 31, 2011. KPNC is an integrated, managed-care group practice with approximately 3.2 million enrollees, totaling 30% of the population of 14 Northern California counties. The KPNC adult membership is demographically similar to the general population of the region, and in particular is well representative of the diverse racial and ethnic population of Northern California16.
The study population consisted of 81,082 adults, 40 years and older, who had a CCT measurement; 3,500 patients (4.31%) were excluded for having at least one encounter related to corneal disease (ICD9 370.0-371.9) during this period, or a history of corneal refractive surgery . As the corneal thicknesses of right and left eyes were highly correlated (Pearson correlation coefficient r = .9150, P<.0001), only right eyes were included in the analysis. For analyses involving IOP, patients who were missing a record of IOP measurement were excluded (N=1550, 1.9% of full sample).
This study was approved by the Institutional Review Board of Kaiser Northern California, Division of Research.
Measures
Demographic information collected from the medical record included age at the time of CCT measurement, sex, and self-reported race and ethnicity. Major race and ethnicity categories included non-Hispanic White, non-Hispanic Black, American Indian/Native American, Hispanic, Asian, and Other/Unknown. Those who self-reported as Asian race were divided into several further groups based on self-report, including Chinese, Japanese, Korean, Filipino, Southeast Asian (including Bamar, Burmese, Cambodian, Hmong, Indonesian, Javanese, Khmer, Laotian, Malaysian, Nepalese, Singaporean, and Thai), Pacific Islander (including Fijian, Guamanian/Chamorro, Native Hawaiian, Maori, New Zealander, Samoan, Tahitian, and Tongan), and South Asian (including Asian Indian, Bangladeshi, Bengali, East Indian, Pakistani, Pathan, Singhalese, and Sri Lankan).
Glaucoma and glaucoma suspect diagnoses were determined by ICD9 codes associated with patient encounters throughout the entire five-year period. Since an individual patient could sometimes receive different variants of ICD9 codes for glaucoma at different encounters during this period, when determining a singular diagnosis for each patient, we used the most specific ICD9 code available. Those coded as glaucoma or open-angle glaucoma (ICD9 365.1, 365.11, 365.9, or 365.71-73) were considered primary open angle glaucoma (POAG). Normal tension glaucoma was identified with ICD9 365.12. For glaucoma suspect, we included open-angle glaucoma suspect (365-365.01, 377.14), and ocular hypertension (365.02). Due to the small number of primary angle-closure glaucoma cases, primary angle closure (ICD9 365.2-24, 365.41, 365.59) and primary angle closure suspect (365.02) were combined into one category (PAC/PACG). Remaining glaucoma-related codes were considered “Other glaucoma” (365.13-4, 365.6-65, 365.82-83, 365.31-32, 365.03). Those without a glaucoma-related code during the study period were designated “No Glaucoma”.
CCT measurements as entered by the clinician were available through the electronic medical record. The standard equipment for measuring CCT in KPNC ophthalmology practices was the DGH-550 or DGH-55 ultrasonic (contact) pachymeter (DGH Technology Inc.; Exton, PA). The Kaiser facility at which CCT was measured was also available through the electronic medical record. Because CCT is not typically billed as a separate procedure in the Kaiser system, the reason for the visit at which CCT was measured was extracted from the medical record in order to characterize the context in which CCT was performed. Patients who did not have a glaucoma diagnosis entered into their medical record had CCT measurements at visits made for a variety of reasons, the most common of which was a routine exam (23.6%, N=4192), followed by glaucoma evaluation, IOP check, or visual field testing (23.6%, N=4192), with the determination that the patient did not have glaucoma or was not a glaucoma suspect. Other reasons included follow-up exams (12.1%, N=2152) or consults, referrals, and new patient visits (7.18%, N=1277), refractive surgery evaluation, cataract evaluation, or a variety of other systemic or ocular complaints or other diagnostic procedures.
Intraocular pressure (IOP) measurements as entered by clinicians at the encounter were available through the medical record, and the maximum recorded IOP from 2007-2011 for each patient was considered as a covariate in our analysis. Maximum recorded IOP has been recently suggested to be more useful than mean IOP in predicting functional progression in glaucoma17. The presence of diabetes was also determined through ICD9 coding in the electronic medical record and considered a covariate in multivariate analyses.
Data Analysis
Data were analyzed using the software program Stata 12.0 (College Station, TX). Raw differences between race and ethnicity categories were compared using analysis of variance for continuous variables (age, CCT) and the chi-squared test for categorical variables (sex, diabetes status, glaucoma diagnosis). Locally weighted scatterplot smoothing (Lowess) curves were generated using a bandwidth of 0.8. Multivariate linear regression was used to assess the relationship of demographic variables to CCT, adjusted for history of diabetes and Kaiser facility at which CCT was measured. Models were stratified by glaucoma diagnosis, due to the significant interaction between the presence and type of glaucoma diagnosis and demographic predictors, indicated by P<.001 for the coefficient of the interaction term. Because of significant nonlinearity in the relationship between age and CCT, models with CCT as the outcome included a quadratic term for age. Significance of the nonlinearity was determined by the P value of the coefficient of the quadratic term for age in the linear regression models, and by comparing the Bayesian Information Criterion (BIC) between models with and without the quadratic term for age. Additional assumptions of the multivariate linear regression models were checked as follows: 1) the model error satisfied a normal distribution, as confirmed by residual plots; 2) homoscedasticity of the residuals was confirmed using residuals versus fitted plots.
