Abstract
Because of the potential morbidity and complications associated with surgical procedures, limiting the extent of orthognathic surgery is a desire for many orthodontic patients. An eighteen-year-old woman had a severe Class III malocclusion and required bi-maxillary surgery. By changing the patient's maxillary occlusal plane using orthodontic mini-implants, she was able to avoid the maxillary surgery; requiring only a mandibular setback surgery. To accurately predict the post-surgery outcome, we applied a new soft tissue prediction method. We were able to follow and report the long-term result of her combined orthodontic and orthognathic treatment. The changes to her occlusal plane continue to appear stable over 6 years later.
Keywords: Mini-implant, Mandibular setback surgery, Soft tissue prediction
INTRODUCTION
Single jaw surgeries are less invasive and more predictable than two-jaw surgeries. However, for many severe Class III patients, mandibular setback surgery alone may be insufficient to achieve a harmonious profile change. Therefore, numerous Class III surgery patients require two-jaw surgery with maxillary clockwise rotation.
Severe Class III patients commonly have extruded upper molars since the lower arch is in a more anterior position leaving the most distal teeth of the upper arch to have no opposing teeth.1 Extruded upper molars, especially the upper second molars, often not only create an upward cant of the maxillary occlusal plane, but also interfere with sufficient backward movement of the chin when correction is required. A number of recent studies demonstrate that mini-implants provide reliable skeletal anchorage to aid with molar intrusion.2,3,4,5,6 Consequently, these interfering molars of Class III patients can be intruded effectively with mini-implants. Severe Class III patients also often have facial asymmetries.7 The facial asymmetry is often caused by a canted occlusal plane. Transverse occlusal plane canting can be caused by extrusion of teeth on one side of maxilla. Likewise, transverse canting due to unilaterally extruded maxillary molars can also be corrected with mini-implants. By correcting the maxillary occlusal plane, a bimaxillary surgery case could be reduced to a simpler single-jaw mandibular setback surgery. If this is possible, the extent of orthognathic surgery would be minimized, benefiting the patient.
