Abstract
Purpose
The present study evaluates health status and its relation with occupational characteristics and with burnout syndrome among embryologists.
Methods
A cross-sectional design was used to conduct an online self-assessment survey, sent to all members of the Spanish Association of Clinical Embryologists. The questionnaire contained occupational questions and two standard instruments: ‘Short Form-12 Health Survey’ as a measure of physical (PCS-12) and mental (MCS-12) health and the Maslach Burnout Inventory-General Survey (MBI-GS) to evaluate the degree of burnout.
Results
The PCS-12 obtained for the Spanish embryologists was higher than that for the reference population. However, the total MCS-12 was significantly lower than that observed in non-institutionalised males and females representative of the general Spanish population aged 35–44 years. In the linear regression model, the dependent variable PCS-12 was related indirectly with the variables number of hours worked per week, BMI, back pain, leg pain and visual discomfort. In the linear regression model, the dependent variable MCS-12 was indirectly related to the gender (male reference; female coefficient regression: −3.23), exhaustion and cynicism dimensions of the MBI-GS. A total of 87 (36.3 %) embryologists presented a high score on at least one of the MBI-GS dimensions.
Conclusion
In this sample of Spanish embryologists, a norm measure (SF-12) showed their physical health to be better than the average for the general population, but that their mental health was poorer. A significant indirect relation was observed between mental health and burnout syndrome. Strategies to reduce occupational stress and problems should form part of the training provided for clinical embryologists.
Keywords: Embryologist, MBI-GS, Burnout, SF-12, IVF
Introduction
Embryologists are highly trained laboratory professionals who play an essential part in the diagnosis and treatment of infertility, in preventing the transmission of genetic and infectious diseases and in cryopreservation as part of infertility treatment. Unlike other clinical laboratories, the embryology laboratory presents little automation and requires the performance of numerous manual techniques. This work is associated with physical tiredness due to long periods of microscope and computer work, and may present potential health hazards including injuries from the manipulation of infectious human cells or tissues or of liquid nitrogen. Moreover, the high degree of attention needed during laboratory work in order to avoid errors of potentially severe consequences in the manipulation of samples frequently provokes mental tiredness. Other factors that aggravate this tiredness are the large amount of paperwork required by quality control and traceability systems, the inevitable periods of intense work in the embryology laboratory, the potential to confuse gametes, resulting in major ethical/legal issues, and the extreme unpredictability of the work schedule involved in most embryology laboratories.
Staff who work in stressful conditions may feel anxious about themselves, their performance, how they are being treated, and about others. They may cope with these anxieties by means of psychological defences that have a major impact on interpersonal relations and work performance. Currently, one of the most important work-related problems resulting from stress is burnout syndrome, which has negative consequences both on those who suffer from it and on the organisations for which they work [1],.
According to Maslach et al. (2001) [2], this syndrome includes exhaustion, cynicism and professional inefficacy, and is the result of prolonged exposure to chronic stressors in the workplace. It can affect an individual’s physical and/or mental health, giving rise to psychosomatic disorders (such as headaches, insomnia, ulcers or gastritis) or psychopathological disorders (including depression, anxiety and obsession-compulsion) [3]. For organizations, it can seriously reduce performance and provoke excessive rotation and absenteeism.
Numerous studies have been made of the mental and physical health of health care personnel in general, and the prevalence of burnout syndrome has been reported to range from 4 to 40 % [3–5]. However, very few studies have been made in this respect of clinical laboratory staff [6] and, to the best of our knowledge, no study has analysed these aspects among clinical embryologists. Accordingly, the present study evaluates physical and mental health status and its relation with different occupational characteristics and with burnout syndrome among Spanish embryologists.
Materials and methods
Study design
A cross-sectional design to conduct an online self-assessment survey.
Participants
The study population consisted of all the embryologists who are members of the Spanish Association of Clinical Embryologists (Asociación para el estudio de la biología de la reproducción; ASEBIR) who had been working during the previous nine months. Two e-mails were sent to all ASEBIR members explaining the aims of the research. At the time of the survey, ASEBIR had a total of 787 members (212 male and 575 female; 26.9–73.1 %), of whom 184 (23.4 %) were working in public laboratories (data obtained from the ASEBIR secretariat). The e-mails sent contained a link to the online questionnaire and the consent form. Google Drive was used as an online platform for the questionnaires. To estimate the true value of the proportion of burnout with a precision of 4, at a 95 % confidence level and assuming a prevalence of 10 % [7], a study population of 217 persons was required. The study was approved by the Research Ethics Committee at Virgen de las Nieves University Hospital (Granada). The mean time required to fill in the survey was 15 min.
Instruments
The questionnaire contained sociodemographic and occupational questions and two standard instruments: the ‘Short Form-12 Health Survey (SF-12)’ as a measure of physical and mental health [6] and the Maslach Burnout Inventory-General Survey (MBI-GS) [8] in its validated Spanish language version [9] to evaluate the degree of burnout.
Measurements
Sociodemographic and occupational characteristics
The subjects were first asked to complete a series of questions related to sociodemographic issues, including age, gender, existence of stable relationship and number of children. Secondly, the questionnaire collected information on occupational characteristics and workload: position as embryologist in the last nine months (yes vs no), type of centre (public vs private), number of hours worked per week, length of service (<10 vs >10 years), contract duration (permanent vs temporary), contract type (full time vs part time) and number of staff in the laboratory.
The participants were also asked to state their view of their own future as an embryologist. For this purpose, we used Question 75 from the European Working Conditions Survey, [10] carried out by the European Foundation for the Improvement of Living and Working Conditions - EuroFound (Do you think you will be able to do your current job when you are 60 years old? A) ‘I would not want to’, B) ‘No, I do not think so’, C) “Yes, I think so”.) These results were then compared with those obtained in Spain in 2010 in a sample of 547 workers aged 30–49 years (14.3, 38.3, 47.4 %, respectively).
Physical and mental health
The SF-12 is a short-form questionnaire developed from the original SF-36 Health Survey. SF-36 contains eight scales (physical functioning, role limitations due to physical and emotional health problems, physical pain, general health perception, vitality, social functioning, and mental health), while SF-12 contains just one or two items from each of these scales. A summary score of physical and mental health is calculated from scoring algorithms applied to all items. To maintain national comparability, the weights were calculated according to the corresponding Spanish reference standard [11]. The physical component summary (PCS-12) and the mental component summary (MCS-12) for the SF-12 were scored in a three-step procedure: a) create indicator variables (scored 1/0) for each response category, except the category for health status (thus, of 47 possible answers, for the 12 items, 35 indicator variables were created); b) calculate the aggregate score, by summing the weighted indicator variables; c) add a constant, such that the aggregate CSF-12 and CSM-12 scores were standardised to obtain a mean value of 50 and a standard deviation of 10 for the Spanish general population. Thus, values higher or lower than 50 are interpreted as better or worse, respectively, than those for the Spanish general population.