To analyze the extent to which CCT is a mediator in the relationship between glaucoma and its risk factors age and race, we calculated the percent of the effect of each predictor (age and race) explained by CCT18. The formula used for calculating the percent explained was (Overall Effect-Direct Effect)/Overall Effect, where overall effect represents the coefficient of the predictor of interest in a model with open-angle glaucoma (including both POAG and NTG) as the outcome and covariates not including CCT, and the direct effect represents the coefficient of the predictor in the same model with CCT additionally included as a covariate. Bootstrapped, bias-corrected confidence intervals for the percent explained were calculated using 1000 replications. The risk models for open-angle glaucoma as an outcome were Poisson-type generalized linear model with robust errors, which generate risk ratios rather than odds ratios; these were used rather than logistic regression models since open-angle glaucoma was a relatively common diagnosis in our study population.
Results
Population characteristics
Our study included 81,082 patients in the Kaiser Permanente Northern California health plan from 2007-2011 who had a CCT measurement in the electronic medical record. Table 1 reports the age, sex, glaucoma diagnoses, and CCT in the entire study population and compared between the different self-reported race categories. Overall, 21.9% of the population did not have any glaucoma-related diagnosis at any encounter during the 5-year study period. Those with primary open angle glaucoma and normal tension glaucoma accounted for 20.5% (N=16,601) and 4.0% (N=3277) of the population, respectively, for a combined total of 24.5% (N=19878) with some form of open-angle glaucoma. Patients with a glaucoma suspect diagnosis or ocular hypertension accounted for 25.1% (N=28,496) and 11.2% (9082) of the population, respectively.
Table 1.
Demographic and clinical characteristics of the study population
| All study subjects (N=81082) | White (N=45133) | Black (N=9140) | Hispanic (N=7261) | Native American (N=525) | Asian (N=12946) | Other/Unknown (N=6077) | P value* | |
|---|---|---|---|---|---|---|---|---|
| Age (years), mean (SD) | 65.1 (12.3) | 67.3 (12.1) | 64.0 (12.0) | 62.3 (12.2) | 63.6 (11.4) | 62.8 (11.8) | 59.0 (11.6) | <.0001 |
| Female, % (N) | 56.6% (45907) | 58.1% (26235) | 58.7% (5365) | 57.5% (4173) | 58.7% (308) | 53.9% (6982) | 46.8% (2844) | <.001 |
| Diabetic, % (N) | 8.3% (6690) | 6.9% (3097) | 14.8% (1354) | 11.1% (804) | 10.7% (56) | 7.7% (996) | 6.3% (383) | <.001 |
| Diagnosis, % (N) | <.001 | |||||||
| No glaucoma-related diagnosis | 21.9% (17779) | 23.8% (10729) | 12.8% (1170) | 20.8% (1512) | 18.9% (99) | 22.1% (2856) | 23.3% (1413) | |
| POAG suspect | 35.1% (28496) | 32.4% (14642) | 36.7% (3350) | 37.9% (2751) | 37.9% (199) | 39.8% (5155) | 39.5% (2399) | |
| OHTN | 11.2% (9082) | 13.7% (6164) | 9.2% (836) | 9.3% (678) | 11.2% (59) | 5.3% (690) | 10.8% (655) | |
| POAG | 20.5% (16601) | 19.6% (88861) | 33.1% (3026) | 19.8% (1437) | 20.8% (109) | 16.5% (2134) | 17.0% (1034) | |
| NTG | 4.0% (3277) | 3.2% (1433) | 3.6% (328) | 4.5% (327) | 3.6% (19) | 7.9% (1017) | 2.5% (153) | |
| PAC/PACG | 4.2% (3418) | 3.7% (1654) | 2.7% (245) | 4.9% (359) | 4.2% (22) | 6.7% (864) | 4.5% (274) | |
| Other glaucoma | 3% (2429) | 3.7% (1650) | 2.0% (185) | 2.7% (197) | 3.4% (18) | 1.8% (230) | 2.5% (149) | |
| CCT (μm), mean (SD) | 553.7 (40.5) | 558.5 (40.3) | 537.3 (39.9) | 550.4 (39.2) | 557.0 (42.5) | 550.4 (39.0) | 554.0 (40.0) | <.0001 |
SD = Standard Deviation. POAG = Primary Open Angle Glaucoma. OHTN = Ocular Hypertension. NTG = Normal Tension Glaucoma. PAC = Primary Angle Closure. PACG = Primary Angle Closure Glaucoma. CCT = Central Corneal Thickness.
