Abstract
AIM: To analyze the spectrum and risk factors of gastroesophageal reflux disease (GERD) based on presenting symptoms and endoscopic findings.
METHODS: A cross-sectional survey in a cluster random sample was conducted from November 2004 to June 2005 using a validated Chinese version Reflux Disease Questionnaire (RDQ) and other items recording the demographic characteristics and potential risk factors for GERD. Subjects were defined as having GERD symptoms according to the RDQ score (> 12). All subjects were endoscopied and the definition and severity of erosive esophagitis were evaluated by Los Angeles classification. The statistical analysis was performed with SPSS13.0 programs.
RESULTS: Of 2231 recruited participants, 701 (31.40%) patients were diagnosed as having GERD while 464 (20.80%) patients had objective findings of reflux esophagitis (RE). Of those 464 patients, only 291 (13.00%) were reported as subjects with GERD symptoms. A total of 528 (23.70%) patients were found to have GERD symptoms, including 19.50% patients with grade A or B reflux esophagitis, 0.90% with grade C and 0.40% with grade D. On multivariate analysis, old age, male, moderate working burden, divorced/widowed and strong tea drinking remained as significant independent risk factors for erosive esophagitis. Meanwhile, routine usage of greasy food and constipation were considered as significant independent risk factors for non-erosive reflux disease (NERD).
CONCLUSION: GERD is one of the common GI diseases with a high occurrence rate in China and its main associated factors include sex, anthropometrical variables and sociopsychological characteristics.
Keywords: Gastroesophageal reflux disease, Reflux esophagitis, Non-erosive reflux disease, Prevalence, Risk factors, Endoscopy
INTRODUCTION
Gastroesophageal reflux disease (GERD) is a common disorder with a high incidence rate of 10%-38% of adults in the Western population occurring at least once a week[1,2]. The prevalence of GERD has been increasing[3]. The diagnosis and treatment of GERD are therefore, important because the disease, in addition to the highly disturbing typical symptoms, has a series of known consequences. The presence of GERD may affect the patients’ quality of life[4], decrease functional activity[5], increase the economic burden[6] and the risk of esophageal carcinoma in the cases of Barrett’s esophagus[7]. With an emphasis on morphological diagnosis, endoscopy has become a major tool to assess the final consequences of GERD, which is especially useful for population-based screening.
Although many investigators have reported the prevalence of erosive esophagitis[8], the prevalence of NERD has not been investigated in China. Our study was designed to analyze the spectrum of GERD subjects based on presenting symptoms and endoscopic findings. In order to determine the risk factors for such disease in outpatients from Zhejiang Province of East China, a cross-sectional survey in a cluster random sample was conducted from November 2004 to June 2005.
MATERIALS AND METHODS
Subjects
From November 2004 to June 2005, outpatients visiting departments of medicine in 10 hospitals from island, mountainous area, plain, city, countryside and suburb, in the Zhejiang Province of East China were recruited to the study. Subjects were excluded if they were not permanent inhabitants of East China, less than 18 years old, and had major psychotic episodes, mental retardation, dementia, severe visual or hearing abnormalities or other illnesses that might render them unable to complete the questionnaire or undergo the endoscopy (e.g. stroke). Excluding criteria also contained a history of peptic ulcer disease and receiving proton pump inhibitors or H2-blockers over the preceding 2 wk. A total of 2278 individuals who had GI endoscopy were recruited, of which 2231 were eligible with a response rate of 97.9%.
Questionnaire
The gastroesophageal reflux questionnaire, a self-report instrument that to evaluate reflux-associated symptoms during the prior month, included the Chinese version of the Reflux Diagnostic Questionnaire (RDQ)[9] and items concerning the demographic characteristics and probable risk factors for GERD. It comprised the following parts: (1) General information: gender and age. (2) The Chinese version of the Reflux Diagnostic Questionnaire (RDQ): its framework of the RDQ was based on a validated questionnaire previously published[3]. The Chinese version of the RDQ was designed to measure symptoms suggestive of GERD appearing during the previous month. The intraclass correlation coefficient of the Chinese version of the RDQ was 0.9, thus it was validated and found to be a useful screening test for GERD-associated symptoms in China[9]. The symptoms suggestive of GERD in the RDQ included heartburn, substernal chest pain, acid eructation and food regurgitation. The following definitions were used to identify the symptoms in the RDQ: (1) heartburn, a burning sensation located beneath the sternum; (2) substernal chest pain: any pain felt inside in the chest but not including heartburn or any pain that is primarily originated from the abdomen; (3) acid regurgitation, a bitter- or sour-tasting fluid coming into the throat or mouth; and (4) food regurgitation, unpleasant movement of material upwards from the stomach but not vomit. Each symptom was scored according to the frequency and severity (5-point scale). The highest score for one subject was 40. The frequency was measured according to the following scale: 0, no symptom in the past month; 1, less than once a week; 2, once a week; 3, two to three days a week; 4, four to five days a week; and 5, almost daily. Symptom severity was assessed on the following scale:0, none; 1, very mild (symptoms can be easily ignored unless reminded of them); 2, mild (between 1 and 3); 3, moderate (symptoms are obvious and sufficient to influence normal activities, and occasionally need treatment); 4, severe (between 3 and 5); and 5, very severe (symptoms are obvious and sufficient to influence normal activities, and need long-term medication).