Norm-based comparisons require valid norms to ensure a well-defined and representative sample of the population of interest. Because health status scores for some concepts differ significantly across age groups and between men and women, we used norms based on a cross-sectional survey of a sample of 1730 non-institutionalised males and females representative of the general Spanish population aged 35–44 years [11]. The representative sample of the Spanish population used by these authors was obtained from the cross-sectional study “Design consumption home survey”. In addition to the Body Mass Index (BMI), the following aspects of physical health were evaluated: physical complaints caused by poor posture or physical strain at work during the last year, visual discomfort (“No” vs. “Yes”), loss of visual acuity (“No” vs. “Yes”), headaches, neck pain, back pain or complaints affecting the arms or legs. Responses to these last five items were rated on a six-point Likert scale ranging from “Always” to “Never”.
MBI-GS
This survey consists of 15 items grouped into three dimensions or subscales: ‘exhaustion’, ‘cynicism’ and ‘efficacy’. Responses are classified on a Likert-type scale with 7 response options, scored from 0 (‘never’) to 6 (‘always’). The ‘exhaustion’ dimension consists of 5 items (e.g. “I feel emotionally drained from my work”), the ‘cynicism’ dimension consists of 4 items (e.g. “I’ve become more callous toward people since I took this job”) and the ‘efficacy’ dimension consists of 5 items (e.g. “I deal very effectively with the problems of my work”). Total scores for each subscale were calculated by summing the scores for each item and dividing this total by the number of items in the subscale. Because we wished to study how these different components would affect embryologists’ physical and mental health, each score was applied separately in the analyses. Burnout cases were defined according to cutoff points based on a standardised regulatory reference framework [9, 12], as having a score higher than or equal to the 75th percentile for exhaustion (2.9) and for cynicism (2.26) or a score lower than or equal to the 25th percentile for professional efficacy (3.83).
The reference population used to determine the prevalence of BMI in our study was that validated by the Spanish Institute of Health and Hygiene in the Workplace (Instituto Nacional de Salud e Higiene en el Trabajo: Ministerio de Trabajo). This sample was composed of 1963 workers employed in diverse occupations (office workers, machine operators in the ceramics industry, teachers, users of information and communication technologies, healthcare workers, etc.). [12] Both the factorial validity of the MBI-GS and the internal consistency of its dimensions were satisfactory [13]. An explanatory factor analysis using principal component analysis with varimax rotation identified three underlying dimensions of burnout. The three-factor solution contained few cross-loadings and captured 64 % of the total variance in the embryologists’ responses. The first factor was interpreted as the “exhaustion” dimension (Cronbach α = 0.86), the second as “cynicism” (Cronbach α = 0.88) and the third as ‘efficacy” (Cronbach α = 0.82). The scores for the subscales were constructed by averaging the items grouped by factor analysis, whenever half or more of the corresponding items were not missing. The subscales were only moderately correlated with each other (Pearson coefficients ranging from −0.20 to 0.59).
Statistical analyses
We report the univariate statistics for the PCS-12 and MCS-12 scores as means and standard deviations for the categorical variables and as tertiles for the quantitative variables, including the three MBI-GS subscales, except the BMI results, which were divided into three classes: <25, 25–29 and ≥30 Kg/m2. Student’s t test and analysis of the variance were used to compare the means between the different groups. In addition, Pearson correlation coefficients were used to study correlations between the PCS-12 and MCS-12 scores and the MBI subscales. The mean PCS-12 and MCS-12 scores obtained for the embryologists were compared to the Spanish gender-specific reference samples for adults (aged 35–44 years) [12] using the two-tailed Student’s t test. Differences between categorical measures were assessed using the chi-square test. Two multivariate linear regression models were built with the two principal variables, PCS-12 and MCS-12. First, a bivariate analysis was carried out of all the variables, after which the candidates for the multivariate analysis were selected. These variables were any variable whose bivariate test had a p-value < 0.30 as well as variables of known biological importance. Backward stepwise selection was used to determine the final models. The three MBI subscales used were the values obtained from factorial analysis.
Results
Participants
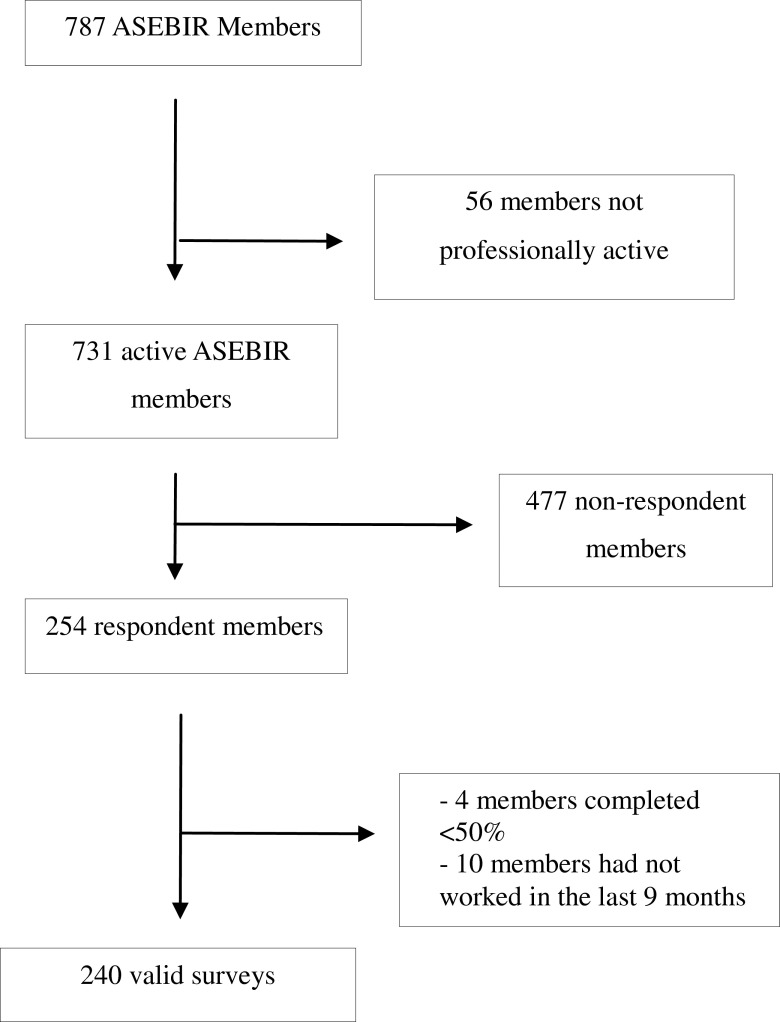
After two reminders had been sent out, the final response rate was 34.7 % (254/731). Ten questionnaires were excluded because the respondents had not worked during the previous 9 months, and another four were excluded because the respondents had answered fewer than 50 % of the survey questions. Thus, 240 valid questionnaires were finally computed (Fig. 1). The mean age of the respondents was 38 years and 77.9 % of them were women. Most participants were in a stable personal relationship (80.0 %), and half (50.8 %) had children. Regarding job characteristics, most worked in private laboratories (77.8 %) with a permanent contract (80.2 %), on a full-time basis of 35–45 h per week; 67.5 % had worked as an embryologist for less than 10 years and 41.8 % worked with more than five embryologists in the laboratory. Between the participants in this survey and total ASEBIR partners, there were no differences in gender (22.1 vs. 26.9 % male, respectively) or type of laboratory (22.2 versus 23.4 % work in a public laboratory), respectively (Tables 1 and 2).
