Abstract
AIM: There is strong evidence that tyrosine kinases are involved in the regulation of tumor progression, cellular growth and differentiation. Recently, many kinds of tyrosine kinase receptors have been reported, among them Tie-1 and Tie-2 receptors constitute a major class. Angiopoietin (Ang)-1 is known as a ligand of Tie-2 tyrosine kinase receptor. The objective of this study was to establish a comprehensive Tie-1 and Tie-2 and Ang-1, 2 and 4 expression profile in human colorectal adenocarcinomas.
METHODS: We examined 96 cases of surgically resected human colorectal adenocarcinoma by immunohistochemistry and investigated the statistical correlation between the expressions of Ties and Angs and clinicopathological factors.
RESULTS: Among the 96 cases of adenocarcinoma, 87 (90.6%), 92 (95.8%), 83 (86.5%), 89 (92.7%), and 76 cases (79.2%) showed positive staining in the cytoplasm of carcinoma cells for the Tie-1 and Tie-2 and Ang-1, 2 and 4 proteins, respectively. Histologically, the expressions of Ties and Angs were variable. The expressions of Ties and Angs were correlated with several clinicopathological factors, but did not correlate with the presence of lymph node metastasis. Ties and Angs were highly expressed in human colorectal adenocarcinoma cells.
CONCLUSION: These findings suggest that the Tie-Ang receptor-ligand complex is one of the factors involved in the cellular differentiation and progression of human colorectal adenocarcinoma.
Keywords: Tie, Angiopoietin, Colorectal carcinoma
INTRODUCTION
The prognosis of colorectal cancer patients is based on the depth of invasion and the presence of lymph node metastasis[1]. Usually, these parameters can be determined by microscopic examination of tissue sections from the primary neoplasm and lymph nodes[2]. However, only histopathological examination of primary colorectal carcinoma specimens cannot always elucidate the prognosis[2]. Recently, the occurrence and progression of cancer are suggested to be related to a series of genetic events affecting the structure and/or the expression of a number of oncogenes, anti-oncogenes and growth factors. However, the mechanism of the invasion of colorectal carcinomas has not been fully elucidated.
Several tyrosine kinase receptors (TKRs) have been identified that are associated with tumor cell proliferation and differentiation, including the vascular endothelial growth factor (VEGF) family TKRs, Flt-1, Flt-4 and KDR/Flk-1 TKRs[3]. As both Tie-1 and Tie-2 possess unique, multiple extracellular domains, they are thought to represent a new subfamily of TKRs[4,5]. Like the VEGF receptors, Tie-1 and Tie-2 are highly expressed and play critical roles during embryonic development[4-7]. Experimental evidence from the targeted disruption of Tie-1 and Tie-2 gene function suggests that Tie-2 plays a pivotal role in developmental angiogenesis and vascular remodeling[6,7], whereas Tie-1 appears to be required for the maintenance of vascular integrity in adult mice and rats in addition to its role in angiogenesis[8,9]. The Tie-2 receptor is up-regulated in breast cancer, particularly at the periphery of invasive carcinomas[10]. Recently, a soluble truncated Tie-2 receptor mutant has been shown to act in a dominant-negative manner to block the growth of primary murine tumors and their metastases[11,12].
The angiopoietin family of growth factors has been recently identified as ligands for Tie-2. Angiopoietin (Ang)-1 activates Tie-2 leading to receptor autophosphorylation upon binding and stimulates endothelial cell migration in vitro[13,14]. Ang-2 appears to be a natural inhibitor of Tie-2 function, binding to Tie-2 with an affinity similar to that of Ang-1 and blocks Ang-1-stimulated receptor phosphorylation in endothelial cells[14,15]. Deletion of the Ang-1 gene[16] or overexpression of Ang-2[15] in transgenic mice results in death in utero due to a broad failure of microvascular morphogenesis similar to that observed in Tie-2 knock-out mice[7].
The objective of the present study was to evaluate the role of Ties and Angs in the progression and differentiation of human colorectal adenocarcinoma.
MATERIALS AND METHODS
Cases and tissues
We studied 11 colorectal adenomas and 96 primary human colorectal adenocarcinomas. All specimens of adenoma were resected by endoscopy and all specimens of adenocarcinoma were obtained from patients operated on at Nagasaki University Hospital between 1999 and 2003. Each tumor was assigned a histological type according to the World Health Organization classification[17] and a depth grading of infiltration according to the TNM staging system by the American Joint Commission on Cancer[18]. Fifteen specimens of normal colon mucosal tissue, that were taken from patients without colorectal cancer, were evaluated as the normal control.
The desmoplastic stromal reaction was graded according to the extent of the stromal area involved. It was defined as “slight” (when the fibrous stromal area was less than 25% of the whole tumor), “moderate” (between 25% and 50%), and “extensive” (when it exceeded 75% of the whole tumor) based on the overall pattern[19]. The examination was performed on routine slides to identify lymphatic, venous and perineural invasions. In addition to hematoxylin and eosin staining, we also used elastic van Gieson staining in all cases. Each parameter was defined as “present” when the invasion was identified with certainty, but defined as “absent” when either was not observed at all or not observed with certainty[20,21]. Lymph node metastasis was defined as “present” only when it was histologically proven. Diagnosis was established by two independent pathologists (TN, IS), and cases of questionable diagnosis were omitted from the study.