P values generated by analysis of variance for continuous variables, and chi-squared test for categorical variables
Demographic predictors of CCT
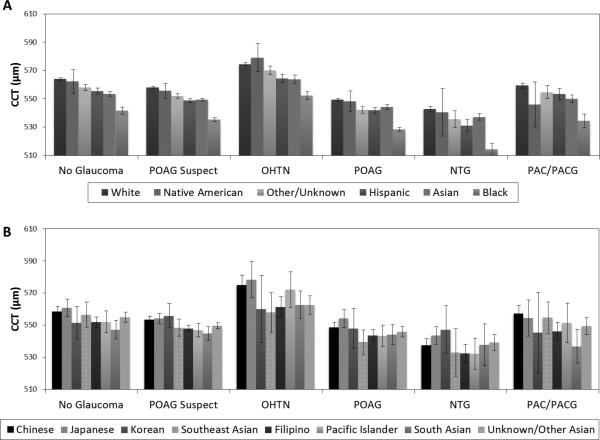
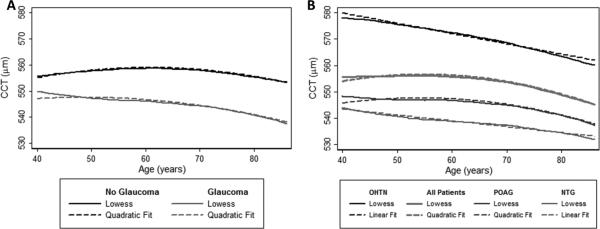
We investigated the relationship between CCT and demographic predictors sex, race, and age in both univariate and multivariate analyses. In univariate analyses, mean CCT was slightly thinner in women compared to men (553.0 μm, standard deviation [SD] 40.0 vs. 554.6 μm, SD 41.0, P <.0001). The mean CCT also varied by race in a univariate analysis (P<.0001), with the thinnest corneas in Blacks (537.3 μm, SD 39.9) and the thickest corneas in Whites (558.5 μm, SD 40.3) (Table 1), and corneas of intermediate thickness among Asians and Hispanics. The relationship between age and CCT is depicted in Figure 1, which demonstrates a nonlinear relationship between age and CCT, confirmed by fitted lines with a quadratic term for age which closely follow the locally weighted scatterplot smoothing (Lowess) curves representing the original data. Stratifying by presence of glaucoma (Figure 1A) and type of glaucoma diagnosis (Figure 1B) demonstrated that the relationship between age and CCT varied by glaucoma diagnosis. Formal testing for interaction confirmed that the presence and type of glaucoma were effect modifiers of the relationship between age and CCT (P<.001). Further multivariate analyses of CCT were stratified by diagnosis and additionally adjusted for a history of diabetes and the facility at which the CCT measurement was made and included a quadratic term for age. Results were similar to the univariate analyses, with women typically having thinner corneas than men (no greater than 3 μm difference with any diagnosis), Blacks and Whites having the thinnest and thickest corneas, respectively (Figure 2A), and a similar relationship demonstrated between age and CCT. For the “No Glaucoma” stratum, we also performed a sensitivity analysis including only patients whose CCT was measured during encounters documented to be “routine”; results were similar.
Figure 1. Relationship between central corneal thickness (CCT) and age.
The curvature in the relationship between CCT and age is depicted by a locally-weighted scatterplot smoothing (Lowess) representation of the 81,082 patients in our study sample, as well as a fitted line which included a quadratic term for age as a predictor of CCT. Patients were stratified by (A) presence or absence of glaucoma, and (B) type of glaucoma-related diagnosis, including ocular hypertension (OHTN), all patients regardless of diagnosis, primary open angle glaucoma (POAG), and normal tension glaucoma (NTG).
Figure 2. Relationship between central corneal thickness (CCT), race, and ethnicity.
CCT adjusted for age, sex, diabetes status, and Kaiser facility is depicted with error bars representing the 95% confidence interval, for (A) self-reported race (non-Hispanic White, non-Hispanic Black, non-Hispanic Asian) as well as Hispanic and Native American ethnicities, and (B) self-reported Asian ethnicities. Patients were stratified by diagnosis, including normal, primary open angle glaucoma (POAG) suspect, ocular hypertension (OHTN), POAG, normal tension glaucoma (NTG), and primary angle closure (PAC) or primary angle closure glaucoma (PACG).
CCT and glaucoma among Asians
A unique aspect of this study population was the rich composition of many different Asian groups, reflective of the diversity of the area served by the Kaiser Permanente Northern California health plan, allowing us to perform a subgroup analysis to explore differences in CCT between various Asian groups. Characteristics of patients of different Asian groups are shown in Table 2. Specific data on ethnic origin was not available for all patients who self-reported as Asian; therefore, we separately analyzed those whose Asian ethnicity was unknown.
Table 2.