Fig. 1.
Participants
Table 1.
Sociodemographic variables, physical health (PCS-12) and mental health (MCS-12)
| N (%) | PCS-12 | MCS-12 | |
|---|---|---|---|
| Age (years) | |||
| Lower tertile ≤33 | 86 (34.68) | 54.05 ± 6.39 | 42.49 ± 9.66 |
| Middle tertile 34–39 | 83 (33.47) | 54.25 ± 5.77 | 42.66 ± 11.37 |
| Upper tertile ≥40 | 79 (31.85) | 54.02 ± 6.01 | 43.94 ± 12.05 |
| Stable relationship | |||
| No | 48 (20.0) | 54.18 ± 5.84 | 42.42 ± 9.90 |
| Yes | 192 (80.0) | 54.09 ± 6.10 | 43.15 ± 11.28 |
| Children | |||
| No | 118 (49.16) | 54.05 ± 5.87 | 42.51 ± 10.16 |
| Yes | 122 (50.83) | 54.16 ± 6.23 | 43.48 ± 11.78 |
| Sex | |||
| Male | 53 (22.08) | 53.43 ± 6.47 | 45.39 ± 11.28 |
| Female | 187 (77.91) | 54.30 ± 5.92 | 42.33 ± 10.86a |
| Body mass index | |||
| Normal <25 | 189 (77.14) | 54.82 ± 5.71 | 42.36 ± 10.88 |
| Overweight 25–29 | 52 (21.22) | 51.82 ± 6.84 b | 45.14 ± 11.33 |
| Obesity ≥30 | 4 (1.63) | 51.01 ± 4.34 | 47.11 ± 10.79 |
a p < 0.05
b Overweight vs Normal p < 0.05
Table 2.
Work conditions, physical health (PCS-12) and mental health (MCS-12)
| N (%) | PCS-12 | MCS-12 | |
|---|---|---|---|
| Type of laboratory | |||
| Private | 186 (77.82) | 54.23 ± 5.76 | 42.64 ± 10.88 |
| Public | 53 (22.17) | 53.95 ± 6.77 | 44.60 ± 11.25 |
| Type of contract | |||
| Permanent | 190 (80.16) | 54.17 ± 6.22 | 42.77 ± 11.22 |
| Other | 47 (19.83) | 54.36 ± 4.99 | 44.75 ± 9.86 |
| Part/Full time employment | |||
| Full time | 213 (89.4) | 54.00 ± 6.11 | 42.96 ± 11.09 |
| Part time | 25 (10.50) | 54.65 ± 5.56 | 43.71 ± 10.57 |
| Work history | |||
| ≤10 years | 166 (69.16) | 54.05 ± 6.12 | 42.88 ± 10.56 |
| >10 years | 74 (30.83) | 54.24 ± 5.90 | 43.29 ± 12.00 |
| Persons working in the laboratory | |||
| 1–2 persons | 77 (32.21) | 54.95 ± 5.00 | 43.73 ± 9.61 |
| 3–4 persons | 62 (25.94) | 53.20 ± 6.22 | 41.95 ± 11.64 |
| ≥5 persons | 100 (41.84) | 54.02 ± 6.63 | 43.11 ± 11.69 |
| Hours worked per week | |||
| <35 | 38 (15.89) | 55.17 ± 4.94 | 42.86 ± 11.71 |
| 35–45 | 161 (67.36) | 54.52 ± 5.65 | 43.07 ± 10.87 |
| >45 | 40 (16.73) | 51.45 ± 7.80 a | 42.88 ± 11.24 |
| Perform the same job at age 60 | |||
| I don’t think so | 119 (49.79 %) | 53.46 ± 6.78 | 41.29 ± 11.00 |
| I would not want to | 34 (14.22 %) | 53.07 ± 6.07 | 42.16 ± 11.61 |
| Yes, I think so | 86 (35.98 %) | 55.37 ± 4.66 | 45.09 ± 10.62 |
a >45 vs <35 p < 0.05; >45 vs 35–45 p < 0.05
Over 90 % of these Spanish embryologists suffered musculoskeletal problems. The most common complaints concerned the arms (94.9 %), followed by the back (76.7 %) and the neck (70.6 %). About 45 % reported having frequent headaches. The prevalence of visual discomfort was 46 %, with 55.6 % of embryologists having lost visual acuity in the past year (Table 3). Only 35.9 % of the embryologists thought they would still be doing the same job at 60 years old (Table 2). This percentage is lower than the corresponding rate for a reference Spanish population of same-age workers obtained from the European Foundation for the Improvement of Living and Working Conditions (47.4 %) (p < 0.01) [10].
Table 3.
