Abstract
AIM: To evaluate the risk factors for lateral lymph node metastasis in patients with advanced low rectal cancer, in order to make the effective selection of patients who could benefit from lateral lymph node dissection, as well as the relationship of lateral lymph node metastasis with local recurrence and survival of patients with advanced low rectal cancer.
METHODS: A total of 96 consecutive patients who underwent curative surgery with lateral pelvic lymphadenectomy for advanced lower rectal cancer were retrospectively analyzed. The relation of lateral lymph node metastasis with clinicopathologic characteristics, local recurrence and survival of patients was identified.
RESULTS: Lateral lymph node metastasis was observed in 14.6% (14/96) of patients with advanced low rectal cancer. Lateral lymph node metastasis was detected in 10 (25.0%) of 40 patients with tumor diameter ≥ 5 cm and in 4 (7.1%) of 56 patients with tumor diameter < 5 cm. The difference between the two groups was statistically significant (χ2 = 5.973, P = 0.015). Lateral lymph node metastasis was more frequent in patients with 4/4 diameter of tumor infiltration (7 of 10 cases, 70.0%), compared with patients with 3/4, 2/4 and 1/4 diameter of tumor infiltration (3 of 25 cases, 12.0%; 3 of 45 cases, 6.7%; 1 of 16 cases, 6.3%) (χ2 = 27.944, P = 0.0001). The lateral lymph node metastasis rate was 30.0% (9 of 30 cases), 9.1% (4 of 44 cases) and 4.5% (1 of 22 cases) for poorly, moderately and well-differentiated carcinoma, respectively. The difference between the three groups was statistically significant (χ2 = 8.569, P = 0.014). Local recurrence was 18.8% (18 of 96 cases), 64.3% (9 of 14 cases), and 11.0% (9 of 82 cases) in patients with advanced low rectal cancer, in those with and without lateral lymph node metastasis, respectively. The difference between the two groups was statistically significant (χ2 = 22.308, P = 0.0001). Kaplan-Meier survival analysis showed significant improvements in median survival (80.9 ± 2.1 m, 95% CI: 76.7-85.1 m vs 38 ± 6.7 m, 95% CI: 24.8-51.2 m) of patients without lateral lymph node metastasis compared with those with lateral lymph node metastasis (log-rank, P = 0.0001).
CONCLUSION: Tumor diameter, infiltration and differentiation are significant risk factors for lateral lymph node metastasis. Lateral pelvic lymphadenectomy should be performed following surgery for patients with tumor diameter ≥ 5 cm. Lateral lymph node metastasis is an important predictor for local recurrence and survival in patients with advanced low rectal cancer.
Keywords: Low rectal cancer, Lateral lymph node metastasis, Local recurrence, Prognosis
INTRODUCTION
It is well known that rectal carcinoma is one of the most common carcinomas in China. Since total mesorectal excision was adopted as the standard treatment of patients with rectal carcinoma, improvements have been made in decreasing its local recurrence and prolonging survival of patients[1-8]. However, even having undergone radical resection with total mesorectal excision, about 5%-40% of patients with rectal carcinoma have local recurrence[9-14]. The survival of patients with advanced low rectal cancer still remains poor. It was reported that lateral lymph node metastasis may be the most important factor for local recurrence and poor prognosis of advanced low rectal cancer[15-18]. In the current study, the data on 96 consecutive patients who underwent curative surgery with total mesorectal excision and lateral lymph node dissection for advanced low rectal cancer at the Department of General Surgery of Guangdong Provincial People’s Hospital were retrospectively analyzed. The relationship of lateral lymph node metastasis with local recurrence was identified. The prognostic value of lateral lymph node metastasis for advanced low rectal cancer was also evaluated. Moreover, the risk factors for lateral lymph node metastasis and indications of lateral lymph node dissection remain unclear. Therefore, this study was to explore the risk factors for lateral lymph node metastasis in order to make effective selection of patients who could benefit from lateral pelvic lymphadenectomy. The relation of lateral lymph node metastasis with clinicopathologic characteristics of advanced low rectal cancer was analyzed.