Immunohistochemistry
Formalin-fixed and paraffin-embedded tissues were cut into 4 µm sections, deparaffinized in xylene and rehydrated in phosphate-buffered saline. Deparaffinized sections were preincubated with normal bovine serum to prevent nonspecific binding, and then incubated overnight at 4 °C with an optimal dilution (0.1 µg/mL) of a primary polyclonal rabbit antibody against human Tie-1 (C-18), Tie-2 (C-20), Ang-1 (N-18), Ang-2 (N-18) or Ang-4 (L-18). Each antibody was purchased from Santa Cruz Biotechnology Inc., (Santa Cruz, CA, USA). The slides for Tie-1 and Tie-2 were then sequentially incubated with an alkaline phosphatase-conjugated horse antirabbit immunoglobulin antibody, and the reaction products were resolved using a mixture of 5-bromo-4-chloro-3-indolyl phosphate and nitroblue tetrazolium chloride (BCIP/NBT; BRL, Gaithersburg, MD, USA). The slides for Ang-1, 2 and 4 were sequentially incubated with a biotinylated horse antirabbit immunoglobulin antibody, and the reaction products were resolved using diaminobenzidine (DAB; DAKO Ltd., Glostrup, Denmark). Primary antibodies preabsorbed with excess recombinant Tie-1 and Tie-2 and Ang-1, 2 and 4 peptides, respectively (Santa Cruz Biotechnology Inc.) were used as negative controls. Gastric ulcer tissue with capillary proliferation served as the internal positive control for Ties and Angs immunostaining. Analysis of the immunohistochemical staining was performed independently by two investigators (TN, IS). Tie-1 and Tie-2 and Ang-1, 2 and 4 expressions were classified into three categories depending on the percentage of cells stained: -, 0% to 10% positive cells; +, 10% to 50% positive tumor cells; and ++, >50% positive tumor cells.
Statistical analysis
The Stat View II program (Abacus Concepts, Inc., Berkeley, CA, USA) was used for statistical analyses. Analyses comparing the degrees of Tie-1 and Tie-2 and Ang-1, 2 and 4 expressions were performed by the Mann-Whitney and Spearman’s tests. P<0.05 was taken as significant.
RESULTS
Benign colorectal epithelial cells showed focal and patch immunoreactivity of Ties and Angs with faint to mild staining intensity (data not shown). Ties and Angs were also expressed in colorectal adenomas (Table 1). We summarized the immunohistochemical results of colorectal adenocarcinomas in Tables 1, 2 and Figure 1. Among the 96 cases of adenocarcinoma, 87 (90.6%), 92 (95.8%), 83 (86.5%), 89 (92.7%), and 76 cases (79.2%) showed positive staining in the cytoplasm of carcinoma cells for Tie-1 and Tie-2 and Ang-1, 2 and 4 proteins, respectively (Table 1). Histologically, the expressions of Tie-1 and Tie-2 and Ang-1, 2 and 4 were variable. With the exception of mucinous carcinomas, the expressions of Tie-1, Tie-2 and Ang-1,4 were significantly correlated with the degree of well, moderate and poor histological differentiation (P = 0.000123, P = 0.002209, P = 0.000161, P = 0.008193, respectively). Tie-1 and Tie-2 and Ang-1, 2 and 4 expressions correlated with the depth of tumor invasion (P = 0.000473, P = 0.006137, P = 0.000747, P = 0.0097, P = 0.000949, respectively). Tie-1, Tie-2 and Ang-1, 4 expressions correlated with Duke’s classification (P = 0.00038, P = 0.0037, P = 0.00124, P = 0.015936, respectively). The expression of Tie-2 was significantly correlated with the degree of desmoplastic stromal reaction (P = 0.039383) (Table 2). The expressions of Tie-2 and Ang-2 correlated with the degree of venous invasions (P = 0.005992, P = 0.018168, respectively). The expressions of Tie-1 and Tie-2 and Ang-1 correlated with the presence of lymphatic invasion (P = 0.033356, P = 0.001326, P = 0.039066, respectively). There was no correlation between the expression of Angs/Ties and the presence of lymph node metastasis (Table 2).
Table 1.