Physical complaints, physical health status (PCS-12) and mental health status (MCS-12)
| N (%) | PCS-12 | MCS-12 | |
|---|---|---|---|
| Headache | |||
| Always-Almost always | 5 (2.11) | 56.18 ± 6.37 | 39.89 ± 11.04a |
| Often-Sometimes | 100 (42.37) | 52.54 ± 6.95 | 39.54 ± 11.47 |
| Occasionally-Never | 131 (55.50) | 55.18 ± 5.06 | 45.68 ± 9.99 |
| Neck pain | |||
| Always-Almost always | 36 (15.12) | 50.02 ± 7.10 b | 40.16 ± 11.79 |
| Often-Sometimes | 132 (55.46) | 54.37 ± 5.89 | 41.80 ± 11.05 |
| Occasionally-Never | 70 (29.41) | 55.77 ± 4.81 | 46.70 ± 9.78 c |
| Back ache | |||
| Always-Almost always | 44 (18.64) | 50.23 ± 7.85d | 38.92 ± 12.78e |
| Often-Sometimes | 137 (58.05) | 54.38 ± 5.51 | 42.95 ± 10.63 |
| Occasionally-Never | 55 (23.30) | 56.44 ± 4.18 | 46.12 ± 9.77 |
| Pains in the arms | |||
| Always-Almost always | 68 (29.05) | 53.52 ± 6.78 | 41.24 ± 10.91 |
| Often-Sometimes | 154 (65.81) | 54.97 ± 5.15 | 44.13 ± 10.61 |
| Occasionally-Never | 12 (5.12) | 45.57 ± 6.98 | 37.39 ± 13.81 |
| Pains in the legs | |||
| Always-Almost always | 7 (3.03) | 47.53 ± 9.72 | 40.98 ± 14.62 |
| Often-Sometimes | 39 (16.88) | 50.59 ± 7.01 | 43.70 ± 11.69 |
| Occasionally-Never | 185 (80.08) | 54.93 ± 5.26 f | 43.03 ± 10.72 |
| Visual discomfort | |||
| No | 129 (53.97) | 55.41 ± 4.93 | 44.39 ± 10.74 |
| Yes | 110 (46.02) | 52.59 ± 6.87g | 41.36 ± 11.17 |
| Loss of visual acuity | |||
| No | 106 (44.35) | 55.47 ± 5.15 | 45.12 ± 10.49 |
| Yes | 133 (55.64) | 52.96 ± 6.46h | 41.47 ± 11.08i |
a Always-Almost always vs Often-Sometimes p < 0.001
b Always-Almost always vs Often-Sometimes p < 0.001; Always-Almost always vs Occasionally-Never, p < 0.001
c Occasionally-Never vs Always-Almost always p < 0.05; Occasionally-Never vs Often-Sometimes, p < 0.01
d Always-Almost always vs Often-Sometimes p < 0.001; Always-Almost always vs Occasionally-Never p < 0.001
e Always-Almost always vs Occasionally-Never p < 0.01
f Occasionally-Never vs Always-Almost always p < 0.01; Occasionally-Never vs Often-Sometimes p < 0.001
g p < 0.001
h p < 0.01
i p < 0.05
The PCS-12 obtained for Spanish embryologists was higher than that for the reference population aged 35–44 (54.1 ± 6.0 vs 52.6 ± 0.2, p < 0.001). The PCS-12 for the Spanish embryologists was similar among the males (53.4 ± 6.5 vs 53.2 ± 0.4) and significantly higher for the women, compared to a reference group of adults’ aged 35–44 (54.3 ± 5.9 vs 52.1 ± 0.3, p < 0.001). However, the overall MCS-12 result (43.0 ± 11.0 vs 50.6 ± 0.2, p < 0.001) and those for both sexes (males: 45.4 ± 11.3 vs 51.8 ± 0.2, p < 0.001; females: 42.3 ± 10.7 vs 49.5 ± 0.3, p < 0.001) were significantly lower. 20 % of the embryologists reported high scores on the MBI-GS subscale for “emotional exhaustion”, 15.4 % for “cynicism” and 10.8 % for “low professional efficacy”. The mean PCS-12 and MCS-12 scores among the embryologists with high levels of emotional exhaustion were 52.4 ± 7.3 and 33.8 ± 11.2, respectively; for those with high levels of cynicism, the scores were 52.2 ± 7.9 and 33.2 ± 10.8, and for those with low professional efficacy, they were 53.0 ± 7.7 and 36.5 ± 13.2.
A total of 87 (36.3 %) embryologists presented a high score on at least one of the MBI-GS dimensions, with the mean PCS-12 and MCS-12 scores for this group being 53.5 ± 6.6 and 38.1 ± 11.6, respectively. Only 7 (2.9 %) embryologists presented high values in all three MBI-GS dimensions, and in this group the average PCS-12 and MCS-12 scores were 50.2 ± 11.5 and 25.8 ± 9.6, respectively.
Bivariate analysis of health status
Lower PCS-12 scores were obtained for embryologists who were overweight, who worked more than 45 h per week, who had pain in the neck, back or legs, or visual discomfort and/or loss of visual acuity, or higher levels of emotional exhaustion (Tables 1, 2, 3, and 4).
Table 4.
MBI dimensions and physical health (PCS-12) and mental health (MCS-12) status
| N (%) | PCS-12 | MCS-12 | |
|---|---|---|---|
| Emotional exhaustion | |||
| 1st tertile ≤1.5 | 79 (31.73) | 55.32 ± 4.31 | 48.84 ± 8.51 |
| 2nd tertile 1.67–2.33 | 80 (32.13) | 54.80 ± 6.27 | 43.22 ± 9.77b |
| 3rd tertile ≥2.5 | 74 (29.72) | 52.06 ± 7.15 a | 36.36 ± 11.51 |
| Cynicism | |||
| 1st tertile ≤0.5 | 102 (40.96) | 54.75 ± 5.14 | 47.10 ± 9.39 |
| 2nd tertile 0.75–1.5 | 75 (30.12) | 54.39 ± 6.38 | 42.50 ± 10.43c |
| 3rd tertile ≥1.75 | 63 (25.30) | 52.53 ± 7.12 | 35.71 ± 11.03d |
| Professional efficacy | |||
| 1st tertile ≤4.33 | 84 (33.73) | 53.56 ± 6.70 | 39.61 ± 11.72 e |
| 2nd tertile 4.5–5.17 | 72 (28.92) | 53.72 ± 5.40 | 44.62 ± 9.59 |
| 3rd tertile ≥5.33 | 77 (30.92) | 55.06 ± 5.97 | 44.40 ± 10.92 |
a 3rd tertile vs 1st tertile p < 0.01; 3rd tertile vs 2nd tertile p < 0.05
b 2nd tertile vs 1st tertile p < 0.01; 3rd tertile vs 1st tertile p < 0.001; 3rd tertile vs 2nd tertile p < 0.001
c 2nd tertile vs 1st tertile p < 0.05
d 3rd tertile vs 1st tertile p < 0.001; 3rd tertile vs 2nd tertile p < 0.001
e 1st tertile vs 2nd tertile p < 0.05; 1st tertile vs 3rd tertile p < 0.05
Lower mental health scores were obtained for women embryologists, embryologists who suffered headaches or pain in the neck or back, who suffered loss of visual acuity or who presented higher levels of emotional exhaustion or cynicism or lower levels of professional efficacy (Tables 1, 2, 3, and 4).
