Abstract
T cells modified with chimeric antigen receptor are an attractive strategy to treat Epstein-Barr virus (EBV) associated malignancies. The EBV latent membrane protein 1 (LMP1) is a 66-KD integral membrane protein encoded by EBV that consists of transmembrane-spanning loops. Previously, we have identified a functional signal chain variable fragment (scFv) that specifically recognizes LMP1 through phage library screening. Here, we constructed a LMP1 specific chimeric antigen receptor containing anti-LMP1 scFv, the CD28 signalling domain, and the CD3ζ chain (HELA/CAR). We tested its functional ability to target LMP1 positive nasopharyngeal carcinoma cells. HELA/CAR cells were efficiently generated using lentivirus vector encoding the LMP1-specific chimeric antigen receptor to infect activated human CD3+ T cells. The HELA/CAR T cells displayed LMP1 specific cytolytic action and produced IFN-γ and IL-2 in response to nasopharyngeal carcinoma cells overexpressing LMP1. To demonstrate in vivo anti-tumor activity, we tested the HELA/CAR T cells in a xenograft model using an LMP1 overexpressing tumor. Intratumoral injection of anti-LMP1 HELA/CAR-T cells significantly reduced tumor growth in vivo. These results show that targeting LMP1 using HELA/CAR cells could represent an alternative therapeutic approach for patients with EBV-positive cancers.
Keywords: chimeric antigen receptor, LMP1, nasopharyngeal carcinoma, EBV, adoptive T cell therapy
INTRODUCTION
Nasopharyngeal carcinoma (NPC) is a malignant epithelial carcinoma of the head and neck region and most commonly seen in southeast Asia, especially in the southern provinces of China[1]. In contrast to other head and neck cancers, Epstein-Barr virus (EBV) infection has been associated with NPC in general and specifically with undifferentiated NPCs. Most NPC patients are first diagnosed with nodal involvement or distal metastasis. Underlying EBV infection may be one contributing factor to the highly metastatic phenotype of NPC[2].
Latent membrane protein 1 (LMP1) is a 66 KD integral membrane protein in EBV. LMP1 contains three domains: a short cytoplasmic N-terminal, a transmembrane domain with 6 transmembrane-spanning loops and a long cytoplasmic C-terminus[3],[4]. LMP1 is essential for EBV-mediated growth transformation of infected cells. The C-terminus of the protein triggers a variety of signal pathways through three functional domains termed C-terminal activating regions 1–3 (CTAR1, CTAR2 and CTAR3)[5].
In patients with EBV-associated NPC, adoptive cell therapy with EBV-specific autologous cytotoxic T lymphocytes (CTLs) can control disease progression. In these studies, the adoptively transferred CTLs showed significant antitumor activity and were safe for patients[6]-[10]. However, the efficacy of in vitro induction of EBV-specific T cell responses is low. Chimeric antigen receptor (CAR) modified T cell therapy combines the advantages of T cell based therapy and antibody based tumor specificity. In this approach, T cells are genetically modified to recognize tumor-associated antigens (TAAs). The two most common approaches are: 1) expression of TCR variable α and β chains that are derived from tumor-specific T cell clones; 2) T cell genetic modification with CARs that specifically recognize tumors through single-chain variable fragments (scFv) cloned from TAA specific antibodies. An additional advantage to using CAR expressing T cells is that they recognize tumor cells in an HLA-unrestricted manner[11]. Previously, we have identified a human Fab fragment, HELA-Fab, that specifically recognizes a polypeptide in the extramembrane domain of LMP-1[12]. In the current study, we constructed a second generation CAR, based on the HELA-Fab fragment. The second generation CAR, HELA/CAR, consists of the anti-LPM1 scFv, IgG1 CH2CH3, and a CD28/CD3 expression cassette (Lv-anti-LMP1-CH2CH3-CD28-CD3ζ). In this study we developed a novel approach using CAR modified T cells targeting the LMP-1 protein to improve EBV-targeted T cell therapy.
MATERIALS AND METHODS
Construction of the HELA/CAR recombinant lentiviral vector
The CAR HELA/CAR contains genetic elements coding the anti-LMP1 scFv, human IgG1 CH2CH3 domain (CH2CH3) and a CD28-CD3ζ expression cassette. The anti-LMP1 scFv was derived from HELA-Fab, which has the ability to bind to LMP1 extramembrane domain (EMD) (12). The DNA sequence for the anti-LMP1 scFv moiety was optimized and synthesized by Genescript. The optimized sequence contained a heavy chain variable region-(GGGS)3-a light chain variable region sequence. The fragment encoding the anti-LMP1 scFv, CH2CH3, and CD28-CD3ζ was generated by polymerase chain reaction (PCR) using the following primers: F: CGGAATTCCCATGGATTGGATTTGGAGG; R: GCTCTAGAGCATGCTTAGCGAGGGGGC and cloned into EcoRI and XbaI sites of the lentiviral vector pLVX-IRES-ZsGreen (Clontech, USA). The new vector was verified by DNA sequencing.