This article describes a patient with a severe Class III malocclusion treated by mandibular setback surgery combined with the use of mini-implants to intrude upper molars. The stability of the treatment result was evaluated six years after completion of the treatment. After more than six years, the occlusal plane remains stable. This report also introduces an application of a more accurate soft tissue prediction method for determining surgical treatment planning.
DIAGNOSIS AND ETIOLOGY
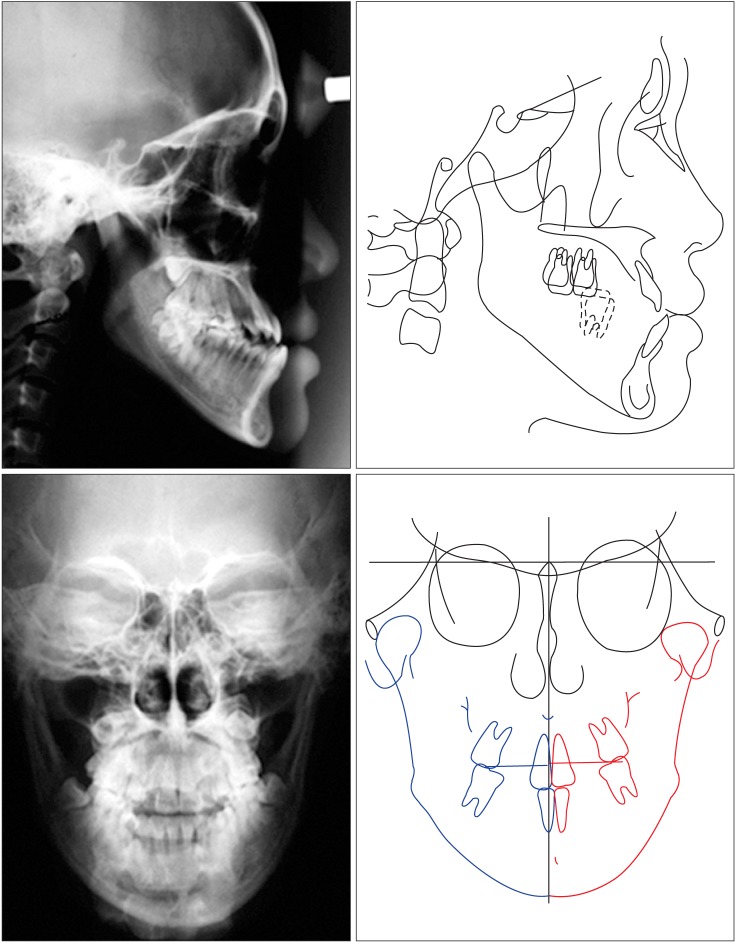
An eighteen-year-old high school girl with a chief complaint of an anterior crossbite sought orthodontic treatment. The extraoral clinical examination revealed a concave profile (Figure 1). Cephalometric analysis indicated a skeletal Class III pattern (Table 1): mandibular prognathism (Pog to N-perpendicular, 10.8 mm; ANB, -5.8°), proclined upper incisors (upper occlusal plane to upper incisors, 51.0°), retroclined lower incisors (lower occlusal plane to lower incisors, 80.5°), and a flat occlusal plane (upper occlusal plane to FH, 7.5°). The intraoral examination demonstrated a Class III malocclusion with anterior and posterior crossbites and extruded upper second molars. The panoramic radiograph revealed the presence of impacted third molars. Analysis of the posteroanterior radiograph revealed occlusal plane canting due to overeruption of the right molars. Her mandible was deviated to the left side as a result of the transverse cant of the maxillary occlusal plane (Figure 2). The mandibular dental midline was shifted to the left side and the maxillary incisors were tilted to the left side due to transverse dentoalveolar compensation.
Figure 1.
Pretreatment facial and intraoral photographs.
Table 1.
Cephalometric measurements
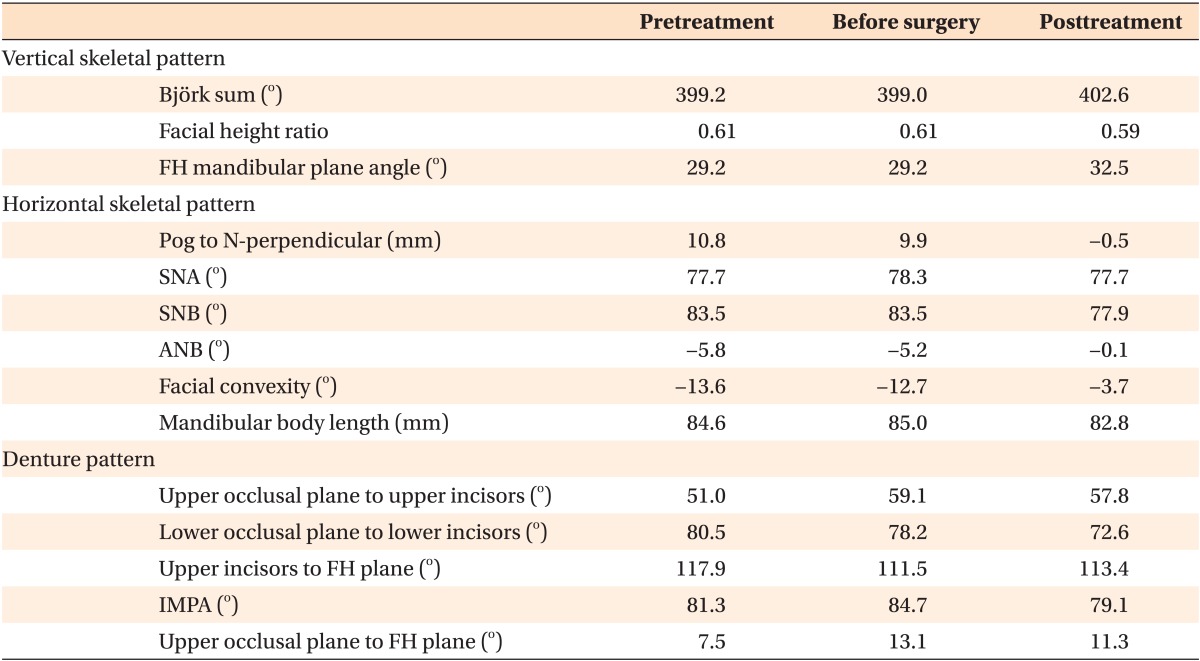
Pog to-N perpendicular, Distance from pogonion to nasion perpendicular line; SNA, sella-nasion-point A angle; SNB, sella-nasion-point B angle; ANB, point A-nasion-point B angle; IMPA, lower incisor-mandibular plane angle; FH, Frankfort horizontal plane.
