Abstract
Previous research suggests positive effects of health information seeking on prevention behaviors such as diet, exercise and fruit and vegetable consumption. The current study builds upon this research, and strengthens causal claims from it, by examining the lagged effect of patient-clinician information engagement (PCIE) on fruit and vegetable consumption as well as the indirect effect on the outcome through seeking information from nonmedical channels. The results are based on data collected from a randomly drawn sample of breast, prostate and colorectal cancer patients from the Pennsylvania Cancer Registry who completed mail surveys in the Fall of 2006 and 2007. There was a 65% response rate for baseline subjects (resulting n = 2,013); of those 1,293 were interviewed one year later and 1,257 were available for our analyses. Results show a positive lagged main effect of PCIE at baseline on fruit and vegetable consumption at follow-up (B = 0.26, SE = 0.10, p = 0.01). The mediation analysis shows that patient-clinician information engagement leads to increased fruit and vegetable consumption among cancer patients, in part through patients’ information seeking from non-medical channels. Implications of these findings for the cancer patient population and for physicians are discussed.
Keywords: Patient-clinician communication, cancer survivors, fruit and vegetable consumption information seeking
Introduction
In recent years, the health information environment has become increasingly crowded and complex. Individuals can access a wide range of channels of information spanning a broad range of topics related to health (Niederdeppe, Frosch, & Hornik, 2008; Viswanath, 2005). In addition, health advocates have begun to encourage patients to take greater responsibility for their health and to increase their participation in the decision-making process (Frosch & Kaplan, 1999). Consequently, many scholars have become interested in exploring the role of patients’ information seeking from media channels (including the Internet), and interpersonal channels, on their decisions about their health and involvement in health practices.
While these endeavors are opportune in light of the increasingly pivotal role of new communication technologies in our lives as well as the increased coverage of health issues in the news, it is also important to understand how information obtained from physicians affects health behaviors. Specifically, in response to the shift from a traditional, paternalistic paradigm of health care delivery to a patient-centered paradigm which emphasizes more shared medical decision making, the current research examines whether medical and nonmedical channels of information work together to shape a health behavior (i.e. fruit and vegetable consumption) among cancer patients, or whether the influence of one information channel is independent of the other.
The Role of Fruit and Vegetable Consumption
Over the last two decades, researchers have debated the role of fruit and vegetable consumption in reducing overall cancer risk. While some of these studies suggest that consumption of fruits and vegetables reduces risk of developing cancers such as breast (Gandini, Merzenich, Robertson, & Boyle, 2000), prostate (McCann, Ambrosone, Moysich, Brasure et al. 2005) and colorectal cancers (Block et al., 1992; Block, Patterson, & Subar, 1992; Gandini, Merzenich, Robertson, & Boyle, 2000; Steinmetz & Potter, 1996), other studies have failed to provide definitive support for the link between fruit and vegetable intake and cancer risk, noting that the relationship was much weaker than initially reported (Boffetta et al., 2010; Key, 2011; Willett, 2001; Willett, 2010).
Despite these differences in opinion with regards to the importance of fruit and vegetable intake in reducing overall cancer risk, evidence argues for a probable protective effect of fruit and vegetable consumption on cancer risk. Specifically, an expert report by the World Cancer Research Fund noted that studies conducted since the mid-1990s have supported this claim (American Institute for Cancer Research, 2007, Chapter 4.2, p. 75).
In addition, there is evidence to suggest that fruit and vegetable consumption can improve cancer patients’ lives by preventing the onset or progression of chronic conditions like cardiovascular diseases (Dauchet, Amouyel, Hercberg, & Dallongeville, 2006; He, Nowson, & MacGregor, 2006; Yusuf, Razeghi, & Yeh, 2008), high blood pressure, diabetes (Bazzano, 2005), weight management (Tohill, 2005) and bone health (New et al., 2000). Together, these findings highlight the importance of consuming fruits and vegetables, and have led to a general recommendation favoring increased fruit and vegetable intake among the general population and cancer patients alike (ACS, 2009). Furthermore, these findings also show that efforts to promote fruit and vegetable consumption are worthwhile and should be encouraged.
Health Information Seeking Behavior
In recent years, health information seeking has come to include a range of dimensions spanning from the nature of information sought, the use of channels to seek information, as well as how various information-seeking strategies are used to obtain information (Lambert & Loiselle, 2007). Scholars have noted the need to expand the current body of research beyond a focus on general health information seeking or seeking in specific contexts (e.g., Brashers, Goldsmith, & Hsieh, 2002) to a focus on research that crosses settings and contexts. One conceptual framework which aims to address this call is the planned risk information seeking model (PRISM: Kahlor, 2010). The PRISM (Kahlor, 2010), which draws from concepts outlined in several health theories1, provides health communication scholars with a unifying framework for health information seeking, which aims to enable scholars to propose universal claims and hypotheses relating to information seeking and its effects, which can be applied beyond specific contexts2.
However, PRISM (Kahlor, 2010) does not theorize about the movement across channels, nor considers the role of social determinants in shaping health information seeking behavior. Current empirical studies suggest that engaging with information from one channel can also trigger additional information seeking activities from other channels (Caiata-Zufferey, Abraham, Sommerhalder, & Schulz, 2010; Nagler, Romantan et al., 2010), and that these activities can jointly influence behaviors. In particular, Shah and colleagues found that mass communication influences individuals’ civic engagement indirectly through interpersonal discussions (Shah, Cho, Eveland, & Kwak, 2005; Shah et al., 2007). Research using the social diffusion theory supports these conclusions in the context of health campaign influence, postulating that campaign messages can ultimately affect individuals’ health behaviors by motivating them to engage in interpersonal communication within their social networks (Hornik & Yanovitzky, 2003; Hwang, 2010; Rogers, 2003).
Furthermore, any study of health information seeking should take into account of the role of social determinants in the context of cancer communication and outcomes. Past research has shown that patient characteristics such as race or ethnicity (Ball-Rokeach & Wilkin, 2009), willingness to communicate about health (Wright & Frey, 2008), socioeconomic status (Perloff, Bonder, Ray et al, 2009), and perceptions of trust in the medical system can affect levels of health information seeking behaviors. According to the structural influence model of communication (SIM: Viswanath, Ramanadhan, & Kontos, 2007), health information seeking may act as an explanatory variable in understanding the processes that shape health disparities as well. This framework argues that inequalities in communication behaviors, including information seeking, tend to parallel inequalities in health: “individual and population health could be understood by examining how social determinants such as race, ethnicity, and class are related to how people access, seek, process, and use health information” (Viswanath & Ackerson, 2011, p. e14550). In the context of this article, however, the social determinants of health, while important predictors of information seeking, are included in order to account for the effect of external influences on proposed outcomes. Addressing their relationship to the study outcomes is not a focus of this paper.