Lentivirus production
To produce lentivirus stocks, the HELA/CAR plasmid described above was transfected into X-293T cells (Clontech) with pMD2.G and psPAX2 using 293fectin™ Transfection Reagent (Invitrogen, Carlsbad, CA, USA). The supernatants harvested from the transfected cells containing the lentivirus particles were filtered and concentrated by ultracentrifugation (Amicon Ultra 100 kD, Millipore, USA). The supernatant lentivirus titers were determined by Lenti-X GoStix (Clontech). The supernatant was snap frozen in liquid nitrogen and stored at −80 °C.
Lentivirus transduction
Non-tissue culture treated 24 well plates (BD Biosciences, USA) were coated with 0.5 mL RetroNectin (20 μg/mL) in PBS for 2 hours at room temperature (RT). The RetroNectin solution was aspirated and the wells were blocked with 0.5 mL Hanks' balanced salt solution (HBSS) plus 2% bovine serum albumin (BSA) for 30 minutes at room temperature. The blocking solution was aspirated and the wells were washed with HBSS plus 2.5% HEPES. 0.1 mL of HELA/CAR and control lentiviral supernatants were thawed, diluted rapidly and added to each RetroNectin-coated well. The plates were centrifuged at 3800 rpm for 2 hours at 32 °C (13). The virus-containing supernatant was aspirated from wells. Blood samples were obtained from healthy donors under protocols approved by Jiangsu Province Blood Center. PBMCs were isolated by Ficoll density gradient separation. Subsequently, PBMCs were activated with anti-CD3 (OKT3) and anti-CD28 antibodies-coated plates for 3 days without IL-2. The HELA/CAR lentivirus coated wells were seeded with 1×106 activated T cells at a concentration of 0.5×106 cell/mL in T cell medium (GT-T551, Takara, Japan) plus 100 U/mL of IL-2. After the T cells were added to each well, they were centrifuged at 1000 g for 10 minutes at 32 °C. The plates were incubated at 37 °C overnight. The transduction was repeated the next day.
Expression of LMP1-CAR on CAR T cells
T cells expressing HELA/CAR were detected by flow cytometry using the ZsGreen fluorescent protein encoded by the lentivirus vector. The percentage of T cells positive for ZsGreen fluorescent protein indicated lentivirus transfection efficiency. Western blot was used to verify HELA/CAR protein expression in T cells. T cells transduced with control lentivirus or lentiviral HELA/CAR were lysed in 100 μL RIPA buffer. After centrifugation, the samples were denatured and electrophoresed by 10% SDS-PAGE. The samples were transferred to a PVDF membrane (Bio-Rad, USA) and immunoblotted with mouse anti-human CD3ζ antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA). The blot was incubated with horseradish peroxidase conjugated goat anti-mouse IgG (Jackson ImmunoResearch, USA) and detected by the ECL Western blot analysis system (Bio-Rad).
Cytotoxicity assay
A slightly modified version of a previously published flow cytometry cytotoxicity assay was used[14]. In this assay, NPC cells SUNE1 (LMP1 negative) or SUNE1-LMP1 (LMP1 positive) were labelled at 1×106 cells/mL with 5 μmol/L Cell Proliferation Dye eFluor® 670 (eBioscience, USA) in PBS. The cells were mixed and incubated at 37 °C for 30 minutes. The cells were washed and suspended in cytotoxicity medium (RMPI1640 + 3% bovine serum albumin [BSA]). HELA/CAR transduced T cells were added at the indicated effect cell:target cell ratios. Four hours after co-incubation, 50 μg/mL propidium iodide (PI; Sigma, St. Louis, MO, USA) was added to stain dead cells, and the cells were immediately analyzed by flow cytometry. Internal controls included single color eFluor® 670 stained target cells and PI and eFluor® 670 double stained targets in the absence of transduced T cells to determine the percentage of target cells undergoing spontaneous lysis. The percentages of eFluor® 670 labelled target cells that were PI+ vs. PI- were determined for each condition. Dead target cells were defined as double positive for eFluor® 670 and PI. Gated eFluor® 670 cells were analyzed for the presence of PI. The percentage of specific tumor cell lysis was calculated using the following equation: (PI+ cells/total number of eFluor® 670+ cells) ×100%, corrected for the number of spontaneously lysed targets.
Interferon-γ ELISA
SUNE1 target cells (+/− LMP1 expression) were washed and suspended at 1×106 cells/mL in T cell medium in the absence of IL-2. Totally 1×105 target cells were plated in a 96 well round bottom plate. An equivalent number of effector T cells, suspended at 1×106 cells/mL in T cell medium in the absence of IL-2, were combined with target cells. The assay was performed in triplicate. The plates were incubated at 37 °C for 24 hours. The supernatant concentration of IFN-γ was determined by ELISA according to the manufacturer's instructions (eBioscience).
