Abstract
Purpose
To investigate the relationship between optical biometry and applanation ultrasound measurement of the axial length of the eye.
Materials and methods
This prospective study enrolled 55 (68 eyes) consecutive patients scheduled for cataract surgery at Dhahran Eye Specialist Hospital (DESH). Every eye underwent two measurements each with an optical biometer and with applanation ultrasound. Only patients with cataract and no other ophthalmic pathology or disease were enrolled. Comparison, correlation and repeatability of axial length with both devices were analyzed. Agreement between devices was evaluated. A regression formula to convert measurements between devices was investigated. A p value less than 0.05 was statistically significant.
Results
There was strong repeatability (99.4%) and agreement (r = 0.987) between both devices (p < 0.001); the difference between devices was mainly in short eyes (p = 0.031).
Conclusion
Optical biometry and applanation ultrasound measurements of axial length correlate well. However, optical biometry is preferable in short eyes.
Keywords: Optical, Axial length, Ultrasound, A-scan, IOLMaster
Introduction
Axial length (AL) measurement utilizes the principle of signal reflection to measure the difference between the various ocular structures and the overall length of the eye. The time a signal is reflected back from an interface is measured and divided by two and multiplied by speed of signal in the corresponding medium.1 Distance is calculated using the formula:
| (1) |
The transmitting signal can be ultrasonic. Ultrasound measurements (ultrasonography) can be performed by applanation of an ultrasound probe to the cornea or by immersion of the probe in a saline filled shell. Ideal measurements consist of three readings within 0.02 mm of each other, maximally high, with steeply rising anterior and posterior lens and retina spikes.1
Over a decade ago, the IOLMaster (Zeiss GmbH, Jena, Germany) optical biometer was introduced into clinical practice. Over time optical biometry has replaced ultrasonography as the standard technique for axial length measurements of the eye. Optical biometry utilizes a laser for the signal transmission. Interference phenomenon between the reflected signal and reference signal is utilized to determine distances between interfaces. Ideal measurements (for the IOLMaster) require a signal-to-noise ratio greater than 2.0, a tall narrow primary maxima with a thin well centered termination and a set of secondary maxima, and a minimum of 4 measurements within 0.02 mm.2,3
Previous comparisons of applanation ultrasound and optical biometry have reported equal or better results with optical biometry.4,5 A recent study concluded that applanation and ultrasound biometry can be used interchangeably for intraocular lens (IOL) implant calculations. However the difference in measurement principles, measurement of differing ocular structures (e.g. corneal apex to ILM for ultrasound) and other factors indicate that a conversion factor may be required for measurement from optical biometry and applanation ultrasound biometry. Applanation ultrasound remains a common method to measure axial length worldwide, especially in developing countries due to familiarity with the technique and cost. This study measures the repeatability of axial length measurements and investigates the mathematical correlation between the optical and applanation ultrasound axial length measurements for a conversion factor between the two modalities.
Patients and methods
Patients, inclusion and exclusion criteria
Patients scheduled for cataract surgery at Dhahran Eye Specialist Hospital (DESH) (DESH), Saudi Arabia were prospectively enrolled. To be included in the study, patients had to have a visually significant cataract in one or both eyes. Patients were excluded if they had a history of trauma or had undergone any previous ocular surgery, or had an ophthalmic condition (other than cataract) that could affect vision or axial length measurements such as, retinal detachment, retinitis pigmentosa or glaucoma. This study was approved by the Institutional Review Board at DESH and adhered to the tenets of the World Medical Association’s Declaration of Helsinki.
Axial length measurements
Axial length measurements were performed with the IOLMaster v.4 optical biometer and the A-scan 1000 (Ophthalmic Technologies International, Toronto, Canada) ultrasound unit. All measurements were performed by an experienced diagnostic ultrasonographer (FN) familiar with both devices. Optical biometry was always performed first followed by ultrasound measurements to avoid the confounding effect of a potential corneal abrasion. Two measurements with each modality were performed and the mean was calculated.