Histological differentiation, invasion and Tie-1, 2 and Ang-1, 2, 4 expressions in human colorectal adenocarcinoma (n = 96), n (%).
| n |
Tie-1 |
Tie-2 |
Ang-1 |
Ang-2 |
Ang-4 |
|||||||||||
| - | + | ++ | - | + | ++ | - | + | ++ | - | + | ++ | - | + | ++ | ||
| Adenoma | 11 | 7 (63.6) | 3 (27.3) | 1 (9.1) | 6 (54.5) | 3 (27.3) | 2 (18.1) | 7 (63.6) | 3 (27.3) | 1 (9.1) | 7 (63.6) | 3 (27.3) | 1 (9.1) | 8 (72.2) | 3 (27.3) | 0 (0.0) |
| Total carcinoma | 96 | 9 (9.4) | 24 (25.0) | 63 (65.6) | 4 (4.2) | 25 (26.0) | 67 (69.8) | 13 (13.5) | 25 (26.0) | 58 (60.4) | 7 (7.3) | 23 (24.0) | 66 (69.0) | 20 (20.8) | 27 (28.1) | 49 (51.0) |
| Histological differentiation | P = 0.000123 | P = 0.002209 | P = 0.000161 | NS | P = 0.008193 | |||||||||||
| Ca in adenoma | 18 | 3 (16.7) | 8 (44.4) | 7 (38.9) | 1 (5.6) | 7 (38.9) | 10 (55.6) | 6 (33.3) | 7 (38.9) | 5 (27.8) | 3 (16.7) | 4 (22.2) | 11 (61.1) | 6 (33.3) | 7 (38.9) | 5 (27.8) |
| Well | 29 | 5 (17.2) | 7 (24.1) | 17 (58.6) | 2 (6.9) | 12 (41.4) | 15 (51.7) | 4 (13.8) | 7 (24.1) | 18 (62.1) | 2 (6.9) | 7 (24.1) | 20 (69.0) | 7 (24.1) | 7 (24.1) | 15 (51.7) |
| Moderate | 38 | 0 (0.0) | 7 (18.4) | 31 (81.6) | 0 (0.0) | 5 (13.2) | 33 (86.8) | 2 (5.3) | 8 (21.1) | 28 (73.7) | 1 (2.6) | 8 (21.1) | 29 (76.3) | 3 (7.9) | 11 (28.9) | 24 (63.2) |
| Poor | 6 | 0 (0.0) | 0 (0.0) | 6 (100.0) | 0 (0.0) | 1 (16.7) | 5 (83.3) | 0 (0.0) | 0 (0.0) | 6 (100.0) | 0 (0.0) | 2 (33.3) | 4 (66.7) | 1(16.7) | 1 (16.7) | 4 (66.7) |
| Mucinous | 5 | 1 (20.0) | 2 (40.0) | 2 (40.0) | 1 (20.0) | 0 (0.0) | 4 (80.0) | 1 (20.0) | 3 (60.0) | 1 (20.0) | 1 (20.0) | 2 (40.0) | 2 (40.0) | 3 (60.0) | 1 (20.0) | 1 (20.0) |
| Depth of tumor invasion | P = 0.000473 | P = 0.006137 | P = 0.000747 | P = 0.0097 | P = 0.000949 | |||||||||||
| Tis | 20 | 4 (20.0) | 9 (45.0) | 7 (35.0) | 2 (10.0) | 7 (35.0) | 11 (55.0) | 7 (35.0) | 8 (40.0) | 5 (25.0) | 3 (15.0) | 6 (30.0) | 11 (55.0) | 7 (35.0) | 8 (40.0) | 5 (25.0) |
| T1 | 8 | 3 (37.5) | 3 (37.5) | 2 (25.0) | 1 (12.5) | 5 (62.5) | 2 (25.0) | 4 (50.0) | 3 (37.5) | 1 (12.5) | 2 (25.0) | 3 (37.5) | 3 (37.5) | 6 (75.0) | 1 (12.5) | 1 (12.5) |
| T2 | 10 | 0 (0.0) | 2 (20.0) | 8 (80.0) | 0 (0.0) | 2 (20.0) | 8 (80.0) | 0 (0.0) | 2 (20.0) | 8 (80.0) | 0 (0.0) | 4 (40.0) | 6 (60.0) | 1 (10.0) | 4 (40.0) | 5 (50.0) |
| T3 | 37 | 1 (2.7) | 6 (16.2) | 30 (81.1) | 0 (0.0) | 9 (24.3) | 28 (75.7) | 2 (5.4) | 5 (13.5) | 30 (81.1) | 1 (2.7) | 7 (18.9) | 29 (78.4) | 4 (10.8) | 7 (18.9) | 26 (70.3) |
| T4 | 21 | 1 (4.8) | 4 (19.0) | 16 (76.2) | 1 (4.8) | 2 (9.5) | 18 (85.7) | 0 (0.0) | 7 (33.3) | 14 (66.7) | 1 (4.8) | 3 (14.3) | 17 (81.0) | 2 (9.5) | 7 (33.3) | 12 (57.1) |
| Duke’s classification | P = 0.00038 | P = 0.0037 | P = 0.00124 | NS | P = 0.015936 | |||||||||||
| A | 38 | 7 (18.4) | 15 (39.5) | 16 (42.1) | 3 (7.9) | 15 (39.5) | 20 (52.6) | 11 (28.9) | 14 (36.8) | 13 (34.2) | 5 (13.2) | 12 (31.6) | 21 (55.3) | 13 (34.2) | 14 (36.8) | 11 (28.9) |
| B | 29 | 1 (3.4) | 4 (13.8) | 24 (82.8) | 0 (0.0) | 6 (20.7) | 23 (79.3) | 1 (3.4) | 2 (6.9) | 26 (89.7) | 1 (3.4) | 5 (17.2) | 23 (79.3) | 3 (10.3) | 2 (6.9) | 24 (82.8) |
| C1 | 17 | 1 (5.9) | 2 (11.8) | 14 (82.4) | 1 (5.9) | 3 (17.6) | 13 (76.5) | 0 (0.0) | 5 (29.4) | 12 (70.6) | 0 (0.0) | 2 (11.8) | 15 (88.2) | 2 (11.8) | 8 (47.1) | 7 (41.2) |