The central variable in the current study is patient-clinician information engagement (PCIE) which we have defined as: doctors’ offering information and advice to patients as well as patient-initiated searches of information from physicians (Martinez 2009). Ultimately, the goal is to examine the role of information seeking behavior in influencing individuals’ health practices and behaviors, particularly fruit and vegetable consumption. Prior research has demonstrated a positive association of information seeking behavior with fruit and vegetable intake (Hornik, Parvanta, Mello, Freres, & Schwartz, 2010; Lewis et al., 2012; Ramirez, Freres, Martinez, Lewis, & Hornik, 2011; Shim, Kelly, & Hornik, 2006), as well as with dieting and exercise behaviors (Tan, Mello, & Hornik, 2012; Shim et al, 2006; Ramirez, Freres, Martinez et al,2013). However, these studies do not describe the effect of information obtained within the healthcare setting on patients’ adoption of lifestyle behaviors. A number of studies have focused specifically on the positive behavioral impact of doctors’ recommendations or advice to patients to increase their consumption of fruits and vegetables (Hunt, Kristal, White, Lynch, & Fries, 1995; Loureiro & Nayga, 2007; Pignone et al., 2003; Sacerdote et al., 2006). However these studies focused less on the role of the patient’s own engagement with their treating physicians or other health professionals for information; they do not address how this participatory aspect of the interaction may contribute to patients’ adoption of preventive practices including their fruit and vegetable intake. With our measure of patient-clinician information engagement (PCIE) we hope to capture both fundamental components of patient centered communication (Roter, 1984).
Building on previous research reviewed here, we propose that engaging with information from medical channels (i.e., clinicians) affects individuals’ fruit and vegetable consumption in part because it triggers additional engagement with channels outside the healthcare system. Figure 1 illustrates the proposed pathways of influence. We outline two potential reasons for expecting this mechanism. First, in an environment in which patients enjoy access to an increasingly broad range of information channels, and also assume greater responsibility for, and involvement in decision-making regarding their health, it is reasonable to expect that discussions with the medical team may fuel additional seeking activities from other channels. Accordingly, qualitative studies have noted that patients sometimes respond to discussions with physicians by turning to nonmedical channels of information to complement, validate and/or challenge the information obtained during the medical encounter (Caiata-Zufferey et al., 2010). Second, clinicians may recognize the shift towards greater patient participation and input in healthcare and encourage their patients to seek information from other channels to further their knowledge about how various habits and lifestyle practices may affect their disease progression or health in general (Lewis, Gray, Freres, & Hornik, 2009). Based on our summary of the current findings, we propose the following two hypotheses:
H1: Cancer patients’ engagement with cancer-related information from their treating physicians or health professionals (PCIE) at baseline will be positively associated with their intake of fruits and vegetables at follow-up adjusting for effects of additional predictors.
H2: The positive association between PCIE and patient intake of fruits and vegetables will be partially mediated by information seeking from nonmedical channels.
Figure 1.
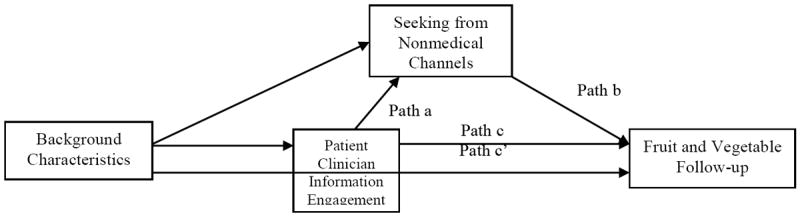
Proposed Mediation Path Between Patient-Clinician Information Engagement (PCIE) and Fruit and Vegetable Consumption.
The current study builds on a previous study which examined the same sample of cancer patients and demonstrated that information seeking from nonmedical channels had a positive lagged association with fruit and vegetable intake (Lewis et al., 2012). The previous study included a measure of patient clinician information engagement as an additional predictor and found no residual main effect when non-medical seeking was in the equation. In contrast, the current study, focuses on PCIE, and complements that previous work; it looks for evidence for effects of PCIE as an antecedent variable on fruit and vegetable consumption, mediated through non-medical seeking.
Method
Participants
In the Fall of 2006, we randomly selected from the Pennsylvania Cancer Registry (PCR) patients who were diagnosed in 2005 with three of the most common cancers in the US (breast – women only, prostate – men only, colorectal) (n = 2,013). Pennsylvania requires that all cancer cases be reported to the PCR within six months of diagnosis. Stage four cancer patients and African-American patients were over-sampled to maximize statistical power. However, in the weighted analyses conducted here these groups are represented in proportion to their presence in the population in the PCR.
Upon completing the first survey, respondents were asked if they agreed to be contacted again in 2007 for a follow-up questionnaire. Approximately 65% percent of the initial sample was retained for the follow-up survey (n = 1,293). In the current analyses, only respondents who completed both surveys (baseline and follow-up) and offered valid responses on the outcome measure (fruit and vegetable consumption at follow-up), were retained (n=1,257).
Procedure
The survey instruments were developed after extensive literature reviews, consultations with expert panels and a pilot study with 29 cancer patients. The questionnaires were tailored to the type of respondents’ cancer and included questions about demographic and disease characteristics, information seeking activities, engagement with physicians, psychosocial factors and preventive and surveillance behaviors. They were distributed to respondents based on recommended methods for mail surveys (Dillman, 2000). The baseline data were collected in Fall 2006 while the follow-up survey was administered in Fall 2007. A more detailed description of the study design and data collection procedures is found elsewhere (Lewis et al., 2009; Martinez, Schwartz, Freres, Fraze, & Hornik, 2009; Nagler et al., 2010).
Measures
Independent Variable
Patient-Clinician Information Engagement (PCIE)) is described in more detail in other studies (Martinez et al., 2009; Tan, Bourgoin, Gray, Armstrong, & Hornik, 2011). However, to summarize, participants were asked to think back to the first few months of their cancer diagnosis and recall whether they sought information about ‘cancer treatment,’ ‘other cancer-related issues’ and ‘quality of life’ from two medical sources; they were asked separately about their treating physicians and about other health professionals. Patients responded on a yes/no scale. The period of recall was from the time of diagnosis to roughly one year post-diagnosis. In addition to these six survey items, the scale includes two more yes/no items which capture (1) whether cancer survivors discussed information they obtained from other channels with their treating doctors and, of particular importance for this study, (2) if their treating doctors recommended other channels for further information. The yes/no responses to these eight items were first individually standardized and then averaged to create the baseline PCIE measure (Cronbach alpha = 0.78).