Intracellular cytokine staining assay
T cells were labelled with CFSE (final concentration of 1 μM) using a standard protocol[15] and mixed with SUNE1-LMP1 and SUNE1 cells separately at a 5:1 ratio and incubated at 37 °C for 2 hours. 1 μg/mL of brefeldin A (eBioscience) was added, and cells were incubated for additional 2 hours. Subsequently, the cells were permeabilized, and intracellular staining was conducted for IFN-γ and IL-2 according to the instructions of staining of intracellular antigens for flow cytometry (eBioscience). Data acquisition was performed with a BD FACSCalibur (BD Biosciences), and analysis was performed with CFSE gate.
Mouse xenograft model
On day 0, 6-week-old male BALB/c nude mice (SLAC Laboratory) were subcutaneously injected with 5×106 SUNE1-LMP1 cells. When the tumor burden reached about 100 mm3 approximately 10 days after tumor cell inoculation, the mice were randomly assigned to three different groups (N = 5/group). The animals were percutaneously intratumorally injected with 5 × 106 T cells/100 μL on day 10, 20, 30, and 40. Group A received HELA/CAR T cells, Group B received control lentivirus transfected cells and Group C received normal saline (NS). Tumor growth was monitored by calliper measurement, and tumor volume was calculated using the formula: 1/2 × length × (width)2. This study was carried out in strict accordance with the institutional and state guidelines for the care and use of laboratory animals.
Statistical analysis
ANOVA was used to identify difference among treatment groups. Once a significant difference was confirmed, Student's t test was used to calculate the significance of difference between two treatment groups (P value). A P value less than 0.05 was considered statistically significant.
RESULTS
Construction of HELA/CAR
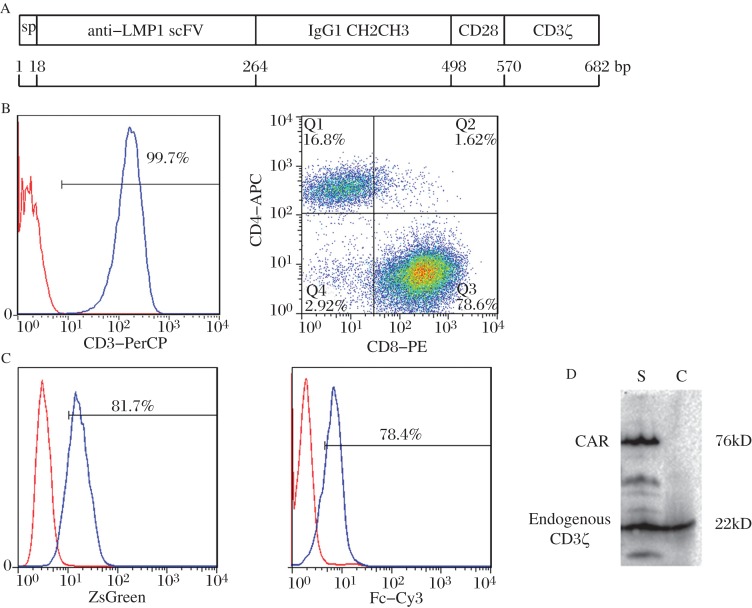
The HELA/CAR construct is shown in Figure 1A. The HELA/CAR vector encodes the anti-LMP1 scFv, IgG1 CH2CH3, a transmembrane domain of CD28 (amino acids 93-136), the cytoplasmic component of CD3ζ chain (amino acids 52-163), and a lentiviral backbone. The anti-LMP1 scFv CD3+ T cells were transduced using lentiviral HELA/CAR at 5×106 U/mL. Five to 7 days after the stimulation, the cultures were almost 100% CD3+ T cells (Fig. 1B; left panel). The CD3+ T cells were 72–79% CD8+ T cells and 14–17% CD4+ T cells (Figure 1B; right panel). Infection with lentivirus at a multiplicity of infection of 30–40 was performed on day 3 in the presence of 100 U/mL recombinant human IL-2. The transduction efficiency was measured by flow cytometric analysis of the ZsGreen positive population. As show in Fig. 1C (left panel), the transduction efficiency was 68–85%. Surface expression of HELA/CAR was confirmed using anti-human Fc-Cy3. The percentage of FC-Cy3+T cells was 72–84% (Fig. 1C; right panel), which is similar to the percentage of ZsGreen positive cells. HELA/CAR protein expression was further verified by Western blotting assays. The HELA/CAR lentiviral transduced T cells had an 80 kD band, consistent with the calculated size of HELA/CAR protein (Fig. 1D).
Fig. 1. Expression of HELA/CAR on human T cells.