Demographic and clinical characteristics of the Asian study population
| Chinese (N=3190) |
Japanese (N=1225) |
Korean (N=243) |
Filipino (N=3053) |
Southeast Asian (N=522) |
Pacific Islander (N=732) |
South Asian (N=810) |
Other/ Unknown Asian (N=3172) |
P value* | |
|---|---|---|---|---|---|---|---|---|---|
| Age (years), mean (SD) | 64.0 (11.6) | 68.5 (11.9) | 63.9 (11.2) | 63.1 (11.2) | 61.2 (11.2) | 63.5 (12.2) | 60.5 (11.4) | 59.8 (11.6) | <.0001 |
| Female, % (N) | 52.6% (1677) | 60.4% (740) | 54.7% (133) | 56.7% (1732) | 50.6% (264) | 54.5% (399) | 42.4% (343) | 53.4% (1694) | <.001 |
| Diabetic, % (N) | 5.4% (172) | 7.4% (90) | 7.4% (18) | 9.3% (284) | 5.8% (30) | 11.1% (81) | 9.3% (75) | 7.8% (246) | <.001 |
| Diagnosis, % (N) | <.0001 | ||||||||
| No glaucoma-related diagnosis | 23.4% (746) | 19.1% (234) | 26.8% (65) | 22.0% (671) | 20.7% (108) | 19.5% (143) | 24.8% (201) | 21.7% (688) | |
| POAG suspect | 36.4% (1161) | 40.2% (493) | 38.3% (93) | 43.2% (1320) | 35.8% (187) | 41.0% (300) | 36.5% (288) | 41.4% (1313) | |
| OHTN | 4.8% (153) | 3.8% (46) | 5.4% (13) | 4.4% (142) | 6.9% (36) | 6.4% (47) | 9.8% (79) | 5.5% (174) | |
| POAG | 17.0% (543) | 14.9% (183) | 14.4% (35) | 15.8% (481) | 18.4% (96) | 16.9% (124) | 17.7% (143) | 16.7% (529) | |
| NTG | 9.6% (306) | 15.9% (195) | 9.9% (24) | 5.7% (174) | 4.6% (24) | 7.8% (57) | 3.8% (31) | 6.5% (206) | |
| PACG/PACS | 7.3% (233) | 3.9% (48) | 3.7% (9) | 6.6% (200) | 11.9% (62) | 5.3% (39) | 6.7% (54) | 6.9% (219) | |
| Other glaucoma | 1.5% (48) | 2.1% (26) | 1.7% (4) | 2.1% (65) | 1.7% (9) | 3.0% (22) | 1.7% (14) | 1.3% (42) | |
| CCT (μm), mean (SD) | 554.4 (40.2) | 552.7 (37.9) | 552.1 (36.3) | 547.4 (37.3) | 548.3 (39.0) | 547.2 (37.4) | 545.8 (39.1) | 550.3 (39.7) | <.0001 |
SD = Standard Deviation. POAG = Primary Open Angle Glaucoma. OHTN = Ocular Hypertension. NTG = Normal Tension Glaucoma. PAC = Primary Angle Closure. PACG = Primary Angle Closure Glaucoma. CCT = Central Corneal Thickness.
P values generated by analysis of variance for continuous variables, and chi-squared test for categorical variables
After adjusting for age and sex and stratifying by diagnosis, relationships between CCT and different Asian groups remained fairly consistent (Figure 2B). East Asians (primarily Chinese and Japanese) had thicker corneas compared to South and Southeast Asians, Filipinos and Pacific Islanders, a relationship that is clearly seen in patients without glaucoma and patients who had POAG suspicion, OHTN, POAG, or NTG. There were fewer patients with PAC/PACG; Chinese and Japanese patients with these diagnoses continued to demonstrate thicker corneas than South Asians and Filipinos, while the relationship between the other ethnicities varied somewhat. Nonetheless, age- and sex-adjusted comparison of Chinese, Japanese, and Koreans as a group to South and Southeast Asians, Filipinos, and Pacific Islanders as a group revealed statistically significant differences of 6-13 μm in cornea thickness for each diagnosis (P<.001 for every diagnosis) between those two larger groups. Across all diagnoses, East Asians had a thicker mean CCT of 553.9 μm (95% confidence interval [CI] 552.8-555.0) compared to 547.2 μm (95% CI 546.1-548.2) in South and Southeast Asians, Filipinos, and Pacific Islanders.