Mediator Variable
Information Seeking from Nonmedical Channels (Nonmedical Seeking) focused on respondent’s breadth of information seeking activities from nonmedical channels about two general topics: cancer treatment or other cancer-related issues, and quality of life. The nonmedical outlets included: 1) television or radio; 2) books, brochures, or pamphlets; 3) newspapers or magazines; 4) the Internet (other than personal e-mail); 5) family members, friends, or coworkers; 6) other cancer patients; 7) face-to-face support groups; 8) On-line support groups; and 9) telephone hotlines from the American Cancer Society. In addition, to capture the time frame of their seeking behavior, at baseline we asked participants to “think back to the first few months after you were diagnosed with your cancer” and report their seeking behaviors. In contrast, at follow-up we asked them to think back to “the past 12 months.” The responses to these items were also binary with yes/no options. In total, the baseline and follow-up measures included 18 yes/no items which were first standardized individually and then averaged to form the final scales (αbaseline= 0.81; αfollow-up = 0.80).
Dependent Variable
Fruit and Vegetable Consumption
Participants responded to two questions about their level of fruit and vegetable intake: “In the past week, on average, how many servings of fruit did you eat or drink per day? Please include 100% fruit juice, and fresh, frozen or canned fruits.” And “In the past week, on average, how many servings of vegetables did you eat or drink per day, not counting potatoes? Please include green salad, 100% vegetable juice, and fresh, frozen or canned vegetables.” Both items included six response options, ranging from “Less than one serving per day,” “one serving per day,” “two servings per day” up to “5 or more servings per day.” As in Ramirez et al. (2011) and Lewis et al. (2012), we combined both measures to create a composite measure of fruit and vegetable intake, with interval-level, response options for each question, ranging from 0 to 5 levels. The summed variable ranged from 0 to 10 levels. Although the extreme categories (0 and 5) of each measure captured multiple responses, fewer than 5% of all respondents fall at the extremes of the 0-10 scale. We thus felt confident in treating this measure as interval. The one year test-retest correlation for the summed scale was high (0.64.) The wording of baseline and the follow-up measures of fruit and vegetable consumption were identical.
Covariates
Disease and Demographic Characteristics
Disease factors were entered in the analyses as additional predictors, including cancer type, stage of cancer, cancer history, self-reported metastatic condition, number of treatments and health status. Cancer type was obtained from the PCR and included breast, prostate and colon cancers. Respondent’s cancer stage, which was consistent with the standard IUCC/TNM system of cancer staging (Greene et al., 2002), was also derived from the PCR. In our analyses, gender and cancer type were combined to create four dichotomous items (i.e. colon cancer male, colon cancer female, breast cancer and prostate cancer) while cancer stage was dichotomized to reflect patients with metastatic cancer versus those with stages 0 through III.
Respondents indicated if they had any family members diagnosed with their same type of cancer (cancer history) and whether their physician has told them the cancer has recurred or progressed in the previous year (becoming metastatic). We also included a measure of how many different types of treatment patients underwent for their cancer. This index was standardized within each cancer since the number of treatments available was different for each type of cancer. In addition, we assessed respondents’ self-perceived health status using a standard item with five-response options ranging from poor to excellent. Demographic characteristics were also included: age in years, race (white vs. other), education (any college vs. high school or less), marital status (married vs. not married) and employment status (employed vs. unemployed). Due to lack of variability, insurance status was omitted from our list of controls - 98% of our sample claimed to have insurance.
In addition to these typical disease and demographic characteristics, other potential confounders include ‘intention to control your diet to lose weight in the next year,’, ‘intention to engage in physical activity at least three times a week in the next year,’ and body mass index (BMI). Intention responses ranged from very likely to very unlikely. The BMI was calculated from self-reported height and weight and was coded as normal (BMI less than 25), overweight (BMI 25 to 34.99) or obese (BMI 35 and over).
Data Analysis
Following standard procedures for datasets where missing values cause the loss of more than 10% of cases, variables were multiply imputed using the ICE add-in for STATA Release 11 through a single multivariate model (Allison, 2001). In addition, we used post-stratification weights to adjust the final sample to the PCR population by type of cancer, age, gender, race, marital status, time of diagnosis and disease stage at diagnosis.
We performed a series of OLS regression analyses to test our main hypotheses of mediated effects. First, we examined the lagged association between PCIE at baseline on fruit and vegetable consumption at follow-up, controlling for baseline behavior, demographics, patient characteristics, and other predictors. We then examined the mediation mechanism, which is portrayed in Figure 1. The decision to perform the mediation test with longitudinal data was based on previous research showing potential biases in mediation analyses relying on cross-sectional data (Cole & Maxwell, 2003).
Our analysis represents a test of simple mediation (Preacher, Rucker, & Hayes, 2007), one in which the indirect effect of PCIE (independent variable) on fruit and vegetable consumption (dependent variable) operates in part through seeking information from nonmedical channels (mediating variable)3. We base our approach to mediation analysis on MacKinnon et al. (2002) which has many advantages over the prior Baron and Kenny (1986) logic. According to the MacKinnon approach, a mediation mechanism is supported if (1) the independent variable is significantly related to the mediator (path a) and (2) the mediator is significantly related to the dependent variable while controlling for the independent factor (path b).
Using two waves of data, it was essential to use a half-longitudinal design (Cole & Maxwell, 2003). For this approach, Cole & Maxwell (2003) recommended a pair of longitudinal tests. In line with their suggestions we first examined the lagged relationship between the independent factor at baseline and the mediator at follow-up controlling for additional predictors and the mediator at baseline. We then assessed the lagged relationship between the mediator at baseline and the outcome at follow-up, adjusting for additional predictors and outcome measured at baseline. The benefit of this design was that it allowed us to control for prior levels of the dependent and mediator variables.
Results
Descriptive Analysis
The final sample included 1,257 cancer survivors. The mean age for the sample was 67 years old. The majority of our sample (88%) was white, with 11% of the sample self-identifying as African American4. Additional characteristics of the sample are found in Table 1. Our sample also reported consuming, on average, less than the recommended number of servings of fruits and vegetables. However, a slight increase in consumption was observed between baseline and follow-up (Table 2). The procedure for creating the information scales (summing standardized items at each measurement wave) meant that the observed mean would be close to 0 at both measurement waves so there would be minimal observed change in information engagement over the year’s period. The descriptive analysis shows that the correlations among the primary variables were all statistically significant at the 0.01 level or less and in the expected direction (Table 3). When examining the unstandardized version of the PCIE scale, 62.7% of patients discussed information from other sources with their treating physician and 44.7% received encouragement from their physician to seek information from other sources. Only 11% of the sample did not seek information from their physician at all at baseline. In contrast, 17.7% and 36.8% of the sample did not seek information from any nonclinical sources at baseline and follow-up respectively.
Table 1.