| C2 | 8 | 0 (0.0) | 1 (12.5) | 7 (87.5) | 0 (0.0) | 1 (12.5) | 7 (87.5) | 1 (12.5) | 2 (25.0) | 5 (62.5) | 0 (0.0) | 4 (50.0) | 4 (50.0) | 1 (12.5) | 3 (37.5) | 4 (50.0) |
| D | 4 | 0 (0.0) | 2 (50.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | 4 (100.0) | 0 (0.0) | 2 (50.0) | 2 (50.0) | 1 (25.0) | 0 (0.0) | 3 (75.0) | 1 (25.0) | 0 (0.0) | 3 (75.0) |
NS; not significant.
Figure 1.
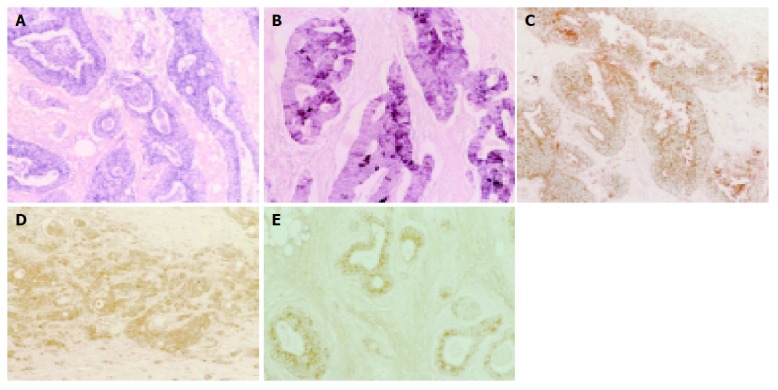
Positive staining in cytoplasm of colorectal adenocarcinoma cells shown by immunohistochemical staining of Ties and Angs. Immunoalkaline phosphatase staining; Tie-1 (A), Tie-2 (B) and DAB staining; Ang-1 (C), Ang-2 (D), and Ang-4 (E). (magnification: ×100, each).
Table 2.
Ductal infiltrations, lymph node metastasis and Tie-1, 2 and Ang-1, 2 and 4 expressions in invasive colorectal adenocarcinoma (n = 76), n (%).
| n |
Tie-1 |
Tie-2 |
Ang-1 |
Ang-2 |
Ang-4 |
|||||||||||
| - | + | ++ | - | + | ++ | - | + | ++ | - | + | ++ | - | + | ++ | ||
| Invasive carcinoma | 76 | 5 (6.6) | 15 (19.7) | 56 (73.7) | 2 (2.6) | 18 (23.7) | 56 (73.7) | 6 (7.9) | 17 (22.4) | 53 (69.7) | 4 (5.3) | 17 (22.4) | 55 (72.4) | 13 (17.1) | 19 (25.0) | 44 (57.9) |
| Desmoplastic stromal reaction | NS | P = 0.039383 | NS | NS | NS | |||||||||||
| Slight | 13 | 2 (15.4) | 2 (15.4) | 9 (69.2) | 1 (7.7) | 5 (38.5) | 7 (53.8) | 4 (30.8) | 2 (15.4) | 7 (53.8) | 1 (7.7) | 4 (30.8) | 8 (61.5) | 4 (30.8) | 0 (0.0) | 9 (69.2) |
| Moderate | 47 | 2 (4.3) | 11 (23.4) | 34 (72.3) | 1 (2.1) | 11 (23.4) | 35 (74.5) | 2 (4.3) | 12 (25.5) | 33 (70.2) | 3 (6.4) | 10 (21.3) | 34 (72.3) | 8 (17.0) | 15 (31.9) | 24 (51.1) |
| Extensive | 16 | 1 (6.3) | 2 (12.5) | 13 (81.3) | 0 (0.0) | 2 (12.5) | 14 (87.5) | 0 (0.0) | 3 (18.8) | 13 (81.3) | 0 (0.0) | 3 (18.8) | 13 (81.3) | 1 (6.3) | 4 (25.0) | 11 (68.8) |
| Venous invasion | NS | P = 0.005992 | NS | P = 0.018168 | NS | |||||||||||
| Present | 35 | 1 (2.9) | 7 (20.0) | 27 (77.1) | 0 (0.0) | 4 (11.4) | 31 (88.6) | 2 (5.7) | 6 (17.1) | 27 (77.1) | 1 (2.9) | 4 (11.4) | 30 (85.7) | 5 (14.3) | 9 (25.7) | 21 (60.0) |
| Absent | 41 | 4 (9.8) | 8 (19.5) | 29 (70.7) | 2 (4.9) | 14 (34.1) | 25 (61.0) | 4 (9.8) | 11 (26.8) | 26 (63.4) | 3 (7.3) | 13 (31.7) | 25 (61.0) | 8 (19.5) | 10 (24.4) | 23 (56.1) |
| Lymphatic invasion | P = 0.033356 | P = 0.001326 | P = 0.039066 | NS | NS | |||||||||||
| Present | 60 | 1 (1.7) | 12 (20.0) | 47 (78.3) | 0 (0.0) | 11 (18.3) | 49 (81.7) | 3 (5.0) | 12 (20.0) | 45 (75.0) | 2 (3.3) | 13 (21.7) | 45 (75.0) | 7 (11.7) | 16 (26.7) | 37 (61.7) |
| Absent | 16 | 4 (25.0) | 3 (18.8) | 9 (56.3) | 2 (12.5) | 7 (43.8) | 7 (43.8) | 3 (18.8) | 5 (31.3) | 8 (50.0) | 2 (12.5) | 4 (25.0) | 10 (62.5) | 6 (37.5) | 3 (18.8) | 7 (43.8) |
| Lymph node metastasis | NS | NS | NS | NS | NS | |||||||||||
| Present | 27 | 1 (3.7) | 4 (14.8) | 22 (81.5) | 1 (3.7) | 4 (14.8) | 22 (81.5) | 1 (3.7) | 8 (29.6) | 18 (66.7) | 1 (3.7) | 6 (22.2) | 20 (74.1) | 4 (14.8) | 11 (40.7) | 12 (44.4) |
| Absent | 49 | 4 (8.2) | 11 (22.4) | 34 (69.4) | 1 (2.0) | 14 (28.6) | 34 (69.4) | 5 (10.2) | 9 (18.4) | 35 (71.4) | 3 (6.1) | 11 (22.4) | 35 (71.4) | 9 (18.4) | 8 (16.3) | 32 (65.3) |