CCT as a mediator for demographic risk factors for open-angle glaucoma
We next sought to investigate and quantify the role CCT may play as a mediator in the relationship between open-angle glaucoma and age and race (Table 3). We used a Poisson generalized linear model with robust errors to determine the effect of age on the risk of open-angle glaucoma, adjusted for sex, race, IOP, history of diabetes, and Kaiser facility. The overall adjusted risk ratio for glaucoma indicated that for each 10-year increase in age, the risk of glaucoma increased by a factor of 1.45 (95% CI 1.43-1.46). After the addition of CCT as a potential mediator in the model, the direct risk ratio for glaucoma for each 10-year increase in age was 1.42 (95% CI 1.41-1.43). Thus, CCT explained only 6.68% (95% CI 6.14-7.24%) of the impact of older age on increasing the risk of glaucoma. We used a similar approach to examine CCT as a mediator between race and glaucoma, examining Blacks and Hispanics compared to Whites, as these groups are known to be at increased risk for open-angle glaucoma. Overall, the risk ratio for glaucoma was 1.60 (1.55-1.66) in Blacks compared to Whites when adjusting for age, sex, IOP, diabetes, and Kaiser facility; the addition of CCT to the model lowered this risk ratio to 1.39 (95% CI 1.35-1.44). CCT explained 29.4% (95% CI 27.0%-32.6%) of the impact of Black race on the increased risk of glaucoma. Similarly, the overall adjusted risk of glaucoma for Hispanics compared to Whites was 1.24 (95% CI 1.18-1.29), which decreased to 1.16 (95% CI 1.11-1.21) with the addition of CCT to the model. Variation in CCT accounted for 29.5% of the increased risk of glaucoma among Hispanics, compared to Whites. We performed a sensitivity analysis in which we excluded patients in the “No Glaucoma” group whose CCT was measured during encounters made for any reason other than “routine”, with similar results.
Table 3.
Central corneal thickness as a mediator in the relationship between glaucoma and its risk factors
| Risk factor for glaucoma | |||
|---|---|---|---|
| Age | Black race | Hispanic ethnicity | |
| Adjusted*, overall RR (95% CI) | 1.45 (1.43-1.46) | 1.60 (1.55-1.66) | 1.24 (1.18-1.29) |
| Adjusted**, direct RR (95% CI) | 1.42 (1.41-1.43) | 1.39 (1.35-1.44) | 1.16 (1.11-1.21) |
| Percent explained, % (95% CI) | 6.68 (6.14-7.24) | 29.4 (27.0-32.6) | 29.5 (23.5-37.0) |
RR = Risk Ratio. CI = Confidence Interval.
Adjusted for race, IOP, sex, diabetes status and Kaiser facility for the analysis of age; adjusted for age, IOP, sex, diabetes status and Kaiser facility for the analysis of race. Risk ratios for age are given per 10-year increase. Reference group for race/ethnicity is Whites.
Adjusted for race, IOP, sex, diabetes status, Kaiser facility and CCT for the analysis of age; adjusted for age, IOP, sex, diabetes status, Kaiser facility and CCT for the analysis of race. Risk ratios for age are given per 10-year increase. Reference group for race/ethnicity is Whites.
Discussion
In this study of a large, diverse, insured population from Northern California, we found that female sex, increasing age, and Black race were associated with thinner corneas in patients with and without a variety of glaucoma-related diagnoses. A subgroup analysis in Asians revealed that those of East Asian descent, particularly Chinese and Japanese, had thicker corneas than those of South and Southeast Asian descent, including Filipinos and Pacific Islanders. Furthermore, in a mediation analysis, we found that CCT explained very little of the effect of age on increasing the risk of glaucoma in most patients, but did appear to explain a substantial portion of the impact of Black race and Hispanic ethnicity on the increased risk of glaucoma.
The relationships we found between demographic factors and CCT have corroborated previous findings, and our large population size allowed the detection of nuances in these relationships that may not have been previously observable in smaller study samples. Although our finding that women had statistically significantly thinner corneas than men is consistent with several previous studies12,19–22, the less than 3 μm difference in CCT that we found between men and women is unlikely to be of clinical import. An inverse relationship between age and CCT has been reported in previous studies12–15. Furthermore, presence or absence of glaucoma and type of glaucoma were found to be effect modifiers of the relationship between CCT and age, which may explain why previous studies in different patient populations have sometimes yielded varying results 12–15,23,24.
Also similar to prior smaller studies were our findings that Blacks had thinner corneas than Whites and that Asians and Hispanics had CCT intermediate between Blacks and Whites11,23,25,26. A unique aspect of our study was the ability to directly compare CCT between several Asian subgroups within one study population. Our findings are consistent with studies in homogeneous Asian populations that have reported relatively thinner corneas in South19,20 and Southeast Asia5,27, and thicker corneas in East Asians13,24,28–30. As CCT is highly heritable31,32, similarities between CCT in Asian patients from this U.S. study population and from populations in Asia despite geographic and environmental differences is not surprising. One notable exception was in the case of the Japanese subpopulation: several previous studies have reported thinner corneas among Japanese12,33, thinner than all comparison groups except Blacks11, which was not replicated in this study. In short, our investigations demonstrated relationships between CCT and race which strengthen previous research findings, and permitted an analysis of multiple Asian groups in a single population which found that those of East Asian descent had thicker corneas than those of South and Southeast Asian descent.