A: Schematic representation of the HELA/CAR construct. It consists of anti-LMP1 scFv, human IgG1 CH2CH3 region, CD28 transmembrane (TM), and human CD3ζ moieties. The IgG signal peptide was used upstream of HELA/CAR. B: Phenotype of stimulated T cells. Left panel: anti-human CD3-PerCP staining (blue curve) and the isotype control antibody (red curve); Right panel: anti-human CD4-APC and anti-human CD8-PE staining. C: FACS analysis of HELA/CAR transfection efficiency and surface expression of HELA/CAR on human T cells. Left panel: FACS detection of ZsGreen, Right panel: anti-human Fc-Cy3 staining. In both panels CAR T cells are shown in blue and non-transfected T cells in red. D: Immunoblot analysis of HELA/CAR expression. Lysates from HELA/CAR lentivirus transfected T cells (lane s) and control lentivirus transfected T cells (lane c) were separated by SDS-PAGE under reducing conditions. A mouse anti-human CD3ζ antibody was used to detect endogenous and chimeric CD3ζ.
Cytotoxicity of HELA/CAR T cells against LMP1 expressing NPC cells in vitro
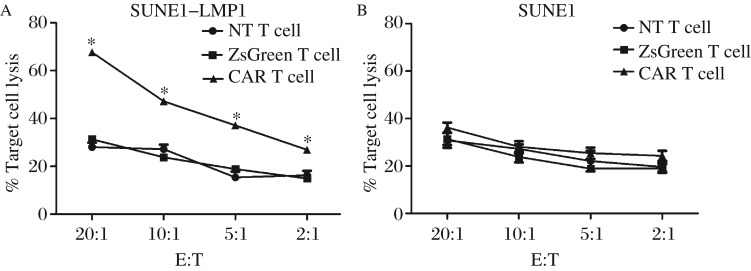
To assess the functionality of the HELA/CAR T cells, we investigated whether they could recognize and kill LMP1 expressing NPC cells. LMP1 positive and negative SUNE1 cells were labelled with eFlour670 and used as target cells to determine the cytotoxic potential of transfected T cells. Neither ZsGreen T cells nor non-transfected T cells effectively killed the LMP1 positive target cells (Fig. 2A). In contrast, the HELA/CAR T cells killed a significantly higher percentage of target cells at each effect:target ratio (P < 0.05). (Fig. 2A). None of the T cells killed the LMP1 negative SUNE cells (Fig. 2B). Thus, the HELA/CAR T cells display specific and efficient targeting of LMP1 positive NPC cells.
Fig. 2. Cytotoxic activity of HELA/CAR, ZsGreen and NT T cells co-cultured with SUNE1-LMP1 and SUNE1 cells.
On day 10, transduced cells were transferred into IL-2 free medium for 24 hours, the HELA/CAR T cells were incubated with SUNE1-LMP1 or SUNE1 cells at the indicated E:T ratio for 4 hours, and killing of target cells was quantified using a FACS-based cytotoxicity assay. Mean values ±SEM calculated from three independent experiments are shown. A: SUNE1 that expressed LMP1 (SUNE-LMP1) cells were used as target cells for the CTL assay. Effector cells were added at the ratio indicated on the x-axis. The differences between the HELA/CAR T cell and control groups are significant at each E:T ratio (ANOVA). B: LMP1-negative SUNE1 cells were used as target cells for the CTL assay. Effector cells were added at the indicated ratios. None of the T cells showed specific cytotoxicity. * indicates P < 0.05.
HELA/CAR T cells produced IL-2 and IFN-γ in a LMP1 specific manner
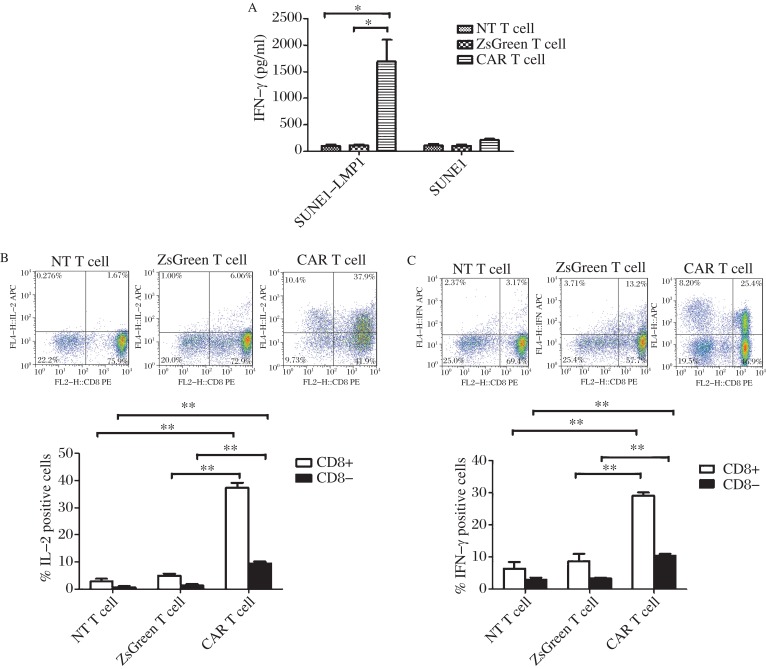
We investigated the functional cytokine response of HELA/CAR T cells to LMP1+ SUNE cells. The transfected T cells and target cells were co-cultured for 24 hours at a 1:1 ratio. IFN-γ levels were detected in the supernatants by ELISA. HELA/CAR T cells, but not ZsGreen T cells and non-transfected T cells were activated and secreted IFN-γ when co-cultured with LMP1 expressing NPC cells (Fig. 3A). Co-culture with LMP1 negative SUNE cells did not induce IFN-γ release (Fig. 3A).