The Chinese version of the RDQ has been tested in a multicenter study including 10 hospitals in China. The specificity and sensitivity of the RDQ were evaluated by comparing the results with those of upper gastrointestinal endoscopy and esophageal 24-h pH monitoring. The RDQ score correlated positively with the severity of reflux esophagitis. Esophageal pH monitoring showed that patients with abnormal RDQ scores had higher Demeester scores than those with normal RDQ scores (20.18 vs 16.84). Taking 12 as the parameter for the threshold of RDQ score for GERD-associated symptoms, the study group obtained the maximal Youden index, the area under the receiver operating characteristic curve (ROC), was 0.71, the true positive diagnostic rate was 88.07% and the true negative diagnostic rate was 68.42% with a sensitivity of 94.12% and specificity of 50.00%. The subject was defined as a patient with GERD symptoms if his/her RDQ score was higher than 12[9]. Probable risk factors for GERD symptoms included life status: working burden, marital status (married, single, divorced/widowed), constipation, dietary and other personal habits: excessive consumption of acidic beverages, coffee, strong tea, spicy food, greasy food, sweet food, cigarette and alcohol. Definitions: heavy smoker (more than 20 cigarettes per day), excessive alcohol (≤ 210 g of alcohol per week), constipation (frequently occurred during last 12 mo), routine use of coffee (more than 100 mL per day on average), acidic beverages and strong tea (more than 200 mL per day on average), dietary habits (taking the food mentioned above more than one time per day on average). The questions about probable risk factors, extra esophageal symptoms and accompanying diseases were all binary: yes or no.
Upper gastrointestinal endoscopy
Patients were examined for the presence of reflux esophagitis. Diagnosis and classification of reflux esophagitis were based on the Los Angeles classification[8]. Barrett’s esophagus was diagnosed when columnar epithelium was seen to extend the Z line and confirmed histologically that showed specialized intestinal metaplasia. These criteria were consistently applied and endoscopic diagnosis was confirmed by either of the authors who were present during each endoscopic procedure. Patients who returned for endoscopic reassessment for any reason were excluded from the analysis to prevent duplication of cases.
Survey design and response rate
The cross-sectional survey in a cluster random sample was conducted from November 2004 to June 2005. The present study was based on a standard protocol including routine internal medicine counseling, endoscopy, and a self-reported questionnaire. Consecutive numbers were assigned to each registered subject and a 1:10 ratio of sample was selected using random number tables. All subjects completed the detailed questionnaire before endoscopy. Confirmed consent was obtained from all patients before the questionnaire was administered. All subjects were given the questionnaire.
A subject with GERD symptoms was defined according to the RDQ score (> 12). Patients who were suspicious of having GERD but without evidence of reflux esophagitis (RE) were diagnosed as having NERD. GERD was diagnosed based on the presence of reflux esophagitis and/or the presence of predominant reflux symptoms. Because the survey explanation is made according to the RDQ score, all the questions in the RDQ must be answered without omission. In this study, a total of 2231 eligible subjects were recruited.
Ethics
The study was approved by the Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University.
Statistical analysis
The database was established with Epidata3.0. Statistical analysis was performed with SPSS13.0 programs. Univariate analysis was performed using χ2 test for categorical variables. Univariate and multivariate logistic regression models were used to identify the potential risk factors of GERD, NERD and reflux esophagitis. The probable risk factors for GERD symptoms were selected by the univariate logistic regression, including life status (labor burden, marital status), dietary and other personal habits such as routine usage of acidic beverage, spicy food, greasy food, coffee, strong tea, sweet food, cigarette and alcohol, and constipation. All risk factors associated with GERD symptoms on univariate analysis were modeled using multivariate forward stepwise logistic regression analysis. To find the best model, a forward elimination stepwise procedure was carried out in a way that the factor would be brought into the analysis if the corresponding P value was less than 0.5. A P value ≥ 0.05 was considered statistically significant and all P values were obtained by two-tailed examination.
RESULTS
Sample characteristics
A total of 2231 (56.6% male, 43.4% female) outpatients aged from 18 to 90 years (a median age of 43 years) were recruited to this study.
Prevalence of GERD, reflux esophagitis and NERD
As shown in Figure 1, 701 (31.40%) patients were diagnosed as having GERD and 464 (20.80%) patients were found to have objective findings of reflux esophagitis. Of the 464 patients, only 291 (13.00%) presented with GERD symptoms. Among the 2231 subjects, 528 (23.70%) presented with GERD symptoms.
Figure 1.
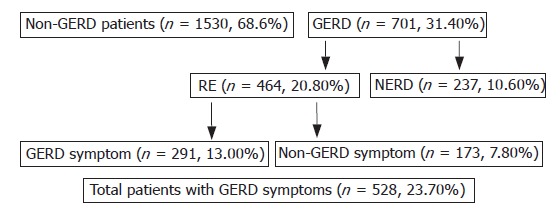
Diagnosis of gastroesophageal reflux disease (GERD) based on symptoms and presence of reflux esophagitis (RE).