The question of whether CCT is an independent risk factor for glaucoma through mechanisms beyond its influence on IOP measurement remains unsettled34, although some have hypothesized that a thinner CCT is associated with structural and mechanical properties of the optic nerve head, such as deformability, which may increase susceptibility to glaucoma5–8. By applying mediation analysis, our study quantified how these factors may account for some of the association between open-angle glaucoma and its well-known demographic risk factors, age and race. Although corneas become thinner with increasing age, our mediation analysis revealed that variation in CCT accounted for only approximately 7% of the effect of age on glaucoma, suggesting that aging increases the risk of glaucoma largely through mechanisms unrelated to thinning CCT. However, variation in CCT explained almost 30% of the increased risk of glaucoma seen among Blacks and Hispanics compared to Whites, even with adjustment for differences in IOP. One interpretation is that CCT and its hypothesized effect on glaucoma is a true physiologic mediator of the relationship between race and glaucoma, such that Blacks and Hispanics are at increased risk of glaucoma partially due to structural differences of the eye, an idea supported by the increased optic disk size seen in Blacks35–37 and Hispanics35. Another interpretation is that since CCT is highly heritable, it may be that genetic risk factors for glaucoma that are unrelated to CCT may nonetheless be co-inherited with CCT. Thus, although CCT does not appear to be a substantial mediator of the relationship between glaucoma and age, it may potentially represent a substantial mediator of the relationship between glaucoma and race.
Strengths of this study include its exceptionally large and diverse, multiracial and multiethnic population. Furthermore, the availability of clinical data such as CCT and IOP is a feature beyond what is usually available from health plan data. However, we recognize several limitations to this study. For example, although most of the Kaiser Permanente Northern California facilities use a standard ultrasonic pachymeter, it is possible that some measurements were made using other equipment. Clinical data may also be limited by variation in the methods of IOP measurement between individual providers and over time. Furthermore, our reliance on ICD9 codes for identification of diagnoses may be affected by variable coding practices. To reduce the impact of variability in data collection practices, all multivariable analyses were adjusted for specific Kaiser facility. In addition, although only right eyes were included in this analysis, ICD9 coding does not provide information on glaucoma diagnosis based on the individual eye; therefore, some misclassification of glaucoma diagnosis for the right eye may have occurred among those patients who did receive a glaucoma-related ICD9 code. However, glaucoma is typically a bilateral disease, with approximately 80% of newly diagnosed POAG occurring bilaterally as reported in the Collaborative Initial Glaucoma Treatment Study38. Furthermore, the close correlation between CCT for left and right eyes is also likely to mitigate this limitation. Another limitation is that although treatment with prostaglandin analogs has been shown in some cases to cause decrease in CCT over time39–41, we do not have information in our dataset regarding use of prostaglandin analogues, and in particular the duration of use and timing of use in relation to CCT measurement. Although typical clinical practice is to measure CCT prior to initiation of glaucoma therapy, one cannot rule out the possibility that measurements in some patients were taken while on prostaglandins. Finally, since patients in this study sought the care of an ophthalmologist for a variety of reasons, results may not generalize to the population at large but are likely to be more representative of a general ophthalmology clinic population, with the exception of those with corneal disease or a history of corneal refractive surgery who were excluded from our study. In particular, caution must be exercised in generalizing the results of our patients whose CCT was measured but who were never coded with a glaucoma-related diagnosis to the normal population at large, although sensitivity analyses among the subgroup whose CCT was measured as part of a routine eye examination revealed similar results as among all study patients without glaucoma.
In summary, our analysis of CCT and demographic characteristics revealed that CCT decreases with age, and that the relationship between CCT and race, as well as CCT and Asian ethnicity in a subgroup analysis, is consistent between patients with and without a variety of glaucoma diagnoses. In an analysis of risk factors for open-angle glaucoma, we found that variation in CCT explains a substantial portion of the increased risk of glaucoma seen among Blacks and Hispanics, even after adjustment for IOP. Our results highlight the importance of pursuing further studies to determine the physiologic mechanisms by which variation in CCT between races may confer increased risk of glaucoma.
Acknowledgements
The authors wish to thank Mark Segal, Ph.D., UCSF Department of Epidemiology and Biostatistics, for many helpful statistical consultations.
Financial Support: Core grant EY002162 from the National Eye Institute; That Man May See, Inc, San Francisco; Research to Prevent Blindness, New York City; and the National Center for Research Resources, the National Center for Advancing Translational Sciences, and the Office of the Director, National Institutes of Health, through UCSF-CTSI Grant Number TL1 RR024129. Contents of the manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies.
Footnotes
Conflicts of interest: The authors declare that they have no conflict of interest.