MATERIALS AND METHODS
Patients and methods
A total of 96 consecutive patients who underwent curative surgery with total mesorectal excision and lateral lymph node dissection for advanced low rectal cancer at the Department of General Surgery of Guangdong Provincial People’s Hospital were retrospectively analyzed. There were 46 men and 50 women, ranging in age from 25 to 86 years, with a mean age of 65 years. None of these patients received preoperative chemotherapy or radiotherapy. Twenty-one patients (21.9%) had a family history, 40 patients (41.6%) had a high cancer embryonic antigen (CEA) level and a tumor diameter ≥ 5 cm, 56 had a tumor diameter < 5 cm. According to the Ming’s criteria, 42 tumors were classified as expansive type carcinoma, 54 tumors as infiltrative type carcinoma. Fifty-six patients (58.3%) had positive lymph node metastases and 36 patients (37.5%) had positive vessel cancerous emboli. Thirty patients had a poorly differentiated carcinoma, 44 patients had a moderately differentiated carcinoma, 22 patients had a well-differentiated carcinoma. Low anterior resection was performed in 68 patients and abdominal perineal resection in 28 patients. A total of 1776 lymph nodes were dissected from these 96 patients (average 18.5 lymph nodes per patient). Two pathologists who were blinded to the clinicopathological data observed the specimens independently.
Statistical analysis
Statistical analysis was performed by chi-square test to examine the association of lateral lymph node metastasis with clinicopathologic characteristics and local recurrence of advanced low rectal cancer. The relationship between lateral lymph node metastasis and survival in patients with advanced low rectal cancer was evaluated by Kaplan-Meier survival analysis and log-rank test. P < 0.05 was considered statistically significant.
RESULTS
Correlation between lateral lymph node metastasis and clinicopathologic characteristics of advanced low rectal cancer
Lateral lymph node metastasis was observed in 14.6 (14/96) of patients with advanced low rectal cancer. Lateral lymph node metastasis was detected in 10 (25.0%) of 40 patients with tumor diameter ≥ 5 cm and in 4 (7.1%) of 56 patients with tumor diameter < 5 cm. The difference between the two groups was statistically significant (χ2 = 5.973, P = 0.015). Lateral lymph node metastasis was more frequent in patients with 4/4 diameter of tumor infiltration (7 of 10 cases, 70.0%), compared with patients with 3/4, 2/4 and 1/4 diameter of tumor infiltration (3 of 25 cases, 12.0%; 3 of 45 cases, 6.7%; 1 of 16 cases, 6.3%) (χ2 = 27.944, P = 0.000). The lateral lymph node metastasis rate for poorly, moderately and well differentiated carcinoma was 30.0% (9 of 30 cases), 9.1% (4 of 44 cases) and 4.5% (1 of 22 cases), respectively. The difference between the three groups was statistically significant (χ2 = 8.569, P = 0.014). No significant correlation was found between lateral lymph node metastasis and other variables such as gender (χ2 = 0.168, P = 0.682), age (χ2 = 0.103, P = 0.749), family history (χ2 = 0.430, P = 0.512), high CEA level (χ2 = 0.468, P = 0.494), Ming’s classification (χ2 = 0.430, P = 0.512), lymph node metastases (χ2 = 0.239, P = 0.625) and vessel cancerous emboli (χ2 = 0.201, P = 0.654) (Table 1).
Table 1.