Distribution of different grades and complications of reflux esophagitis
As shown in Table 1, 435 patients (19.50%) had grade A or B reflux esophagitis while 20 patients had grade C (0.90%) and 9 had grade D (0.40%). The complications of reflux esophagitis are shown in Table 2. The most frequent complication is esophagorrhagia (1.82%).
Table 1.
Grading of reflux esophagitis in 2278 patients
| Grade | Total number | % |
| None | 1767 | 79.20 |
| A | 333 | 14.93 |
| B | 102 | 4.57 |
| C | 20 | 0.90 |
| D | 9 | 0.40 |
| Total | 2231 | 100.00 |
Table 2.
Complications of reflux esophagitis
| Total number | % | |
| Barrett’s esophagus | No 1190 | 98.76 |
| Yes 15 | 1.24 | |
| Esophageal stenosis | No 1191 | 98.76 |
| Yes 15 | 1.24 | |
| Esophagorrhagia | No 1186 | 98.18 |
| Yes 22 | 1.82 |
Comparison between upper gastrointestinal endoscopy and RDQ
As shown in Tables 3 and 4, there is significant difference between the two investigations. The Kappa value was 0.47, P = 0.000, demonstrating no predominant consistency between the two diagnostic methods.
Table 3.
Comparison between upper gastrointestinal endoscopy and RDQ (χ2 test)
| RDQ |
Endoscopy |
P value | |
| Negative | Positive | ||
| Negative | 1530 | 173 | 0.002 |
| Positive | 237 | 291 | |
P = 0.002, there is significant statistical difference between the two investigations.
Table 4.
Comparison between upper gastrointestinal endoscopy and RDQ (Wilcoxon rank-sum test)
| RDQ |
Endoscopy |
Total | U value | P value | ||||
| Negative | A | B | C | D | ||||
| Negative | 1530 | 131 | 34 | 5 | 3 | 1703 | ||
| Positive | 237 | 202 | 68 | 15 | 6 | 528 | 3.60 | 0.000 |
| Total | 1767 | 333 | 102 | 20 | 9 | 2231 | ||
Risk factors in GERD and non-GERD patients
The prevalence of various variables in GERD patients compared to non-GERD patients is shown in Table 5. On univariate analysis, age > 65, male, moderate working burden, divorced/widowed, excessive eating, greasy food, spicy food, strong tea, smoking, alcohol, and constipation were found to be significant participants. On multivariate analysis, old age (OR, 0.57; β, -0.57; 95% CI, 0.40-0.80), male (OR, 0.78; β, -0.25; 95% CI, 0.61-1.00), moderate working burden (OR, 0.58; β, -0.54; 95% CI, 0.39-0.87), divorced/widowed (OR, 1.82; β, 0.60; 95% CI, 1.27-2.60), greasy food (OR, 0.75; β, -0.29; 95% CI, 0.60-0.95), strong tea (OR, 0.67; β, -0.40; 95% CI, 0.50-0.89) remained as significant independent risk factors.
Table 5.
Association between variables determined using univariate analysis: GERD (n = 701) vs non-GERD (n = 1530) patients
| Variables | GERD n (%) | P value | OR |
Univariate (95% CI) |
|
| Low | High | ||||
| Age (yr) | |||||
| > 65 | 106/239 (44.40) | < 0.0001 | 0.53 | 0.41 | 0.70 |
| ≤ 65 | 595/1992 (29.90) | ||||
| Gender | |||||
| Male | 439/1263 (34.80) | < 0.0001 | 0.7 | 0.58 | 0.84 |
| Female | 262/968 (27.10) | ||||
| Working burden | |||||
| Heavy | 64/147 (43.50) | 0.694 | 1.04 | 0.86 | 1.27 |
| Moderate | 299/975 (30.70) | 0.004 | 0.6 | 0.42 | 0.85 |
| Mild | 282/895 (31.50) | ||||
| Marital status | |||||
| Divorced/ widowed | 6/14 (42.90) | < 0.0001 | 2.05 | 1.49 | 2.82 |
| Single | 52/261 (19.90) | 0.478 | 0.68 | 0.24 | 1.97 |
| Married | 592/1752 (33.80) | ||||
| Excessive eating | |||||
| Yes | 245/704 (34.80) | 0.009 | 0.77 | 0.63 | 0.94 |
| No | 372/1276 (29.20) | ||||
| Routine intake of greasy food | |||||
| Yes | 231/618 (37.40) | < 0.0001 | 0.65 | 0.53 | 0.80 |
| No | 375/1347 (27.80) | ||||
| Routine intake of spicy food | |||||
| Yes | 196/512 (38.30) | < 0.0001 | 0.65 | 0.52 | 0.80 |
| No | 418/1463 (28.60) | ||||
| Routine intake of acidic beverage | |||||
| Yes | 118/358 (33.00) | 0.403 | 0.90 | 0.71 | 1.15 |
| No | 493/1606 (30.70) | ||||
| Routine intake of strong tea | |||||
| Yes | 149/343 (43.40) | < 0.0001 | 0.51 | 0.4 | 0.64 |
| No | 451/1613 (28.00) | ||||
| Routine intake of sweet food | |||||
| Yes | 225/683 (32.90) | 0.122 | 0.85 | 0.70 | 1.04 |
| No | 375/1269 (29.60) | ||||
| Heavy smoking | |||||
| Yes | 209/562 (37.20) | < 0.0001 | 0.68 | 0.55 | 0.83 |
| No | 407/1426 (28.50) | ||||
| Excessive alcohol | |||||
| Yes | 185/503 (36.80) | 0.002 | 0.71 | 0.57 | 0.88 |
| No | 434/1486 (29.20) | ||||
| Routine intake of coffee | |||||
| Yes | 26/77 (33.80) | 0.529 | 0.86 | 0.53 | 1.39 |
| No | 568/1869 (30.40) | ||||
| Constipation | |||||
| Yes | 122/316 (38.60) | 0.002 | 0.68 | 0.53 | 0.87 |
| No | 489/1641 (29.80) | ||||
GERD: Gastroesophageal reflux disease.