References
- 1.Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714. doi: 10.1001/archopht.120.6.714. [DOI] [PubMed] [Google Scholar]
- 2.Leske MC, Heijl A, Hyman L, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:1965–72. doi: 10.1016/j.ophtha.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 3.Miglior S, Pfeiffer N, Torri V, et al. Predictive factors for open-angle glaucoma among patients with ocular hypertension in the European Glaucoma Prevention Study. Ophthalmology. 2007;114:3–9. doi: 10.1016/j.ophtha.2006.05.075. [DOI] [PubMed] [Google Scholar]
- 4.Lester M, Mete M, Figus M, et al. Incorporating corneal pachymetry into the management of glaucoma. J Cataract Refract Surg. 2009;35:1623–8. doi: 10.1016/j.jcrs.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 5.Wu R-Y, Zheng Y-F, Wong T-Y, et al. Relationship of central corneal thickness with optic disc parameters: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2011;52:1320–4. doi: 10.1167/iovs.10-6038. [DOI] [PubMed] [Google Scholar]
- 6.Prata TS, Lima VC, Guedes LM, et al. Association between corneal biomechanical properties and optic nerve head morphology in newly diagnosed glaucoma patients. Clin Experiment Ophthalmol. 2012;40:682–8. doi: 10.1111/j.1442-9071.2012.02790.x. [DOI] [PubMed] [Google Scholar]
- 7.Pakravan M, Parsa A, Sanagou M, et al. Central corneal thickness and correlation to optic disc size: a potential link for susceptibility to glaucoma. Br J Ophthalmol. 2007;91:26–8. doi: 10.1136/bjo.2006.106039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lesk MR, Hafez AS, Descovich D. Relationship between central corneal thickness and changes of optic nerve head topography and blood flow after intraocular pressure reduction in open-angle glaucoma and ocular hypertension. Arch Ophthalmol. 2006;124:1568–72. doi: 10.1001/archopht.124.11.1568. [DOI] [PubMed] [Google Scholar]
- 9.Copt RP, Thomas R, Mermoud A. Corneal thickness in ocular hypertension, primary open-angle glaucoma, and normal tension glaucoma. Arch Ophthalmol. 1999;117:14. doi: 10.1001/archopht.117.1.14. [DOI] [PubMed] [Google Scholar]
- 10.Herndon LW, Choudhri SA, Cox T, et al. Central corneal thickness in normal, glaucomatous, and ocular hypertensive eyes. Arch Ophthalmol. 1997;115:1137. doi: 10.1001/archopht.1997.01100160307007. [DOI] [PubMed] [Google Scholar]
- 11.Aghaian E, Choe JE, Lin S, et al. Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology. 2004;111:2211–9. doi: 10.1016/j.ophtha.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 12.Tomidokoro A, Araie M, Iwase A. Corneal Thickness and Relating Factors in a Population-Based Study in Japan: The Tajimi Study. Am J Ophthalmol. 2007;144:152–4. doi: 10.1016/j.ajo.2007.02.031. [DOI] [PubMed] [Google Scholar]
- 13.Lee ES, Kim CY, Ha SJ, et al. Central corneal thickness of Korean patients with glaucoma. Ophthalmology. 2007;114:927–30. doi: 10.1016/j.ophtha.2006.09.036. [DOI] [PubMed] [Google Scholar]
- 14.Lekskul M, Aimpun P, Nawanopparatskul B, et al. The correlations between Central Corneal Thickness and age, gender, intraocular pressure and refractive error of aged 12-60 years old in rural Thai community. J Med Assoc Thai. 2005;88(Suppl 3):S175–179. [PubMed] [Google Scholar]
- 15.Foster PJ, Baasanhu J, Alsbirk PH, et al. Central corneal thickness and intraocular pressure in a Mongolian population. Ophthalmology. 1998;105:969–73. doi: 10.1016/S0161-6420(98)96021-3. [DOI] [PubMed] [Google Scholar]
- 16.Gordon NP. How does the adult Kaiser Permanente membership in Northern California compare with the larger community. Kaiser Permanente Division of Research; Oakland, CA: 2006. [Google Scholar]
- 17.Gardiner SK, Johnson CA, Demirel S. Factors predicting the rate of functional progression in early and suspected glaucoma. Invest Ophthalmol Vis Sci. 2012 doi: 10.1167/iovs.11-9065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vittinghoff Eric, Glidden DV, Shiboski SC, et al. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. 2nd ed. Springer; New York: 2012. [Google Scholar]
- 19.Vijaya L, George R, Arvind H, et al. Central Corneal Thickness in Adult South Indians:: The Chennai Glaucoma Study. Ophthalmology. 2010;117:700–4. doi: 10.1016/j.ophtha.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 20.Nangia V, Jonas JB, Sinha A, et al. Central corneal thickness and its association with ocular and general parameters in Indians: the Central India Eye and Medical Study. Ophthalmology. 2010;117:705– 10. doi: 10.1016/j.ophtha.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Hanna CL, Roberts RT, Hwang S-J, et al. Pachymetry of donor corneas: effect of ethnicity and gender on central corneal thickness. Cornea. 2004;23:701–3. doi: 10.1097/01.ico.0000126327.92475.2b. [DOI] [PubMed] [Google Scholar]