Optical biometry was performed with the patient seated at the IOLMaster and asked to fixate on the fixation target. Applanation ultrasound was performed after instillation of one drop of topical anesthetic (Alcaine 0.5%) on the lower conjunctiva. The A-scan unit was equipped with a 10 MHz transducer probe, electronic calipers (gates) were used and velocities were set by device per medium e.g. 1640 m/s for cornea and lens, 1530 for aqueous and vitreous for axial length measurements. All measurements for both devices were performed based on the manufacturer’s recommendations.
Statistical analysis
Comparison, correlation and repeatability of axial length of the eye with optical biometer and applanation ultrasound were analyzed. Lens thickness, anterior chamber depth and the length of the vitreous cavity of entire study population were reported. Mean ± standard deviation is reported here. Consecutive patients were enrolled for this study. Partial Pearson correlation coefficient was calculated to determine the axial length measurements between devices with age and gender as covariates. Cronbach’s alpha and interclass correlation coefficient were calculated for the axial length. Regression analysis was performed to model the mathematical relationship (conversion factor) for axial length between optical biometry and applanation ultrasound. Confounders of age and gender were included into regression. Bland–Altman plots were used to evaluate the agreement in axial length between devices with 95% confidence intervals (95% CI). Eyes were grouped according to axial length; short (<22 mm); normal (22 to <24.50 mm); and long (>24.50 mm) to determine the accuracy of the results for each group. Stratification was performed to control for axial length. Multivariate analysis of covariance (MANCOVA) with post hoc comparisons were used to compare optical and ultrasound AL measurements in the entire study sample and for each subgroup. The confounding effects of age and gender were removed by considering these factors as covariates. A p value less than 0.05 was statistically significant. Statistical analysis was performed with SPSS v.20 (IBM Corp., New York, NY, USA).
Results
The study sample was comprised of 55 (68 eyes) consecutive patients (32 males and 23 females) with a mean age of 59.04 ± 16.26 years (range, 9–84 years). Both eyes of 13 patients were included in this study. For the entire study sample, the mean keratometry was 43.89 ± 1.67 D, the mean anterior chamber depth was 2.93 ± 0.40 mm, the mean lens thickness was 4.66 ± 0.68 mm and the mean length of the vitreous cavity was 16.27 ± 1.90 mm. The repeatability between devices in this sample was 99.4% with (p < 0.0001; 95% CI: 99.0–99.6%). The mean AL was 23.86 ± 1.85 mm (range, 19.01–29.27 mm) with applanation ultrasound and 23.76 ± 1.87 mm (range, 19.29 mm to 29.88 mm) with optical biometry. The Bland–Altman plot indicates that 94.12% of all differences were within two standard deviations from mean difference (−0.089 ± 0.594 mm i.e. between −0.683 mm and 0.505 mm) (Fig. 1). The use of different biometry methods (e.g. optical versus ultrasound) caused 6.9% of variation in the measurements. The measurement error between devices was 0.21 mm and error width was ±0.41 mm. There was a good correlation between devices that was statistically significant (r = 0.987, p < 0.0001) (Fig. 2) and there were no significant effects due to age or gender. Cronbach’s alpha and the interclass correlation coefficient were 0.994 with (p < 0.0001; 95% CI: 99.0–99.6%). Regression analysis provided the following equation for the range of AL in this study (i.e. 19–29 mm):
| (2) |
where ALop represents axial length from optical biometry and ALus represents axial length from applanation ultrasound (p < 0.0001, F = 2548.418, df (1,66)). Both covariates (age and gender) were not statistically significant (p = 0.895, and p = 0.781 respectively). Based on equation 2, the factor for applanation ultrasound was 0.996 adjusted for heteroscedasticity (p < 0.0001; 95% CI: 1.05–0.94). Pillai’s trace from multivariate analysis of covariates (MANCOVA) and controlling for confounding effects of age and gender indicated a statistically significant difference (p = 0.010; F = 7.082; d.f. (1,63)). Mean difference in AL between optical biometry and applanation ultrasound adjusted for age and gender was statistically significant (p = 0.010) (Table 1). Upon stratification, there were 9 eyes in the short eye group, 41 eyes in the normal group, and 18 long eyes. In comparing devices for each AL group, the overall statistically significant difference was attributed to short eyes (p = 0.033; MANCOVA: Pillai’s trace; F = 4.7763; d.f. (1,63)) and not the normal, and long eyes (p = 0.134, and 0.438 respectively) (Fig. 3).