Relations between lateral lymph node metastasis and clinicopathologic characteristics of patients with advanced low rectal cancer
| Variable | n |
Lateral lymph node metastasis |
||
| Positive (%) | Negative (%) | χ2/P value | ||
| Gender | ||||
| Male | 46 | 6 (13.0) | 40 (87.0) | |
| Female | 50 | 8 (16.0) | 42 (84.0) | χ2 = 0.168/P = 0.682 |
| Age (yr) | ||||
| < 60 | 38 | 5 (13.2) | 33 (86.8) | |
| ≥ 60 | 58 | 9 (15.5) | 49 (84.5) | χ2 = 0.103/P = 0.749 |
| Family history | ||||
| Yes | 21 | 4 (19.0) | 17 (81.0) | |
| No | 75 | 10 (13.3) | 65 (86.7) | χ2 = 0.430/P = 0.512 |
| CEA level | ||||
| High | 40 | 7 (17.5) | 33 (82.5) | |
| Normal | 56 | 7 (14.6) | 49 (85.4) | χ2 = 0.468/P = 0.494 |
| Superficial diameter (cm) | ||||
| < 5 | 56 | 4 (7.1) | 52 (92.9) | |
| ≥ 5 | 40 | 10 (25.0) | 30 (75.0) | χ2 = 5.973/P = 0.015 |
| Diameter of infiltration | ||||
| 1/4 | 16 | 1 (6.3) | 15 (93.7) | |
| 1/2 | 45 | 3 (6.7) | 42 (93.3) | |
| 3/4 | 25 | 3 (12.0) | 22 (88.0) | |
| 4/4 | 10 | 7 (70.0) | 3 (30.0) | χ2 = 27.944/P = 0.000 |
| Ming’s classification | ||||
| Expansive | 42 | 5 (11.9) | 37 (88.1) | |
| Infiltrative | 54 | 9 (16.7) | 45 (83.3) | χ2 = 0.430/P = 0.512 |
| Histologic differentiation | ||||
| Well | 22 | 1 (4.5) | 21 (95.5) | |
| Moderate | 44 | 4 (9.1) | 40 (90.9) | |
| Poorly | 30 | 9 (30.0) | 21 (70.0) | χ2 = 8.569/P = 0.014 |
| Lymph node metastasis | ||||
| Positive | 56 | 9 (16.1) | 47 (83.9) | |
| Negative | 40 | 5 (12.5) | 35 (87.5) | χ2 = 0.239/P = 0.625 |
| Vessel cancerous emboli | ||||
| Positive | 36 | 6 (16.7) | 30 (83.3) | |
| Negative | 60 | 8 (13.3) | 52 (86.7) | χ2 = 0.201/P = 0.654 |
CEA: Carcinoma embryonic antigen.
Correlation between lateral lymph node metastasis and local recurrence of advanced low rectal cancer
Local recurrence was 18.8% (18 of 96 cases), 64.3% (9 of 14 cases), and 11.0% (9 of 82 cases) in patients with advanced low rectal cancer and those with and without lateral lymph node metastasis The difference between the two groups was statistically significant (χ2 = 22.308, P = 0.0001).
Correlation between lateral lymph node metastasis and survival in patients with advanced low rectal cancer
In a median follow-up period of 73 (range 16-90) mo, Kaplan-Meier survival analysis showed a significantly improved median survival (80.9 ± 2.1 m, 95% CI: 76.7-85.1 m vs 38 ± 6.7 m, 95% CI: 24.8-51.2 m) in patients without lateral lymph node metastasis compared with those with lateral lymph node metastasis. The difference between the two groups was statistically significant (log-rank, P = 0.0001) (Figure 1).
Figure 1.
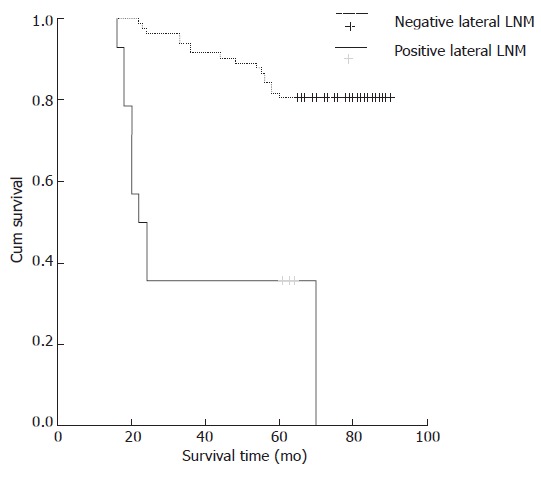
Relations between lateral lymph node metastasis and survival of patients with advanced low rectal cancer (Kaplan-Meier survival analysis). LNM: Lymph node metastasis.