Risk factors in reflux esophagitis and non-GERD patients
The prevalence of various variables in reflux esophagitis patients compared to non-GERD patients is shown in Table 6. On univariate analysis, age > 65, male, moderate working burden, divorced/widowed, spicy food, strong tea, smoking, and alcohol were found to be significant. On multivariate analysis, old age (OR, 1.86; β, 0.62; 95% CI, 1.29-2.70), male (OR, 1.77; β, 0.57; 95% CI, 1.32-2.37), moderate working burden (OR, 1.91; β, 0.65; 95% CI, 1.22-2.97), divorced/widowed (OR, 0.55; β, -0.60; 95% CI, 0.36-0.85), strong tea (OR, 1.62; β, 0.48; 95% CI, 1.18-2.23) were considered as significant independent risk factors.
Table 6.
Association between variables determined using univariate analysis: Reflux esophagitis (n = 464) vs non-GERD (n = 1530) patients
| Variables | RE n (%) | P | OR |
Univariate (95% CI) |
|
| Low | High | ||||
| Age (yr) | |||||
| > 65 | 77/210 (36.70) | < 0.0001 | 2.09 | 1.55 | 2.82 |
| ≤ 65 | 387/1784 (21.70) | ||||
| Gender | |||||
| Male | 322/1146 (28.10) | < 0.0001 | 1.94 | 1.56 | 2.43 |
| Female | 142/848 (16.70) | ||||
| Working burden | |||||
| Heavy | 45/128 (35.20) | 0.353 | 0.90 | 0.71 | 1.13 |
| Moderate | 189/865 (21.80) | 0.006 | 1.74 | 1.17 | 2.59 |
| Mild | 191/804 (23.80) | ||||
| Marital status | |||||
| Divorced/ widowed | 5/13 (38.50) | < 0.0001 | 0.48 | 0.33 | 0.70 |
| Single | 34/243 (14.00) | 0.283 | 1.85 | 0.60 | 5.69 |
| Married | 392/1552 (25.30) | ||||
| Excessive eating | |||||
| Yes | 147/606 (24.30) | 0.346 | 1.12 | 0.89 | 1.41 |
| No | 259/1163 (22.30) | ||||
| Routine intake of greasy food | |||||
| Yes | 129/516 (25.00) | 0.090 | 1.23 | 0.97 | 1.57 |
| No | 263/1235 (21.30) | ||||
| Routine intake of spicy food | |||||
| Yes | 112/428 (26.20) | 0.037 | 1.31 | 1.02 | 1.69 |
| No | 283/1328 (21.30) | ||||
| Routine intake of acidic beverage | |||||
| Yes | 76/316 (24.10) | 0.593 | 1.08 | 0.81 | 1.44 |
| No | 326/1439 (22.70) | ||||
| Routine intake of strong tea | |||||
| Yes | 108/302 (35.80) | < 0.0001 | 2.28 | 1.74 | 2.98 |
| No | 284/1446 (19.60) | ||||
| Routine intake of sweet food | |||||
| Yes | 131/589 (22.20) | 0.769 | 0.97 | 0.76 | 1.22 |
| No | 265/1159 (22.90) | ||||
| Heavy smoking | |||||
| Yes | 153/506 (30.20) | < 0.0001 | 1.75 | 1.38 | 2.22 |
| No | 252/1271 (19.80) | ||||
| Excessive alcohol | |||||
| Yes | 124/442 (71.90) | 0.003 | 1.45 | 1.13 | 1.85 |
| No | 283/1335 (21.20) | ||||
| Routine intake of coffee | |||||
| Yes | 21/72 (29.20) | 0.167 | 1.44 | 0.86 | 2.43 |
| No | 371/1672 (22.20) | ||||
| Constipation | |||||
| Yes | 67/261 (25.70) | 0.275 | 1.18 | 0.87 | 1.60 |
| No | 336/1488 (22.60) | ||||
GERD: Gastroesophageal reflux disease.
Risk factors in NERD and non-GERD patients
The prevalence of various variables in NERD patients compared to non-GERD patients is shown in Table 7. On univariate analysis, divorced/widowed, excessive eating, greasy food, spicy food, strong tea and constipation were found to be significant. On multivariate analysis, greasy food (OR, 1.65; β, 0.50; 95% CI, 1.16-2.36) and constipation (OR, 1.51; β, 0.41; 95% CI, 1.01-2.25) were regarded as significant independent risk factors.