NS; not significant.
DISCUSSION
Tyrosine-kinase receptors (TKRs) are key molecules in signaling pathways leading to growth and differentiation of normal and carcinoma cells[22,23]. The attenuation of subcellular tyrosine phosphorylation has been reported to induce the differentiated phenotypes in human colorectal cancer cells[24]. Aberrant expression of tyrosine kinases, as reflected by aberrant tyrosine phosphorylation in gastric cancer cells, has been reported[25]. Subversion of different signal pathways may contribute to the progression of different types of colorectal cancer.
Tie-1 and Tie-2 were highly expressed in cancer tissues in this study. One report suggested that Tie-1 expression was restricted to endothelial and hematopoietic cells[26]. However, this study showed that Tie-1 and Tie-2 were expressed in colorectal adenocarcinoma cells as well. The expressed Tie-1 and Tie-2 proteins were localized in the cytoplasm of cancer cells, and the invasive front and/or the peripheral parts of the primary tumor were intensely stained compared to the superficial and central parts of the tumor in almost all cases of invasive carcinomas. The expression of Tie-1 in gastric cancer cells was shown to be associated with reduced survival of the patients and served as an independent predictor of survival[27]. In this study we found some correlations between the expression of Ties and histological differentiation, depth of invasion, Duke’s classification and lymphatic invasion of colorectal carcinoma.
In the category of vasculogenesis, a new family of growth factors, termed angiopoietins that are specific for the vascular endothelium has been recently identified[13,15,16,28]. The specificity of the Angs for the vascular endothelium resulted from the restricted distribution of the angiopoietin receptor, Tie-2, to these cells[4,5]. All known angiopoietins bind to Tie-2, but it is still unclear as to whether they use the closely related receptor Tie-1. Transgenic overexpression of Ang-1 could lead to striking hypervascularization[29]. In contrast, transgenic overexpression of Ang-2, a natural competitor of Ang-1 for the Tie-2 receptor, seemed to severely disturb vessel stabilization and remodeling[15]. Ang-3 and Ang-4 were more recently described members of this family that seem to represent the mouse and human counterparts, respectively, of the same genetic locus[28]. Ang-4 seemed to act as an agonist and is expressed at high levels in the lungs[28].
Although the expressions of Ties and Angs have been reported in angiogenesis[30], the expression of Angs in carcinoma cells has led us to consider the possibility that Ang might be involved in the growth or progression of tumor cells. One report showed that the colon carcinoma cell line, transfected with Ang-1 and Ang-2 expression vector, revealed rapid tumor growth[31]. In this study, both Angs and Ties were expressed simultaneously in carcinoma cells. Therefore, tumor cells should respond to the Angs in an autocrine or paracrine fashion to promote the growth of tumors. Nevertheless, more studies are required to elucidate this potential regulation of signaling pathways by Angs in colorectal carcinoma cells.