DISCUSSION
Lateral pelvic lymphadenectomy for advanced low rectal cancer is controversial[19-25]. In Japan, lateral pelvic lymphadenectomy is routinely performed for patients with advanced low rectal cancer, whereas it is not frequently performed in the Western countries[26-28]. In the current study, a retrospective analysis was performed in 96 patients with advanced low rectal cancer who underwent curative surgery with lateral lymph node dissection. The relations of lateral lymph node metastasis with clinicopathologic characteristics, local recurrence and survival of advanced low rectal cancer were analyzed.
In our study, lateral lymph node metastasis was observed in 14.6% (14/96) of patients with advanced low rectal cancer, showing a significant correlation with tumor diameter, infiltration and differentiation. Lateral lymph node metastasis was found in 10 (25.0%) of 40 patients with tumor diameter ≥ 5 cm and in 4 (7.1%) of 56 patients with tumor diameter < 5 cm (χ2 = 5.973, P = 0.015). Lateral lymph node metastasis was more frequent in patients with 4/4 diameter of tumor infiltration (7 of 10 cases, 70.0%) than in patients with 3/4, 2/4 and 1/4 diameter of tumor infiltration (3 of 25 cases, 12.0%; 3 of 45 cases, 6.7%; 1 of 16 cases, 6.3%) (χ2 = 27.944, P = 0.000). The lateral lymph node metastasis rate of poorly, moderately and well differentiated carcinoma was 30.0% (9 of 30 cases), 9.1% (4 of 44 cases) and 4.5% (1 of 22 cases), respectively (χ2 = 8.569, P = 0.014), indicating that tumor diameter ≥ 5 cm, tumor infiltration and differentiation are risk factors for lateral lymph node metastasis of advanced low rectal cancer. Therefore, lateral pelvic lymphadenectomy should be performed following the management of patients with tumor diameter ≥ 5 cm, tumor infiltration or differentiation.
It is well known that local recurrence is the most important prognostic factor for rectal carcinoma[29-31]. It was reported that local recurrence can be found in 4%-50% of patients with rectal carcinoma after curative resection, and lateral lymph node metastasis may be the important factor for local recurrence[15,16]. Ueno et al[15] reported that patients with lateral node metastases have an increased risk for local recurrence (44% vs 11.7%; P < 0.001) compared with those without lateral node metastases. Sugihara et al[16] also reported that positive lateral lymph nodes are significantly associated with increased local recurrence of rectal cancer. Similarly in this study, lateral lymph node metastasis was significantly correlated with local recurrence of advanced low rectal cancer. The local recurrence rate of advanced low rectal cancer was 64.3% (9 of 14 cases) and 11.0% (9 of 82 cases) in patients with and without lateral lymph node metastasis (χ2 = 22.308, P = 0.000), respectively, indicating that lateral pelvic lymphadenectomy can significantly reduce local recurrence of advanced low rectal cancer.
In the present study, patients without lateral lymph node metastasis had significant improvements in median survival (80.9 ± 2.1 m, 95% CI: 76.7-85.1 m vs 38 ± 6.7 m, 95% CI: 24.8-51.2 m) compared to those with lateral lymph node metastasis. The difference between the two groups was statistically significant (log-rank, P = 0.0001), supporting that lateral lymph node metastasis has a significant prognostic value for advanced low rectal cancer. Lateral pelvic lymphadenectomy may effectively improve the survival of patients with advanced low rectal cancer. Ueno et al[32] also reported that advanced low rectal cancer patients having lymph node involvement in the lateral pelvic area are likely to benefit from lymphadenectomy.