Figure 2.
Pretreatment cephalograms.
According to the aforementioned findings, she was diagnosed as a skeletal Class III malocclusion due to mandibular prognathism along with facial asymmetry.
TREATMENT OBJECTIVES
Since the patient had mild crowding, a posterior crossbite, and proclined maxillary incisors, we planned to extract the maxillary first premolars for pre-surgical orthodontic treatment. Surgical setback movement of the mandible was necessary to obtain facial esthetics and normal occlusion.
TREATMENT ALTERNATIVES
There were two treatment options to achieve a favorable final result. The first option was two-jaw surgery combining mandibular surgery with clockwise rotation of the maxilla. The second option was mandibular surgery combined with intrusion of the maxillary posterior teeth during pre-surgical orthodontic treatment, instead of the surgical repositioning of the maxilla. We chose the second option in order to simplify the surgical procedure as well as to achieve the desired esthetic profile. Thus, the treatment plan was as follows:
1) Extract the upper first premolars and the lower third molars;
2) Intrude the upper molars during pre-surgical orthodontic treatment; intrude the right posterior teeth more than the left posterior teeth to resolve the transverse canting of the occlusal plane;
3) Reassess whether backward movement of the chin can be sufficiently achieved by one-jaw surgery;
4) Perform mandibular setback surgery to correct the sagittal skeletal discrepancy;
5) Complete postsurgical orthodontic treatment to establish an ideal occlusal relationship.
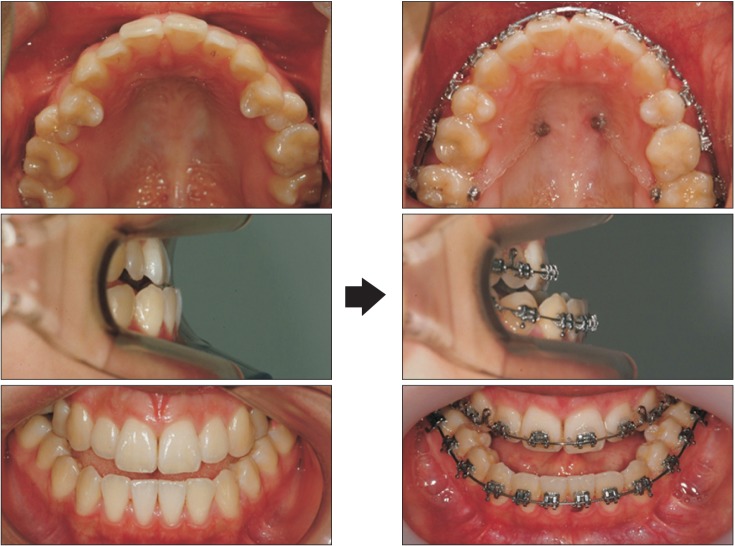
TREATMENT PROGRESS
After the upper first premolars were extracted, the upper teeth were bonded with 0.022-slot brackets. Considering the additional time required for the upper arch space closure, lower brackets were placed after initial alignment of the upper teeth to minimize the amount of time with lower brackets. After 10 months of treatment, two mini-implants of 8 mm in length were placed in the palate bilaterally. The upper molars were intruded by elastic chains, which spanned from the mini-implants to the upper second molar lingual buttons. In order to resolve the occlusal plane canting of this patient, we intruded the extruded teeth on the right side more than the teeth on the left side. After 14 months of treatment, the extraction spaces were closed completely, and the maxillary molars were intruded (Figure 3). After pre-surgical orthodontic treatment, the upper and lower incisor angles were within normal range (upper occlusal plane to upper incisors, 59.1°; lower occlusal plane to lower incisors, 78.2°; upper occlusal plane to FH, 13.1°). After we reassessed the patient to confirm whether an esthetic treatment outcome could be achieved by one-jaw surgery, mandibular set back surgery was performed. The orthodontic braces were removed 10 months after the orthognathic surgery. The overall active treatment duration was 24 months. Hawley retainers were delivered within a week.