Fig. 3. HELA/CAR T cells produced IFN-γ and IL-2 upon stimulation with SUNE1-LMP1 cells.
A: HELA/CAR T cells released significant amounts of IFN-γ when co-cultured with SUNE1-LMP1 cells. Results are expressed as mean ± SEM and reflect data from three biological replicates. The y axis indicates the concentration of IFN-γ. *There was a significant difference between the HELA/CAR T cell and control groups when co-cultured with SUNE-LMP1 cells (P < 0.001). B and C: HELA/CAR, ZsGreen, and NT T cells were stimulated with SUNE1-LMP1 cells for 4 hours. Intracellular cytokine staining for IL-2 (B) and IFN-γ (C) were performed (n = 3). Only HELA/CAR T cells produced IL-2 and IFN-γ in a LMP1-specific manner. * indicate P < 0.05. Error barrs, mean±SEM.
We demonstrated LMP1-specific cytokine production by HELA/CAR T cells by intracellular cytokine staining (Fig. 3B and 3C). Approximately 48% and 34% of the HELA/CAR T cells produced IL-2 and IFN-γ when co-cultured with LMP1 expressing SUNE1 cells. However, only 2% and 5% of the nontransduced T cells co-cultured with LMP1-SUNE1 cells produced IL-2 and IFN-γ, respectively. In addition, only 6% and 17% of ZsGreen transduced T cells produced IL-2 and IFN-γ, respectively (Fig. 3B). Data from 3 different experiments confirmed that the differences in cytokine production between the experimental and control groups were significant (P < 0.05).Thus, in general, more HELA/CAR T cells than control effector cells (ZsGreen and non-transfected T cells) produced cytokine in response to LMP1+ NPC tumor cells.
HELA/CAR T cells inhibited the growth of LMP1 expressing NPC cells in a subcutaneous xenograft model
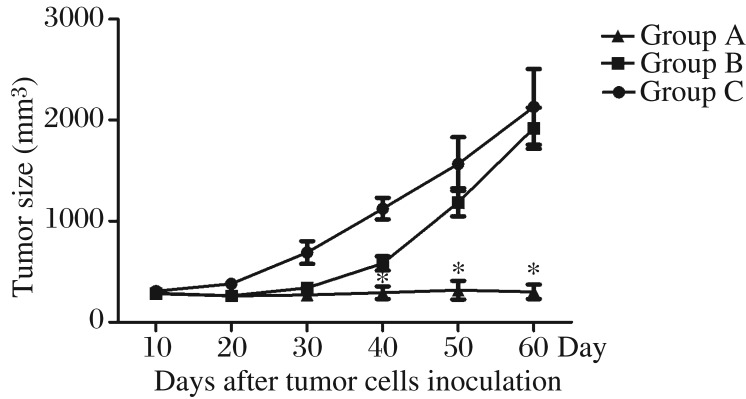
To evaluate the in vivo antitumor activity of HELA/CAR T cells, we used a xenograft model. BALB/c nude mice were inoculated with SUNE1-LMP1 cells in the flanks. In this model, the HELA/CAR T cells substantially inhibited the growth of tumors, while control T cells did not. Statistical analysis of the tumor growth curve revealed significant differences between the HELA/CAR and control groups (P < 0.05, Fig. 4).
Fig. 4. In vivo antitumor activity of HELA/CAR T cells in a xenograft model.
BALB/c nude mice were inoculated with SUNE cells overexpressing LMP1 and allowed to develop established tumors over 10 days. The mice were then randomly assigned to three groups, Group A received HELA/CAR T cells, Group B received control lentivirus transfected cells, and Group C received normal saline (NS). The results are expressed as the mean tumor volume (mm3±SD) for the three groups (N = 5 per group). The standard deviation (SD) is represented by error bars, * indicate P < 0.05.