Figure 1.
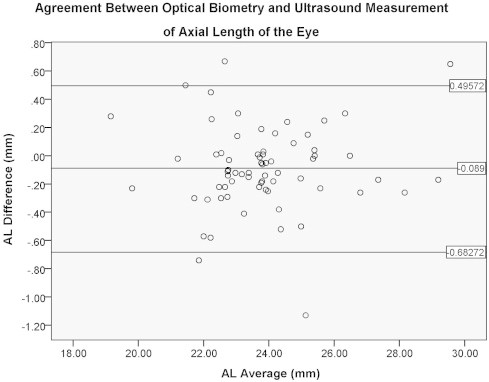
Bland–Altman plot of the agreement in axial length measurements (AL) with applanation ultrasound versus optical biometry.
Figure 2.
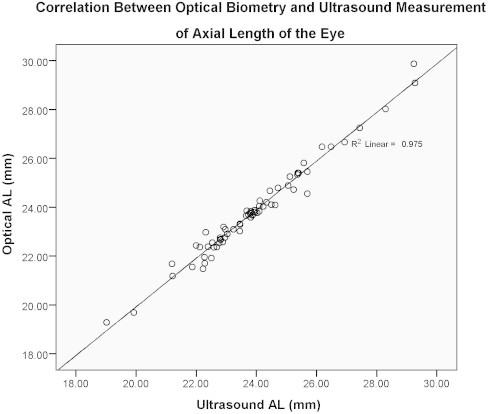
Correlation of axial length measurements with applanation ultrasound versus optical biometry.
Table 1.
Axial length measurements with optical biometry and applanation ultrasound adjusted for age and gender.
| Mean | Standard deviation | P value | 95% Confidence Interval |
||
|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||
| Optical axial length | 23.548 | 1.20 | |||
| Ultrasound axial length | 23.665 | 1.23 | |||
| Difference | −0.117 | 0.36 | 0.010 | −0.205 | −0.029 |
Values were evaluated at age = 59.87, sex = 0.53. p < 0.05 is statistically significant.
Figure 3.
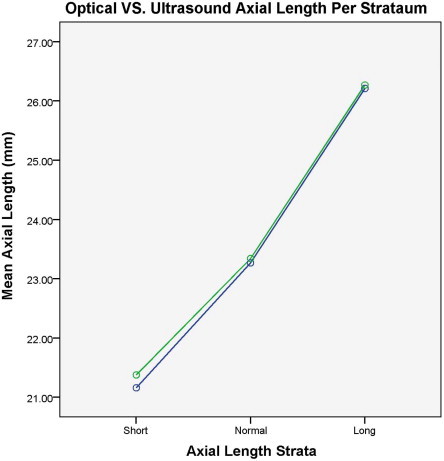
Comparison of axial length measurements with applanation ultrasound versus optical biometry stratified according to length. Green line: Optical length. Blue line: ultrasound length.