Figure 3.
Pretreatment photographs and photographs before surgery demonstrating the mechanics used to intrude the upper molars.
RESULTS
The patient showed a dramatic change in the facial profile after treatment. The prognathic chin moved backward properly. The actual treatment outcome was consistent with the soft tissue profile predicted by a new prediction method we have developed. The amount of mandibular setback was approximately 10 mm (Figure 4). The sagittal relationship of the jaws was improved (Pog to N-perpendicular, -0.5 mm; ANB, -0.1°), and the asymmetry was corrected. Class I canine and Class II molar relationships with ideal overbite/overjet and coincident dental midlines were attained after treatment (Figure 5).
Figure 4.
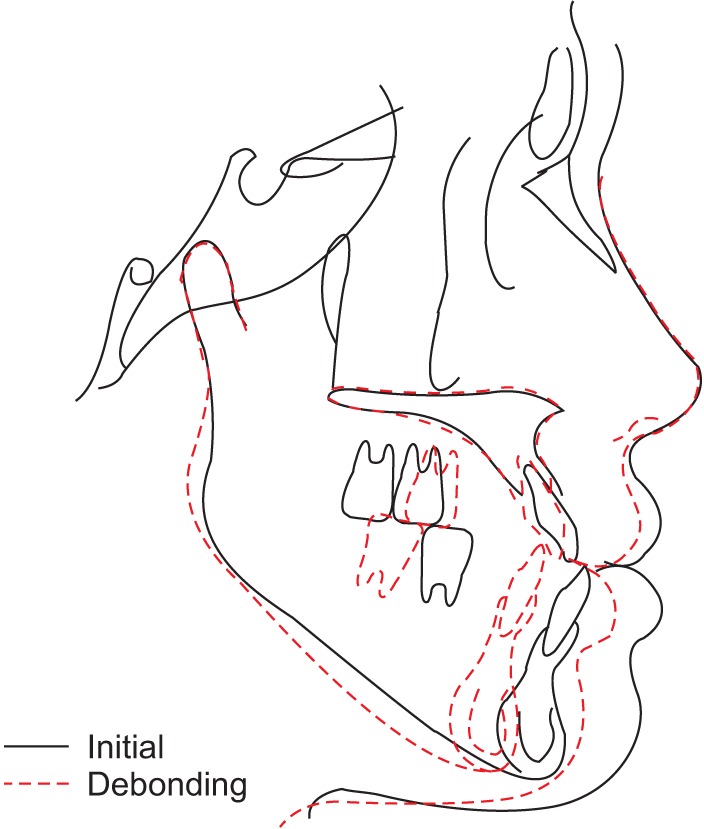
Superimposition of cephalometric tracings.