Disease and Demographic Characteristics of the Sample (n = 1,257)
| Mean | SD | % | |
|---|---|---|---|
|
| |||
| Age | 67.74 | 12.45 | |
| Race/Ethnicity | |||
| White | 87.47 | ||
| Non-White | 12.53 | ||
| Education | |||
| High school or less | 51.39 | ||
| Any college | 48.61 | ||
| Marital Status | |||
| Married | 61.16 | ||
| Not Married | 38.84 | ||
| Employment Status | |||
| Employed | 33.65 | ||
| Non-Employed | 66.35 | ||
| BMI | |||
| Normal | 30.77 | ||
| Overweight | 39.47 | ||
| Obese | 29.76 | ||
| Type of Cancer | |||
| Colon Cancer Male | 15.38 | ||
| Colon Cancer Female | 16.01 | ||
| Prostate Cancer | 33.19 | ||
| Breast Cancer | 35.42 | ||
| Stage | |||
| Stage 0-II | 76.88 | ||
| Stage III | 12.93 | ||
| Stage IV | 10.19 | ||
| Became Metastatic | |||
| Yes | 11.89 | ||
| No | 88.11 | ||
| Health Status (1-5) | 3.20 | 0.90 | |
| Dieting Intention (1-5) | 3.23 | 1.28 | |
| Exercising Intention (1-5) | 3.55 | 1.28 | |
| Number of Treatments | -0.05 | 0.95 | |
Table 2.
Characteristics of Follow-up Sample on Primary Variables (n = 1,257)
| Mean | SD | |
|---|---|---|
|
| ||
| Fruit and Vegetable Consumption Baseline (0-10) | 3.85 | 2.10 |
| Fruit and Vegetable Consumption Follow-up (0-10) | 4.08 | 2.16 |
| Patient-Clinician Information Engagement Baseline | 0.02 | 0.64 |
| Seeking Nonmedical Baseline | 0.00 | 0.49 |
| Seeking Nonmedical Follow-up | -0.04 | 0.44 |
Table 3.
Correlation Matrix of Primary Variables (n = 1,257)
| Patient-Clinician Information Engagement Baseline | Seeking Nonmedical Channels Baseline | Seeking Nonmedical Channels Follow-up | Fruit & Vegetable Consumption Baseline | |
|---|---|---|---|---|
|
| ||||
| Seeking Nonmedical Channels Baseline | 0.755 | |||
| Seeking Nonmedical Channels Follow-up | 0.522 | 0.626 | ||
| Fruit & Vegetable Consumption Baseline | 0.189 | 0.415 | 0.673 | |
| Fruit & Vegetable Follow-up | 0.294 | 0.533 | 0.656 | 0.665 |
All displayed variables are statistically significant at p<.01 or less.
Main Effect
The main hypothesis (H1) posited that engaging with information from medical channels would predict subsequent fruit and vegetable consumption after adjusting for baseline intake of fruits and vegetables as well as disease and demographic characteristics. The results support this hypothesis; baseline PCIE positively predicted fruit and vegetable consumption one year later (B = 0.26, SE = 0.10, p = 0.01), above and beyond the effect of the additional predictors and baseline behavior (path c). This analysis does not include seeking information from nonmedical channels.
Test of Mediation
The second hypothesis postulated that PCIE would indirectly affect fruit and vegetable consumption by increasing engagement with information from channels outside the healthcare system. The results support this hypothesis as well. Following the requirements of the half-longitudinal mediation approach, we showed that patient-clinician information engagement at baseline was positively related to seeking information from nonmedical channels at follow-up (B = 0.05, SE = 0.025 p = 0.045), adjusting for additional predictors and baseline behavior (path a). Additionally, seeking information from nonclinical channels at baseline was significantly related to fruit and vegetable intake at follow-up (B = 0.40, SE = 0.12, p < 0.01) in a model that adjusted for the effect of additional predictors and baseline behavior but excluded the influence of baseline patient-clinician information engagement. Finally, actively seeking information from nonmedical channels at baseline was positively and significantly related to fruit and vegetable consumption at follow-up (B = 0.31, SE = 0.14, p = 0.03) after controlling for baseline PCIE, baseline behavior and additional predictors (path b). In addition, the effect of PCIE at baseline on fruit and vegetable consumption at follow-up was decreased in magnitude (from regression coefficients of 0.26 to 0.15), and lost statistical significance upon introducing the effect of actively seeking information from nonmedical channels at baseline, adjusting for baseline fruit and vegetable consumption and additional predictors (path c’)5.
Thus, we concluded that the results provided evidence in support of partial mediation. In sum, patient-clinician information engagement appears to trigger consumption of fruits and vegetables among cancer survivors directly but also indirectly by encouraging information seeking from channels outside the healthcare system.
Discussion
There is evidence consistent with benefit of fruit and vegetable consumption for cancer patients., This study explores information engagement with medical and nonmedical channels, as potential influences on fruit and vegetable intake among cancer patients at the survivorship stage. Our findings suggest that engagement with clinicians triggers higher intake of fruits and vegetables, in part, because it motivates additional information seeking activities from nonclinical channels.
This result is conceptually intriguing in several ways. First it is consistent with a claim that patients are embedded within a multi-faceted communication network that affects their decisions. The history of communication effects scholarship, starting with its early theorists (cf. Katz and Lazarsfeld, 1955) investigates how mass media effects occur in the context of social networks. While early theorizing often focused on how mass media activated social network diffusion of influence, here the effects run from expert source through mediated and personal channels, perhaps reversing the traditional two-step flow of media effects. But the deeper idea, that media effects and interpersonal effects occur in the context of each other, is certainly supported here., These results support the operation of a de facto participatory patient model in the cancer patient population. Specifically, patients do not end their searches for cancer-related information in their physician’s office but also engage with nonmedical information channels to satisfy their informational needs and to help them make sound decisions about their health. Also, our study provides empirical evidence for a trigger effect of information seeking from clinical channels to seeking from non-medical channels, suggesting that movement across channels represents an important part of the information seeking process, and is worth further study (Nagler, Gray et al, 2010). Qualitative studies have supported this flow from medical to nonmedical outlets (Caiata-Zufferey et al., 2010; Nagler, Romantan et al., 2010). Our study expands this research by confirming the mediation model with a longitudinal study design.
Second, the findings are consistent with and add to previous reports, which highlighted the rising importance of nonmedical channels of information in determining healthy choices (Lee, 2010; Lewis et al., 2012; Ramirez et al. 2011; Shim et al., 2006). Internet use for seeking health information in particular holds much promise for improving perceptions of the patient-provider relationship, question asking, and treatment compliance among newly diagnosed cancer patients (Bass, Ruzek, Gordon, Fleisher, McKeown-Conn, & Moore, 2006). As these channels become more prevalent in patients’ health information environment and central to their decisions, public health practitioners and scholars should encourage greater dissemination of information about positive lifestyle practices through the Internet, coverage in the media, and interpersonal conversations within social networks.
Several design characteristics make the results of this study even more compelling. For instance, we tested the proposed relationships using a longitudinal design, which allowed us to make more confident claims about the causal direction between our main variables. Additionally, we employed a population based sample of breast, prostate and colon cancer patients in Pennsylvania in combination with probability weighting. This allowed us to generalize the results across all patients in the state who were diagnosed with three of the most common types of cancers. Finally, our measure of patient-clinician information engagement included an understudied aspect of patient-physician communication, namely patient-initiated efforts to obtain information from physicians, which are perceived as integral components of patient centered communication (Roter, 1984). This is distinct from previous studies which have examined the effect of clinicians offering information or making recommendations to patients.