COMMENTS
Background
Even having undergone radical resection with total mesorectal excision, about 5%-40% of patients with rectal cancer have local recurrence. The survival of patients with advanced low rectal cancer remains poor. Whether patients with advanced low rectal cancer could benefit from lateral lymph node dissection is still controversial.
Research frontiers
At present, lateral lymphadenectomy for advanced low rectal cancer is controversial. However, lateral lymph node metastasis is significantly associated with local recurrence and poor prognosis of advanced low rectal cancer.
Innovations and breakthroughs
The results of this study indicate that tumor diameter ≥ 5 cm, tumor infiltration and differentiation are risk factors for lateral lymph node metastasis of advanced low rectal cancer. Lateral lymph node metastasis is significantly correlated with local recurrence and prognosis of advanced low rectal cancer.
Applications
Lateral pelvic lymphadenectomy may effectively reduce local recurrence and improve the survival in patients with advanced low rectal cancer.
Peer review
The present study investigated the relations of lateral lymph node metastasis with local recurrence and survival in patients with advanced low rectal cancer. The study design is good and data analysis is extensive. The manuscript is well written.
Footnotes
Supported by the WST Foundation of Guangdong Province, No. 2000112736580706003
S- Editor Zhu LH L- Editor Wang XL E- Editor Lu W
References
- 1.Laurent C, Nobili S, Rullier A, Vendrely V, Saric J, Rullier E. Efforts to improve local control in rectal cancer compromise survival by the potential morbidity of optimal mesorectal excision. J Am Coll Surg. 2006;203:684–691. doi: 10.1016/j.jamcollsurg.2006.07.021. [DOI] [PubMed] [Google Scholar]
- 2.Bernardshaw SV, Øvrebø K, Eide GE, Skarstein A, Røkke O. Treatment of rectal cancer: reduction of local recurrence after the introduction of TME - experience from one University Hospital. Dig Surg. 2006;23:51–59. doi: 10.1159/000093494. [DOI] [PubMed] [Google Scholar]
- 3.Liang YC, Qing SH, Ding WX, Chen PY, Huang YB, Yu HT. Total mesorectal excision versus conventional radical surgery for rectal cancer: a meta analysis. Zhonghua Weichangwaike Zazhi. 2007;10:43–48. [PubMed] [Google Scholar]
- 4.Tzardi M. Role of total mesorectal excision and of circumferential resection margin in local recurrence and survival of patients with rectal carcinoma. Dig Dis. 2007;25:51–55. doi: 10.1159/000099170. [DOI] [PubMed] [Google Scholar]
- 5.Wibe A, Eriksen MT, Syse A, Myrvold HE, Søreide O. Total mesorectal excision for rectal cancer--what can be achieved by a national audit? Colorectal Dis. 2003;5:471–477. doi: 10.1046/j.1463-1318.2003.00506.x. [DOI] [PubMed] [Google Scholar]
- 6.Visser O, Bakx R, Zoetmulder FA, Levering CC, Meijer S, Slors JF, van Lanschot JJ. The influence of total mesorectal excision on local recurrence and survival in rectal cancer patients: a population-based study in Greater Amsterdam. J Surg Oncol. 2007;95:447–454. doi: 10.1002/jso.20713. [DOI] [PubMed] [Google Scholar]
- 7.Szynglarewicz B, Matkowski R, Forgacz J, Pudelko M, Smorag Z, Dryl J, Kornafel J. Clinical factors in prediction of prognosis after anterior resection with total mesorectal excision for carcinoma of the rectum. Oncol Rep. 2007;17:471–475. [PubMed] [Google Scholar]