Statistical analyses of our data showed a correlation only between Tie-1 and Tie-2 and Ang-1 and Ang-4 expressions and histological differentiations. Poorly differentiated adenocarcinomas were strongly positive for each protein in the cytoplasm of carcinoma cells. In gastric cancer, some reports have described a correlation between the expressions of Ties or Angs and histological differentiations[31-33], but these reports showed variable results. The present study is the only report on correlation between expressions of Ties and Angs and differentiation of colorectal carcinomas. However, more studies are needed to clarify the correlation between expressions of Ties and Angs and histopathological differentiation.
Prognosis in patients with colorectal cancer has conventionally been determined by the extent of the primary tumor and the presence or absence of metastasis[1]. However, the mechanism of invasion and metastasis of colorectal carcinoma has not been fully elucidated. In our study, Ties and Angs were expressed in normal colorectal epithelium, although these expressions were weak (data not shown). Ties and Angs were also expressed in colorectal adenomas (Table 1). Some reports showed that the expressions of Ties and Angs were correlated with tumor invasion or prognosis of patients with gastric carcinoma[27,32]. However, in colorectal carcinoma, there was no report of the correlation between expressions of Ties and Angs and prognostic factors. In our study, the expression of Ties and Angs correlated significantly with the depth of tumor invasion, Duke’s classification, venous invasion, lymphatic invasion. It showed no correlation between expressions of Ties and Angs and lymph node metastasis. Further investigations are thus required to establish the details in the correlation between expressions of Ties and Angs and tumor progression and metastasis to lymph nodes in colorectal carcinoma.
Tumor desmoplasia is a common feature in several malignant human tumors, and it has been reported that a well-marked desmoplastic stromal reaction was associated with a poorer prognosis in colorectal cancer[34]. In this study, many cases of colorectal carcinoma expressed Ties and Angs in the cytoplasm of carcinoma cells. However, fibrous stromal cells did not show high expression of Ties and Angs (data not shown). Tie-2 was significantly correlated with the extent of fibrous stromal tissue. Our results suggest that the expression of Tie-2 protein may be used as one of the prognostic factors in colorectal cancer.
In previous reports, Angs were shown to be mainly produced by endothelial cells and pericites, and their receptor, Tie-2, was also expressed in endothelial cells[35]. Angs were expressed in endothelial cells of tumor-associated vessels[36], and Ang-1 induced angiogenesis[13,14]. In this study, Ties and Angs were expressed in vessel cells (data not shown), and the expressions of Tie-2 and Ang-2 correlated with venous invasion. These results suggest that Tie-2 and Ang-2 produced by tumor cells in human colorectal adenocarcinoma induce angiogenesis, which facilitates tumor nutrition. New vessels might be used to make metastasis easy to other organs.
This study demonstrates that Ties and Angs are highly expressed in human colorectal adenocarcinoma cells. It suggests that the Tie-Ang receptor-ligand complex is one of the factors involved in cellular differentiation and progression of human colorectal adenocarcinoma.
ACKNOWLEDGEMENTS
We are grateful to Mr. Toshiyuki Kawada for his excellent immunohistochemical assistance.
References
- 1.Newland RC, Dent OF, Lyttle MN, Chapuis PH, Bokey EL. Pathologic determinants of survival associated with colorectal cancer with lymph node metastases. A multivariate analysis of 579 patients. Cancer. 1994;73:2076–2082. doi: 10.1002/1097-0142(19940415)73:8<2076::aid-cncr2820730811>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Steinberg SM, Barwick KW, Stablein DM. Importance of tumor pathology and morphology in patients with surgically resected colon cancer. Findings from the Gastrointestinal Tumor Study Group. Cancer. 1986;58:1340–1345. doi: 10.1002/1097-0142(19860915)58:6<1340::aid-cncr2820580626>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 3.Mustonen T, Alitalo K. Endothelial receptor tyrosine kinases involved in angiogenesis. J Cell Biol. 1995;129:895–898. doi: 10.1083/jcb.129.4.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maisonpierre PC, Goldfarb M, Yancopoulos GD, Gao G. Distinct rat genes with related profiles of expression define a TIE receptor tyrosine kinase family. Oncogene. 1993;8:1631–1637. [PubMed] [Google Scholar]