DISCUSSION
Gene transfer to redirect the specificity of T lymphocytes to recognize cancer cells through the expression of a CAR specific for a tumor cell-surface molecule is an active area of cancer research. CAR T cells are able to recognize tumor antigen through specific scFv without MHC restriction. Recent clinical studies have shown that CD19-CAR T cells can eliminate CD19+ tumor cells in the bone marrow and blood in patients with advanced chronic or acute lymphocytic leukemia (CLL)[16]-[18]. These data suggest that CAR T cells are a powerful tool for cancer therapy. However, there are safety concerns associated with using CAR T cells to target TAAs. In a phase I study on adoptive immunotherapy using gene-modified T cells for ovarian cancer, CAR T cells specific for carbonic anhydrase IX (CAIX) damaged the bile duct epithelium due to the expression of the target antigen CAIX on normal tissue[19]. Some toxicity was observed in Her2/neu specific CAR trials. One patient died 5 days after adoptive transfer of HER2-CAR T cells because a large number of HER2-CAR T cells localized to the lung and released cytokines in response to low levels of ERBB2/HER2 on lung epithelial cells[20]. To minimize the risk of toxicity to normal tissue, we selected a virus-specific antigen, LMP1, as the target for therapy. LMP1 is expressed only in virus-infected cells and not in normal cells. Thus, off-target toxicity should be limited in clinical application of HELA/CAR T cells.
Anti-EBV T cells have become powerful therapeutic tools for the treatment of EBV-associated malignancies. Promising early studies used EBV-specific T cells (EBV-CTL) stimulated with EBV-transformed B cells (LCL) to effectively treat post-transplant lymphomas in stem cell transplant patients[21]. However, EBV-CTL therapy for EBV-associated malignancies such as NPC and Hodgkin lymphoma has had only mixed success[22]-[24]. Indeed, evidence suggests that EBV-specific T cells expanded by LCL are specific for EBNA3 proteins that are not expressed in NPC cells[25]. To overcome this limitation, more recent approaches have targeted LMP1 in NPC with LMP-specific T cells and have improved the efficacy of current adoptive immunotherapy approaches[26],[27]. LMP1-specific T cells were undetectable in PBMCs from donors, but the HELA/CAR T cells produced in this study specifically recognized LMP1 positive NPC cells and could be an ideal choice for immunotherapy.
Another concern with using CAR T cells as a therapeutic is that they may be immunogenic in a patient. In vivo immunogenicity of CAR T cells could also affect their persistence post-transfer. If murine Ig VH and VL are used to make the scFv fragments incorporated in the CAR, the mouse domain will induce humoral and cellular immune responses[28]. To prevent this, the HELA/CAR cells use a human anti-LMP1 scFv[12]. Thus the potential for immunogenicity of the HELA/CAR T cells is limited.
First generation CARs featured a single signalling domain (typically CD3ζ), and were found to have limited clinical activity for several carcinomas[19],[29],[30]. The second generation CARs include a costimulatory domain such as CD28, CD134, CD137, CD244, or ICOS[31]-[34]. Incorporating a CD28 domain into a CAR can enhance IL2 production and improve T cell expansion and persistence[35]. The HELA/CAR cells generated here exhibit LMP1 specific recognition of NPC cells in vitro, have efficient killing activity and produce IFN-γ and IL-2 in response to LMP1+ tumor cells. Most importantly, these cells were able to control LMP1+ tumor growth in an in vivo model. The results from our studies indicate that the HELA/CAR T cells could warrant further testing in clinical studies for treatment of EBV-positive cancer patients.