- 8.Mortenson MM, Khatri VP, Bennett JJ, Petrelli NJ. Total mesorectal excision and pelvic node dissection for rectal cancer: an appraisal. Surg Oncol Clin N Am. 2007;16:177–197. doi: 10.1016/j.soc.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Radice E, Dozois RR. Locally recurrent rectal cancer. Dig Surg. 2001;18:355–362. doi: 10.1159/000050173. [DOI] [PubMed] [Google Scholar]
- 10.Piso P, Dahlke MH, Mirena P, Schmidt U, Aselmann H, Schlitt HJ, Raab R, Klempnauer J. Total mesorectal excision for middle and lower rectal cancer: a single institution experience with 337 consecutive patients. J Surg Oncol. 2004;86:115–121. doi: 10.1002/jso.20062. [DOI] [PubMed] [Google Scholar]
- 11.Maslekar S, Sharma A, Macdonald A, Gunn J, Monson JR, Hartley JE. Do supervised colorectal trainees differ from consultants in terms of quality of TME surgery? Colorectal Dis. 2006;8:790–794. doi: 10.1111/j.1463-1318.2006.01127.x. [DOI] [PubMed] [Google Scholar]
- 12.Rengan R, Paty PB, Wong WD, Guillem JG, Weiser M, Temple L, Saltz L, Minsky BD. Ten-year results of preoperative radiation followed by sphincter preservation for rectal cancer: increased local failure rate in nonresponders. Clin Colorectal Cancer. 2006;5:413–421. doi: 10.3816/CCC.2006.n.012. [DOI] [PubMed] [Google Scholar]
- 13.Hohenberger W, Merkel S, Matzel K, Bittorf B, Papadopoulos T, Göhl J. The influence of abdomino-peranal (intersphincteric) resection of lower third rectal carcinoma on the rates of sphincter preservation and locoregional recurrence. Colorectal Dis. 2006;8:23–33. doi: 10.1111/j.1463-1318.2005.00839.x. [DOI] [PubMed] [Google Scholar]
- 14.Lezoche E, Guerrieri M, De Sanctis A, Campagnacci R, Baldarelli M, Lezoche G, Paganini AM. Long-term results of laparoscopic versus open colorectal resections for cancer in 235 patients with a minimum follow-up of 5 years. Surg Endosc. 2006;20:546–553. doi: 10.1007/s00464-005-0338-8. [DOI] [PubMed] [Google Scholar]
- 15.Ueno M, Oya M, Azekura K, Yamaguchi T, Muto T. Incidence and prognostic significance of lateral lymph node metastasis in patients with advanced low rectal cancer. Br J Surg. 2005;92:756–763. doi: 10.1002/bjs.4975. [DOI] [PubMed] [Google Scholar]
- 16.Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, Shirouzu K, Muto T. Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 2006;49:1663–1672. doi: 10.1007/s10350-006-0714-z. [DOI] [PubMed] [Google Scholar]
- 17.Fujita S, Yamamoto S, Akasu T, Moriya Y. Lateral pelvic lymph node dissection for advanced lower rectal cancer. Br J Surg. 2003;90:1580–1585. doi: 10.1002/bjs.4350. [DOI] [PubMed] [Google Scholar]
- 18.Ueno H, Mochizuki H, Hashiguchi Y, Hase K. Prognostic determinants of patients with lateral nodal involvement by rectal cancer. Ann Surg. 2001;234:190–197. doi: 10.1097/00000658-200108000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sadahiro S, Ishikawa K, Suzuki T, Mukoyama S, Tanaka Y, Yasuda S, Tajima T, Makuuchi H. [Optimal lymph node dissection for colorectal cancer] Nihon Geka Gakkai Zasshi. 2001;102:497–500. [PubMed] [Google Scholar]