Emotional exhaustion and cynicism were negatively associated with PCS-12 (Pearson coefficient, −0.25 (p < 0.001) and −0.13 (NS), respectively) and MCS-12 (Pearson coefficient, −0.55 (p < 0.001) and −0.45 (p < 0.001), respectively), whereas professional efficacy was positively associated with PCS-12 and MCS-12 (Pearson coefficient, 0.10 (NS) and 0.26 (p < 0.001), respectively).
Multiple linear regression analyses
The multiple linear regression model for the dependent variable PCS-12, adjusted for gender, number of persons working in the laboratory and exhaustion, included the variables number of hours worked per week, BMI, back pain, leg pain and visual discomfort (Table 5). This model explained 27 % of the variance in PCS-12. The multiple linear regression model for the dependent variable MCS-12 adjusted by type of laboratory and type of contract included the gender, exhaustion and cynicism dimensions of the MBI-GS (Table 6). These variables contributed significantly to explaining 30.4 % of the variance in MCS-12.
Table 5.
Multiple regression of the physical component (PCS-12)
| Coef. | Std. Err. | [95 % Coef. Interval] | t | p | ||
|---|---|---|---|---|---|---|
| Constant | 66.61 | 5.91 | 54.94 | 78.28 | 11.27 | 0.00 |
| Hours worked per week | ||||||
| <35 (reference) | ||||||
| 35–45 | −0.052 | 1.15 | −2.32 | 2.22 | −0.05 | 0.96 |
| >45 | −2.82 | 1.44 | −5.67 | 0.02 | −1.96 | 0.05 |
| BMI | −0.36 | 0.15 | −0.65 | −0.06 | −2.40 | 0.01 |
| Back ache | ||||||
| Occasionally-Never (reference) | ||||||
| Often-Sometimes | −0.79 | 0.97 | −2.71 | 1.12 | −0.82 | 0.41 |
| Always-Almost always | −3.60 | 1.34 | −6.26 | −0.94 | −2.68 | 0.00 |
| Pains in the legs | ||||||
| Occasionally-Never (reference) | ||||||
| Often-Sometimes | −2.57 | 1.10 | −4.76 | −0.38 | −2.32 | 0.02 |
| Always-Almost always | −3.50 | 2.46 | −8.36 | 1.35 | −1.42 | 0.15 |
| Visual discomfort | ||||||
| No (reference) | ||||||
| Yes | −1.91 | 0.83 | −3.56 | −0.26 | −2.29 | 0.02 |
Adjusted for gender, persons working in the laboratory and emotional exhaustion
Table 6.
Multiple regression of the mental component (MCS-12)
| Coef. | Std. Err. | [95 % Coef. Interval] | t | p | ||
|---|---|---|---|---|---|---|
| Constant | 47.78 | 6.87 | 34.23 | 61.34 | 6.95 | 0.00 |
| Sex | ||||||
| Male (reference) | ||||||
| Female | −3.23 | 1.58 | −6.36 | −0.11 | −2.04 | 0.04 |
| Emotional exhaustion | −5.10 | 0.69 | −6.47 | −3.74 | −7.39 | 0.00 |
| Cynicism | −3.52 | 0.70 | −4.91 | −2.13 | −5.01 | 0.00 |
Adjusted for type of laboratory and type of contract in the laboratory
Discussion
PCS-12
The physical health score of the embryologists surveyed was higher than that of the reference population, probably because healthcare personnel tend to have better health habits than the general population; they also tend to be healthier than other persons with a high socioeconomic status [13]. The distribution of the locations of musculoskeletal problems among the embryologists was very similar to that described for microscopists and pathologists [7, 14], with pain in the arms, neck and back being most commonly cited. Frizstche et al. (2012) observed that the most common locations for musculoskeletal pain in 163 pathologists were the neck (78 %) and the shoulders (60 %). In our study, back and leg pain were independent factors in the linear regression model for physical health. No musculoskeletal pain was included in the regression model for mental health. This result agrees with the findings of Hartvigsen et al. (2004) [15], who found insufficient evidence for any positive association between psychological factors (stress at work) and low back pain in their systematic review of prospective cohort studies.
The prevalence of musculoskeletal problems among embryologists is high compared with that for working populations [15, 16], but similar to that observed for pathologists or microscopists (ranging from 76 to 57 %) [7, 14, 17]. Among the risk factors associated with the development of these symptoms are hours of microscope work, duration of work without a break, fast work pace and poor workstation ergonomics [17]. The use of ergonomically optimized equipment could alleviate the pain suffered by a high percentage of embryologists with musculoskeletal problems, as reported by Fritzsche et al. (2012) [7] in a study of pathologists.
Embryology work is associated with possibly eye-straining activities such as long-duration microscopy and computer work. Visual refractive errors are more common among persons in this field. It has been reported that almost 90 % of pathologists have visual refraction problems [7]. The loss of visual acuity among 55 % of embryologists might be part of the normal time course of conventional visual refractive errors, but it may also be associated with the continuous near-field work required [7]. This would explain why the loss of visual acuity was not included in the PCS-12 prediction model. The presence of visual discomfort in this model was considered as a separate factor, possibly more closely related to ergonomic aspects such as humidity, light and temperature in the laboratory than to visual refractive errors.
Working time was inversely related with PCS-12, although it was of borderline significance for embryologists working more than 45 h per week. A high workload has a direct impact on health status. A significant relationship between workload and health complaints has been reported by other authors [18, 19].
Our findings show that BMI is strongly associated with the physical component summary measure but not with the mental component summary, which is in accordance with prior research in this field [20, 21]. Compared to normal weight patients, overweight and obese patients have larger decrements in the subscales, with larger contributions to the physical component summary measure being made by physical function, physical role function, general health and vitality than by the subscales that represent mental, emotional and social functioning [22].
MCS-12
The mean mental health score for the embryologists as a whole (43) was moderately lower than that for the general population [11]. However, the mental health score for embryologists in the upper tertile for burnout dimensions (36) was similar to or somewhat lower than that for a sample of psychiatric patients with depressive disorders or current symptoms [23]. Similar results have been obtained in studies of mental health and burnout in German physicians [24] and Swiss physicians [25]. Interestingly, low mental health levels have also been observed in polycystic ovary syndrome patients [26] and endometriosis patients [27].
In this cross-sectional survey of Spanish embryologists, we found that the lower mental health components of health status were associated with high levels of emotional exhaustion and cynicism. In this study, 36.3 % of Spanish embryologists reported high levels of burnout, which suggests that over a third of all embryologists in Spain are at high risk of burnout syndrome [8]. These findings may have troubling implications, given the growing evidence linking burnout to lower quality of care [28].