However, this study has some limitations. First, the findings presented here cannot be extended to patients with other types of cancers or individuals in other parts of the US. Further studies should examine these patterns with other patient populations. Second, although the hypothesized patterns materialized as expected, the magnitude of follow-up effects are modest, and follow-up behavior is, to a large extent, explained by baseline behavior. This suggests that fruit and vegetable consumption is in great part driven by habit. Although other predictors are significant, they do not radically alter the individuals’ dietary behaviors.
Additionally, the data are based on self-report and are thus subject to possibly fallible patient recall of their interactions with their doctors, with other information channels as well as their involvement in healthy behaviors. Confidence in these measures derives from two sources: first there is consistency in reports one year apart (fruit and vegetable consumption r=.67) non-medical channel seeking (r= 0.630) and for patient clinical information engagement (r=.42). Second, poor measurement would have undermined the finding of effects, so the fact that there is evidence for lagged effects is consistent with adequate measurement, although the effects may be underestimated.
As depicted in the measures section, both patient-clinician information engagement and seeking information from nonmedical channels focus on fairly broad cancer topics such as cancer treatment and quality of life. Thus, we were not able to distinguish how much of survivors’ engagement was specifically related to their actively seeking information about fruits and vegetables within those topics. Nevertheless, we are confident that throughout their engagement with nonclinical channels patients encountered information about fruits and vegetables; cancer organizations and other similar entities widely disseminate the importance of healthy diet during cancer treatment and post-treatment phases and highlight the role of fruits and vegetables in improving quality of life and health in general (Blanchard, Courneya, & Stein, 2008; Brown et al., 2003).
A final limitation relates to the use of a half-longitudinal design to assess the mediational process. This approach assumes that the primary variables are not time-dependent or varying across time, and are thus not in violation of the stationarity assumption. However, our analyses suggest that the correlations of primary variables across both waves of data are moderate to strong in magnitude and their means and standard deviations do not vary substantially from baseline to follow-up. Nevertheless, longitudinal mediation should be assessed ideally with at least three waves of data (Cole & Maxwell, 2003).
In conclusion, this study sheds light into how information obtained from physicians affects health behaviors in the context of a complex health information environment. It concludes that cancer survivors take a two-pronged approach to gathering information by engaging with medical channels, which in turn drives them to media or nonmedical interpersonal outlets of information and that these joint activities have a positive impact on individuals’ lifestyle practices such as fruit and vegetable consumption. These findings extend the work of other scholars who found similar influences of information seeking on behavior, but in different contexts (Hornik & Yanovitzky, 2010; Hwang, 2010; Shah et al., 2007; Shah, Cho, Eveland and Kwak, 2005; Rogers, 2003), showing that these relationships extent beyond one topic and one context. Furthermore, this study makes a unique contribution to the existing literature by introducing the role of patient initiated searches of information from physician, not just nonclinical sources, in shaping individual health behavior. As such, physician recognition of the motivation among patients to seek out information from clinical and nonclinical channels may help them better guide their patients toward more reliable nonclinical channels and more productive use of these channels.
Table 4.
Regression Analysis of the Main Effect of Patient-Clinician Information Engagement on Fruit and Vegetable Consumption at Follow-up (N = 1,257)
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Fruit and Vegetable Consumption Follow-up | Seeking Nonmedical Channels Follow-up | Fruit and Vegetable Consumption Follow-up | Fruit and Vegetable Consumption Follow-up | |||||
|
| ||||||||
| B | SE | B | SE | B | SE | B | SE | |
| Age | 0.014 * | 0.007 | 0.001 | 0.002 | 0.016* | 0.007 | 0.017* | 0.007 |
| Race/Ethnicity | 0.446 * | 0.181 | -0.105* | 0.041 | 0.468** | 0.18 | 0.461* | 0.181 |
| Education | 0.125 | 0.118 | 0.018 | 0.025 | 0.213 | 0.119 | 0.203 | 0.118 |
| Marital Status | 0.063 | 0.12 | 0.018 | 0.029 | 0.063 | 0.119 | 0.063 | 0.119 |
| Employment Status | -0.227 | 0.163 | 0.014 | 0.041 | -0.215 | 0.161 | -0.22 | 0.161 |
| Health Status | -0.029 | 0.07 | -0.016 | 0.014 | -0.021 | 0.07 | -0.019 | 0.07 |
| BMI Overweight | -0.292* | 0.147 | -0.063 | 0.034 | -0.284 | 0.147 | -0.286 | 0.147 |
| BMI Obese | -0.022 | 0.171 | -0.054 | 0.039 | -0.016 | 0.169 | -0.014 | 0.169 |
| Cancer History | -0.004 | 0.116 | 0.02 | 0.024 | -0.02 | 0.115 | -0.015 | 0.115 |
| Stage 0-II | 0.198 | 0.231 | -0.04 | 0.046 | 0.265 | 0.228 | 0.236 | 0.23 |
| Stage III | 0.061 | 0.291 | -0.04 | 0.054 | 0.1 | 0.286 | 0.078 | 0.29 |
| Becoming Metastatic | 0.022 | 0.261 | 0.036 | 0.052 | 0.059 | 0.257 | 0.035 | 0.259 |
| Colon Cancer Male | -0.089 | 0.194 | -0.014 | 0.039 | -0.053 | 0.195 | -0.044 | 0.195 |
| Colon Cancer Female | 0.074 | 0.183 | 0.034 | 0.039 | 0.087 | 0.183 | 0.103 | 0.183 |
| Prostate Cancer | -0.363** | 0.139 | -0.071 | 0.033 | -0.312* | 0.138 | -0.335* | 0.139 |
| Number of Treatments | 0.018 | 0.07 | -0.016 | 0.013 | 0.001 | 0.07 | 0.002 | 0.07 |
| Intention to Diet | 0.036 | 0.057 | 0.022 | 0.013 | 0.027 | 0.056 | 0.027 | 0.056 |
| Intention to Exercise | 0.133 * | 0.061 | 0.019 | 0.012 | 0.133* | 0.061 | 0.130* | 0.061 |
| Fruit and Vegetable Baseline | 0.612*** | 0.029 | - | - | 0.610*** | 0.029 | 0.609 *** | 0.029 |
| Seeking Nonmedical Baseline | - | - | 0.468*** | 0.04 | 0.403*** | 0.122 | 0.306* | 0.136 |
| Patient-Clinician Information Engagement Baseline | 0.258 * | 0.103 | 0.050* | 0.025 | - | - | 0.147 | 0.155 |
| R-squared | 44.50% | 34.80% | 44.60% | 44.70% | ||||
Note:
p-value < .05,
p-value < .01,
p-value < .001.