Discussion
To our knowledge this is the first publication to present a conversion factor for optical biometer and applanation ultrasound measurements. The advantage of the applanation method is the faster measurements in the hands of a skilled operator. However, the disadvantage is the potential for corneal compression that may result in shorter axial length measurements. The disadvantage of the first optical biometer (e.g. IOLMaster) in common clinical use, was the inaccurate measurement in cases of media opacities such as corneal scar and vitreous hemorrhage.6 Newer versions of the IOLMaster and other optical biometers (e.g. Al-Scan; NIDEK Co. Ltd., Gamagori, Japan and, Lenstar; Haag-Streit Group, Koeniz, Switzerland) may be more robust.
The differences between ultrasound biometry and optical biometry have clinical implications. Firstly, resolution improves as wavelength decreases. Hence, as light has a very short wavelength compared to sound, the laser light has better resolution. Therefore, the accuracy of AL with ultrasound AL is approximately 0.10–0.12 mm compared to 0.012 mm for optical AL.7 Measurement accuracy is limited by variation in retinal thickness surrounding the fovea.8 The second difference is the starting point of measurement between the two modalities. For example, ultrasound measures AL from the anterior surface of the corneal apex to the internal limiting membrane (ILM) of the fovea, whereas optical biometry measures AL from the second principal plane of the cornea (0.05 mm deeper than the corneal apex) to photoreceptor layer (0.25 mm deeper than ILM) of the fovea.1 Theoretically, optical biometry reads longer than ultrasonic axial length. Hence:
| (3) |
Lastly, ultrasound measurements are performed on the anatomic axis i.e. through the center of the cornea measuring anatomic axis as axial length whereas optical biometry measurements are performed on the visual axis measuring visual axis as axial length.2 As visual axis is shorter than anatomic axis; hence, optical measurements read shorter axial length compared to ultrasound measurements.7
This comparison of axial length measurements with optical biometry and applanation ultrasound did correlate well for clinical purposes. The Bland–Altman plots showed good agreement between devices with less than 6% of eyes that were outliers (Fig. 1). There was a mean difference of −0.117 mm in axial length measurements between devices after controlling for age and gender. Although this difference was statistically significant, it was not clinically significant. For example a difference of −0.117 mm translates to 0.29 D which is clinically insignificant. Additionally, statistically significant differences were only present when comparing measurements between devices for short eyes (p = 0.033; MANOVA: Pillai’s trace) but not normal to long eyes. Hence, the difference was rewritten in an equation format to relate axial length from applanation ultrasound to optical biometry.
| (4) |
where ALop represents axial length from optical biometry and ALus represents axial length from applanation ultrasound. The difference between methods might be attributed to the need for meticulous alignment in short eyes because the posterior pole anatomy is so small that the slightest misalignment can result in misdirection of an ultrasound signal from the fovea.
There was excellent repeatability of measurement with both devices. The statistically significant Pearson’s correlation coefficient of 0.987 and Fig. 2 indicates excellent correlation of axial length measurements between devices (p < 0.0001). However, the correlation proved that a pair of measurements increased or decreased together but did not indicate if a pair of measurements was identical. Cronbach’s Alpha and Interclass correlation coefficient of 0.994 indicated 99.4% agreement (identical) between pairs of measurements. Hence, given these outcomes, the regression Eq. (4) should be able to predict axial length with optical biometry in 97.4% (adjusted R2) of future cases.
The outcomes of the current study are similar to previous publications. For example, the lack of a statistical difference in long eyes between devices in the current study is similar to a recent study that showed that optical and applanation ultrasound biometry (random measurement of IOLMaster or Lenstar) was comparable for long eyes.4
There were some limitations to this study. Although the small sample size may seem small, a statistically significant difference was seen due to the use of same devices and operator plus precision (small standard deviation). We used the common optical biometer (IOLMaster) on the market for the current study. However, the outcomes of the current study may not be applicable to other biometers without further study. Previous comparisons of the IOLMaster and Lenstar optical biometer have indicated slightly different measurements of axial length in cataractous and clear lenses.10 A recent comparison of the IOLMaster to the AL-Scan indicates almost perfect correlation in axial length measurements between devices.11 A recent study also reported statistical differences (−0.1 ± 0.76 mm) in axial length between the IOLMaster and Lenstar (p < 0.001; 95% CI: 1.39 to −1.59).12 However, the study population had keratoconus.12 Due to the differences in various studies with different biometers compared to the IOLMaster, we urge caution in applying the outcomes of the current study to other types of optical biometers. Age and gender were confounding factors that were controlled in this study.