References
- 1.Husaini R, Ahmad M, Soo-Beng Khoo A. Epstein-Barr virus Latent Membrane Protein LMP1 reduces p53 protein levels independent of the PI3K-Akt pathway. BMC Res Notes. 2011;4:551. doi: 10.1186/1756-0500-4-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lan YY, Hsiao JR, Chang KC, Chang JS, Chen CW, Lai HC, et al. Epstein-Barr virus latent membrane protein 2A promotes invasion of nasopharyngeal carcinoma cells through ERK/Fra-1-mediated induction of matrix metalloproteinase 9. J Virol. 2012;86:6656–67. doi: 10.1128/JVI.00174-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smee RI, Meagher NS, Broadley K, Ho T, Williams JR, Bridger GP. Recurrent nasopharyngeal carcinoma: current management approaches. Am J Clin Oncol. 2010;33:469–73. doi: 10.1097/COC.0b013e3181b4b037. [DOI] [PubMed] [Google Scholar]
- 4.Tarrand JJ, Keating MJ, Tsimberidou AM, O'Brien S, LaSala RP, Han XY, et al. Epstein-Barr virus latent membrane protein 1 mRNA is expressed in a significant proportion of patients with chronic lymphocytic leukemia. Cancer. 2010;116:880–7. doi: 10.1002/cncr.24839. [DOI] [PubMed] [Google Scholar]
- 5.Li HP, Chang YS. Epstein-Barr virus latent membrane protein 1: structure and functions. J Biomed Sci. 2003;10:490–504. doi: 10.1007/BF02256110. [DOI] [PubMed] [Google Scholar]
- 6.Straathof KC, Bollard CM, Popat U, Huls MH, Lopez T, Morriss MC, et al. Treatment of nasopharyngeal carcinoma with Epstein-Barr virus–specific T lymphocytes. Blood. 2005;105:1898–904. doi: 10.1182/blood-2004-07-2975. [DOI] [PubMed] [Google Scholar]
- 7.Lee SP. Nasopharyngeal carcinoma and the EBV-specific T cell response: prospects for immunotherapy. Semin Cancer Biol. 2002;12:463–71. doi: 10.1016/s1044-579x(02)00089-5. [DOI] [PubMed] [Google Scholar]
- 8.Louis CU, Straathof K, Bollard CM, Gerken C, Huls MH, Gresik MV, et al. Enhancing the in vivo expansion of adoptively transferred EBV-specific CTL with lymphodepleting CD45 monoclonal antibodies in NPC patients. Blood. 2009;113:2442–50. doi: 10.1182/blood-2008-05-157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chua D, Huang J, Zheng B, Lau SY, Luk W, Kwong DL, et al. Adoptive transfer of autologous Epstein-Barr virus-specific cytotoxic T cells for nasopharyngeal carcinoma. Int J Cancer. 2001;94:73–80. doi: 10.1002/ijc.1430. [DOI] [PubMed] [Google Scholar]
- 10.Comoli P, De Palma R, Siena S, Nocera A, Basso S, Del Galdo F, et al. Adoptive transfer of allogeneic Epstein-Barr virus (EBV)-specific cytotoxic T cells with in vitro antitumor activity boosts LMP2-specific immune response in a patient with EBV-related nasopharyngeal carcinoma. Ann Oncol. 2004;15:113–7. doi: 10.1093/annonc/mdh027. [DOI] [PubMed] [Google Scholar]
- 11.Jena B, Dotti G, Cooper LJ. Redirecting T-cell specificity by introducing a tumor-specific chimeric antigen receptor. Blood. 2010;116:1035–44. doi: 10.1182/blood-2010-01-043737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen R, Zhang D, Mao Y, Zhu J, Ming H, Wen J, et al. A human Fab-based immunoconjugate specific for the LMP1 extracellular domain inhibits nasopharyngeal carcinoma growth in vitro and in vivo. Mol Cancer Ther. 2012;11:594–603. doi: 10.1158/1535-7163.MCT-11-0725. [DOI] [PubMed] [Google Scholar]
- 13.Lee HJ, Lee YS, Kim HS, Kim YK, Kim JH, Jeon SH, et al. Retronectin enhances lentivirus-mediated gene delivery into hematopoietic progenitor cells. Biologicals. 2009;37:203–9. doi: 10.1016/j.biologicals.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Kochenderfer JN, Feldman SA, Zhao Y, Xu H, Black MA, Morgan RA, et al. Construction and preclinical evaluation of an anti-CD19 chimeric antigen receptor. J Immunother. 2009;32:689–702. doi: 10.1097/CJI.0b013e3181ac6138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parish CR, Glidden MH, Quah BJ, Warren HS. Use of the intracellular fluorescent dye CFSE to monitor lymphocyte migration and proliferation. Curr Protoc Immunol. 2009 doi: 10.1002/0471142735.im0409s84. Chapter 4: Unit4 9. [DOI] [PubMed] [Google Scholar]
- 16.Porter DL, Levine BL, Kalos M, Bagg A, June CH. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365:725–33. doi: 10.1056/NEJMoa1103849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kochenderfer JN, Wilson WH, Janik JE, Dudley ME, Stetler-Stevenson M, Feldman SA, et al. Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood. 2010;116:4099–102. doi: 10.1182/blood-2010-04-281931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grupp SA, Kalos M, Barrett D, Aplenc R, Porter DL, Rheingold SR, et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med. 2013;368:1509–18. doi: 10.1056/NEJMoa1215134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kershaw MH, Westwood JA, Parker LL, Wang G, Eshhar Z, Mavroukakis SA, et al. A phase I study on adoptive immunotherapy using gene-modified T cells for ovarian cancer. Clin Cancer Res. 2006;12:6106–15. doi: 10.1158/1078-0432.CCR-06-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan RA, Yang JC, Kitano M, Dudley ME, Laurencot CM, Rosenberg SA. Case report of a serious adverse event following the administration of T cells transduced with a chimeric antigen receptor recognizing ERBB2. Mol Ther. 2010;18:843–51. doi: 10.1038/mt.2010.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bollard CM, Savoldo B, Rooney CM, Heslop HE. Adoptive T-cell therapy for EBV-associated post-transplant lymphoproliferative disease. Acta Haematol. 2003;110:139–48. doi: 10.1159/000072463. [DOI] [PubMed] [Google Scholar]
- 22.Comoli P, Pedrazzoli P, Maccario R, Basso S, Carminati O, Labirio M, et al. Cell therapy of stage IV nasopharyngeal carcinoma with autologous Epstein-Barr virus-targeted cytotoxic T lymphocytes. J Clin Oncol. 2005;23:8942–9. doi: 10.1200/JCO.2005.02.6195. [DOI] [PubMed] [Google Scholar]
- 23.Louis CU, Straathof K, Bollard CM, Ennamuri S, Gerken C, Lopez TT, et al. Adoptive transfer of EBV-specific T cells results in sustained clinical responses in patients with locoregional nasopharyngeal carcinoma. J Immunother. 2010;33:983–90. doi: 10.1097/CJI.0b013e3181f3cbf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chia WK, Teo M, Wang WW, Lee B, Ang SF, Tai WM, et al. Adoptive T-cell Transfer and Chemotherapy in the First-line Treatment of Metastatic and/or Locally Recurrent Nasopharyngeal Carcinoma. Mol Ther. 2014;22:132–9. doi: 10.1038/mt.2013.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riddell SR. Finding a place for tumor-specific T cells in targeted cancer therapy. J Exp Med. 2004;200:1533–7. doi: 10.1084/jem.20042004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gottschalk S, Edwards OL, Sili U, Huls MH, Goltsova T, Davis AR, et al. Generating CTLs against the subdominant Epstein-Barr virus LMP1 antigen for the adoptive immunotherapy of EBV-associated malignancies. Blood. 2003;101:1905–12. doi: 10.1182/blood-2002-05-1514. [DOI] [PubMed] [Google Scholar]
- 27.Smith C, Tsang J, Beagley L, Chua D, Lee V, Li V, et al. Effective treatment of metastatic forms of Epstein-Barr virus-associated nasopharyngeal carcinoma with a novel adenovirus-based adoptive immunotherapy. Cancer Res. 2012;72:1116–25. doi: 10.1158/0008-5472.CAN-11-3399. [DOI] [PubMed] [Google Scholar]
- 28.Lamers CH, Willemsen R, van Elzakker P, van Steenbergen-Langeveld S, Broertjes M, Oosterwijk-Wakka J, et al. Immune responses to transgene and retroviral vector in patients treated with ex vivo-engineered T cells. Blood. 2011;117:72–82. doi: 10.1182/blood-2010-07-294520. [DOI] [PubMed] [Google Scholar]
- 29.Till BG, Jensen MC, Wang J, Chen EY, Wood BL, Greisman HA, et al. Adoptive immunotherapy for indolent non-Hodgkin lymphoma and mantle cell lymphoma using genetically modified autologous CD20-specific T cells. Blood. 2008;112:2261–71. doi: 10.1182/blood-2007-12-128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park JR, Digiusto DL, Slovak M, Wright C, Naranjo A, Wagner J, et al. Adoptive transfer of chimeric antigen receptor re-directed cytolytic T lymphocyte clones in patients with neuroblastoma. Mol Ther. 2007;15:825–33. doi: 10.1038/sj.mt.6300104. [DOI] [PubMed] [Google Scholar]
- 31.Finney HM, Lawson AD, Bebbington CR, Weir AN. Chimeric receptors providing both primary and costimulatory signaling in T cells from a single gene product. J Immunol. 1998;161:2791–7. [PubMed] [Google Scholar]
- 32.Pule MA, Straathof KC, Dotti G, Heslop HE, Rooney CM, Brenner MK. A chimeric T cell antigen receptor that augments cytokine release and supports clonal expansion of primary human T cells. Mol Ther. 2005;12:933–41. doi: 10.1016/j.ymthe.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 33.Hombach AA, Abken H. Costimulation by chimeric antigen receptors revisited the T cell antitumor response benefits from combined CD28-OX40 signalling. Int J Cancer. 2011;129:2935–44. doi: 10.1002/ijc.25960. [DOI] [PubMed] [Google Scholar]
- 34.Altvater B, Landmeier S, Pscherer S, Temme J, Juergens H, Pule M, et al. 2B4 (CD244) signaling via chimeric receptors costimulates tumor-antigen specific proliferation and in vitro expansion of human T cells. Cancer Immunol Immunother. 2009;58:1991–2001. doi: 10.1007/s00262-009-0704-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Savoldo B, Ramos CA, Liu E, Mims MP, Keating MJ, Carrum G, et al. CD28 costimulation improves expansion and persistence of chimeric antigen receptor-modified T cells in lymphoma patients. J Clin Invest. 2011;121:1822–6. doi: 10.1172/JCI46110. [DOI] [PMC free article] [PubMed] [Google Scholar]