Model 1 highlights the main effect of the independent factor on the outcome. Model 2 features the effect of the independent factor on the mediator. Model 3 highlights the effect of the mediator on the outcome excluding the effect of the independent factor. Model 4 adds the effect of the independent factor.
Acknowledgments
We are grateful to Katrina Armstrong, MD, Heather Forquer, MPH, Laura Gibson, Ph.D., J. Sanford Schwartz, MD, Andy SL Tan, MBBS, MPH for analytic and editorial contributions.
Research Support: 5P50CA095856-05 and P20-CA095856-06 from the National Cancer Institute
Footnotes
Theory of planned behavior (TPB; Ajzen, 1991), the risk information seeking and processing model (RISP; Griffin, Dunwoody, & Neuwirth, 1999), the theory of motivated information management (TMIM: Afifi & Weiner, 2004), the comprehensive model of information seeking (CMIS: Johnson & Meischke, 1993), the health information acquisition model (HIAM: Freimuth, Stein, & Kean, 1989), the integrative model of online health information seeking (IMOHS: Dutta-Bergman, 2006) and the extended parallel processing model (EPPM: Witte, 1998).
To note, even though we acknowledge that PRISM includes a role for affective responses to risk as triggering information seeking (Kahlor, 2010), similar to RISP (Griffin, Dunwoody, & Neuwirth, 1999), this aspect is not examined in the current study.
Past research examining mediating models of effects have traditionally drawn from the causal steps approach outlined by Baron and Kenny (1986). According to this approach, evidence for a mediating effect is supported when four conditions are fulfilled: (1) the independent variable shows a direct and significant association with the dependent variable (path c); (2) the independent variable demonstrates a significant association with the mediating variable (path a); (3) in turn, the mediating variable shows a significant association with the dependent variable (path b); (4) the direct effect of the independent variable on the dependent variable is weakened or eliminated entirely when the effect of the mediating variable is entered into the model (path c’). Although the use of the causal steps approach is seen ubiquitously in past mediation research, MacKinnon, Fairchild, and Fritz (2007) describe three important limitations to this method. Most relevant to the present study is the limitation of the first requirement in the causal steps approach stating that the independent variable must be significantly associated with the dependent variable, which is particularly problematic for studies attempting to show a lagged association between independent and dependent variables. On the contrary, Mackinnon and Fairchild, (2009) note that mediation processes do not necessarily require the presence of a direct effect between independent and dependent variables. Other limitations related to the causal steps approach also include a general weakened power to detect effects (Fritz & Mackinnon, 2007; MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002), and an inability to assign a numerical value capturing the magnitude of the effect under study (Mackinnon & Fairchild, 2009).
Less than 1% of respondents were of Asian, American Indian, Native Hawaiian or other descent. Among all respondents, 3% considered themselves to be Hispanic or Latino, and of these respondents the majority also identified themselves as white. Given the distributions of participants across race/ethnicity categories, we dichotomized race/ethnicity between white and non-white categories for all analyses.
In a separate analysis using cross-sectional data, the association between seeking from nonmedical channels and fruit and vegetable consumption was not statistically significant. However, Maxwell and Cole (2007) observe that some mediation processes may not be captured in cross-sectional data as they require sufficient passage of time before they unfold. This is consistent with our finding a lagged association between seeking from nonmedical channels and fruit and vegetable consumption controlling for the effects of patient-clinician information engagement.
Financial disclosures: None
References
- Allison P. Missing data Quantitative applications in the social sciences. Thousand Oaks: Sage Publications; 2001. [Google Scholar]
- Afifi W, Weiner J. Toward a theory of motivated information management. Communication Theory. 2004;14:167–190. [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- American Cancer Society. American Cancer Society guidelines on nutrition and physical activity for cancer prevention. 2011 Retrieved on June 2, 2011 http://www.cancer.org/acs/groups/cid/documents/webcontent/002577-pdf.pdf. [PubMed]
- Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Karanja N, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH collaborative research group. The New England Journal of Medicine. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- Ball-Rokeach AJ, Wilkin HA. Ethnic differences in health information-seeking behavior: Methodological and applies issues. Communication Research Reports. 2009;26(1):22–29. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bass SB, Ruzek SB, GorFkadon TF, Fleisher L, McKeown-Conn N, Moore D. Relationship of internet health information use with patient behavior and self-efficacy: Experiences of newly diagnosed cancer patients who contact the National Cancer Institute’s Cancer Information Service. Journal of Health Communication. 2006;11:219–236. doi: 10.1080/10810730500526794. [DOI] [PubMed] [Google Scholar]
- Bazzano LA. Dietary intake of fruit and vegetable and risk of diabetes mellitus and cardiovascular diseases 2005 [Google Scholar]
- Blanchard CM, Courneya KS, Stein K. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: Results from the American cancer society’s SCS-II. Journal of Clinical Oncology. 2008;26(13):2198–2204. doi: 10.1200/JCO.2007.14.6217. [DOI] [PubMed] [Google Scholar]
- Block G, Patterson B, Subar A. Fruit, vegetables, and cancer prevention: A review of the epidemiological evidence. Nutrition and Cancer. 1992;18(1):1–29. doi: 10.1080/01635589209514201. [DOI] [PubMed] [Google Scholar]
- Boffetta P, Couto E, Wichmann J, Ferrari P, Trichopoulos D, Bueno-de-Mesquita HB, Trichopoulou A, et al. Fruit and vegetable intake and overall cancer risk in the European prospective investigation into cancer and nutrition (EPIC) Journal of the National Cancer Institute. 2010;102(8):529–537. doi: 10.1093/jnci/djq072. [DOI] [PubMed] [Google Scholar]
- Boreham P, Gibson D. The informative process in private medical consultations: A preliminary investigation. Social Science & Medicine. 1978;12(5A):409–416. [PubMed] [Google Scholar]
- Brashers DE, Goldsmith DJ, Hsieh E. Information seeking and avoiding in health contexts. Human Communication Research. 2002;28:258–271. [Google Scholar]
- Brown JK, Byers T, Doyle C, Courneya KS, Demark-Wahnefried W, Kushi LH, Sawyer KA, et al. Nutrition and physical activity during and after cancer treatment: An American cancer society guide for informed choices. CA: A Cancer Journal for Clinicians. 2003;53(5):268–291. doi: 10.3322/canjclin.53.5.268. [DOI] [PubMed] [Google Scholar]