Table 7.
Association between variables determined using univariate analysis: NERD (n = 237) vs non-GERD (n = 1530) patients
| Variables | NERD n (%) | P | OR |
Univariate (95% CI) |
|
| Low | High | ||||
| Age (yr) | |||||
| > 65 | 29/162 (17.90) | 0.08 | 1.46 | 0.96 | 2.25 |
| ≤ 65 | 208/1605 (13.00) | ||||
| Gender | |||||
| Male | 117/941 (12.40) | 0.198 | 0.84 | 0.64 | 0.10 |
| Female | 120/826 (14.50) | ||||
| Working burden | |||||
| Heavy | 19/102 (8.60) | 0.547 | 1.10 | 0.81 | 1.48 |
| Moderate | 110/786 (14.00) | 0.119 | 1.54 | 0.89 | 2.66 |
| Mild | 91/704 (12.90) | ||||
| Marital status | |||||
| Divorced/ widowed | 1/9 (11.10) | 0.007 | 0.5 | 0.30 | 0.83 |
| Single | 18/227 (7.90) | 0.762 | 0.73 | 0.09 | 5.83 |
| Married | 200/1360 (14.70) | ||||
| Excessive eating | |||||
| Yes | 98/557 (17.60) | < 0.0001 | 1.71 | 1.27 | 2.29 |
| No | 113/1017 (11.10) | ||||
| Routine intake of greasy food | |||||
| Yes | 102/489 (20.90) | < 0.0001 | 2.29 | 1.71 | 3.07 |
| No | 112/1084 (10.30) | ||||
| Routine intake of spicy food | |||||
| Yes | 84/400 (21.00) | < 0.0001 | 2.06 | 1.52 | 2.78 |
| No | 135/1180 (11.40) | ||||
| Routine intake of acidic beverage | |||||
| Yes | 42/282 (14.900 | 0.41 | 1.17 | 0.81 | 1.68 |
| No | 167/1280 (13.00) | ||||
| Routine intake of strong tea | |||||
| Yes | 41/235 (17.40) | 0.043 | 1.47 | 1.01 | 2.14 |
| No | 167/1329 (12.60) | ||||
| Routine intake of sweet food | |||||
| Yes | 94/552 (17.00) | 0.001 | 1.67 | 1.24 | 2.25 |
| No | 110/1004 (11.00) | ||||
| Heavy smoking | |||||
| Yes | 56/409 (13.70) | 0.802 | 1.04 | 0.75 | 1.45 |
| No | 155/1174 (13.20) | ||||
| Excessive alcohol | |||||
| Yes | 61/379 (16.10) | 0.078 | 1.34 | 0.97 | 1.85 |
| No | 151/1203 (12.60) | ||||
| Routine intake of coffee | |||||
| Yes | 5/56 (8.90) | 0.36 | 0.65 | 0.26 | 1.64 |
| No | 197/1498 (13.20) | ||||
| Constipation | |||||
| Yes | 55/249 (22.10) | < 0.001 | 2.14 | 1.51 | 3.01 |
| No | 153/1305 (11.70) | ||||
GERD: Gastroesophageal reflux disease; NERD: Non-erosive reflux disease.
DISCUSSION
Traditionally, GERD is defined based on three major diagnostic parameters: (1) ambulatory 24-h esophageal pH monitoring; (2) upper gastrointestinal (GI) tract endoscopic examination for erosive esophagitis; and (3) clinical evaluation by physicians and clinical therapeutic treatment by acid suppression agents. The sensitivity of endoscopic examination is limited, as most patients with GERD do not have obvious mucosa injury. Therefore, most of their disease is categorized as non-erosive reflux disease (NERD). Ambulatory 24-h esophageal pH monitoring also has problems with sensitivity for the intermittent nature of symptoms and daily activities may disturb the placement of a pH probe. Endoscopy can be more easily applied to healthy participants than ambulatory 24-h esophageal pH monitoring. Furthermore, it is more objective in terms of finding reflux disease, which has been investigated in many previous studies. Erosive esophagitis is classified using the LA system, which appears to be the most unambiguous and simple method to apply. However, endoscopic examination alone can not rule out GERD or acid-induced epithelial injury. A variety of questionnaires designed for GERD clinical trials have been developed. The Gastrointestinal Symptom Rating Scale (GSRS)[10] comprises 15 items addressing five symptom clusters (gastroesophageal reflux, abdominal pain, indigestion, diarrhoea, and constipation). The GSRS used graded response categories from “none” to “very severe” without defining what these adjectives meant. This can produce subjective answers, reducing reliability and validity[11]. The “CarlssonDent Self-Administered Questionnaire (QUEST)”[12] had a good face validity, since it incorporated “word pictures” using simple English to describe symptoms of GERD. The GERQ[13] is a self-administered validated instrument that identifies the onset of GERD symptoms and grades the frequency and severity of symptoms over a prior year. It was a long questionnaire containing 80 questions, making it inconvenient for use in clinical trials.