- 20.Nagawa H, Muto T, Sunouchi K, Higuchi Y, Tsurita G, Watanabe T, Sawada T. Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum. 2001;44:1274–1280. doi: 10.1007/BF02234784. [DOI] [PubMed] [Google Scholar]
- 21.Shiozawa M, Akaike M, Yamada R, Godai T, Yamamoto N, Saito H, Sugimasa Y, Takemiya S, Rino Y, Imada T. Lateral lymph node dissection for lower rectal cancer. Hepatogastroenterology. 2007;54:1066–1070. [PubMed] [Google Scholar]
- 22.Di Matteo G, Peparini N, Maturo A, Di Matteo FM, Zeri KP, Redler A, Mascagni D. Lateral pelvic lymphadenectomy and total nerve sparing for locally advanced rectal cancer in Western patients. Panminerva Med. 2001;43:95–101. [PubMed] [Google Scholar]
- 23.Shirouzu K, Ogata Y, Araki Y, Sasatomi T, Nozoe Y, Nakagawa M, Matono K. Total mesorectal excision, lateral lymphadenectomy and autonomic nerve preservation for lower rectal cancer: significance in the long-term follow-up study. Kurume Med J. 2001;48:307–319. doi: 10.2739/kurumemedj.48.307. [DOI] [PubMed] [Google Scholar]
- 24.Koda K, Saito N, Oda K, Takiguchi N, Sarashina H, Miyazaki M. Evaluation of lateral lymph node dissection with preoperative chemo-radiotherapy for the treatment of advanced middle to lower rectal cancers. Int J Colorectal Dis. 2004;19:188–194. doi: 10.1007/s00384-003-0548-2. [DOI] [PubMed] [Google Scholar]
- 25.Sato H, Maeda K, Maruta M, Masumori K, Koide Y. Who can get the beneficial effect from lateral lymph node dissection for Dukes C rectal carcinoma below the peritoneal reflection? Dis Colon Rectum. 2006;49:S3–12. doi: 10.1007/s10350-006-0699-7. [DOI] [PubMed] [Google Scholar]
- 26.Koch M, Kienle P, Antolovic D, Büchler MW, Weitz J. Is the lateral lymph node compartment relevant? Recent Results Cancer Res. 2005;165:40–45. doi: 10.1007/3-540-27449-9_6. [DOI] [PubMed] [Google Scholar]
- 27.Kusunoki M, Inoue Y. Current surgical management of rectal cancer. Dig Surg. 2007;24:115–119. doi: 10.1159/000101898. [DOI] [PubMed] [Google Scholar]
- 28.Matsuoka H, Masaki T, Sugiyama M, Atomi Y. Impact of lateral pelvic lymph node dissection on evacuatory and urinary functions following low anterior resection for advanced rectal carcinoma. Langenbecks Arch Surg. 2005;390:517–522. doi: 10.1007/s00423-005-0577-0. [DOI] [PubMed] [Google Scholar]
- 29.Noda K, Umekita N, Tanaka S, Ohkubo T, Inoue S, Kitamura M. [A clinical study of therapy for local recurrent rectal cancer] Gan To Kagaku Ryoho. 2006;33:1830–1833. [PubMed] [Google Scholar]
- 30.Bedrosian I, Giacco G, Pederson L, Rodriguez-Bigas MA, Feig B, Hunt KK, Ellis L, Curley SA, Vauthey JN, Delclos M, et al. Outcome after curative resection for locally recurrent rectal cancer. Dis Colon Rectum. 2006;49:175–182. doi: 10.1007/s10350-005-0276-5. [DOI] [PubMed] [Google Scholar]
- 31.Moriya Y, Akasu T, Fujita S, Yamamoto S. Total pelvic exenteration with distal sacrectomy for fixed recurrent rectal cancer. Surg Oncol Clin N Am. 2005;14:225–238. doi: 10.1016/j.soc.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 32.Ueno H, Mochizuki H, Hashiguchi Y, Ishiguro M, Miyoshi M, Kajiwara Y, Sato T, Shimazaki H, Hase K. Potential prognostic benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection. Ann Surg. 2007;245:80–87. doi: 10.1097/01.sla.0000225359.72553.8c. [DOI] [PMC free article] [PubMed] [Google Scholar]