- 5.Sato TN, Qin Y, Kozak CA, Audus KL. Tie-1 and tie-2 define another class of putative receptor tyrosine kinase genes expressed in early embryonic vascular system. Proc Natl Acad Sci USA. 1993;90:9355–9358. doi: 10.1073/pnas.90.20.9355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dumont DJ, Gradwohl G, Fong GH, Puri MC, Gertsenstein M, Auerbach A, Breitman ML. Dominant-negative and targeted null mutations in the endothelial receptor tyrosine kinase, tek, reveal a critical role in vasculogenesis of the embryo. Genes Dev. 1994;8:1897–1909. doi: 10.1101/gad.8.16.1897. [DOI] [PubMed] [Google Scholar]
- 7.Sato TN, Tozawa Y, Deutsch U, Wolburg-Buchholz K, Fujiwara Y, Gendron-Maguire M, Gridley T, Wolburg H, Risau W, Qin Y. Distinct roles of the receptor tyrosine kinases Tie-1 and Tie-2 in blood vessel formation. Nature. 1995;376:70–74. doi: 10.1038/376070a0. [DOI] [PubMed] [Google Scholar]
- 8.Wong AL, Haroon ZA, Werner S, Dewhirst MW, Greenberg CS, Peters KG. Tie2 expression and phosphorylation in angiogenic and quiescent adult tissues. Circ Res. 1997;81:567–574. doi: 10.1161/01.res.81.4.567. [DOI] [PubMed] [Google Scholar]
- 9.Koblizek TI, Runting AS, Stacker SA, Wilks AF, Risau W, Deutsch U. Tie2 receptor expression and phosphorylation in cultured cells and mouse tissues. Eur J Biochem. 1997;244:774–779. doi: 10.1111/j.1432-1033.1997.00774.x. [DOI] [PubMed] [Google Scholar]
- 10.Peters KG, Coogan A, Berry D, Marks J, Iglehart JD, Kontos CD, Rao P, Sankar S, Trogan E. Expression of Tie2/Tek in breast tumour vasculature provides a new marker for evaluation of tumour angiogenesis. Br J Cancer. 1998;77:51–56. doi: 10.1038/bjc.1998.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin P, Polverini P, Dewhirst M, Shan S, Rao PS, Peters K. Inhibition of tumor angiogenesis using a soluble receptor establishes a role for Tie2 in pathologic vascular growth. J Clin Invest. 1997;100:2072–2078. doi: 10.1172/JCI119740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin P, Buxton JA, Acheson A, Radziejewski C, Maisonpierre PC, Yancopoulos GD, Channon KM, Hale LP, Dewhirst MW, George SE, et al. Antiangiogenic gene therapy targeting the endothelium-specific receptor tyrosine kinase Tie2. Proc Natl Acad Sci USA. 1998;95:8829–8834. doi: 10.1073/pnas.95.15.8829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis S, Aldrich TH, Jones PF, Acheson A, Compton DL, Jain V, Ryan TE, Bruno J, Radziejewski C, Maisonpierre PC, et al. Isolation of angiopoietin-1, a ligand for the TIE2 receptor, by secretion-trap expression cloning. Cell. 1996;87:1161–1169. doi: 10.1016/s0092-8674(00)81812-7. [DOI] [PubMed] [Google Scholar]
- 14.Witzenbichler B, Maisonpierre PC, Jones P, Yancopoulos GD, Isner JM. Chemotactic properties of angiopoietin-1 and -2, ligands for the endothelial-specific receptor tyrosine kinase Tie2. J Biol Chem. 1998;273:18514–18521. doi: 10.1074/jbc.273.29.18514. [DOI] [PubMed] [Google Scholar]
- 15.Maisonpierre PC, Suri C, Jones PF, Bartunkova S, Wiegand SJ, Radziejewski C, Compton D, McClain J, Aldrich TH, Papadopoulos N, et al. Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science. 1997;277:55–60. doi: 10.1126/science.277.5322.55. [DOI] [PubMed] [Google Scholar]
- 16.Suri C, Jones PF, Patan S, Bartunkova S, Maisonpierre PC, Davis S, Sato TN, Yancopoulos GD. Requisite role of angiopoietin-1, a ligand for the TIE2 receptor, during embryonic angiogenesis. Cell. 1996;87:1171–1180. doi: 10.1016/s0092-8674(00)81813-9. [DOI] [PubMed] [Google Scholar]
- 17.Jass SR, Sobin LH. Histological Typing of Intestinal Tumours. World Health Organization (2nd ed) Berlin, Germany: Springer-Verlag; 1989. [Google Scholar]
- 18.Beahrs OH, Henson DE, Hutter RVP (eds) Mannual for Staging of Cancer (4th ed) Philadelphia: JB Lippincott;; 1992. pp. 69–73. [Google Scholar]
- 19.Jass JR, Atkin WS, Cuzick J, Bussey HJ, Morson BC, Northover JM, Todd IP. The grading of rectal cancer: historical perspectives and a multivariate analysis of 447 cases. Histopathology. 1986;10:437–459. doi: 10.1111/j.1365-2559.1986.tb02497.x. [DOI] [PubMed] [Google Scholar]