The Chinese version of the Reflux Diagnostic Questionnaire (RDQ): Its framework of the RDQ was based on a validated questionnaire published before[3]. Shaw et al[3] found that the RDQ demonstrated validity and reliability and was responsive to change for reflux. The reliability coefficient of the RDQ scales ranged from 0.8 to 0.88, well beyond the acceptable level of 0.70. It was tested in the multicenters and found that it could accurately identify the presence of symptoms suggestive of GERD[9]. It was designed to measure GERD symptoms over the previous month, not the previous year. It was feasible to prevent the recall bias since McColl found that 1-mo was the maximum period over which patients could provide reliable data due to recall errors[14]. Four symptoms were included in the RDQ that may be somewhat different from the definition of the previous studies[10,12-13]. It would be more accurate to include substernal chest pain and food regurgitation to make a diagnosis of GERD[9,15]. Complete satisfaction of multitrait scaling criteria justifies combining the items into scales that can be scored with simple addition, thus eliminating the need for item weighting[16]. As our study confirmed there was no significant statistical difference between the two investigations. The Kappa-value was 0.4-0.75, which demonstrated no predominant consistency between the two diagnostic methods.
GERD becomes more common in Asian countries, resulting in more people coming to the gastroenterology outpatient department for treatment. A 13%-15% prevalence of reflux symptoms has been reported in Asian GERD patients, which is comparable with results in many Western series. However, the definition of GERD may alter estimated prevalence. In the present study, data for subjects with GERD symptoms (23.70%) support previous prevalence rates[17].
We showed for the first time that the prevalence of NERD in the Chinese is 10.60% (237 of 2231 investigated persons), which is lower than that of erosive esophagitis (20.80%), while the prevalence rate of symptomatic GERD is 10%-30% in Western countries, and more than half of the patients lack endoscopically proven erosive esophagitis[18,19]. In Western countries, the majority of patients with GERD have been reported to have NERD, but not erosive esophagitis, even in cases with severe symptoms[18].
The factors that determine the form of NERD versus erosive esophagitis have not yet been clarified. However, we elucidated differences in the possible causative factors of NERD and erosive esophagitis. By multivariate logistic regression analysis, it was found that old age, male, moderate working burden, divorced and strong tea remained as significant independent risk factors for erosive esophagitis, meanwhile, greasy food consumption, constipation were regarded as significant independent risk factors for NERD.
Several risk factors associated with GERD have been reported as follows. Old age has been shown to be associated with increased risk of erosive esophagitis, Berrat’s esophagus, and esophageal adenocarcinoma[20].
The previous studies showed that male gender is a risk factor for erosive esophagitis; whereas female is more likely to be associated with NERD[21,22]. Less parietal cell mass in women may be underlining reasons for the lower risk of GE[23].
Tea drinking has previously only been studied in a case series of reflux episodes[24]. While from another previous population-based study, the tea drinking does not seem to be a risk factor for GERD[25].
Coffee has been reported to be a reduced risk of reflux symptoms among coffee drinkers compared with non-coffee drinkers[25,26]. But previous cross sectional epidemiological studies have been able to establish that coffee drinking is a risk factor for GERD[24]. To accurately evaluate the long term effects of coffee drinking on the risk of reflux, an analysis of prospective exposure data would be necessary.
Smoking has often been cited as risk factors for GERD, although the findings of studies on this matter have been inconsistent[25,27]. Smoking was inversely related to NERD compared with RE[22]. Smoking decreases lower esophageal sphincter pressure and increases the frequency of reflux episodes. In addition, deleterious effects on esophageal defenses such as reduction of esophageal clearance and salivary function have been described[22].
Erosive esophagitis was positively related to alcohol consumption[28]. The mechanism is that alcohol intake induces nausea and vomiting and directly causes mucosal impairment, while food intake at late night elevates the risk of esophagitis[29].
In this cross sectional study, greasy food consumption was associated with an increased risk of GERD symptoms and erosive esophagitis. Several physiological studies of human volunteers have shown increased frequency of transient lower esophageal sphincter relaxation and increased esophageal acid exposure with greasy food consumption[30].
However, a limitation of the current study involves the subject sample. Subjects were outpatients from 10 hospitals and therefore probably represent a population of intermediate GERD severity between subjects recruited from gastrointestinal clinics and those randomly selected from the general population. In addition, other potential risk factors of GERD such as H pylori, hiatal hernia and BMI were not assessed in our study. Whether these factors are positively associated with GERD, calls for further observations.
In conclusion, GERD is a highly prevalent disease. Old age, male, moderate working burden, divorced and strong tea remained as significant independent risk factors for erosive esophagitis, meanwhile, midst bodily form, greasy food consumption, and constipation were considered as significant independent risk factors for NERD.
COMMENTS
Background
Gastroesophageal reflux disease (GERD) is a common disorder with a high occurrence of up to 10%-38% of adults in the Western population at least once a week. The prevalence of GERD has been increasing year after year. The diagnosis and treatment of GERD are important because the disease, in addition to the highly disturbing typical symptoms, has a series of known consequences. The presence of GERD may affect the patients' quality of life, decrease functional activity, increase the economic burden associated and highlight the risk of esophageal carcinoma in the cases of Barrett's esophagus. With an emphasis on morphological diagnosis, endoscopy has become a major tool to assess the final consequences of GERD, which is especially useful for population-based screening.