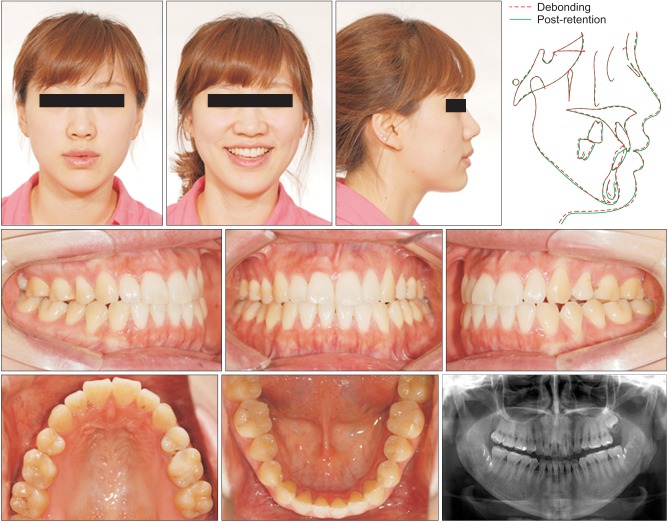
Figure 5.
Posttreatment records.
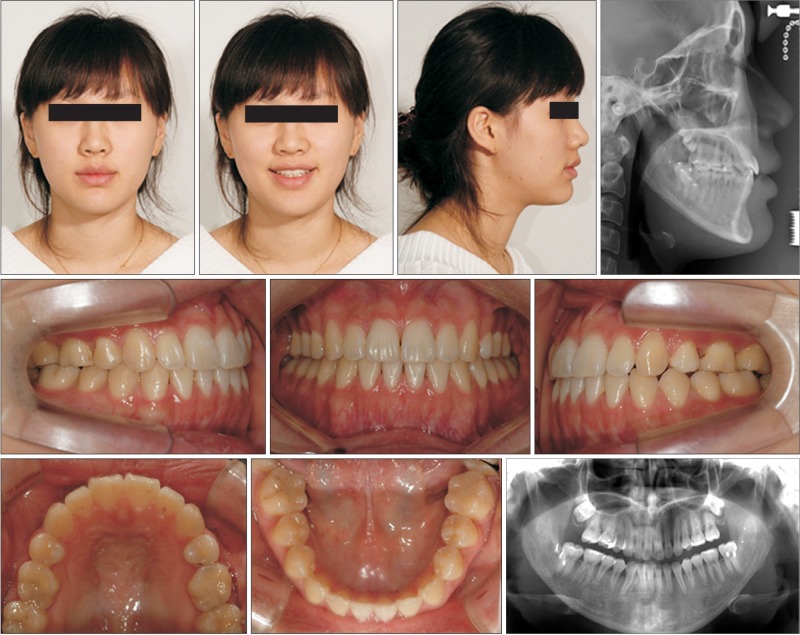
Six years after the orthodontic treatment, the patient reported no discomfort and maintained relatively stable occlusion (Figure 6).
Figure 6.
Records at six years after treatment completion.
DISCUSSION
Orthognathic surgery has become a common clinical procedure in the correction of dento-skeletal imbalances. A recent article reported that 70.7% of patients undergoing orthognathic surgery had Class III malocclusion before treatment.8 The combination of an osteotomy of the maxilla and a mandibular setback surgery with an additional genioplasty seems to be the current trend for skeletal Class III treatment.9,10 Combining orthodontic and surgical treatment provides a more efficient and esthetic treatment. Due to potential complications and possibly longer recovery times, it would be desirable if the complexity of the orthognathic surgery component of treatment could be minimized through effective pre-surgical orthodontic treatment. Intrusion of the posterior teeth can easily be obtained with mini-implants.11 This also permits more flexibility for the surgeon with regards to the amount of the positioning of the mandibular setback. By intruding the maxillary molars and consequently rotating the maxillary occlusal plane clockwise, a more favorable rotation of the distal segment of the mandible can be achieved during mandibular setback surgery. A number of skeletal Class III patients with facial asymmetry have transverse canting of the occlusal plane due to unilaterally extruded maxillary molars. These molars can also be intruded with mini-implants in order to correct a canted occlusal plane. To resolve the occlusal plane canting of the patient in this study, we intruded the right posterior teeth more than the left posterior teeth. By altering the maxillary occlusal planes both in the sagittal and transverse planes with mini-implants during pre-surgical orthodontic treatment, the surgical procedure was simplified.