- 20.Seefeld PH, Bargen JA. The spread of cancer of the rectum: Invasion of the lymphatics, veins and nerves. Ann Surg. 1943;118:76–90. doi: 10.1097/00000658-194311810-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Talbot IC, Ritchie S, Leighton M, Hughes AO, Bussey HJ, Morson BC. Invasion of veins by carcinoma of rectum: method of detection, histological features and significance. Histopathology. 1981;5:141–163. doi: 10.1111/j.1365-2559.1981.tb01774.x. [DOI] [PubMed] [Google Scholar]
- 22.Marshall CJ. Specificity of receptor tyrosine kinase signaling: transient versus sustained extracellular signal-regulated kinase activation. Cell. 1995;80:179–185. doi: 10.1016/0092-8674(95)90401-8. [DOI] [PubMed] [Google Scholar]
- 23.Lin W, Kao HW, Robinson D, Kung HJ, Wu CW, Chen HC. Tyrosine kinases and gastric cancer. Oncogene. 2000;19:5680–5689. doi: 10.1038/sj.onc.1203924. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz B, Lamprecht SA, Polak-Charcon S, Niv Y, Kim YS. Induction of the differentiated phenotype in human colon cancer cell is associated with the attenuation of subcellular tyrosine phosphorylation. Oncol Res. 1995;7:277–287. [PubMed] [Google Scholar]
- 25.Takeshima E, Hamaguchi M, Watanabe T, Akiyama S, Kataoka M, Ohnishi Y, Xiao HY, Nagai Y, Takagi H. Aberrant elevation of tyrosine-specific phosphorylation in human gastric cancer cells. Jpn J Cancer Res. 1991;82:1428–1435. doi: 10.1111/j.1349-7006.1991.tb01816.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hashiyama M, Iwama A, Ohshiro K, Kurozumi K, Yasunaga K, Shimizu Y, Masuho Y, Matsuda I, Yamaguchi N, Suda T. Predominant expression of a receptor tyrosine kinase, TIE, in hematopoietic stem cells and B cells. Blood. 1996;87:93–101. [PubMed] [Google Scholar]
- 27.Lin WC, Li AF, Chi CW, Chung WW, Huang CL, Lui WY, Kung HJ, Wu CW. tie-1 protein tyrosine kinase: a novel independent prognostic marker for gastric cancer. Clin Cancer Res. 1999;5:1745–1751. [PubMed] [Google Scholar]
- 28.Valenzuela DM, Griffiths JA, Rojas J, Aldrich TH, Jones PF, Zhou H, McClain J, Copeland NG, Gilbert DJ, Jenkins NA, et al. Angiopoietins 3 and 4: diverging gene counterparts in mice and humans. Proc Natl Acad Sci USA. 1999;96:1904–1909. doi: 10.1073/pnas.96.5.1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suri C, McClain J, Thurston G, McDonald DM, Zhou H, Oldmixon EH, Sato TN, Yancopoulos GD. Increased vascularization in mice overexpressing angiopoietin-1. Science. 1998;282:468–471. doi: 10.1126/science.282.5388.468. [DOI] [PubMed] [Google Scholar]
- 30.Yancopoulos GD, Davis S, Gale NW, Rudge JS, Wiegand SJ, Holash J. Vascular-specific growth factors and blood vessel formation. Nature. 2000;407:242–248. doi: 10.1038/35025215. [DOI] [PubMed] [Google Scholar]
- 31.Ahmad SA, Liu W, Jung YD, Fan F, Reinmuth N, Bucana CD, Ellis LM. Differential expression of angiopoietin-1 and angiopoietin-2 in colon carcinoma. A possible mechanism for the initiation of angiogenesis. Cancer. 2001;92:1138–1143. doi: 10.1002/1097-0142(20010901)92:5<1138::aid-cncr1431>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 32.Etoh T, Inoue H, Tanaka S, Barnard GF, Kitano S, Mori M. Angiopoietin-2 is related to tumor angiogenesis in gastric carcinoma: possible in vivo regulation via induction of proteases. Cancer Res. 2001;61:2145–2153. [PubMed] [Google Scholar]
- 33.Nakayama T, Yoshizaki A, Kawahara N, Ohtsuru A, Wen CY, Fukuda E, Nakashima M, Sekine I. Expression of Tie-1 and 2 receptors, and angiopoietin-1, 2 and 4 in gastric carcinoma; immunohistochemical analyses and correlation with clinicopathological factors. Histopathology. 2004;44:232–239. doi: 10.1111/j.0309-0167.2004.01817.x. [DOI] [PubMed] [Google Scholar]
- 34.Halvorsen TB, Seim E. Association between invasiveness, inflammatory reaction, desmoplasia and survival in colorectal cancer. J Clin Pathol. 1989;42:162–166. doi: 10.1136/jcp.42.2.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis S, Yancopoulos GD. The angiopoietins: Yin and Yang in angiogenesis. Curr Top Microbiol Immunol. 1999;237:173–185. doi: 10.1007/978-3-642-59953-8_9. [DOI] [PubMed] [Google Scholar]
- 36.Stratmann A, Risau W, Plate KH. Cell type-specific expression of angiopoietin-1 and angiopoietin-2 suggests a role in glioblastoma angiogenesis. Am J Pathol. 1998;153:1459–1466. doi: 10.1016/S0002-9440(10)65733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