Research frontiers
The definition or the diagnostic parameters of GERD and the factors that determine the form of NERD versus erosive esophagitis have not yet been clarified.
Innovations and breakthroughs
Although many investigators have reported the prevalence of erosive esophagitis, the prevalence of NERD has not been investigated in China. We showed for the first time that the prevalence of NERD in the Chinese is 10.60% (237 of 2231 investigated persons), which is lower than that of erosive esophagitis (20.80%), While the rate of symptomatic GERD is 10% to 30% in Western countries, and more than half of these patients lack endoscopically proven erosive esophagitis. The factors that determine the form of NERD versus erosive esophagitis have not yet been clarified. However, we elucidated differences in the possible causative factors of NERD and erosive esophagitis.
Applications
Our study was designed to analyze a spectrum of GERD subjects based on presenting symptoms and endoscopic findings. In order to determine the risk factors for such disease in outpatients from department of internal medicine in Zhejiang Province of East China, a cross-sectional survey in a cluster random sample was conducted from November 2004 to June 2005.
Peer review
This is a report designed to analyze a spectrum of GERD subjects based on presenting symptoms and endoscopic findings in Eastern part of China, surveyed by RDQ Chinese version. This clinical study was well designed.The limitation of the study was absence of assessment of the other important risk factors of GERD such as H pylori, hiatal hernia, and BMI. It is well known that negative association between H pylori and GORD does exist, especially in Asia (Kupcinskas L, Malfertheiner P. Helicobacter. 2005; 10 Suppl 1: 26-33). In case the other GERD risk factors would be assessed, the results of multivariate analysis could be substantially different.
Footnotes
S- Editor Liu Y L- Editor Ma JY E- Editor Wang HF
References
- 1.Kennedy T, Jones R. The prevalence of gastro-oesophageal reflux symptoms in a UK population and the consultation behaviour of patients with these symptoms. Aliment Pharmacol Ther. 2000;14:1589–1594. doi: 10.1046/j.1365-2036.2000.00884.x. [DOI] [PubMed] [Google Scholar]
- 2.Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 3.Shaw MJ, Talley NJ, Beebe TJ, Rockwood T, Carlsson R, Adlis S, Fendrick AM, Jones R, Dent J, Bytzer P. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:52–57. doi: 10.1111/j.1572-0241.2001.03451.x. [DOI] [PubMed] [Google Scholar]
- 4.Chen M, Xiong L, Chen H, Xu A, He L, Hu P. Prevalence, risk factors and impact of gastroesophageal reflux disease symptoms: a population-based study in South China. Scand J Gastroenterol. 2005;40:759–767. doi: 10.1080/00365520510015610. [DOI] [PubMed] [Google Scholar]
- 5.Wahlqvist P. Symptoms of gastroesophageal reflux disease, perceived productivity, and health-related quality of life. Am J Gastroenterol. 2001;96:S57–S61. doi: 10.1016/s0002-9270(01)02590-4. [DOI] [PubMed] [Google Scholar]
- 6.Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C, Gemmen E, Shah S, Avdic A, Rubin R. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500–1511. doi: 10.1053/gast.2002.32978. [DOI] [PubMed] [Google Scholar]
- 7.Moss SF, Armstrong D, Arnold R, Ferenci P, Fock KM, Holtmann G, McCarthy DM, Moraes-Filho JP, Mutschler E, Playford R, et al. GERD 2003 -- a consensus on the way ahead. Digestion. 2003;67:111–117. doi: 10.1159/000071290. [DOI] [PubMed] [Google Scholar]
- 8.Amano K, Adachi K, Katsube T, Watanabe M, Kinoshita Y. Role of hiatus hernia and gastric mucosal atrophy in the development of reflux esophagitis in the elderly. J Gastroenterol Hepatol. 2001;16:132–136. doi: 10.1046/j.1440-1746.2001.02408.x. [DOI] [PubMed] [Google Scholar]
- 9.Value of reflux diagnostic questionnaire in the diagnosis of gastroesophageal reflux disease. Chin J Dig Dis. 2004;5:51–55. doi: 10.1111/j.1443-9573.2004.00155.x. [DOI] [PubMed] [Google Scholar]
- 10.Talley NJ, Fullerton S, Junghard O, Wiklund I. Quality of life in patients with endoscopy-negative heartburn: reliability and sensitivity of disease-specific instruments. Am J Gastroenterol. 2001;96:1998–2004. doi: 10.1111/j.1572-0241.2001.03932.x. [DOI] [PubMed] [Google Scholar]
- 11.Streiner DL, Norman GR. Health measurement scales: A practical guide to their development and use. Oxford: Oxford University Press; 1995. [Google Scholar]