Exhaustion has been related to overload and lack of control over results and decision-making, and mainly reflects feelings about the organizational and social climate of the work environment. Low levels of mental health among embryologists could be caused, in part, by their poor adaptation to the climate of the organization [29], for example when expectations about the work environment are contradicted by experience. Cynicism can be related to indifference (an absence of desire to succeed) and an impression of a lack of opportunities for development. These factors could result in a diminished sense of professional worth, low self-esteem and a feeling of frustration and boredom, which according to our results would have a negative impact on the embryologists’ MCS-12 scores. Although the bivariate analysis revealed differences in mental health scores between the different tertiles of the efficacy subscale, these dimensions did not provide new information on MCS-12 other than that provided by the exhaustion and cynicism dimensions. This apparent inconsistency is the result of the control exerted by some variables over others when they are all consolidated within the regression model.
The prevalence of burnout among Spanish embryologists (36.3 %) is greater than that observed in other clinical laboratory staff (8.6 % of pathologists) [7], and that observed in physicians (22 %) [24, 30], but lower than that described in surgeons (47.6 %) [3] or obstetricians (ranging from 36 to 58 %) [5, 31, 32]. Care should be taken when comparing the prevalence of burnout, as discrepancies have been reported in the criteria used for its definition after using MBI [33–35]. Future studies should examine certain factors that correlate with burnout, such as personal traits (for example, self-esteem), organizational questions (for example, organizational support, human resources and materials), work-related factors (for example, workload, weekend work, salary-satisfaction, physical and environmental conditions, staggered shifts) and social factors (for example, work-family conflict).
The lower scores recorded for mental health could account for the fact that fewer embryologists believe that at age 60 they will be doing the same work, compared to a reference population. Although the differences were not statistically significant, the average MCS-12 was lower among embryologists who did not expect to be doing the same work at age 60 than among those who did.
Various measures have been described for preventing burnout syndrome, some of which are related to contextual factors (such as increasing professional autonomy and control, decreasing administrative burdens, improving organisational support or providing models of low-threshold support for persons in need), while others are related to personal well-being and social support (for example, participating in research, continuing educational activities outside work, paying particular attention to important personal relationships and spiritual practices, recognizing the importance of one’s work, cultivating personal interests outside work, and creating a balance between personal and professional life) [3]. Recently, Gerber et al. (2013) [36] highlighted the utility of aerobic exercise training to reduce stress and prevent the development of deeper depression in workers with burnout syndrome.
Gender is an independent factor for MCS-12; women have lower MCS-12 scores, and so the gender factor provides new information on MCS-12, other than that provided by the dimensions of exhaustion and cynicism. This result coincides with that observed in other studies of predictors of mental health among physicians. In these studies, the lower mental health scores observed among female physicians were found to be related more to a pattern of over exertion (over commitment) than burnout [24, 37]. This over exertion can lead to an interference of work with other concerns and increase the work-family conflict [38, 39]. This conflict occurs when the demands of working life are incompatible with the demands of family life [40]. Several authors [4] have reported that women are more prone to suffer work-family conflict, which could partly account for our findings. The interaction between work and home is considered an important factor in mental health [40, 41]. The fact that, in our study, MCS-12 is not related to having children or to being in a stable relationship suggests that issues related to family-work conflicts are not the only factors underlying the relation observed between gender and MCS-12. Other authors have suggested that the higher levels of work-related stress observed among women may result from structured but implicitly different gender-related work expectations that come from a variety of important sources, such as patients, colleagues, administrators or co-workers. These expectations may work in such a way as to be built into the job of being a woman embryologist [42].
Limitations
Although our response rate was similar to that achieved in other studies using similar on-line data collection procedures [29, 43, 44] and there were no significant differences in gender balance or type of laboratory between respondents and total ASEBIR members, the risk of some biased responses (for example, embryologists with poor work conditions could be more motivated to participate) cannot be ruled out. Because the data for the mailing were provided by ASEBIR, the conclusions drawn may not be applicable to all Spanish embryologists or to other countries. Nevertheless, the fact that the results obtained for some occupational variables (such as type of laboratory: public or private) are similar to those described for Spain in general [45], leads us to believe that our findings could have a high degree of external validity nationwide. However, any extrapolation of these findings to embryologists working in other countries should be performed with caution, because of large differences in the size of laboratories. Thus, the proportion of small laboratories (<200 IVF cycles/year) in Spain and Italy is much higher (>40 %) than that found in other countries with similar levels of activity (<10 %) [46].
In addition, our BMI values were calculated from self-reported height and weight, and studies have suggested that some respondents, especially women, tend to overestimate their height and underestimate their weight, leading to an underestimation of BMI [47, 48] whereas others, including men and older adults, tend to over-report weight [49]. These misclassifications will tend to bias findings toward detecting no difference and might underestimate potential differences across BMI. However, our multivariable models were adjusted for these demographic factors.
Although we used hours worked per week as a general indicator of embryologists overworking, other factors are also likely to contribute to overwork among embryologists; such factors include weekend work, unpaid overtime after the end of the working day, or the obligation to be in mobile phone contact 24 h a day, 7 days a week. These conditions have been reported to impact negatively on mental health among other healthcare workers [50].
Embryologists play various roles in ART centres. In some clinics, they are in constant direct contact with the patients, while in others the embryologists’ activities are restricted to laboratory work, and they have no contact with external clientele. This variability in the roles of embryologists may influence the prevalence of burnout, as burnout syndrome is observed more often among professionals in closer contact with persons [2]. Our study did not take into account the type of activity carried out by the embryologists, but in order to prevent this factor from influencing the results presented, we used the MBI-General Survey (MBI-GS) rather than the Human Services Survey (MBI-HSS), which is more widely used for healthcare workers who work in direct contact with people. MBI-GS is valid for analysing burnout syndrome both among professionals dedicated to services and among those involved in other activities, and its results are comparable with those obtained with MBI-HSS [9, 51]. Embryologists always have to meet the demands of internal clientele (gynaecologists, andrologists, managers, etc.), and this task is demanding not only regarding the immediate evidence of outcome success or failure (pregnancy rates), but also, in many cases, in terms of the unsatisfactory institutional conditions in which their work must be carried out.