Conclusion
Based on the outcomes of this study we advise that optical biometry should be used to measure short eyes. Optical biometry to measure axial length is very precise and interchangeable with ultrasound measurement with no clinical difference. A correction factor of −0.117 should be added to applanation ultrasound for values that are clinically similar to axial length with optical biometry. This study provided a regression equation that may be used to predict axial length with optical biometry from axial length from applanation ultrasound. Although a statistically significant difference in axial length measurements exists between optical biometry and applanation ultrasound, it exists mainly in short eyes.
Acknowledgement
I would like to thank Prof. Saleh al Twaijri, Head of Research, SAAD Specialist Hospital, for his helpful comments.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Byrne S.F. Grove Park Publishers; New York: 1995. A-scan axial length measurements: a handbook for IOL calculations. [Google Scholar]
- 2.Hill W.E. The IOLMaster. Tech Ophthalmol. 2003;1:62–67. [Google Scholar]
- 3.Garg A. Optical biometry with IOLMaster (partial coherence interferometry) In: Garg A., Latkany R., Bovet J., Haigis W., editors. Mastering the techniques of IOL power calculations. JAYPEE; India: 2009. pp. 24–26. [Google Scholar]
- 4.Shen P., Zheng Y., Ding X., Liu B., Congdon N., Morgan I. Biometric measurements in highly myopic eyes. J Cataract Refract Surg. 2013;39(2 (February)):180–187. doi: 10.1016/j.jcrs.2012.08.064. [DOI] [PubMed] [Google Scholar]
- 5.Bjeloš Rončević M., Bušić M., Cima I., Kuzmanović Elabjer B., Bosnar D., Miletić D. Comparison of optical low-coherence reflectometry and applanation ultrasound biometry on intraocular lens power calculation. Graefes Arch Clin Exp Ophthalmol. 2011;249(1 (January)):69–75. doi: 10.1007/s00417-010-1509-4. [DOI] [PubMed] [Google Scholar]
- 6.Doctor K.J. JAYPEE; India: 2009. IOL calculations: when, how and which? Mastering the techniques of IOL power calculations. p. 36–45. [Google Scholar]
- 7.Holladay J.T. Ultrasound and optical biometry. Cataract Refract Surg Today Eur. 2009 [Google Scholar]
- 8.Alpins N.A., Walsh G. accurate biometry and intraocular lens power calculations. In: Agarwal A., editor. Refractive Surgery Nightmares – Conquering Refractive Surgery Catastrophes. Slack Inc; NJ: 2008. p. 581. p. 581–585.8. [Google Scholar]
- 10.Hoffer K.J., Shammas H.J., Savini G. Comparison of 2 laser instruments for measuring axial length. J Cataract Refract Surg. 2010;36(4 (April)):644–648. doi: 10.1016/j.jcrs.2009.11.007. Erratum in J Cataract Refract Surg 2010;36(6 June):1066. [DOI] [PubMed] [Google Scholar]
- 11.Kaswin G., Rousseau A., Mgarrech M., Barreau E., Labetoulle M. Biometry and IOL power calculation results with a new optical biometry device: comparison to the gold standard. J Cataract Refract Surg. 2014;40(4):593–600. doi: 10.1016/j.jcrs.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 12.Çinar Y., Cingü A.K., Sahin M., Sahin A., Yükse H., Türkcü F.M. Comparison of optical versus ultrasonic biometry in keratoconic eyes. J Ophthalmol. 2013;2013 doi: 10.1155/2013/481238. Article ID 481238, 6 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]