- Caiata-Zufferey M, Abraham A, Sommerhalder K, Schulz PJ. Online health information seeking in the context of the medical consultation in Switzerland. Qualitative Health Research. 2010;20(8):1050–1061. doi: 10.1177/1049732310368404. [DOI] [PubMed] [Google Scholar]
- Case DO, Andrews JE, Johnson JD, Allard SL. Avoiding versus seeking: The relationship of information seeking to avoidance, blunting, coping, dissonance, and related concepts. J Med Libr Assoc. 2005;93(3):353–362. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Morbidity and mortality weekly report state-specific trends in fruit and vegetable consumption among adults — united states, 2000–2009. 2011 [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: A meta-analysis of cohort studies. The Journal of Nutrition. 2006;136(10):2588–2593. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- Dillman D. Mail and internet surveys: The tailored design method. 2. New York: Wiley; 2000. [Google Scholar]
- Dutta-Bergman M. Media use theory and Internet use for health care. In: Rice R, Muriero M, editors. The Internet and health care: Theory, research and practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2006. pp. 88–103. [Google Scholar]
- Epstein RM, Street RL., Jr . Patient-centered communication in cancer care: Promoting healing and reducing suffering NIH Publication No 07-6225. Bethesda, MD: 2007. [Google Scholar]
- Freimuth VS, Stein JA, Kean TJ. Searching for health information: The Cancer Information Service model. Philadelphia: University of Pennsylvania Press; 1989. [Google Scholar]
- Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. Am J Prev Med. 1999;17(4):285–94. doi: 10.1016/s0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- Gandini S, Merzenich H, Robertson C, Boyle P. Meta-analysis of studies on breast cancer risk and diet: The role of fruit and vegetable consumption and the intake of associated micronutrients. European Journal of Cancer. 2000;36(5):636–646. doi: 10.1016/S0959-8049(00)00022-8. [DOI] [PubMed] [Google Scholar]
- Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, Morrow M. AJCC cancer staging manual. 6. New York, NY: Springer; 2002. [Google Scholar]
- Griffin R, Dunwoody S, Neuwirth K. Proposed model of the relationship of risk information seeking and processing to the development of preventive behaviors. Environmental Research. 1999;80:230–245. doi: 10.1006/enrs.1998.3940. [DOI] [PubMed] [Google Scholar]
- He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: Meta-analysis of cohort studies. The Lancet. 2006;367(9507):320–326. doi: 10.1016/S0140-6736(06)68069-0. [DOI] [PubMed] [Google Scholar]
- Hewitt M, Rowland JH, Yancik R. Cancer survivors in the united states: Age, health, and disability. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2003;58(1):82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- Hornik R, Parvanta S, Mello SL, Freres D, Schwartz JS. Effects of scanning—routine health information exposure—on cancer prevention and screening behaviors in the general population. Journal of Health Communication. doi: 10.1080/10810730.2013.798381. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornik R, Yanovitzky I. Using theory to design evaluations of communication campaigns: The case of the national youth anti-drug media campaign. Communication Theory. 2003;13(2):204–224. doi: 10.1111/j.1468-2885.2003.tb00289.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt JR, Kristal AR, White E, Lynch JC, Fries E. Physician recommendations for dietary change: Their prevalence and impact in a population-based sample. American Journal of Public Health. 1995;85(5):722–726. doi: 10.2105/ajph.85.5.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang Y. Social diffusion of campaign effects: Campaign-generated interpersonal communication as a mediator of antitobacco campaign effects. Communication Research. 2010 doi: 10.1177/0093650210389029. [DOI] [Google Scholar]
- Johnson JD, Meischke H. A comprehensive model of cancerrelated information seeking applied to magazines. Human Communication Research. 1993;19:343–367. [Google Scholar]
- Kahlor L. PRISM: A planned risk information seeking model. Health Communication. 2010;25:345–356. doi: 10.1080/10410231003775172. [DOI] [PubMed] [Google Scholar]
- Katz E, Lazarsfeld P. Personal Influence. Vol. 1955 New York: Free Press; [Google Scholar]
- Key TJ. Fruit and vegetables and cancer risk. British Journal of Cancer. 2011;104(1):6–11. doi: 10.1038/sj.bjc.6606032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SD, Loiselle CG. Health information-seeking behavior. Qualitative Health Research. 2007;17(8):1006–1019. doi: 10.1177/1049732307305199. [DOI] [PubMed] [Google Scholar]
- Lee C. The interplay between media use and interpersonal communication in the context of healthy lifestyle behaviors: Reinforcing or substituting? Mass Communication and Society. 2010;13(1):48. doi: 10.1080/15205430802694869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis N, Gray SW, Freres DR, Hornik RC. Examining cross-source engagement with cancer-related information and its impact on doctor-patient relations. Health Communication. 2009;24(8):723–734. doi: 10.1080/10410230903264030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis N, Martinez L, Freres D, Schwartz JS, Armstrong K, Gray SW, Fraze T, Nagler R, Bourgoin A, Hornik R. Information seeking from media and Family/Friends increases fruit and vegetable consumption among cancer patients. Health Communication. 2012;27(2):380–388. doi: 10.1080/10410236.2011.586990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loureiro ML, Nayga RM. Physician’s advice affects adoption of desirable dietary behaviors. Applied Economic Perspectives and Policy. 2007;29(2):318–330. doi: 10.1111/j.1467-9353.2007.00345.x. [DOI] [Google Scholar]
- Mackinnon DP, Fairchild AJ. Current directions in mediation analysis. Current Directions in Psychological Science : A Journal of the American Psychological Society. 2009;18(1):16. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez LS, Schwartz JS, Freres D, Fraze T, Hornik RC. Patient-clinician information engagement increases treatment decision satisfaction among cancer patients through feeling of being informed. Patient Education and Counseling. 2009;77(3):384–390. doi: 10.1016/j.pec.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer DK, Terrin NC, Menon U, Kreps GL, McCance K, Parsons SK, Mooney KH. Health behaviors in cancer survivors. Oncology Nursing Forum. 2007;34(3):643–651. doi: 10.1188/07.ONF.643-651. [DOI] [PubMed] [Google Scholar]
- Nagler RH, Gray SW, Romantan A, Kelly BJ, DeMichele A, Armstrong K, Hornik RC, et al. Differences in information seeking among breast, prostate, and colorectal cancer patients: Results from a population-based survey. Patient Education and Counseling. 2010;81(Suppl):S54–62. doi: 10.1016/j.pec.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, Romantan A, Kelly BJ, Stevens RS, Gray SW, Hull SJ, Hornik RC, et al. How do cancer patients navigate the public information environment? Understanding patterns and motivations for movement among information sources. Journal of Cancer Education : The Official Journal of the American Association for Cancer Education. 2010;25(3):360–370. doi: 10.1007/s13187-010-0054-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New SA, Robins SP, Campbell MK, Martin JC, Garton MJ, Bolton-Smith C, Reid DM, et al. Dietary influences on bone mass and bone metabolism: Further evidence of a positive link between fruit and vegetable consumption and bone health?1. The American Journal of Clinical Nutrition. 2000;71(1):142–151. doi: 10.1093/ajcn/71.1.142. [DOI] [PubMed] [Google Scholar]