- 22.Garcia-Medina M, Garcia-Medina JJ, Garrido-Fernandez P, et al. Central corneal thickness, intraocular pressure, and degree of myopia in an adult myopic population aged 20 to 40 years in southeast Spain: determination and relationships. Clin Ophthalmol. 2011;5:249–58. doi: 10.2147/OPTH.S16594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brandt JD, Beiser JA, Kass MA, et al. Central corneal thickness in the ocular hypertension treatment study (OHTS). Ophthalmology. 2001;108:1779–88. doi: 10.1016/s0161-6420(01)00760-6. [DOI] [PubMed] [Google Scholar]
- 24.Kamiya K, Shimizu K, Ohmoto F. Effect of aging on corneal biomechanical parameters using the ocular response analyzer. J Refract Surg. 2009;25:888–93. doi: 10.3928/1081597X-20090917-10. [DOI] [PubMed] [Google Scholar]
- 25.Shimmyo M, Ross AJ, Moy A, et al. Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am J Ophthalmol. 2003;136:603–13. doi: 10.1016/s0002-9394(03)00424-0. [DOI] [PubMed] [Google Scholar]
- 26.La Rosa FA, Gross RL, Orengo-Nania S. Central corneal thickness of Caucasians and African Americans in glaucomatous and nonglaucomatous populations. Arch Ophthalmol. 2001;119:23. [PubMed] [Google Scholar]
- 27.Casson RJ, Abraham LM, Newland HS, et al. Corneal thickness and intraocular pressure in a nonglaucomatous Burmese population: the Meiktila Eye Study. Arch Ophthalmol. 2008;126:981–5. doi: 10.1001/archopht.126.7.981. [DOI] [PubMed] [Google Scholar]
- 28.Cho P, Lam C. Factors affecting the central corneal thickness of Hong Kong-Chinese. Curr Eye Res. 1999;18:368–74. doi: 10.1076/ceyr.18.5.368.5347. [DOI] [PubMed] [Google Scholar]
- 29.Zhang H, Xu L, Chen C, et al. Central corneal thickness in adult Chinese. Association with ocular and general parameters. The Beijing Eye Study. Graefes Arch Clin Exp Ophthalmol. 2008;246:587–92. doi: 10.1007/s00417-007-0760-9. [DOI] [PubMed] [Google Scholar]
- 30.Xu L, Zhang H, Wang YX, et al. Central corneal thickness and glaucoma in adult Chinese: the Beijing Eye Study. J Glaucoma. 2008;17:647. doi: 10.1097/IJG.0b013e3181666582. [DOI] [PubMed] [Google Scholar]
- 31.Landers JA, Hewitt AW, Dimasi DP, et al. Heritability of Central Corneal Thickness in Nuclear Families. Invest Ophthalmol Vis Sci. 2009;50:4087–90. doi: 10.1167/iovs.08-3271. [DOI] [PubMed] [Google Scholar]
- 32.Toh T, Liew SHM, MacKinnon JR, et al. Central Corneal Thickness Is Highly Heritable: The Twin Eye Studies. Invest Ophthalmol Vis Sci. 2005;46:3718–22. doi: 10.1167/iovs.04-1497. [DOI] [PubMed] [Google Scholar]
- 33.Suzuki S, Suzuki Y, Iwase A, et al. Corneal thickness in an ophthalmologically normal Japanese population. Ophthalmology. 2005;112:1327–36. doi: 10.1016/j.ophtha.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 34.Medeiros FA, Weinreb RN. Is corneal thickness an independent risk factor for glaucoma? Ophthalmology. 2012;119:435–6. doi: 10.1016/j.ophtha.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seider MI, Lee RY, Wang D, et al. Optic disk size variability between African, Asian, white, Hispanic, and Filipino Americans using Heidelberg retinal tomography. J Glaucoma. 2009;18:595–600. doi: 10.1097/IJG.0b013e3181996f05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marsh BC, Cantor LB, WuDunn D, et al. Optic nerve head (ONH) topographic analysis by stratus OCT in normal subjects: correlation to disc size, age, and ethnicity. J Glaucoma. 2010;19:310–8. doi: 10.1097/IJG.0b013e3181b6e5cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Varma R, Tielsch JM, Quigley HA, et al. Race-, Age-, Gender-, and Refractive Error--Related Differences in the Normal Optic Disc. Arch Ophthalmol. 1994;112:1068–76. doi: 10.1001/archopht.1994.01090200074026. [DOI] [PubMed] [Google Scholar]
- 38.Musch DC, Shimizu T, Niziol LM, et al. Clinical characteristics of newly diagnosed primary, pigmentary and pseudoexfoliative open-angle glaucoma in the Collaborative Initial Glaucoma Treatment Study. Br J Ophthalmol. 2012;96:1180–4. doi: 10.1136/bjophthalmol-2012-301820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Viswanathan D, Goldberg I, Graham SL. Longitudinal effect of topical antiglaucoma medications on central corneal thickness. Clin Experiment Ophthalmol. 2013;41:348–54. doi: 10.1111/j.1442-9071.2012.02870.x. [DOI] [PubMed] [Google Scholar]
- 40.Zhong Y, Shen X, Yu J, et al. The comparison of the effects of latanoprost, travoprost, and bimatoprost on central corneal thickness. Cornea. 2011;30:861–4. doi: 10.1097/ICO.0b013e3182000c27. [DOI] [PubMed] [Google Scholar]
- 41.Kim HJ, Cho BJ. Long-term effect of latanoprost on central corneal thickness in normal tension glaucoma. J Ocul Pharmacol Ther. 2011;27:73–6. doi: 10.1089/jop.2010.0071. [DOI] [PubMed] [Google Scholar]