In conclusion, the present study shows that embryologists’ physical health status is better than that of a reference population. As is the case with other clinical laboratory staff, musculoskeletal complaints and visual discomfort are inversely related with the embryologists’ physical health status. Moreover, there is an inverse relationship between the number of hours worked and BMI, on the one hand, and physical health status, on the other. Embryologists, especially women, present poor levels of mental health related to burnout syndrome. Since this syndrome has been related with potentially substandard patient care and with errors, strategies for improving conditions in the workplace are of fundamental importance. Attention should be paid not only to working time but also to qualitative aspects of work. Finally, strategies to reduce occupational stress and problems should form part of the training provided for clinical embryologists.
Acknowledgements
We would like to thank the ASEBIR executive committee and the staff of the ASEBIR secretariat. We also thank all the ASEBIR members for their cooperation.
Conflict of interest
None declared.
Footnotes
Capsule
Embryologists’ physical health status is better than that of a reference population. However, embryologists, especially women, present poor levels of mental health related to burnout syndrome.
This article is related to the Ph.D. Doctoral thesis by B. López-Lería.
References
- 1.Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav. 1981;2:99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 2.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 3.Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons; understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009;144:371–376. doi: 10.1001/archsurg.2008.575. [DOI] [PubMed] [Google Scholar]
- 4.Adams S, Györffy Z, Susanszky E. Physician burnout in Hungary: a potential role for work family conflict. J Health Psychol. 2008;13:847–856. doi: 10.1177/1359105308095055. [DOI] [PubMed] [Google Scholar]
- 5.Fontán IM, Dueñas JL. Burnout syndrome in an obstetrics and gynaecology management unit. Rev Calid Asist. 2010;25:260–267. doi: 10.1016/j.cali.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 6.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Fritzsche FR, Ramach C, Soldini D, Caduff R, Tinguely M, Cassoly E, et al. Occupational health risks of pathologists–results from a nationwide online questionnaire in Switzerland. BMC Public Health. 2012;12:1054–1066. doi: 10.1186/1471-2458-12-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schaufeli WB, Leiter MP, Maslach C, Jackson SE. The Maslach Burnout inventory-general survey. In: Maslach C, Jackson SE, Leiter MP, editors. Maslach burnout inventory manual. Palo Alto: Consulting Psychologists Press; 1996. pp. 19–26. [Google Scholar]
- 9.Gil-Monte PR. Factorial validity of the Spanish adaptation of the Maslach Burnout Inventory-General Survey. Salud Publica Mex. 2002;44:33–40. doi: 10.1590/S0036-36342002000100005. [DOI] [PubMed] [Google Scholar]
- 10.European Foundation for the Improvement of Living and Working Conditions: http://www.eurofound.europa.eu/surveys/smt/ewcs/ewcs2010_07_07.htm.
- 11.Vilagut G, Valderasa JM, Ferrera M, Garina O, López-García E, Alonso J. Interpretación de los cuestionarios de salud SF-36 y SF-12 en España: componentes físico y mental. Med Clin (Barc) 2008;130:726–735. doi: 10.1157/13121076. [DOI] [PubMed] [Google Scholar]
- 12.Bresó E, Salanova M, Schaufeli W, Nogareda C. NTP 732: Sindrome de estar quemado por el trabajo “Burnout” (III): Instrumento de medición. INSHT. Ministerio de Trabajo y Asuntos Sociales, España. 2003. http://www.insht.es/InshtWeb/Contenidos/Documentacion/FichasTecnicas/NTP/Ficheros/701a750/ntp_732.pdf Last accessed 8 August 2013.
- 13.Frank E. Physician health and patient care. JAMA. 2004;291:637. doi: 10.1001/jama.291.5.637. [DOI] [PubMed] [Google Scholar]
- 14.Thompson SK, Mason E, Dukes S. Ergonomics and cytotechnologists: reported musculoskeletal discomfort. Diagn Cytopathol. 2003;29:364–367. doi: 10.1002/dc.10377. [DOI] [PubMed] [Google Scholar]
- 15.Hartvigsen J, Lings S, Leboeuf-Y de C, Bakketeig L. Psychosocial factors at work in relation to low back pain and consequences of low back pain; a systematic, critical review of prospective cohort studies. Occup Environ Med. 2004;61:e2. [PMC free article] [PubMed] [Google Scholar]
- 16.Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol. 2004;14:13–23. doi: 10.1016/j.jelekin.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 17.Lorusso A, Bruno S, Caputo F, et al. Risk factors for musculoskeletal complaints among microscope workers. G Ital Med Lav Ergon. 2007;29:932–937. [PubMed] [Google Scholar]
- 18.Kawada T, Ooya M. Workload and health complaints in overtime workers: a survey. Arch Med Res. 2005;36:594–597. doi: 10.1016/j.arcmed.2005.03.048. [DOI] [PubMed] [Google Scholar]
- 19.Krantz G, Berntsson L, Lundberg U. Total workload, work stress and perceived symptoms in Swedish male and female white collar employees. Eur J Public Health. 2005;15:209–214. doi: 10.1093/eurpub/cki079. [DOI] [PubMed] [Google Scholar]
- 20.Yancy WS, Jr, Olsen MK, Westman EC, Bosworth HB, Edelman D. Relationship between obesity and health-related quality of life in men. Obes Res. 2002;10:1057–1064. doi: 10.1038/oby.2002.143. [DOI] [PubMed] [Google Scholar]
- 21.Wee CC, Davis RB, Hamel MB. Comparing the SF-12 and SF-36 health status questionnaires in patients with and without obesity. Health Qual Life Outcomes. 2008;6:11–18. doi: 10.1186/1477-7525-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Katz DA, McHorney CA, Atkinson RL. Impact of obesity on health-related quality of life in patients with chronic illness. J Gen Intern Med. 2000;15:789–796. doi: 10.1046/j.1525-1497.2000.90906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gill SC, Butterworth P, Rodgers B, Mackinnon A. Validity of the mental health component scale of the 12-item Short-Form Health Survey (MCS-12) as a measure of common mental disorders in the general population. Psychiatry Res. 2007;152:63–71. doi: 10.1016/j.psychres.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Voltmer E, Schwappach DL, Frank E, Wirsching M, Spahn C. Work-related behavior and experience patterns and predictors of mental health in German physicians in medical practice. Fam Med. 2010;42:433–439. [PubMed] [Google Scholar]