During molar intrusion, the first, second, and third order relationship of the intruded molars should be monitored.12 The posterior torque control is the most important factor.11 Maxillary second molars often possess buccal crown inclination and distal crown angulation before treatment. Distal tipping and flaring of molars are common in Class III malocclusion patients whose maxillae often have deficient room for posterior teeth.1 Because a palatal and slightly mesial vector was preferred in this patient, we placed mini-implants bilaterally in the palate at the level of the premolars. Mini-implants and mini-plates are reliable devices when absolute anchorage is necessary. Palatal mini-implants pose little danger of root damage, and they are less susceptible to inflammation. A number of investigations indicate that bone thickness and density of the palate are favorable for mini-implant placement near the mid-palate at the level of the premolars.13,14
When predicting the final surgical outcome, we applied a new prediction method to this patient. The partial least squares method predicted more accurate results than the conventional method. For a more detailed discussion regarding the prediction method, please refer to the previous publications.15,16,17,18 The use of computers and graphics in treatment planning is increasing and with software based on this new algorithm, more precise predictions of resulting soft tissue profiles will be possible.19
We assessed the stability of the treatment result after six years. Clinical examination at six years after completion of orthodontic treatment revealed some relapse of only the buccal occlusion when compared to the point of treatment completion. Factors contributing to stability in this case would be relapse after intrusion and postoperative relapse after mandibular setback surgery. Postoperative relapse might be more related to the degree of the intraoperative clockwise movement of the proximal segment, rather than the amount of setback movement.12,20 Superimposition of cephalometric tracings at treatment completion and at six years post-treatment revealed a small extent of clockwise rotation of mandible; yet there was no extrusion of the molars (Figure 6). This type of change in occlusion after treatment is due to the progressive uprighting of lower molars which were originally tilted lingually. It is known that increased tongue pressure against the distally repositioned mandible can upright the mandibular posterior teeth in a buccal direction.1 Anticipating that the upper third molars would occlude with the mandibular second molars, we extracted only the lower third molars in this upper premolar extraction case (Figure 5).
CONCLUSION
It is certainly beneficial to combine surgical and orthodontic treatment in order to provide an efficient and esthetic result. Surgical interferences and occlusal plane canting caused by extruded molars can be corrected with mini-implants, as with this patient, obviating the need for maxillary surgery.
ACKNOWLEDGEMENTS
The authors express gratitude to Dr. Richard E Donatelli, at University of Florida College of Dentistry, for his invaluable assistance to improve this manuscript.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
This work was partly supported by the Basic Science Research Program [Grant No. NRF 2012-0007574] and partly by grant number 02-2014-0003 from the Seoul National University Dental Hospital Research Fund.
References
- 1.Lee SJ, Kim TW, Nahm DS. Transverse implications of maxillary premolar extraction in Class III presurgical orthodontic treatment. Am J Orthod Dentofacial Orthop. 2006;129:740–748. doi: 10.1016/j.ajodo.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Lee SJ, Lin L, Kim SH, Chung KR, Donatelli RE. Survival analysis of a miniplate and tube device designed to provide skeletal anchorage. Am J Orthod Dentofacial Orthop. 2013;144:349–356. doi: 10.1016/j.ajodo.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 3.Lee SJ, Ahn SJ, Lee JW, Kim SH, Kim TW. Survival analysis of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:194–199. doi: 10.1016/j.ajodo.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 4.Yao CC, Lee JJ, Chen HY, Chang ZC, Chang HF, Chen YJ. Maxillary molar intrusion with fixed appliances and mini-implant anchorage studied in three dimensions. Angle Orthod. 2005;75:754–760. doi: 10.1043/0003-3219(2005)75[754:MMIWFA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Park YC, Lee SY, Kim DH, Jee SH. Intrusion of posterior teeth using mini-screw implants. Am J Orthod Dentofacial Orthop. 2003;123:690–694. doi: 10.1016/s0889-5406(03)00047-7. [DOI] [PubMed] [Google Scholar]