- 12.Carlsson R, Dent J, Bolling-Sternevald E, Johnsson F, Junghard O, Lauritsen K, Riley S, Lundell L. The usefulness of a structured questionnaire in the assessment of symptomatic gastroesophageal reflux disease. Scand J Gastroenterol. 1998;33:1023–1029. doi: 10.1080/003655298750026697. [DOI] [PubMed] [Google Scholar]
- 13.Locke GR, Talley NJ, Weaver AL, Zinsmeister AR. A new questionnaire for gastroesophageal reflux disease. Mayo Clin Proc. 1994;69:539–547. doi: 10.1016/s0025-6196(12)62245-9. [DOI] [PubMed] [Google Scholar]
- 14.McColl E. Best practice in symptom assessment: a review. Gut. 2004;53 Suppl 4:iv49–iv54. doi: 10.1136/gut.2003.034355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong WM, Lam KF, Lai KC, Hui WM, Hu WH, Lam CL, Wong NY, Xia HH, Huang JQ, Chan AO, et al. A validated symptoms questionnaire (Chinese GERDQ) for the diagnosis of gastro-oesophageal reflux disease in the Chinese population. Aliment Pharmacol Ther. 2003;17:1407–1413. doi: 10.1046/j.1365-2036.2003.01576.x. [DOI] [PubMed] [Google Scholar]
- 16.Shaw M. Diagnostic utility of reflux disease symptoms. Gut. 2004;53 Suppl 4:iv25–iv27. doi: 10.1136/gut.2003.034280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–180. doi: 10.1136/gut.45.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fass R, Fennerty MB, Vakil N. Nonerosive reflux disease--current concepts and dilemmas. Am J Gastroenterol. 2001;96:303–314. doi: 10.1111/j.1572-0241.2001.03511.x. [DOI] [PubMed] [Google Scholar]
- 19.Agréus L, Svärdsudd K, Talley NJ, Jones MP, Tibblin G. Natural history of gastroesophageal reflux disease and functional abdominal disorders: a population-based study. Am J Gastroenterol. 2001;96:2905–2914. doi: 10.1111/j.1572-0241.2001.04680.x. [DOI] [PubMed] [Google Scholar]
- 20.Sonnenberg A, El-Serag HB. Clinical epidemiology and natural history of gastroesophageal reflux disease. Yale J Biol Med. 1999;72:81–92. [PMC free article] [PubMed] [Google Scholar]
- 21.Lee YC, Wang HP, Chiu HM, Liao SC, Huang SP, Lai YP, Wu MS, Chen MF, Lin JT. Comparative analysis between psychological and endoscopic profiles in patients with gastroesophageal reflux disease: a prospective study based on screening endoscopy. J Gastroenterol Hepatol. 2006;21:798–804. doi: 10.1111/j.1440-1746.2005.04034.x. [DOI] [PubMed] [Google Scholar]
- 22.Fujiwara Y, Higuchi K, Shiba M, Yamamori K, Watanabe Y, Sasaki E, Tominaga K, Watanabe T, Oshitani N, Arakawa T. Differences in clinical characteristics between patients with endoscopy-negative reflux disease and erosive esophagitis in Japan. Am J Gastroenterol. 2005;100:754–758. doi: 10.1111/j.1572-0241.2005.40966.x. [DOI] [PubMed] [Google Scholar]
- 23.El-Serag HB, Graham DY, Satia JA, Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005;100:1243–1250. doi: 10.1111/j.1572-0241.2005.41703.x. [DOI] [PubMed] [Google Scholar]
- 24.Chang CS, Poon SK, Lien HC, Chen GH. The incidence of reflux esophagitis among the Chinese. Am J Gastroenterol. 1997;92:668–671. [PubMed] [Google Scholar]
- 25.Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut. 2004;53:1730–1735. doi: 10.1136/gut.2004.043265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brazer SR, Onken JE, Dalton CB, Smith JW, Schiffman SS. Effect of different coffees on esophageal acid contact time and symptoms in coffee-sensitive subjects. Physiol Behav. 1995;57:563–567. doi: 10.1016/0031-9384(94)00363-a. [DOI] [PubMed] [Google Scholar]
- 27.Nocon M, Labenz J, Willich SN. Lifestyle factors and symptoms of gastro-oesophageal reflux -- a population-based study. Aliment Pharmacol Ther. 2006;23:169–174. doi: 10.1111/j.1365-2036.2006.02727.x. [DOI] [PubMed] [Google Scholar]
- 28.Lee SJ, Song CW, Jeen YT, Chun HJ, Lee HS, Um SH, Lee SW, Choi JH, Kim CD, Ryu HS, et al. Prevalence of endoscopic reflux esophagitis among Koreans. J Gastroenterol Hepatol. 2001;16:373–376. doi: 10.1046/j.1440-1746.2001.02464.x. [DOI] [PubMed] [Google Scholar]
- 29.Castell DO, Murray JA, Tutuian R, Orlando RC, Arnold R. Review article: the pathophysiology of gastro-oesophageal reflux disease - oesophageal manifestations. Aliment Pharmacol Ther. 2004;20 Suppl 9:14–25. doi: 10.1111/j.1365-2036.2004.02238.x. [DOI] [PubMed] [Google Scholar]
- 30.Hills JM, Aaronson PI. The mechanism of action of peppermint oil on gastrointestinal smooth muscle. An analysis using patch clamp electrophysiology and isolated tissue pharmacology in rabbit and guinea pig. Gastroenterology. 1991;101:55–65. doi: 10.1016/0016-5085(91)90459-x. [DOI] [PubMed] [Google Scholar]