- 25.Bovier PA, Arigoni F, Schneider M, Gallacchi MB. Relationships between work satisfaction, emotional exhaustion and mental health among Swiss primary care physicians. Eur J Public Health. 2009;19:611–617. doi: 10.1093/eurpub/ckp056. [DOI] [PubMed] [Google Scholar]
- 26.Benson S, Hahn S, Tan S, Mann K, Janssen OE, Schedlowski M, et al. Prevalence and implications of anxiety in polycystic ovary syndrome: results of an internet-based survey in Germany. Hum Reprod. 2009;24:1446–1451. doi: 10.1093/humrep/dep031. [DOI] [PubMed] [Google Scholar]
- 27.Abbott JA, Hawe J, Clayton RD, Garry R. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2–5 year follow-up. Hum Reprod. 2003;18:1922–1927. doi: 10.1093/humrep/deg275. [DOI] [PubMed] [Google Scholar]
- 28.West CP, Tan AD, Habermann TM, et al. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302:1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 29.Montero-Marín J, Araya R, Blazquez BO, Skapinakis P, Vizcaino VM, García-Campayo J. Understanding burnout according to individual differences: ongoing explanatory power evaluation of two models for measuring burnout types. BMC Public Health. 2012;12:922–933. doi: 10.1186/1471-2458-12-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright JG, Khetani N, Stephens D. Burnout among faculty physicians in an academic health science centre. Paediatr Child Health. 2011;16:409–413. doi: 10.1093/pch/16.7.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palmer-Morales Y, Prince-Vélez R, Searcy-Bernal R. Burnout syndrome associated factors in gynecologists. Ginecol Obstet Mex. 2007;75:379–383. [PubMed] [Google Scholar]
- 32.Yoon JD, Rasinski KA, Curlin FA. Conflict and emotional exhaustion in obstetrician gynaecologists: a national survey. J Med Ethics. 2010;36:731–735. doi: 10.1136/jme.2010.037762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trufelli DC, Bensi CG, Garcia JB, Narahara JL, Abrão MN, Diniz RW, et al. Burnout in cancer professionals: a systematic review and meta-analysis. Eur J Cancer Care (Engl) 2008;17:524–531. doi: 10.1111/j.1365-2354.2008.00927.x. [DOI] [PubMed] [Google Scholar]
- 34.Nienhaus A, Westermann C, Kuhnert S. Burnout among elderly care staff. A review of its prevalence. Bitusnsdcehsugtzesundheitsblatt-Gesund. 2012;55:211–222. doi: 10.1007/s00103-011-1407-x. [DOI] [PubMed] [Google Scholar]
- 35.Roberts DL, Cannon KJ, Wellik KE, Wu Q, Budavari AI. Burnout in inpatient-based versus outpatient-based physicians: a systematic review and meta-analysis. J Hosp Med. 2013;8(11):653–664. doi: 10.1002/jhm.2093. [DOI] [PubMed] [Google Scholar]
- 36.Gerber M, Brand S, Elliot C, Holsboer-Trachsler E, Pühse U, Beck J. Aerobic exercise training and burnout: a pilot study with male participants suffering from burnout. BMC Res Notes. 2013;6:78–86. doi: 10.1186/1756-0500-6-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buddeberg-Fischer B, Klaghofer R, Buddeberg C. Arbeitsstress und gesundheitliches Wohlbefinden junger Ärztinnen und Ärzte. Z Psychosom Med Psychother. 2005;51:163–178. doi: 10.13109/zptm.2005.51.2.163. [DOI] [PubMed] [Google Scholar]
- 38.Peeters MCW, de Jonge J, Janssen PPM, van der Linden S. Work-home interference, job stressors, and employee health in a longitudinal perspective. Int J Stress Manag. 2004;11:305–322. doi: 10.1037/1072-5245.11.4.305. [DOI] [Google Scholar]
- 39.Dikkers JS, Geurts SA, Kinnunen U, Kompier MA, Taris TW. Crossover between work and home in dyadic partner relationships. Scand J Psychol. 2007;48:529–538. doi: 10.1111/j.1467-9450.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- 40.Hämmig O, Bauer GF. Work-life imbalance and mental health among male and female employees in Switzerland. Int J Public Health. 2009;54:88–95. doi: 10.1007/s00038-009-8031-7. [DOI] [PubMed] [Google Scholar]
- 41.Knecht M, Bauer GF, Klaghofer R, Buddeberg-Fischer B, Stamm M, Hämmig O. Work-life conflicts and health among Swiss physicians–in comparison with other university graduates and with the general Swiss working population. Swiss Med Wkly. 2010;140:w13063. doi: 10.4414/smw.2010.13063. [DOI] [PubMed] [Google Scholar]
- 42.McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K. The work lives of women physicians: results from the physician work life study. The SGIM Career Satisfaction Study Group. J Gen Intern Med. 2000;15:372–380. doi: 10.1111/j.1525-1497.2000.im9908009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaplowitz MD, Hadlock TD, Levine R. A comparison of web and mail survey response rates. Public Opin Q. 2004;68:94–101. doi: 10.1093/poq/nfh006. [DOI] [Google Scholar]
- 44.Heiervang E, Goodman R. Advantages and limitations of web-based surveys: evidence from a child mental health survey. Soc Psychiatry Psychiatr Epidemiol. 2011;46:69–76. doi: 10.1007/s00127-009-0171-9. [DOI] [PubMed] [Google Scholar]
- 45.Castilla JA, Hernandez E, Cabello Y, Navarro JL, Hernandez J, Gomez JL, et al. Assisted reproductive technologies in public and private clinics. Reprod Biomed Online. 2009;19:872–878. doi: 10.1016/j.rbmo.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 46.Ferraretti AP, Goossens V, Kupka M, Bhattacharya S, de Mouzon J, Castilla JA, et al. Assisted reproductive technology in Europe, 2009: results generated from European registers by ESHRE. Hum Reprod. 2013;28:2318–2331. doi: 10.1093/humrep/det278. [DOI] [PubMed] [Google Scholar]
- 47.Rowland ML. Self-reported weight and height. Am J Clin Nutr. 1990;52:1125–1133. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 48.Jefferey RW. Bias in reported body weight as a function of education, occupation, health and weight concern. Addict Behav. 1996;21:217–222. doi: 10.1016/0306-4603(95)00050-X. [DOI] [PubMed] [Google Scholar]
- 49.Villanueva EV. The validity of self-reported weight in US adults: a population based cross-sectional study. BMC Public Health. 2001;1:11. doi: 10.1186/1471-2458-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tokuda Y, Hayano K, Ozaki M, Bito S, Yana H, Koizumi S. The interrelationships between working conditions, job satisfaction, burnout and mental health among hospital physicians in Japan: a path analysis. Ind Health. 2009;47:166–172. doi: 10.2486/indhealth.47.166. [DOI] [PubMed] [Google Scholar]
- 51.Gil-Monte PR. Factorial validity of the Maslach Burnout Inventory (MBI-HSS) among Spanish professionals. Rev Saude Publica. 2005;39:1–8. doi: 10.1590/S0034-89102005000100001. [DOI] [PubMed] [Google Scholar]