- 6.Deguchi T, Takano-Yamamoto T, Kanomi R, Hartsfield JK, Jr, Roberts WE, Garetto LP. The use of small titanium screws for orthodontic anchorage. J Dent Res. 2003;82:377–381. doi: 10.1177/154405910308200510. [DOI] [PubMed] [Google Scholar]
- 7.Choi HJ, Kim TW, Ahn SJ, Lee SJ, Donatelli RE. The relationship between temporomandibular joint disk displacement and mandibular asymmetry in skeletal Class III patients. Angle Orthod. 2011;81:624–631. doi: 10.2319/091210-532.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jung MH. Age, extraction rate and jaw surgery rate in Korean orthodontic clinics and small dental hospitals. Korean J Orthod. 2012;42:80–86. doi: 10.4041/kjod.2012.42.2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoon KS, Lee HJ, Lee SJ, Donatelli RE. Testing a better method of predicting postsurgery soft tissue response in Class II patients: A prospective study and validity assessment. Angle Orthod. 2014 doi: 10.2319/052514-370.1. doi: 10.2319/052514-370.1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bailey LJ, Cevidanes LH, Proffit WR. Stability and predictability of orthognathic surgery. Am J Orthod Dentofacial Orthop. 2004;126:273–277. doi: 10.1016/S0889540604005207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park YC, Lee HA, Choi NC, Kim DH. Open bite correction by intrusion of posterior teeth with miniscrews. Angle Orthod. 2008;78:699–710. doi: 10.2319/0003-3219(2008)078[0699:OBCBIO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Lee SJ, Jang SY, Chun YS, Lim WH. Three-dimensional analysis of tooth movement after intrusion of a supraerupted molar using a mini-implant with partial-fixed orthodontic appliances. Angle Orthod. 2013;83:274–279. doi: 10.2319/060912-480.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moon SH, Park SH, Lim WH, Chun YS. Palatal bone density in adult subjects: implications for mini-implant placement. Angle Orthod. 2010;80:137–144. doi: 10.2319/011909-40.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang S, Lee SJ, Ahn SJ, Heo MS, Kim TW. Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop. 2007;131(4 Suppl):S74–S81. doi: 10.1016/j.ajodo.2005.09.029. [DOI] [PubMed] [Google Scholar]
- 15.Lee HJ, Suh HY, Lee YS, Lee SJ, Donatelli RE, Dolce C, et al. A better statistical method of predicting postsurgery soft tissue response in Class II patients. Angle Orthod. 2014;84:322–328. doi: 10.2319/050313-338.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donatelli RE, Lee SJ. How to report reliability in orthodontic research: Part 2. Am J Orthod Dentofacial Orthop. 2013;144:315–318. doi: 10.1016/j.ajodo.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 17.Suh HY, Lee SJ, Lee YS, Donatelli RE, Wheeler TT, Kim SH, et al. A more accurate method of predicting soft tissue changes after mandibular setback surgery. J Oral Maxillofac Surg. 2012;70:e553–e562. doi: 10.1016/j.joms.2012.06.187. [DOI] [PubMed] [Google Scholar]
- 18.Lee YS, Suh HY, Lee SJ, Donatelli RE. More accurate soft-tissue prediction model for Class III 2-jaw surgeries. Am J Orthod Dentofacial Orthop. 2014;146:724–733. doi: 10.1016/j.ajodo.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 19.Jeon H, Lee SJ, Kim TW, Donatelli RE. Three-dimensional analysis of lip and perioral soft tissue changes after debonding of labial brackets. Orthod Craniofac Res. 2013;16:65–74. doi: 10.1111/ocr.12006. [DOI] [PubMed] [Google Scholar]
- 20.Han JJ, Yang HJ, Lee SJ, Hwang SJ. Relapse after SSRO for mandibular setback movement in relation to the amount of mandibular setback and intraoperative clockwise rotation of the proximal segment. J Craniomaxillofac Surg. 2014;42:811–815. doi: 10.1016/j.jcms.2013.11.018. [DOI] [PubMed] [Google Scholar]