- Niederdeppe J, Frosch DL, Hornik RC. Cancer news coverage and information seeking. Journal of Health Communication. 2008;13(2):181–199. doi: 10.1080/10810730701854110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perloff RM, Bonder B, Ray GB, Ray EB, Siminoff LA. Doctor-patient communication, cultural competence, and minority health. American Behavioral Scientist. 2006;49(6):835–852. [Google Scholar]
- Pignone MP, Ammerman A, Fernandez L, Orleans CT, Pender N, Woolf S, Sutton S, et al. Counseling to promote a healthy diet in adults: A summary of the evidence for the U.S. preventive services task force. American Journal of Preventive Medicine. 2003;24(1):75–92. doi: 10.1016/s0749-3797(02)00580-9. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Ramanadhan S, Viswanath K. Health and the information nonseeker: A profile. Health Communication. 2006;20(2):131–139. doi: 10.1207/s15327027hc2002_4. [DOI] [PubMed] [Google Scholar]
- Ramirez AS, Freres D, Martinez LS, Lewis N, Bourgoin A, Kelly B, Lee C, Nagler R, Schwartz JS, Hornik RC. Information Seeking from Media and Family/Friends Increases Likelihood of Engaging in Healthy Lifestyle Behaviors. Journal of Health Communication. doi: 10.1080/10810730.2012.743632. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 5. New York, NY: Free Press; 2003. [Google Scholar]
- Roter DL. Patient question asking in physician-patient interaction. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association. 1984;3(5):395–409. [PubMed] [Google Scholar]
- Sacerdote C, Fiorini L, Rosato R, Audenino M, Valpreda M, Vineis P. Randomized controlled trial: Effect of nutritional counseling in general practice. International Journal of Epidemiology. 2006;35(2):409–415. doi: 10.1093/ije/dyi170. [DOI] [PubMed] [Google Scholar]
- Sacks H, Schegloff EA, Jefferson G. A simplest systematics for the organization of turn-taking for conversation. Language. 1974;50(4, Part 1):696–735. [Google Scholar]
- Shah DV, Cho J, Eveland WP, Kwak N. Information and expression in a digital age. Communication Research. 2005;32(5):531–565. doi: 10.1177/0093650205279209. [DOI] [Google Scholar]
- Shah DV, Cho J, Nah S, Gotlieb MR, Hwang H, Lee N, McLeod DM, et al. Campaign ads, online messaging, and participation: Extending the communication mediation model. Journal of Communication. 2007;57(4):676–703. doi: 10.1111/j.1460-2466.2007.00363.x. [DOI] [Google Scholar]
- Shim M, Kelly B, Hornik R. Cancer information scanning and seeking behavior is associated with knowledge, lifestyle choices, and screening. Journal of Health Communication. 2006;11(Suppl 1):157–172. doi: 10.1080/10810730600637475. [DOI] [PubMed] [Google Scholar]
- Steinmetz KA, Potter JD. Vegetables, fruit, and cancer prevention: A review. Journal of the American Dietetic Association. 1996;96(10):1027–1039. doi: 10.1016/S0002-8223(96)00273-8. [DOI] [PubMed] [Google Scholar]
- Street RL., Jr Information-giving in medical consultations: The influence of patients’ communicative styles and personal characteristics. Social Science & Medicine (1982) 1991;32(5):541–548. doi: 10.1016/0277-9536(91)90288-n. [DOI] [PubMed] [Google Scholar]
- Tan ASL, Bourgoin A, Gray SW, Armstrong K, Hornik RC. How does patient-clinician information engagement influence self-reported cancer-related problems? Cancer. 2011;117(11):2569–2576. doi: 10.1002/cncr.25804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan AS, Mello S, Hornik RC. A longitudinal study on engagement with dieting information as a predictor of dieting behavior among adults diagnosed with cancer. Patient Education & Counseling. 2012;88:305–310. doi: 10.1016/j.pec.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tohill BC. Dietary intake of fruit and vegetables and management of body weight 2005 [Google Scholar]
- Vainio H, Bianchini F. Fruit and vegetables IARC handbooks of cancer prevention. Lyon, France: IARC Press; 2003. p. 376. [Google Scholar]
- Viswanath K. The communications revolution and cancer control. Nature Reviews Cancer. 2005;5(10):835. doi: 10.1038/nrc1718. [DOI] [PubMed] [Google Scholar]
- Viswanath K, Ramanadhan S, Kontos EZ. Mass media. In: Galea S, editor. Macrosocial determinants of population health. New York: Springer; 2007. pp. 275–294. [Google Scholar]
- Viswanath K, Ackerson LK. Race, ethnicity, language, social class, and health communication inequalities: a nationally-representative cross-sectional study. PLoS One. 2011;6(1):e14550. doi: 10.1371/journal.pone.0014550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willems S, de Maesschalck S, Deveugele M, Derese A, de Maeseneer J. Socioeconomic status of the patient and doctor-patient communication: Does it make a difference? Patient Education and Counseling. 2005;26:139–146. doi: 10.1016/j.pec.2004.02.011. [DOI] [PubMed] [Google Scholar]
- Willett WC. Diet and cancer: One view at the start of the millennium. Cancer Epidemiology Biomarkers & Prevention. 2001;10(1):3–8. largely responsible for the common cancers in Western countries Dietary fat has been hypothesized to be the key factor because national consumption is correlated with the international differences, but these correlations are potentially conf(TRUNCATED) [PubMed] [Google Scholar]
- Willett WC. Fruits, vegetables, and cancer prevention: Turmoil in the produce section. Journal of the National Cancer Institute. 2010;102(8):510–511. doi: 10.1093/jnci/djq098. [DOI] [PubMed] [Google Scholar]
- Witte K. Theory based interventions and evaluations of outreach efforts. Seattle, WA: National Network of Libraries of Medicine/Pacific Northwest Region; 1998. (commissioned publication). Retrieved from http://www.nnlm.nlm.nih.gov/pnr/eval/witte.html. [Google Scholar]
- World Cancer Research Fund / American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Washington DC: 2007. [Google Scholar]
- Wright KB, Frey LR. Communication and care in an acute cancer center: The effects of patients’ willingness to communicate about health, health-care environment perceptions, and health status on information seeking, participation in care practices, and satisfaction. Health Communication. 2008;23:369–379. doi: 10.1080/10410230802229886. [DOI] [PubMed] [Google Scholar]
- Yancik R, Wesley MN, Ries LAG, Havlik RJ, Long S, Edwards BK, Yates JW. Comorbidity and age as predictors of risk for early mortality of male and female colon carcinoma patients. Cancer. 1998;82(11):2123–2134. doi: 10.1002/(SICI)1097-0142(19980601)82:11<2123∷AID-CNCR6>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Yang ZJ, McComas KA, Gay G, Leonard JP, Dannenberg AJ, Dillon H. Information seeking related to clinical trial enrollment. Communication Research. 2011;38(6):856–882. [Google Scholar]
- Yusuf SW, Razeghi P, Yeh ET. The diagnosis and management of cardiovascular disease in cancer patients. Current Problems in Cardiology. 2008;33(4):163–196. doi: 10.1016/j.cpcardiol.2008.01.002. [DOI] [PubMed] [Google Scholar]


